Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Pediatric Rehabilitation Program Development interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Pediatric Rehabilitation Program Development Interview
Q 1. Describe your experience in developing and implementing pediatric rehabilitation programs.
My experience in developing and implementing pediatric rehabilitation programs spans over 15 years, encompassing various settings from large hospital systems to smaller community-based clinics. I’ve been involved in the entire program lifecycle, from initial needs assessment and program design to implementation, evaluation, and ongoing refinement. For example, at Children’s Hospital, I led the development of a new program for children with cerebral palsy, which involved recruiting a specialized team, securing funding, designing a comprehensive curriculum, and implementing a robust data collection system to track progress. This program significantly improved patient outcomes, as measured by increased functional independence and reduced caregiver burden. In another instance, at a smaller clinic, I helped revamp an existing program for children with autism spectrum disorder, integrating new evidence-based therapies and improving interdisciplinary collaboration. This resulted in increased engagement and better therapeutic outcomes for the children involved.
Q 2. How do you assess the needs of children requiring pediatric rehabilitation services?
Assessing the needs of children requiring pediatric rehabilitation services is a multi-faceted process that involves gathering information from various sources. It starts with a comprehensive evaluation of the child’s medical history, developmental milestones, and current functional abilities. We use standardized assessments like the Gross Motor Function Measure (GMFM) or the Bayley Scales of Infant and Toddler Development to obtain objective measurements. However, it is equally important to understand the family’s perspective, their goals for the child, and the challenges they face in supporting their child’s development. We involve parents and caregivers in the assessment process, ensuring their input is valued and integrated into the plan of care. This holistic approach ensures we address not only the child’s physical, cognitive, and emotional needs but also the family’s needs and priorities.
For instance, a child diagnosed with a traumatic brain injury might require assessments focusing on cognitive function, speech therapy, and physical therapy needs. These assessments would guide the creation of a tailored program to address their specific deficits and reach their unique rehabilitation goals.
Q 3. Explain your approach to designing a comprehensive pediatric rehabilitation program.
Designing a comprehensive pediatric rehabilitation program involves a structured, systematic approach. It begins with clearly defined goals and objectives, aligned with the needs identified during the assessment process. We then create an individualized plan of care for each child, outlining specific interventions, frequency of treatment, and expected outcomes. This plan is developed collaboratively with the family, therapists, and other healthcare professionals involved. The program should incorporate a range of therapeutic modalities tailored to the child’s individual needs, including physical therapy, occupational therapy, speech therapy, and potentially psychological support. It’s crucial to consider the child’s age, developmental stage, and learning style when choosing these interventions. We also focus on incorporating family-centered care, providing education and support to parents and caregivers so they can actively participate in their child’s rehabilitation journey. Regular progress monitoring is crucial, allowing us to adjust the program as needed to optimize outcomes.
Think of it like building a house: The assessment phase is like surveying the land and determining the client’s needs (foundation). The design phase is where we plan the structure and rooms (program design). Finally, construction and ongoing maintenance are the implementation and evaluation (program implementation and refinement).
Q 4. What are the key performance indicators (KPIs) you would use to measure the success of a pediatric rehabilitation program?
Key Performance Indicators (KPIs) for a successful pediatric rehabilitation program are multifaceted and should reflect both clinical and functional outcomes. These include:
- Functional improvements: Measured through standardized assessments such as the GMFM or Pediatric Evaluation of Disability Inventory (PEDI), tracking progress in areas like mobility, self-care, and communication.
- Participation in activities: Assessing the child’s ability to engage in daily activities and participate in social settings.
- Parent/caregiver satisfaction: Gauging their satisfaction with the program’s effectiveness and the services provided using surveys or feedback sessions.
- Discharge readiness: Measuring the child’s preparedness for transitioning back to their home environment and community.
- Treatment adherence: Tracking attendance rates and compliance with the treatment plan.
- Team collaboration effectiveness: Monitoring interdisciplinary communication and the efficiency of team meetings.
By tracking these KPIs, we can objectively evaluate the program’s effectiveness and identify areas for improvement. For example, a low parent satisfaction score might indicate a need for improved communication or family-centered care practices.
Q 5. How do you ensure the program aligns with evidence-based practices and current research?
