Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Regulatory Compliance (CLIA, CAP) interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Regulatory Compliance (CLIA, CAP) Interview
Q 1. Explain the key differences between CLIA and CAP accreditation.
CLIA (Clinical Laboratory Improvement Amendments) and CAP (College of American Pathologists) accreditation are both crucial for clinical laboratories in the US, ensuring quality and accuracy of test results. However, they differ significantly in their scope and approach. CLIA is a federal regulatory program mandating minimum standards for all laboratory testing performed on humans in the US. It’s a legal requirement. CAP, on the other hand, is a voluntary accreditation program offered by a professional organization. It’s a more comprehensive and rigorous process focusing on quality and performance beyond the basic CLIA requirements.
- CLIA: Focuses on compliance with minimum regulatory standards, offering different levels of complexity based on the tests performed. Think of it as the ‘baseline’ you must meet.
- CAP: Emphasizes continuous quality improvement, offering a more detailed assessment covering a wider range of quality aspects. Think of it as ‘going above and beyond’ the minimum standards to achieve higher quality and recognition within the field.
In essence, you must have CLIA certification, but CAP accreditation is a prestigious mark of excellence many labs strive for.
Q 2. Describe the process for obtaining CLIA certification.
Obtaining CLIA certification involves several steps. First, you must determine the complexity of your tests (waived, moderate, or high complexity). This dictates the level of regulatory requirements. Next, you’ll complete an application, providing information about your laboratory, personnel, and testing procedures. This is submitted to your state’s licensing authority. They will conduct an onsite inspection to assess your compliance with regulations. This inspection will cover facilities, equipment, procedures, personnel qualifications, and quality control measures. Following a successful inspection, your lab receives certification, which must be renewed periodically.
Think of it like getting a business license, but far more rigorous and focused on the accuracy and safety of your testing processes. The whole process can take several months from application to final certification.
Q 3. What are the major components of a CLIA-compliant quality system?
A CLIA-compliant quality system is the backbone of a successful clinical laboratory. It ensures accurate and reliable test results. Key components include:
- Quality Control (QC): Regularly testing controls (known samples with known values) to ensure the accuracy and precision of test results. Think of this as regular calibration of your lab’s testing procedures.
- Quality Assurance (QA): A broader system encompassing all aspects of laboratory operation to ensure the accuracy, reliability, and timeliness of test results. This is the overall strategy to maintain high quality.
- Proficiency Testing (PT): Participating in external quality assessment programs to compare results with other labs, identifying any inconsistencies. It’s like a benchmark test to see how your lab compares to others.
- Personnel Qualifications: Ensuring all personnel are appropriately trained and qualified for their roles. This is crucial for accurate and efficient testing procedures.
- Record Keeping: Maintaining detailed and accurate records of all testing procedures, results, and quality control data. This allows for auditing and identification of areas for improvement.
- Corrective Actions: Implementing effective processes to address identified deficiencies. This involves identifying the root cause of problems and developing solutions to prevent recurrence.
Failure to maintain a strong quality system can lead to inaccurate results, potential harm to patients, and loss of certification.
Q 4. How does CAP accreditation differ from CLIA certification?
While both CLIA and CAP aim to ensure high-quality laboratory testing, their approaches differ. CLIA is a mandatory government regulation focused on meeting minimum standards for safety and accuracy. CAP accreditation is a voluntary process that goes beyond the minimum requirements, providing a more comprehensive evaluation of the laboratory’s operations and quality management system.
- CLIA: Minimum requirements, government-mandated, focused on compliance. Think of it as passing the bar exam – it’s the minimum needed to practice.
- CAP: Higher standards, voluntary accreditation, focuses on continuous improvement. Think of it as completing a prestigious fellowship beyond the bar exam – it shows advanced expertise.
Many labs pursue CAP accreditation even after satisfying CLIA requirements to demonstrate a commitment to quality beyond the baseline. CAP accreditation signifies a higher level of competency and excellence within the clinical laboratory field.
Q 5. Explain the significance of proficiency testing in a CLIA/CAP certified lab.
Proficiency testing (PT) is a critical component of a CLIA/CAP-certified lab’s quality system. It involves participation in external quality assessment programs where labs receive unknown samples and compare their results to those of other participating labs. This process helps identify potential problems with testing procedures, equipment, or personnel. Think of it like a ‘blind taste test’ for labs, allowing for unbiased comparison and revealing any systematic errors or biases.
The significance of PT includes early detection of systematic errors, identification of areas needing improvement, and demonstration of consistent performance. Failing PT can lead to corrective action plans, even potential sanctions from regulatory bodies, highlighting its critical role in maintaining quality and patient safety.
Q 6. What are the requirements for personnel qualifications under CLIA?
CLIA has specific requirements for personnel qualifications based on the complexity of tests performed. Personnel must meet education, experience, and training criteria relevant to their roles. For example, high-complexity testing typically requires personnel with advanced degrees or extensive experience under the supervision of qualified personnel. This ensures that individuals performing tests have the necessary knowledge and skills to produce accurate and reliable results. The regulatory requirements are detailed and specific, and failure to meet them can result in sanctions.
