Unlock your full potential by mastering the most common Suture Removal and Wound Care interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Suture Removal and Wound Care Interview
Q 1. Describe the proper technique for removing sutures.
Proper suture removal requires a gentle, methodical approach to minimize patient discomfort and prevent complications. First, ensure you have the necessary sterile supplies: sterile gloves, forceps, scissors, antiseptic solution, and a dressing. After cleansing the area, carefully grasp one suture with the forceps, close to the skin’s surface. Gently lift the suture and snip the knot with the scissors as close to the skin as possible. Then, gently pull the suture through, avoiding sudden jerks that could tear the skin. Each suture should be removed individually and the wound should be checked for any bleeding or signs of infection. Finally, the wound should be cleaned and covered with a fresh dressing.
Imagine removing a knot from a delicate piece of fabric—you wouldn’t yank it, would you? The same care is needed with sutures.
Q 2. What are the signs of a suture infection?
Signs of a suture infection can manifest in several ways. Early signs include localized redness, swelling, pain, warmth to the touch around the suture line, and possibly some purulent (pus-filled) drainage. More serious signs could involve increased pain, fever, spreading redness (cellulitis), red streaks extending from the wound (lymphangitis), or the appearance of abscesses. Any of these warrants immediate medical attention.
Think of it like this: a small, localized redness might be a mild irritation, but spreading redness is a clear warning sign of something more serious.
Q 3. How do you assess wound healing?
Assessing wound healing involves a multi-faceted approach. We look at several key factors: Approximation: How well the wound edges are together. Good approximation is crucial for proper healing. Inflammation: The presence of redness, swelling, or warmth indicates an inflammatory response, which is initially normal but excessive or prolonged inflammation suggests problems. Granulation tissue: Healthy healing shows the formation of healthy, pink, granular tissue filling the wound. Epithelialization: The process of new skin cell growth across the wound, closing it. Wound contraction: The gradual shrinking of the wound as it heals. Regular observation and documentation of these factors help guide treatment.
Imagine building a house; you assess the foundation (approximation), the walls (granulation), the roof (epithelialization), and the surrounding landscaping (contraction).
Q 4. What are the different types of sutures and their applications?
Sutures come in various materials and sizes, each suited to specific applications. Absorbable sutures, such as gut or polyglycolic acid (PGA), dissolve over time and are often used internally or in areas where removing them would be difficult. Non-absorbable sutures, like nylon, polypropylene, or silk, require removal. Nylon is strong and is often used for skin closure. Silk is strong but tends to cause more inflammation. The choice depends on the tissue type, wound tension, and location. Size is expressed with a gauge (e.g., 3-0 is finer than 2-0), with finer sutures generally preferred for skin.
Consider it like choosing the right tool for a job: a delicate screwdriver for fine electronics, a robust hammer for heavier tasks.
Q 5. Explain the process of staple removal.
Staple removal is similar to suture removal, though slightly different tools are used. Using a sterile staple remover, gently spread the arms of the remover under a staple to create space, and then squeeze the remover handles, which dislodges the staple and lifts it clear from the skin. The skin may be more sensitive and prone to bleeding than after suture removal. Gentle pressure with sterile gauze is often needed to stop bleeding after staple removal. The wound should then be cleaned and dressed.
Think of it like gently unbending a paperclip—you need to apply pressure at the right points.
Q 6. How do you manage a wound dehiscence?
Wound dehiscence, the separation of wound edges, is a serious complication that requires immediate medical attention. Management involves gently cleansing the wound, approximating the edges (if possible) and dressing the wound with a moist-to-dry dressing to encourage healing. In some cases, surgery may be necessary to close the wound. Antibiotics might be prescribed to prevent infection. Close monitoring and supportive care are crucial for minimizing complications.
Imagine a crack appearing in a wall—it needs immediate repair to prevent further damage.
Q 7. What are the complications associated with suture removal?
Complications associated with suture removal can include: Infection: Redness, swelling, pain, and purulent drainage at the suture site. Bleeding: Minor bleeding is common but excessive bleeding requires attention. Scarring: Excessive scarring is possible depending on the wound and healing process. Suture reaction: Some individuals might have allergic reactions to certain suture materials. Dehiscence: As mentioned above, separation of wound edges. Proper technique and meticulous care can significantly reduce these risks.
Just like any surgical procedure, there are potential complications to be aware of and manage. Good practice is key to minimizing these.
Q 8. How do you handle a patient with excessive bleeding during suture removal?
Excessive bleeding during suture removal is a serious complication that requires immediate attention. It’s crucial to remember that the risk is higher in certain areas, such as the face, where blood vessels are more prominent. The first step is to apply direct pressure to the bleeding site using a sterile gauze pad. Maintain consistent, firm pressure for at least 5-10 minutes, ensuring the gauze doesn’t get saturated and replaced with a fresh one if needed. Elevating the injured area above the heart can also help reduce blood flow. If bleeding persists or is profuse, I would immediately assess the wound for potential underlying causes, such as incomplete hemostasis at the time of surgery, or a slipped suture. Depending on the severity and location, I may need to apply additional sutures or even consider further intervention by a surgeon, such as cauterization.