Ensuring alignment with evidence-based practices is paramount. We regularly review the latest research in pediatric rehabilitation, attending conferences, participating in professional development activities, and subscribing to relevant journals. Our treatment protocols are continuously updated to incorporate new findings and best practices. We utilize systematic reviews and meta-analyses to guide our decisions on treatment choices. For example, if a new study demonstrates the superior efficacy of a specific therapy for a particular condition, we integrate this into our program after careful evaluation and consideration of its applicability to our patient population. We also maintain a strong relationship with academic institutions and research centers to stay informed about the latest advancements in the field.
Q 6. Describe your experience in budget management for pediatric rehabilitation programs.
Budget management for pediatric rehabilitation programs requires careful planning and resource allocation. I have experience creating detailed budgets that encompass personnel costs, equipment, supplies, and administrative expenses. This involves forecasting needs, negotiating with vendors, and seeking grants or funding opportunities to support program operations. We use data-driven decision making, analyzing the cost-effectiveness of various interventions and prioritizing those with the highest impact on patient outcomes. Regular budget monitoring is critical to ensure we stay within allocated funds and identify any potential financial challenges early on. For example, at one facility, I successfully secured a grant that allowed us to purchase new, technologically advanced equipment that improved both the quality and efficiency of our services.
Q 7. How do you manage interdisciplinary collaboration within a pediatric rehabilitation team?
Effective interdisciplinary collaboration is crucial in pediatric rehabilitation. I foster a team environment that prioritizes open communication, mutual respect, and shared decision-making. We hold regular team meetings where therapists, physicians, nurses, and other professionals share information, coordinate care, and discuss patient progress. Using a shared electronic health record (EHR) system facilitates efficient information sharing and reduces redundancy. Establishing clear roles and responsibilities, along with a collaborative problem-solving approach, prevents conflicts and ensures a cohesive and efficient treatment plan. I also emphasize the importance of clear communication with families, making sure they understand the roles of each team member and are actively involved in the decision-making process.
For example, in a case of a child with cerebral palsy, our team might include a physical therapist, occupational therapist, speech-language pathologist, and a psychologist. Regular meetings and a well-defined plan ensures everyone’s expertise is utilized for the best possible outcome for the child.
Q 8. Explain your experience in working with families and caregivers of children in rehabilitation.
Working with families and caregivers is the cornerstone of successful pediatric rehabilitation. It’s not just about treating the child; it’s about empowering the entire family to support the child’s progress. My approach involves building strong, trusting relationships based on open communication and shared decision-making. I believe in actively listening to their concerns, understanding their hopes and anxieties, and collaboratively setting realistic goals.
For example, I recently worked with a family whose child had cerebral palsy. We developed a home exercise program tailored to their lifestyle and the parents’ comfort level. Regular check-ins, both in-person and via phone, allowed us to address challenges, provide ongoing support, and adjust the program as needed. We also connected them with relevant support groups, providing valuable peer-to-peer learning and emotional support. This collaborative approach fostered a sense of teamwork, leading to excellent outcomes for both the child and family.
Q 9. How do you adapt programs to meet the diverse needs of children with varying disabilities?
Children with disabilities exhibit a wide range of needs, and a ‘one-size-fits-all’ approach simply doesn’t work. My strategy focuses on individualized program development. This begins with a thorough assessment that considers the child’s specific diagnosis, functional limitations, developmental stage, and unique strengths. We then utilize a multidisciplinary team approach—physical therapists, occupational therapists, speech therapists, etc.—to create a customized plan addressing the child’s holistic needs.
For instance, a child with autism may benefit from structured routines and visual supports within their therapy sessions, whereas a child with Down syndrome might require adaptive equipment and strategies focused on gross motor skills. Regular monitoring and adjustments ensure the program continues to meet the evolving needs of the child as they progress.
Q 10. What strategies do you use to engage children in their rehabilitation programs?
Engaging children in their rehabilitation is crucial for successful outcomes. It’s about transforming therapy from a chore into a fun and rewarding experience. I employ several strategies, including play-based therapy, incorporating the child’s interests, and using positive reinforcement. We might use video games to improve fine motor skills, incorporate music into physical therapy, or create a ‘treasure hunt’ to encourage participation in exercises.
For children with limited communication abilities, I utilize assistive technology and alternative communication methods to foster participation and understanding. Regular feedback from the child is invaluable in adapting our approach and ensuring the program remains engaging and motivating.
Q 11. How do you address challenges in program implementation, such as staffing shortages or resource limitations?