Think of it as a licensing process for specific lab professionals. Each role within the lab has its own specific qualifications depending on the complexity of the tests they perform.
Q 7. Describe your experience with internal audits and corrective actions in a CLIA/CAP setting.
In my previous roles, I’ve been actively involved in conducting internal audits and implementing corrective actions in CLIA/CAP compliant labs. Internal audits involve a systematic review of the laboratory’s operations, procedures, and records, ensuring compliance with regulatory requirements and internal quality standards. This involves examining everything from equipment maintenance logs to staff training records, and proficiency testing results. Any non-compliance issues are documented, and corrective action plans (CAPs) are developed to address the root cause of deficiencies.
For instance, during an internal audit, we discovered a discrepancy in temperature control for a reagent. The corrective action involved not only rectifying the immediate issue but also reviewing all temperature-sensitive reagents and implementing a more robust monitoring and alert system to prevent future occurrences. This demonstrates a proactive approach to quality management and risk mitigation, central to maintaining CLIA/CAP compliance.
Q 8. How do you ensure compliance with CLIA regulations regarding quality control?
Ensuring CLIA compliance regarding quality control is paramount for maintaining the accuracy and reliability of laboratory test results. This involves a multi-faceted approach that includes meticulous adherence to established protocols, rigorous monitoring, and proactive corrective actions.
- Internal Quality Control (IQC): We implement a robust IQC program using commercially available controls run with each analytical run. These controls assess the precision and accuracy of the analytical methods. Any values falling outside the predetermined acceptable ranges trigger investigation and corrective actions, such as instrument recalibration or reagent replacement. For example, if our glucose IQC consistently shows high bias, we’d investigate factors like instrument malfunction, reagent degradation, or even technician error.
- External Quality Assessment (EQA): Participation in EQA programs, like those offered by CAP or other accredited providers, is crucial. These proficiency testing programs provide an external evaluation of our laboratory’s performance, comparing our results to those of other laboratories. Discrepancies need thorough investigation and documentation.
- Quality Control Records: Maintaining meticulous records of all IQC and EQA results is non-negotiable. This includes documentation of any discrepancies, corrective actions taken, and the effectiveness of those actions. These records are subject to internal and external audits.
- Preventive Maintenance: Regular preventive maintenance of all laboratory instruments is scheduled and documented to ensure optimal performance and minimize the risk of errors. We adhere to manufacturer’s recommendations and maintain a detailed log of maintenance activities.
Ultimately, a strong quality control program is a proactive approach to prevent errors and ensure the reliability of our results, protecting both the laboratory and patient care.
Q 9. What is your experience with handling CLIA deficiencies and non-compliance issues?
Handling CLIA deficiencies and non-compliance is a critical aspect of laboratory management. My experience involves a systematic approach focused on immediate corrective action and prevention of recurrence.
- Immediate Corrective Action: Upon identification of a deficiency, whether through internal audit, external inspection, or incident report, we immediately implement corrective actions to address the root cause. This might involve retraining staff, revising procedures, replacing equipment, or improving record-keeping practices.
- Root Cause Analysis: We perform thorough root cause analyses to understand why the deficiency occurred. This often involves interviewing staff, reviewing records, and examining workflows. The goal is to identify systemic issues, not just treat symptoms.
- Corrective Action Plan (CAP): We develop a detailed CAP outlining the steps taken to correct the deficiency, prevent recurrence, and demonstrate improvement. This plan is documented thoroughly and submitted to the relevant regulatory bodies as required.
- Monitoring and Follow-up: Following implementation of the CAP, we continuously monitor for effectiveness. This may include additional audits, process checks, and performance monitoring to ensure the corrective actions have resolved the issue and prevent future occurrences. This proactive approach demonstrates continuous improvement and commitment to compliance.
For example, if a deficiency was identified regarding inadequate temperature monitoring of reagents, our response would involve not just fixing the immediate temperature issue but also reviewing our procedures, retraining staff on proper temperature monitoring techniques, implementing alarm systems, and potentially procuring a more robust temperature monitoring system.
Q 10. Explain the role of a laboratory director in maintaining CLIA and CAP compliance.
The laboratory director plays a crucial role in maintaining CLIA and CAP compliance. They are ultimately responsible for ensuring the laboratory operates according to regulatory guidelines and provides accurate and reliable testing services.
- Oversight of Compliance Programs: The laboratory director oversees all aspects of compliance, including quality control, quality assurance, personnel qualifications, and proficiency testing.
- Policy and Procedure Development: They are responsible for developing and implementing laboratory policies and procedures that adhere to CLIA and CAP regulations. These procedures must be clear, concise, and easily accessible to all staff.
- Personnel Management: The director ensures that all personnel are appropriately trained, qualified, and competent to perform their duties. This involves overseeing training programs and competency assessments.