For instance, I once had a patient who experienced unexpected bleeding during suture removal from a facial laceration. Applying direct pressure for a prolonged time successfully stemmed the bleeding, preventing further complications. However, I closely monitored the patient for a few hours post-removal, ensuring no recurrence of bleeding. It is always wise to document the event meticulously, including the volume of bleeding, actions taken, and patient’s response.
Q 9. Describe your experience with different types of wound dressings.
My experience encompasses a wide range of wound dressings, each suited for different wound types and stages of healing. Simple dressings like gauze pads are excellent for absorbing exudate and maintaining a moist wound environment, ideal for superficial wounds. For wounds requiring more moisture retention, I often use hydrocolloids, which form a gel-like substance on contact with wound fluid. These are great for preventing adherence to the wound bed. Hydrogel dressings, on the other hand, are very effective at hydrating dry wounds and easing pain. Alginate dressings are particularly useful for heavily exudating wounds, as they absorb a significant amount of drainage. Finally, for protecting and covering wounds, transparent films are invaluable, allowing for easy monitoring of the wound healing process.
The choice of dressing depends heavily on the wound’s specific characteristics, including size, depth, exudate level, and location. For example, a minor abrasion might only need a simple gauze dressing, while a deep, infected wound might require a specialized dressing like an alginate to manage significant drainage and promote healing.
Q 10. Explain the importance of proper wound cleaning.
Proper wound cleaning is paramount to preventing infection and promoting optimal healing. It helps remove debris, bacteria, and dead tissue, creating a clean environment conducive to healing. The process typically involves gently cleansing the wound with sterile saline solution or a prescribed antiseptic solution. It’s crucial to avoid harsh scrubbing, which can damage the delicate tissues and delay healing. The technique I usually employ involves irrigating the wound with a syringe to dislodge debris. The wound is then gently cleaned, moving outward from the wound center to avoid contaminating the clean area.
Imagine a garden – if you don’t remove weeds (debris and bacteria) and cultivate the soil (clean the wound bed), healthy growth (healing) will be hindered. Poor wound cleaning can easily lead to delayed healing, infection, and scarring.
Q 11. How do you determine the appropriate time for suture removal?
Determining the appropriate time for suture removal depends on several factors, including the location of the wound, the type of suture material used, the patient’s overall health, and the wound’s healing progress. Generally, sutures placed on the face are removed earlier (around 3-5 days) due to the skin’s rapid healing rate in this area. Sutures in other areas like the extremities are usually left in place longer (7-14 days). The wound’s appearance is also a vital indicator: If the wound edges are well approximated, there’s minimal inflammation, and the surrounding skin is healthy, it’s often a sign that the sutures can be safely removed.
However, each case is unique. I always assess the wound’s progress thoroughly before proceeding with removal, and sometimes opt for delayed removal if needed. For instance, a wound on the lower leg might heal slower due to reduced blood supply, thus necessitating a longer duration for the sutures.
Q 12. What are the different stages of wound healing?
Wound healing is a complex process typically characterized by four distinct stages: inflammation, proliferation, remodeling, and maturation. The inflammatory phase is the initial response, involving blood clotting, swelling, and pain as the body works to clean the wound and prevent infection. The proliferation phase focuses on tissue repair, with the formation of new collagen and granulation tissue filling the wound. Remodeling involves restructuring of the collagen, leading to increased wound strength. Finally, maturation is the stage where the scar matures, reaching its full tensile strength, though the process can take several months.
Understanding these stages is crucial for effective wound care. For instance, during the inflammatory phase, appropriate wound cleaning and dressing are essential. In the proliferation phase, attention shifts towards promoting collagen formation and preventing excessive scarring.
Q 13. How do you educate a patient about post-suture removal care?
Educating patients about post-suture removal care is an essential part of my practice. I typically explain the importance of keeping the wound clean and dry, avoiding harsh scrubbing or rubbing. I emphasize the use of appropriate dressings as needed and advise patients to watch for any signs of infection, such as increased pain, swelling, redness, or discharge. I also provide clear instructions on activities to avoid, such as strenuous exercise or activities that could cause trauma to the healing wound. Specific instructions might include recommendations about wound dressing changes, pain management techniques, and follow-up appointments.
A simple analogy I often use is comparing the wound to a delicate plant needing careful nurturing to grow. Through clear, patient-focused communication, I strive to empower patients to actively participate in their recovery.
Q 14. How do you assess a patient’s pain level during suture removal?
Assessing a patient’s pain level during suture removal involves employing a combination of verbal and non-verbal cues. I usually start by asking the patient to rate their pain on a scale of 0-10, where 0 represents no pain and 10 represents the worst imaginable pain. While the numerical rating scale offers a quantifiable assessment, I also carefully observe the patient’s facial expressions, body language, and vocalizations for additional insights. For patients who are unable to self-report their pain level accurately, such as very young children or individuals with cognitive impairments, observing their behavior and reaction during the procedure provides valuable clues about their discomfort.