Challenges such as staffing shortages and limited resources are realities in many healthcare settings. To address these, I prioritize efficient resource allocation and creative problem-solving. This may involve collaborating with community organizations, leveraging telehealth technologies to expand access to care, and implementing standardized protocols to streamline processes. For example, if we face a shortage of therapists, we might explore collaborative care models, where therapists from different disciplines work together to maximize efficiency. Similarly, we can develop cost-effective program options that utilize readily available resources in the community.
Q 12. Describe your experience in evaluating the effectiveness of pediatric rehabilitation interventions.
Evaluating the effectiveness of interventions is essential to ensure we’re providing the best possible care. My experience includes utilizing both quantitative and qualitative data to assess program outcomes. Quantitative data might include standardized assessments measuring motor skills, language development, or cognitive abilities. These provide objective measures of progress.
Qualitative data, gathered through interviews with families and observations during therapy sessions, provides valuable insight into the child’s experience and overall well-being. This rich data helps us understand the impact of our interventions beyond just numerical scores. Comparing pre- and post-intervention data allows us to determine the effectiveness of our strategies and make necessary modifications.
Q 13. What data collection methods do you use to monitor program outcomes?
We employ a variety of data collection methods to monitor program outcomes. This includes standardized assessments, such as the Gross Motor Function Measure (GMFM) or the Bayley Scales of Infant and Toddler Development, to track functional abilities. We also use observation checklists to document behavioral changes, and parent/caregiver questionnaires to gather feedback on the child’s progress and satisfaction with the program. Data is meticulously documented, analyzed, and used to inform program modifications and future planning.
Q 14. How do you ensure the program complies with relevant regulations and accreditation standards?
Compliance with regulations and accreditation standards is paramount. We maintain up-to-date knowledge of all relevant laws and guidelines, including HIPAA regulations for patient privacy, and state licensing requirements. Our program adheres to standards set by organizations like the Joint Commission, ensuring the delivery of high-quality, safe, and ethical care. Regular internal audits and staff training ensure compliance and continuous improvement. We also engage in ongoing professional development to remain informed about best practices and evolving standards in pediatric rehabilitation.
Q 15. How do you utilize technology to enhance pediatric rehabilitation program delivery?
Technology plays a crucial role in enhancing the effectiveness and accessibility of pediatric rehabilitation programs. We utilize various tools to improve patient outcomes and streamline operations.
Telehealth: We leverage telehealth platforms for remote therapy sessions, allowing us to reach children in remote areas or those with mobility limitations. This involves video conferencing, remote monitoring of exercises using wearable sensors, and providing educational resources online. For example, we’ve successfully implemented a virtual reality (VR) program for children with cerebral palsy, using VR games to improve motor skills and engagement.
Assistive Technology: We incorporate various assistive technologies like adaptive toys, communication devices (AAC), and specialized equipment into therapy sessions, tailoring them to each child’s unique needs. A recent success involved using a customized robotic arm to help a child with limited upper limb function regain independence in daily tasks.
Data Analytics: We use data analytics to track patient progress, identify areas needing improvement, and personalize treatment plans. This includes monitoring therapy session attendance, exercise completion rates, and functional outcomes. This data allows for a more objective and responsive treatment approach.
Gamification and Interactive Apps: Incorporating game-like elements and engaging apps into therapy makes the process more fun and motivating for children. Many apps track progress and provide immediate feedback, which helps keep children engaged and encourages active participation.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience in marketing and promoting pediatric rehabilitation programs.
Marketing and promoting pediatric rehabilitation programs require a multifaceted approach that focuses on building trust and showcasing the positive impact we have on children’s lives.
Community Outreach: We actively engage with local schools, hospitals, and community organizations to raise awareness about our programs and services. We participate in health fairs, host workshops, and offer educational materials to parents and caregivers.
Digital Marketing: We utilize a robust online presence through a user-friendly website, social media engagement, and targeted online advertising. We share success stories and testimonials to build credibility and connect with families.
Partnerships: We collaborate with other healthcare providers, insurance companies, and advocacy groups to expand our reach and ensure our programs are easily accessible. For example, we recently formed a strong partnership with a local children’s hospital, referring patients and sharing resources effectively.
Public Relations: We actively seek media coverage through press releases, interviews, and participation in local news segments, highlighting our achievements and the positive impact on children. This approach builds public awareness and showcases the excellence of our programs.
Q 17. How do you identify and address ethical dilemmas in pediatric rehabilitation?
Ethical dilemmas in pediatric rehabilitation are complex and require careful consideration. Our approach involves a multi-pronged strategy focusing on transparency, collaboration, and adherence to ethical guidelines.