- Regulatory Audits and Inspections: They are responsible for preparing for and responding to regulatory audits and inspections. This involves maintaining comprehensive documentation and proactively addressing any deficiencies.
- Communication and Training: The laboratory director fosters a culture of compliance within the laboratory through clear communication, regular training, and open dialogue about regulatory requirements.
Essentially, the laboratory director acts as the guarantor of compliance, ensuring the laboratory meets the highest standards of quality and regulatory adherence. They are responsible for fostering a culture where compliance is not just a checklist, but an integral part of the laboratory’s operational philosophy.
Q 11. How do you ensure the accuracy and reliability of test results under CLIA guidelines?
Ensuring the accuracy and reliability of test results under CLIA guidelines requires a multifaceted strategy. Accuracy and reliability are not just about individual tests but the entire testing process.
- Calibration and Maintenance: Regular calibration and preventive maintenance of all analytical instruments are essential. We follow manufacturer recommendations and meticulously document all activities. This is critical for ensuring consistent and accurate measurements. For example, if a spectrophotometer is out of calibration, the absorbance readings will be inaccurate, leading to unreliable test results.
- Quality Control Procedures: As mentioned earlier, a robust quality control program, including IQC and EQA, is the cornerstone of accurate and reliable results. We consistently monitor the performance of our assays and address any deviations promptly.
- Staff Competency: Ensuring the competency of laboratory personnel is crucial. Our staff undergo rigorous training and competency assessments to ensure proficiency in performing tests and interpreting results. Regular continuing education programs are utilized to maintain and update their skills.
- Standard Operating Procedures (SOPs): Clearly defined and consistently followed SOPs for all tests and procedures are essential. This minimizes variability and ensures that each test is performed according to established protocols. We regularly review and update our SOPs to reflect current best practices and any changes in methodology or technology.
- Proficiency Testing: Participation in proficiency testing programs allows for external validation of our laboratory’s performance. Results are carefully evaluated, and any issues identified are investigated thoroughly.
This comprehensive approach ensures that our results are not only accurate but also reliable, allowing healthcare providers to make informed decisions based on the data we provide.
Q 12. What is your understanding of the CLIA ‘waived’ testing category?
CLIA ‘waived’ testing refers to a category of laboratory tests that are deemed simple enough to be performed with minimal risk of error. These tests are considered so simple and accurate that the FDA has determined they don’t require the same level of regulatory oversight as other tests.
Examples include:
- Dipstick urinalysis
- Some blood glucose meters (using specific FDA-cleared devices)
- Ovulation tests
- Pregnancy tests
The key is that these tests are typically self-administered and/or have inherent accuracy due to the simplicity of the methodology. Even with waived tests, laboratories must still adhere to basic quality control guidelines, and manufacturers of these tests often provide quality control materials. While less stringent than for non-waived testing, it’s vital to maintain accurate records and ensure the integrity of the process, as incorrect results can still have patient health implications. For example, false negative pregnancy tests or falsely elevated blood glucose readings could have significant ramifications.
Q 13. Describe your experience with document control and record keeping in a regulated laboratory.
Document control and record-keeping are vital in a regulated laboratory environment. Maintaining accurate and accessible records is crucial for demonstrating compliance with CLIA and other regulations, tracing results, and performing audits.
- Document Control System: We utilize a robust document control system to manage all laboratory documents, including SOPs, quality manuals, test methods, and training materials. This system ensures that all documents are current, reviewed regularly, and readily available to all relevant personnel. Version control is extremely important.
- Electronic Record-Keeping: We primarily use electronic record-keeping systems to maintain laboratory data. These systems provide secure storage, efficient retrieval, and audit trails. We use electronic systems that are compliant with 21 CFR Part 11 regulations for electronic records and signatures.
- Data Integrity: Maintaining the integrity of our data is a paramount concern. We implement measures to prevent unauthorized access, modification, or deletion of records. This includes security protocols, access controls, and regular data backups.
- Record Retention Policies: We follow specific record retention policies that comply with both CLIA and CAP guidelines. Records are retained for the required timeframes, and appropriate disposal methods are used when records are no longer needed.
- Regular Audits: We conduct regular internal audits to ensure that our documentation practices comply with regulations and that our records are accurate and complete. This helps to identify areas for improvement and prevent potential compliance issues.
In essence, our document control and record-keeping system are the foundation upon which compliance rests. A well-organized and easily accessible system is essential for efficient laboratory operations and successful audits.
Q 14. Explain your familiarity with CAP inspection procedures and requirements.
My familiarity with CAP inspection procedures and requirements is extensive. CAP accreditation is a rigorous process demonstrating commitment to quality and compliance.
- CAP Checklist: I understand the detailed CAP accreditation checklist and its various sections, covering areas such as personnel qualifications, quality control programs, equipment maintenance, and proficiency testing. We prepare diligently for these inspections by ensuring all documentation is up-to-date and readily accessible.