Informed Consent: We ensure parents and guardians fully understand the treatment plan, potential risks and benefits, and have the opportunity to ask questions before consenting to any intervention. This includes explaining the use of data collected during therapy.
Confidentiality: Protecting the privacy of children and their families is paramount. We adhere to strict confidentiality protocols and ensure all data is securely stored and accessed only by authorized personnel.
Conflict of Interest: We proactively address any potential conflicts of interest, ensuring transparency and objectivity in decision-making. For example, if a therapist has a personal connection with a patient’s family, we would ensure this is declared and appropriate steps are taken to prevent any bias.
Collaboration and Consultation: When facing complex ethical dilemmas, we consult with our ethics committee, legal counsel, and other relevant professionals to ensure we make the most ethical and responsible decisions in the best interest of the child.
Q 18. How do you ensure the safety of children participating in rehabilitation programs?
Ensuring the safety of children is the highest priority in our rehabilitation programs. We implement comprehensive safety measures at every level.
Risk Assessment: Thorough risk assessments are conducted for each child upon enrollment, identifying potential hazards based on their individual needs and medical history. This guides the development of individualized safety plans.
Environment Safety: Our facilities are designed with safety in mind, featuring child-proofed areas, age-appropriate equipment, and clear emergency procedures. Regular safety inspections are conducted to ensure the environment remains safe and hazard-free.
Staff Training: All our staff receive comprehensive training in child safety protocols, including CPR, first aid, and emergency response procedures. They are also trained in recognizing and responding to signs of child abuse or neglect.
Equipment Safety: We regularly inspect and maintain all equipment to ensure it is functioning correctly and meets safety standards. We use only approved and age-appropriate equipment for therapy sessions.
Supervision: Children are always under appropriate supervision during therapy sessions and activities. The level of supervision is adjusted based on the child’s age, abilities, and the specific activity being undertaken.
Q 19. What is your experience with different pediatric rehabilitation treatment modalities?
My experience encompasses a wide range of pediatric rehabilitation treatment modalities. I’m proficient in applying evidence-based practices tailored to individual needs.
Physical Therapy: I have extensive experience in designing and implementing physical therapy programs focusing on gross motor skills, mobility, strength, and balance. This includes techniques like neurodevelopmental treatment (NDT) and constraint-induced movement therapy (CIMT).
Occupational Therapy: I’m skilled in occupational therapy interventions focusing on fine motor skills, adaptive techniques, daily living skills, and sensory integration. This involves using various tools and techniques to improve hand-eye coordination, self-care, and participation in everyday activities.
Speech-Language Therapy: I collaborate closely with speech-language pathologists to address communication, articulation, and feeding difficulties. This includes the use of AAC devices and strategies for improving speech production.
Developmental Therapy: My expertise includes working with children with developmental delays across various domains, using play-based therapy and other child-centered approaches to promote overall development.
I frequently integrate these modalities for a holistic approach, ensuring comprehensive and effective treatment.
Q 20. How do you develop and implement a plan for program growth and expansion?
Developing a plan for program growth and expansion involves a strategic, data-driven approach. It requires careful planning and consideration of several factors.
Needs Assessment: We conduct regular needs assessments to identify unmet needs in the community and potential areas for expansion. This could involve surveying families, collaborating with local organizations, and reviewing relevant demographic data.
Market Analysis: We conduct market research to understand the competitive landscape, identify potential target markets, and assess the demand for specific services. This helps us tailor our programs to meet the needs of the community.
Financial Planning: We develop detailed financial projections to secure funding for expansion, including exploring grant opportunities, fundraising initiatives, and partnerships.
Staffing and Resources: We ensure we have the necessary staffing and resources to support program expansion. This involves recruiting qualified professionals, securing appropriate space, and acquiring necessary equipment.
Program Development: We develop new programs or expand existing ones based on the needs assessment and market analysis. This could involve creating specialized programs for specific populations or expanding services to new geographical locations.
Evaluation and Monitoring: We regularly evaluate the effectiveness of our programs and monitor key performance indicators (KPIs) to ensure our expansion efforts are successful and meet our goals. Regular feedback from families and staff are integral to this process.
Q 21. Describe a time you had to make a difficult decision regarding resource allocation in a pediatric rehab program.
One challenging decision involved resource allocation between two competing needs: expanding our early intervention program for toddlers with autism and upgrading our therapy equipment. Both were crucial, but budget constraints forced a difficult choice.
We used a structured decision-making process that included:
Data Analysis: We analyzed data on waitlists for both services, the potential impact of each decision on patient outcomes, and the long-term costs and benefits.
Stakeholder Input: We gathered input from therapists, parents, and administrators to understand their perspectives and prioritize needs.
Cost-Benefit Analysis: We conducted a cost-benefit analysis for each option, comparing the potential return on investment (ROI) for each.
Ultimately, we decided to prioritize expanding our early intervention program due to the potential for long-term positive impact on young children. We secured additional funding for equipment upgrades through grants and fundraising initiatives. While this was a difficult decision, the process ensured transparency and fairness, balancing immediate needs with long-term strategic goals. The positive outcomes from the expansion of the early intervention program justified the decision.
Q 22. How do you incorporate feedback from families and staff to improve the program?
Incorporating feedback from families and staff is crucial for a thriving pediatric rehabilitation program. It’s not just about collecting opinions; it’s about actively listening, understanding perspectives, and using that information to make meaningful changes. We employ a multi-pronged approach:
Regular Family Surveys and Interviews: We use both structured surveys and informal interviews to gather feedback on various aspects of the program, including therapy effectiveness, communication, and overall satisfaction. For example, after a therapy session, we might ask parents to complete a brief questionnaire about their child’s engagement and progress, allowing for immediate feedback.
Staff Meetings and Suggestion Boxes: Regular team meetings provide a platform for therapists, nurses, and other staff to share their experiences and suggestions. We also use anonymous suggestion boxes to encourage open and honest feedback, ensuring that even less vocal team members feel heard.
Focus Groups: Periodically, we conduct focus groups with families and staff to discuss specific program areas needing improvement. This facilitates deeper discussions and allows for collaborative problem-solving. For instance, we held a focus group that helped us redesign our waiting area to be more child-friendly and comfortable.
Data-Driven Feedback: We analyze program data (e.g., patient outcomes, therapist performance) to identify areas for improvement and incorporate these insights into our feedback mechanisms. We might find a particular therapy technique consistently producing better results, which would then inform training for staff.
This continuous feedback loop ensures that our program remains relevant, responsive, and truly beneficial for the children and families we serve.
Q 23. What is your experience with developing and implementing discharge planning protocols?
Discharge planning is a critical component of pediatric rehabilitation, ensuring a smooth transition back to the child’s home and community. My experience involves developing and implementing protocols that are comprehensive, individualized, and family-centered.
Early and Collaborative Planning: We begin the discharge planning process early in the child’s rehabilitation journey, working closely with the family to understand their goals and resources. This collaborative approach ensures that the plan aligns with the family’s needs and capabilities.
Comprehensive Assessment: A thorough assessment of the child’s functional abilities, medical needs, and family support systems is crucial. This includes identifying potential challenges the family might face post-discharge and developing strategies to address them. We utilize standardized assessment tools to track progress and inform discharge decisions.
Goal Setting and Intervention Planning: Discharge planning includes specific, measurable, achievable, relevant, and time-bound (SMART) goals for the child’s continued progress. We create a detailed plan outlining the interventions needed to support these goals in the home environment.
Resource Identification and Referral: We identify and connect families with appropriate community resources such as home health care, specialized equipment providers, educational services, and support groups.
Follow-up and Support: Post-discharge follow-up is essential to monitor the child’s progress and provide ongoing support to the family. We conduct regular phone calls, home visits, or clinic appointments as needed.
For example, we recently worked with a family to transition their child home after extensive physical therapy. We coordinated home health visits, arranged for adaptive equipment delivery, and connected the parents with a local support group for parents of children with similar disabilities. The successful transition was a direct result of our well-structured and collaborative discharge planning process.
Q 24. How do you ensure program accessibility for children with diverse cultural backgrounds and needs?
Ensuring accessibility for children from diverse cultural backgrounds and needs requires a multifaceted approach. We strive for inclusivity by:
Culturally Competent Care: We train our staff on cultural sensitivity and awareness, emphasizing the importance of understanding and respecting diverse family values and communication styles. This includes training on recognizing and addressing potential cultural barriers to care.
Language Access: We provide interpretation and translation services to ensure effective communication with families who speak languages other than English. We work with professional interpreters and utilize translation technology where appropriate.
Adaptive Programs: Our programs are designed to be flexible and adaptive to meet the unique needs of individual children, regardless of their cultural background. We recognize that traditional therapeutic approaches may not always be culturally appropriate, so we tailor our interventions accordingly.