- On-site Inspection: I am experienced in working with CAP inspectors during on-site visits. This includes providing documentation, answering questions, and addressing any queries or concerns raised by the inspectors. Open communication is crucial during these inspections.
- Inspection Preparation: We undertake comprehensive preparation for CAP inspections, including internal audits, staff training, and verification of compliance with all relevant requirements. This proactive approach minimizes any surprises and ensures a smooth inspection process.
- Corrective Action Plans: In the event any deficiencies are identified during the inspection, we promptly develop and implement corrective action plans to address the identified issues. These plans are thoroughly documented and submitted to CAP as required. We focus on not just fixing the problem but improving the underlying process to prevent recurrence.
- Continuous Improvement: We actively use CAP accreditation as a tool for continuous improvement. The inspection process itself helps us identify areas where we can enhance our processes, improve efficiency, and strengthen our commitment to quality.
CAP accreditation is not just about meeting minimum requirements; it’s about striving for excellence and demonstrating a commitment to providing high-quality laboratory services. My experience underscores this commitment, from thorough preparation to proactive improvement.
Q 15. How would you address a discrepancy between test results and expected values?
Discrepancies between test results and expected values are a critical aspect of quality control in any clinical laboratory. My approach involves a systematic investigation to identify the root cause. First, I would verify the pre-analytical phase, checking for correct patient identification, proper sample collection and handling, and appropriate storage conditions. Any deviation from established protocols at this stage could lead to erroneous results.
Next, I’d examine the analytical phase. This includes reviewing the instrument’s calibration records, performing QC checks, and inspecting the test methodology. Was the instrument functioning correctly? Were controls within acceptable ranges? Were there any unusual reagent lot numbers used? Identifying trends in discrepancies, such as consistently high or low values, helps pinpoint systemic issues.
Finally, I’d consider the post-analytical phase. Were the results reported accurately? Were any transcription errors made? If the discrepancy persists after thoroughly investigating all these stages, I’d initiate a full-scale investigation, possibly involving peer review, instrument servicing, or even reagent replacement, depending on the nature of the issue. Proper documentation at every step is essential for tracing the error and preventing future occurrences. For example, if we consistently see lower-than-expected results on a glucose assay, it may indicate a problem with the reagent, necessitating its replacement and recalibration of the instrument.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you ensure the proper maintenance and calibration of laboratory equipment?
Maintaining and calibrating laboratory equipment is paramount to ensure accurate and reliable test results. Our lab adheres to a rigorous preventive maintenance schedule, outlining specific tasks and frequencies for each instrument. These schedules are often manufacturer-recommended and are tailored to the specific needs of each device. For example, we have specific schedules for centrifuges (checking for balance, rotor integrity), autoclaves (temperature and pressure monitoring), and analyzers (daily QC checks and regular preventative maintenance by certified technicians).
Calibration is performed according to manufacturer instructions and using traceable standards. We maintain comprehensive calibration records, documenting the date, time, results, and any corrective actions taken. We use a combination of internal and external quality control checks to validate the accuracy of our equipment. Internal QC utilizes our own prepared controls, while external QC involves participation in proficiency testing programs, which give us an unbiased assessment of our performance compared to other labs. This two-pronged approach helps to identify potential problems with our equipment or techniques early on. Failure to meet quality control standards triggers an immediate investigation and correction, ranging from simple adjustments to complete recalibration or instrument repair.
Q 17. Describe your experience with developing and implementing quality control procedures.
I have extensive experience in developing and implementing quality control (QC) procedures. My approach is based on the principles of the CAP and CLIA guidelines, emphasizing a comprehensive system that covers all aspects of laboratory operations, from pre-analytical to post-analytical phases. This includes establishing written procedures for specimen collection, handling, storage, testing, and reporting. We meticulously document every step, ensuring traceability and accuracy.
For example, I helped develop a new QC procedure for our hematology analyzer. This included establishing acceptable ranges for various controls, defining corrective actions in case of out-of-range results, and implementing a system for trend analysis. We regularly review our QC data to identify potential problems before they escalate. We also use statistical process control (SPC) charts to visually monitor our QC performance and identify any patterns or trends that may indicate issues with our equipment or procedures. The process incorporates regular training for all staff, ensuring everyone understands the importance of following the standardized procedures.
Our QC program also involves participation in proficiency testing programs, providing an external assessment of our lab’s performance and helping us identify areas for improvement. Regular audits are conducted, both internal and by external accreditation bodies, to evaluate the effectiveness of our QC program and ensure compliance with all regulatory requirements. We maintain comprehensive records of all QC activities, and this data is regularly reviewed to make any necessary improvements to our processes.
Q 18. How would you handle a complaint regarding the quality of laboratory services?
Handling complaints regarding the quality of laboratory services is a crucial aspect of maintaining patient trust and regulatory compliance. My approach follows a structured process. First, I would acknowledge the complaint, thank the patient or referring physician for bringing the issue to our attention, and assure them that their concerns are being taken seriously.