Community Partnerships: We build partnerships with community organizations and leaders from diverse cultural backgrounds to help us understand community needs and tailor our programs effectively.
Inclusive Materials: We use culturally appropriate and inclusive educational materials and resources. This includes using diverse imagery in our therapy materials and ensuring that our communication reflects the diversity of our patient population.
For instance, we developed a culturally sensitive program for refugee children who had experienced trauma, collaborating with local community leaders to create a comfortable and supportive environment.
Q 25. Describe your experience in fostering a positive and supportive therapeutic environment.
Creating a positive and supportive therapeutic environment is paramount. It involves building a sense of trust, safety, and collaboration among children, families, and staff. Key elements include:
Play-Based Therapy: We utilize play-based therapy techniques to make rehabilitation fun and engaging for children. This helps to reduce anxiety and encourage active participation.
Family-Centered Care: Families are active participants in the therapy process. We involve them in goal setting, treatment planning, and progress monitoring, empowering them to play a crucial role in their child’s recovery.
Positive Reinforcement: We focus on positive reinforcement and celebrate successes, no matter how small. This helps to build children’s confidence and motivation.
Comfortable and Child-Friendly Space: Our therapy spaces are designed to be inviting, safe, and stimulating. We use bright colors, toys, and other elements that appeal to children.
Staff Training: Our staff receives training on child development, communication techniques, and trauma-informed care. This ensures that they can effectively create a supportive and nurturing environment.
I remember one child who initially resisted therapy. By creating a playful environment using his favorite toys and incorporating his interests into the sessions, we transformed his attitude from resistance to enthusiastic participation.
Q 26. How do you ensure the ongoing professional development of the pediatric rehabilitation team?
Ensuring ongoing professional development is essential for maintaining a high standard of care. We implement a comprehensive program that includes:
Continuing Education Opportunities: We provide staff with access to conferences, workshops, and online courses relevant to pediatric rehabilitation. We encourage attendance at relevant conferences and provide financial assistance where needed.
Mentorship Programs: We establish mentorship programs where experienced therapists guide and support newer team members, promoting knowledge transfer and skill development.
Internal Training Sessions: We hold regular internal training sessions to update staff on the latest research, evidence-based practices, and best practices in pediatric rehabilitation. We often have guest speakers from related fields.
Clinical Supervision: Regular clinical supervision provides opportunities for therapists to review their cases, receive feedback, and discuss challenging situations.
Certification and Credentialing: We encourage and support staff in pursuing certifications and credentials relevant to their areas of expertise. We recognize the importance of professional recognition.
For example, we recently implemented a new evidence-based intervention for a specific condition and provided comprehensive training for our entire team to ensure consistent application of this new technique. We also have a regular internal journal club where we discuss latest research and clinical findings.
Q 27. Describe your experience in managing a budget and securing funding for pediatric rehabilitation programs.
Managing a budget and securing funding for pediatric rehabilitation programs requires a strategic approach. My experience involves:
Budget Development and Monitoring: I develop detailed budgets that align with program goals and operational needs. I closely monitor expenses and ensure that resources are allocated efficiently.
Grant Writing and Fundraising: I have extensive experience in writing grant proposals and seeking funding from various sources, including government agencies, foundations, and private donors. I develop compelling narratives and clearly articulate the program’s impact.
Cost-Effectiveness Analysis: I conduct cost-effectiveness analyses to demonstrate the value of our programs and justify the need for continued funding. I highlight the long-term cost savings associated with early intervention.
Collaboration with Stakeholders: I work closely with hospitals, health systems, and government agencies to identify funding opportunities and build collaborative partnerships. These partnerships are crucial to secure funding and sustainability.
Outcome Measurement: I use data to demonstrate program outcomes and success, which strengthens funding applications and builds confidence in our work. I track key performance indicators and demonstrate return on investment.
For instance, I successfully secured a three-year grant to expand our program’s reach to underserved communities. This grant was based on a strong proposal that highlighted our program’s effectiveness and its potential to improve the lives of many children.
Q 28. How do you use data analysis to inform program improvements and decision-making?
Data analysis is essential for continuous quality improvement and informed decision-making. We utilize data to:
Track Program Outcomes: We collect and analyze data on patient outcomes, including functional improvements, developmental milestones, and quality of life measures. This helps us to measure the effectiveness of our interventions.
Evaluate Treatment Effectiveness: We use data to compare the effectiveness of different treatment approaches. This allows us to identify best practices and refine our therapeutic strategies.