Next, I’d gather detailed information about the complaint, documenting all relevant facts and specifics. This could involve reviewing the patient’s records, test results, and any related communications. I would also carefully listen to the patient’s concerns, showing empathy and understanding. Based on the information gathered, I would initiate an investigation to determine the root cause of the problem. This might involve reviewing laboratory procedures, equipment performance data, and personnel actions.
Once the root cause is identified, appropriate corrective actions would be taken. These actions could include retraining staff, improving procedures, replacing equipment, or modifying protocols. The patient or referring physician would be notified of the findings and the corrective actions taken. A follow-up communication would ensure they’re satisfied with the resolution. Finally, I would document the entire complaint process, including the complaint itself, the investigation, the corrective actions taken, and the outcome, to continuously improve our services and prevent similar occurrences in the future.
Q 19. What is your understanding of the regulatory requirements for handling patient samples?
Understanding and adhering to regulatory requirements for handling patient samples is crucial for maintaining the integrity of test results and protecting patient confidentiality. CLIA and CAP regulations mandate strict procedures, emphasizing proper identification, handling, storage, and disposal of samples. Patient identification is paramount; we employ multiple identifiers to prevent mix-ups, and samples are labeled clearly and accurately.
Proper handling involves using appropriate collection devices, avoiding contamination, and maintaining the sample’s integrity. For example, blood samples must be collected in the correct tubes with the appropriate anticoagulants, and specimens should be promptly processed to prevent degradation. Storage conditions are critical; samples are stored at designated temperatures according to their nature and the type of tests ordered, preventing spoilage. We follow strict chain-of-custody procedures, meticulously documenting the handling of every sample from collection to disposal. Finally, regulated disposal procedures, adhering to local and national guidelines, are used to ensure safe and environmentally compliant disposal of hazardous materials.
Our lab’s protocols emphasize the principles of patient safety and confidentiality. All samples are handled confidentially, and strict protocols are followed for data privacy and security. Regular training and competency assessments ensure all staff are aware of and comply with these regulations. Non-compliance can result in serious consequences, such as loss of accreditation, fines, and legal action. Therefore, a strong emphasis on compliance is crucial for the lab’s integrity and the safety of its patients.
Q 20. How do you stay updated on changes in CLIA and CAP regulations?
Staying updated on changes in CLIA and CAP regulations is essential for maintaining compliance and ensuring the quality of laboratory services. My strategy involves a multi-pronged approach. Firstly, I subscribe to professional journals and newsletters published by organizations like the CAP and AACC. These publications often provide updates on regulatory changes, best practices, and emerging technologies.
Secondly, I actively participate in professional development activities such as workshops, conferences, and webinars. These events provide opportunities to learn about the latest regulations and interact with other professionals in the field. Thirdly, I utilize online resources, such as the websites of the CMS (Centers for Medicare & Medicaid Services) and the CAP, to stay informed about regulatory changes and announcements. These websites offer access to the most up-to-date information regarding compliance standards. Finally, I maintain a strong network of colleagues within the clinical laboratory field, exchanging information and best practices with them.
Our laboratory also designates a compliance officer responsible for monitoring regulatory changes and disseminating important information to the staff. Regular meetings are conducted to ensure that everyone is aware of any changes that may affect their work. This proactive approach ensures our laboratory remains up-to-date with all the regulatory requirements and best practices, maintaining a high standard of quality and compliance.
Q 21. Describe your experience with risk assessment and management in a laboratory setting.
Risk assessment and management are integral to maintaining a safe and efficient laboratory environment. We use a systematic approach to identify, analyze, and mitigate potential risks. We start by identifying potential hazards in the laboratory, which includes equipment malfunctions, reagent hazards, biohazards, and ergonomic risks. For each hazard, we conduct a risk assessment, evaluating the likelihood of occurrence and the potential severity of the consequences.
For example, we assessed the risk associated with handling infectious specimens. We implemented strict protocols for personal protective equipment (PPE), including gloves, gowns, and eye protection. We also established procedures for decontamination and disposal of infectious waste. Similarly, we evaluated the risk of equipment malfunction, implementing a preventative maintenance program to minimize equipment failure. We also developed backup plans in case of equipment failure to ensure uninterrupted service.
Once the risks have been assessed, we develop and implement control measures to mitigate those risks. These measures might involve engineering controls (e.g., installing safety cabinets), administrative controls (e.g., developing standard operating procedures), or personal protective equipment (e.g., providing gloves and safety glasses). We regularly review and update our risk assessment and management plan to reflect any changes in our laboratory operations or regulatory requirements. This ensures that our risk management program remains effective and proactive, protecting both our staff and our patients.
Q 22. How do you ensure effective communication of compliance matters to lab personnel?
Effective communication of compliance matters is crucial for a smoothly functioning and compliant laboratory. My approach is multifaceted and relies on a combination of methods tailored to the audience and the complexity of the information.
- Regular Meetings: I conduct regular team meetings, both large and small group sessions, dedicated to discussing updates, clarifications, and potential compliance issues. These meetings provide a platform for open dialogue and address questions proactively. For example, we’d discuss a recent change to CLIA regulations regarding proficiency testing or a new policy on handling patient samples.
- Training Programs: Comprehensive training programs are essential. These programs go beyond simple presentations; they incorporate interactive exercises, case studies, and quizzes to ensure understanding and retention. We use a blended learning approach, combining online modules with hands-on workshops tailored to different job roles. New hires receive extensive training, while existing staff receive regular updates and refresher courses.
- Written Communication: Clear, concise, and easily accessible written materials are a cornerstone. These include updated standard operating procedures (SOPs), compliance manuals, newsletters, and email updates. Using plain language and avoiding jargon is key to ensuring comprehension across all levels of expertise.
- Open-Door Policy: Fostering a culture of open communication is critical. I maintain an open-door policy, encouraging employees to raise compliance concerns without fear of reprisal. Anonymous suggestion boxes or online platforms can also provide alternative avenues for communication.
- Regular Audits and Feedback: I conduct regular compliance audits and provide constructive feedback to individuals and teams. This feedback loop helps identify areas for improvement and reinforce good practices.
This multi-pronged approach ensures that compliance information is not only disseminated but also understood and adopted by all laboratory personnel.
Q 23. Explain your understanding of the regulatory requirements for laboratory safety.
Laboratory safety is paramount and directly impacts both personnel and patient well-being. Regulatory requirements, largely driven by OSHA (Occupational Safety and Health Administration) and often incorporated into CLIA and CAP regulations, focus on several key areas:
- Hazard Communication: Proper labeling, safety data sheets (SDS), and employee training are vital. Employees must understand the hazards associated with chemicals, biological materials, and equipment. This includes proper handling, storage, and disposal procedures.
- Personal Protective Equipment (PPE): Appropriate PPE, such as gloves, lab coats, eye protection, and respirators, must be readily available and used consistently. Training is crucial to ensure proper selection and use of PPE.
- Infection Control: Strict adherence to infection control protocols is essential to prevent the spread of infectious agents. This involves proper hand hygiene, sterilization and disinfection procedures, waste management, and spill response plans.
- Waste Management: Safe disposal of hazardous waste, including chemical, biological, and radioactive materials, must follow all applicable regulations. This involves proper segregation, packaging, and labeling of waste before disposal.
- Emergency Preparedness: Laboratories must have comprehensive emergency preparedness plans addressing fire safety, chemical spills, and other potential hazards. Regular drills and training are vital to ensure preparedness.
- Biosafety: Laboratories working with infectious agents must adhere to biosafety guidelines, including appropriate containment levels (BSL) and safety equipment. This may involve the use of biological safety cabinets (BSCs) and other specialized equipment.
Non-compliance can lead to serious consequences, including fines, sanctions, and even legal action. Therefore, maintaining a culture of safety, through continuous training, regular inspections, and proactive hazard identification and mitigation, is crucial.
Q 24. How do you ensure compliance with data security and privacy regulations?
Ensuring compliance with data security and privacy regulations, such as HIPAA (Health Insurance Portability and Accountability Act) and potentially state-specific regulations, is crucial for protecting patient information. My approach involves several key steps:
- Data Encryption: All electronic protected health information (ePHI) is encrypted both in transit and at rest. This protects data from unauthorized access even if a breach occurs.
- Access Control: Strict access control measures are implemented, ensuring that only authorized personnel can access sensitive data. This involves role-based access control (RBAC) and regular audits of access logs.
- Data Backup and Disaster Recovery: Regular data backups and a robust disaster recovery plan are in place to protect data from loss or damage. This ensures business continuity and prevents data loss in case of emergencies.
- Security Awareness Training: All staff receive regular training on data security best practices, including password management, phishing awareness, and social engineering prevention. This helps prevent human error, a leading cause of data breaches.
- Regular Security Audits and Penetration Testing: We conduct regular security audits and penetration testing to identify vulnerabilities and ensure the effectiveness of our security measures. This proactive approach helps detect and address potential threats before they can be exploited.
- Compliance with HIPAA and other regulations: We diligently follow all requirements of HIPAA, including the Privacy Rule and Security Rule, along with other relevant data privacy regulations. This includes developing and maintaining a comprehensive security awareness program, implementing appropriate safeguards, and responding appropriately to security incidents.
These measures ensure that patient data is protected, regulatory compliance is maintained, and the laboratory’s reputation is preserved. Regular review and updates of these procedures are essential to adapt to evolving threats and regulations.
Q 25. What is your approach to investigating and resolving compliance issues?
My approach to investigating and resolving compliance issues is systematic and thorough. It focuses on identifying the root cause, implementing corrective actions, and preventing recurrence.
- Identify and Report: When a compliance issue is identified (whether through audit, self-reporting, or employee notification), it is immediately documented and reported to appropriate personnel. This includes documenting the nature of the issue, the date of discovery, and any potential impact.
- Investigate: A thorough investigation is conducted to determine the root cause of the issue. This often involves interviewing staff, reviewing records, and analyzing processes. The goal is to understand not just what happened, but why it happened.