Monitor Patient Satisfaction: We track patient and family satisfaction through surveys and feedback mechanisms. This helps us identify areas for improvement in service delivery.
Identify Trends and Patterns: We analyze data to identify trends and patterns in patient demographics, diagnoses, and outcomes. This informs program planning and resource allocation.
Benchmark Performance: We compare our program’s performance to other similar programs to identify areas for improvement and best practices.
Inform Program Development: Data analysis guides our program development and expansion efforts. We use data to make decisions about resource allocation, staffing, and program design.
For example, through data analysis, we discovered that a particular type of therapy was less effective for a specific age group. This finding allowed us to adjust our approach and improve the overall effectiveness of our program. We use statistical software and data visualization tools to effectively analyze data and present insights clearly.
Key Topics to Learn for Pediatric Rehabilitation Program Development Interview
- Needs Assessment & Program Design: Understanding the unique needs of pediatric populations and designing programs to address developmental delays and disabilities. This includes considering age appropriateness, developmental stages, and family involvement.
- Evidence-Based Practices: Applying research-based interventions and therapeutic approaches within the program. This requires familiarity with current literature and the ability to justify treatment choices.
- Team Collaboration & Communication: Effectively collaborating with therapists, physicians, educators, and families to ensure coordinated and comprehensive care. Demonstrate understanding of interprofessional communication strategies.