- Develop Corrective Actions: Based on the investigation findings, corrective actions are developed and implemented to address the root cause of the issue. This may involve revising SOPs, providing additional training, or implementing new control measures.
- Implement and Monitor: The corrective actions are implemented and monitored to ensure their effectiveness. This may involve tracking key metrics and conducting follow-up audits. The goal is to confirm that the issue has been resolved and that there is no likelihood of recurrence.
- Document Everything: Every step of the investigation and resolution process is meticulously documented. This documentation serves as a record of the issue, the actions taken, and the outcome. It also helps prevent future occurrences and demonstrates due diligence to regulatory bodies.
- Preventative Measures: Beyond correcting the immediate issue, we focus on identifying systemic weaknesses that contributed to the problem and implementing preventative measures to avoid similar incidents in the future. This might involve enhanced training, process improvements, or technology upgrades.
This structured approach ensures that compliance issues are handled effectively, efficiently, and with minimal disruption to laboratory operations. Regular review of our processes and internal audits are key to preventing future occurrences.
Q 26. Describe a time you had to navigate a complex regulatory challenge.
One particularly challenging situation involved a significant change to CLIA regulations regarding waived testing. Our lab had several waived tests, and the updated guidelines significantly altered the documentation and quality control requirements. The challenge wasn’t simply updating our SOPs; it involved retraining all personnel on the new protocols and ensuring complete compliance within the stipulated timeframe. The complexities lay in:
- Understanding the Nuances: The new regulations were quite detailed and contained several nuances. We needed to ensure that we fully understood all aspects of the changes, as even small misinterpretations could lead to non-compliance.
- Effective Communication: Communicating the changes to staff, many of whom were not highly scientifically trained, required careful planning and execution. We utilized a tiered training approach, ensuring all staff understood their respective responsibilities and had the appropriate level of training.
- Time Constraints: The deadline for compliance was quite short. We needed to implement the changes quickly without compromising accuracy or quality. This involved careful prioritization and a collaborative team effort.
Our approach involved:
- Expert Consultation: We sought input from regulatory compliance experts to fully understand the implications of the changes.
- Phased Implementation: We rolled out the changes in phases, starting with a pilot program to test the new protocols and refine the training materials.
- Detailed SOP Updates: We created very clear, simple SOPs that included flowcharts, illustrative examples, and step-by-step instructions.
- Ongoing Monitoring: After implementation, we conducted regular audits to ensure compliance and identify any areas that needed further refinement.
Successfully navigating this challenge reinforced the importance of meticulous planning, clear communication, and proactive collaboration within the team and with regulatory experts. The experience also improved our internal processes and strengthened our compliance program.
Q 27. How would you train new employees on CLIA and CAP compliance procedures?
Training new employees on CLIA and CAP compliance procedures is a crucial aspect of maintaining a compliant laboratory. My approach is comprehensive and multi-layered:
- Orientation and Introduction: The training begins with an orientation outlining the importance of compliance and the potential consequences of non-compliance. This sets the tone for a culture of compliance.
- Modular Training: Training is delivered in modules, each focusing on a specific aspect of CLIA and CAP regulations. This includes topics such as quality control, quality assurance, proficiency testing, safety procedures, documentation, and record keeping. This modular approach allows for flexibility and targeted training based on the employee’s role.
- Interactive Sessions: Training sessions are interactive, incorporating discussions, case studies, and practical exercises. This helps employees apply the learned concepts to real-world scenarios. We simulate different scenarios that might occur in the lab to help them develop problem-solving skills in a safe environment.
- Hands-on Training: Practical, hands-on training is provided in the laboratory setting. This allows employees to practice the procedures and gain experience under the supervision of experienced staff. We emphasize the importance of following SOPs diligently.
- SOP Review and Quizzes: All employees are required to review and sign off on the laboratory’s SOPs. Regular quizzes and tests are conducted to assess understanding and retention of the materials. This ensures that employees fully understand and can apply the procedures.
- Mentorship and Shadowing: New employees are paired with experienced staff members for mentorship and shadowing opportunities. This provides additional support and guidance, enhancing their ability to perform tasks accurately and safely.
- Continuing Education: Ongoing training and updates are provided to keep employees informed of any changes in regulations or best practices. This ensures that the lab’s procedures and staff training stay current and effective.
This comprehensive training approach helps equip new employees with the knowledge and skills necessary to perform their duties in compliance with CLIA and CAP regulations, creating a safe and efficient work environment.
Key Topics to Learn for Regulatory Compliance (CLIA, CAP) Interview
- CLIA Regulations: Understanding the different CLIA categories (waived, moderate, high complexity), proficiency testing requirements, quality control procedures, and record-keeping regulations. Practical application: Explain how you’d implement a quality control program to ensure compliance.
- CAP Accreditation: Familiarize yourself with the CAP checklist and inspection process. Understand the importance of maintaining accreditation and the consequences of non-compliance. Practical application: Describe your experience (if any) in preparing for or undergoing a CAP inspection.
- Quality Assurance & Quality Control: Master the concepts of quality assurance (QA) and quality control (QC) within a clinical laboratory setting. Understand the difference between internal and external quality controls and their roles in ensuring accurate and reliable results. Practical application: Develop a plan to address a QC failure.
- Personnel Qualifications & Training: Know the regulatory requirements for personnel qualifications, competency assessments, and continuing education in CLIA and CAP-accredited labs. Practical application: Explain how you would ensure staff competency for a specific test or procedure.
- Regulatory Documentation & Record Keeping: Understand the importance of meticulous record-keeping and documentation. Know the specific requirements for maintaining accurate and readily retrievable records. Practical application: Discuss your approach to maintaining compliant documentation in a high-volume testing environment.
- Risk Management & Corrective Actions: Develop a strong understanding of risk management principles in a regulatory environment. Know how to identify, assess, and mitigate risks related to CLIA and CAP compliance. Practical application: Describe a situation where you identified a compliance risk and the steps you took to correct it.
- Interpreting and Applying Regulations: Demonstrate your ability to interpret complex regulatory language and apply it to practical situations. Show your understanding of how different regulations interact. Practical application: Explain how you would interpret a new regulatory guideline and its implications for your lab’s operations.
Next Steps
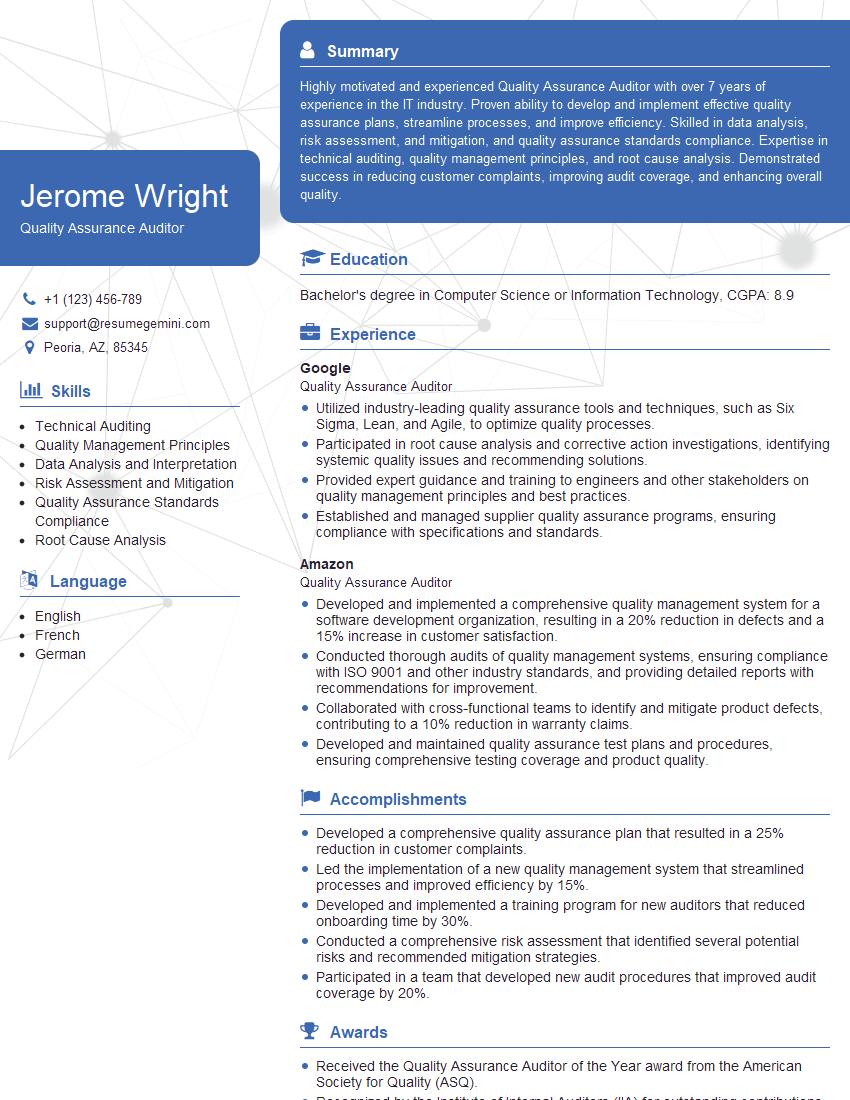
Mastering Regulatory Compliance (CLIA, CAP) is crucial for career advancement in the clinical laboratory industry. It demonstrates a commitment to quality, accuracy, and patient safety, opening doors to leadership roles and increased earning potential. To maximize your job prospects, it’s essential to create an ATS-friendly resume that highlights your relevant skills and experience. ResumeGemini is a trusted resource to help you build a professional and impactful resume that gets noticed. Examples of resumes tailored to Regulatory Compliance (CLIA, CAP) roles are available to guide you through the process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.