- Program Evaluation & Outcomes Measurement: Developing and implementing methods to track progress, measure effectiveness, and demonstrate program impact. Familiarize yourself with various outcome measures and data analysis techniques.
- Budgeting & Resource Management: Understanding the financial aspects of program development, including budget planning, resource allocation, and grant writing.
- Regulatory Compliance & Ethical Considerations: Navigating relevant regulations, ensuring program adherence to ethical guidelines, and maintaining patient confidentiality.
- Program Sustainability & Growth: Planning for long-term program viability, exploring opportunities for expansion, and adapting to changing needs and resources.
- Technology Integration in Pediatric Rehabilitation: Exploring the use of assistive technology, telehealth, and other technological advancements to enhance program effectiveness and accessibility.
Next Steps
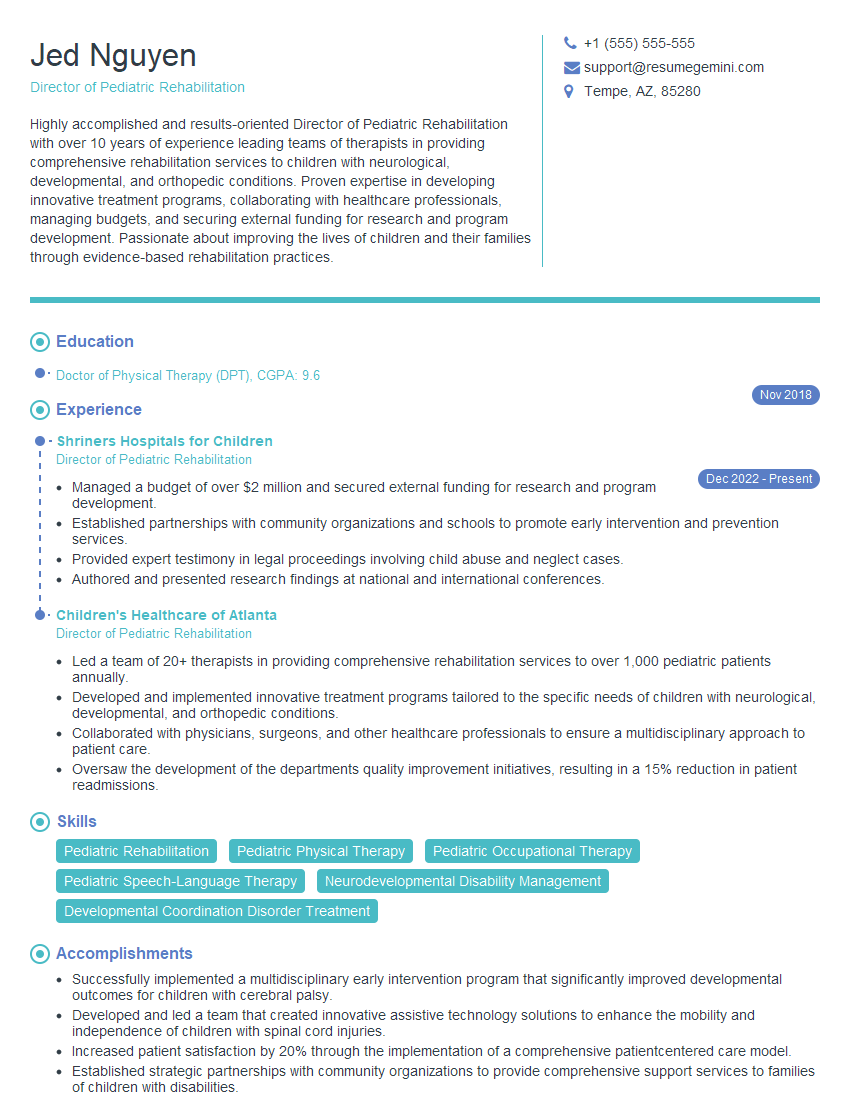
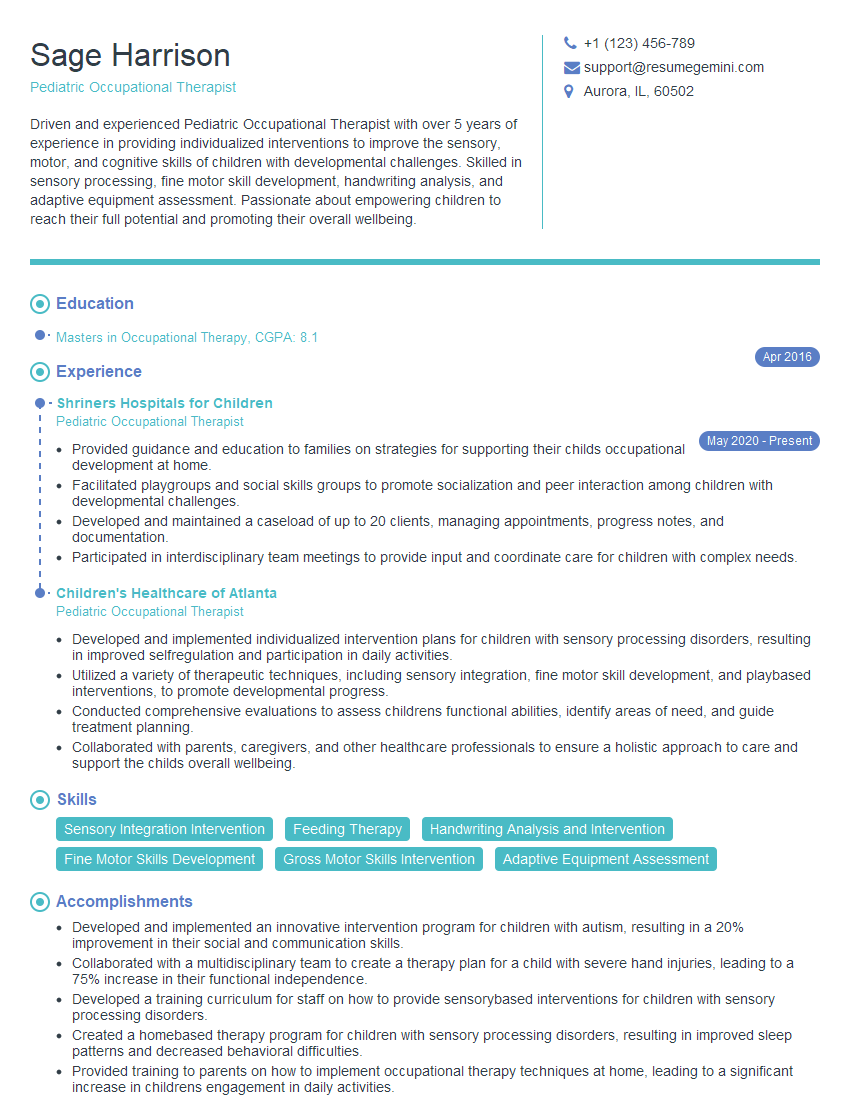
Mastering Pediatric Rehabilitation Program Development is crucial for career advancement in this rewarding field. It demonstrates your expertise in creating impactful and evidence-based programs that improve the lives of children. To maximize your job prospects, focus on building a strong, ATS-friendly resume that highlights your skills and experience. ResumeGemini is a trusted resource that can help you craft a professional and effective resume tailored to the specific demands of this competitive field. Examples of resumes tailored to Pediatric Rehabilitation Program Development are available to guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.