Based on the pain assessment, I may administer local anesthetic before removing the sutures if pain is significant, or use other strategies to ease the discomfort, like slower removal or brief pauses.
Q 15. What are the contraindications for suture removal?
Contraindications for suture removal are situations where removing sutures would risk significant complications. This isn’t about simply delaying removal; it’s about understanding when it’s unsafe.
- Signs of infection: Increased redness, swelling, warmth, pain, purulent drainage (pus) around the wound are major red flags. Removing sutures in an infected wound risks spreading the infection and delaying healing. Think of it like trying to mend a torn fabric when it’s already soaked in a contaminating substance – you need to address the contamination first.
- Wound dehiscence (separation): If the wound edges are not well approximated (close together), removing sutures prematurely could lead to further separation and potentially evisceration (organs protruding through the wound). This is a serious complication requiring immediate medical attention.
- Insufficient healing: The wound should show signs of adequate healing, including the formation of granulation tissue (pink, healthy tissue) and reduced inflammation. Premature suture removal in a weak wound will compromise its integrity and healing process.
- Specific surgical sites: Certain surgical sites might require longer suture retention times for optimal healing, especially those under tension or involving complex procedures. For instance, facial sutures often remain in place longer than those on an extremity.
- Patient factors: Factors like patient compliance (following post-operative instructions), underlying health conditions (diabetes, poor circulation), and medication use (immunosuppressants) can impact healing and influence the timing of suture removal.
In essence, the decision to remove sutures hinges on a holistic assessment of the wound and the patient’s overall condition. A careful examination is crucial to prevent unnecessary complications.
Career Expert Tips:
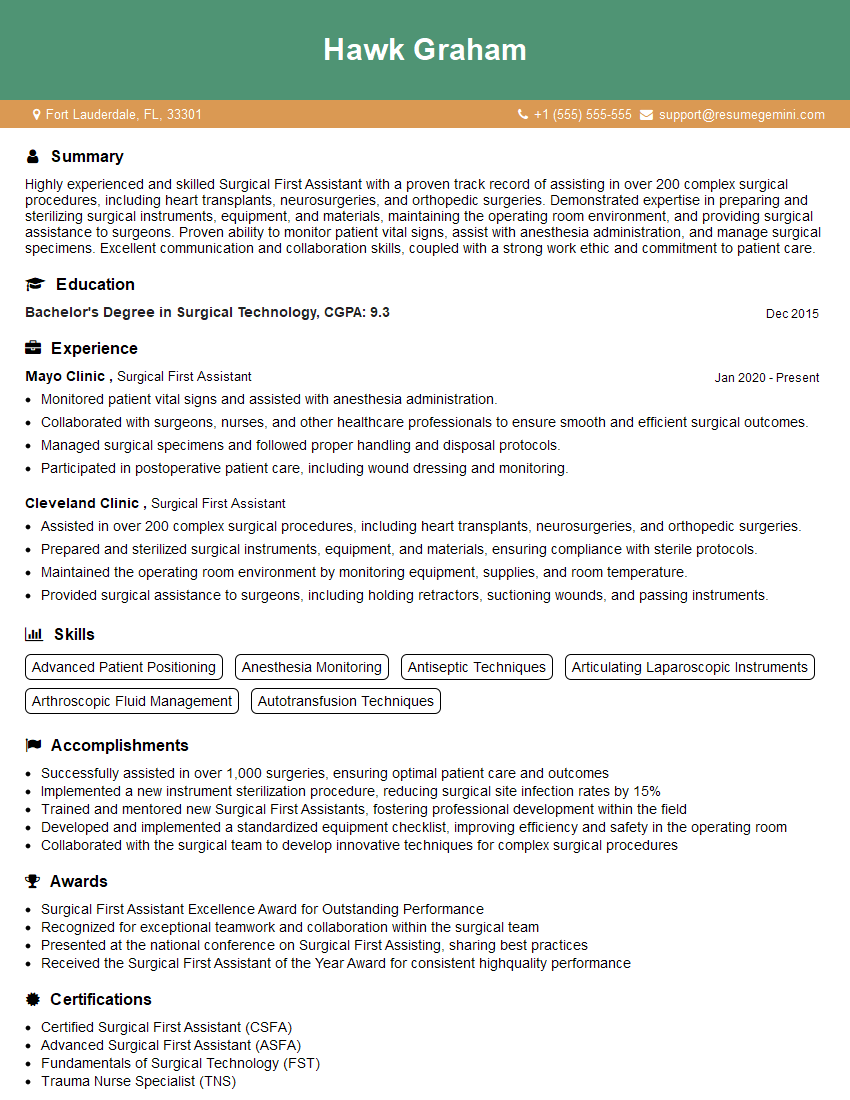
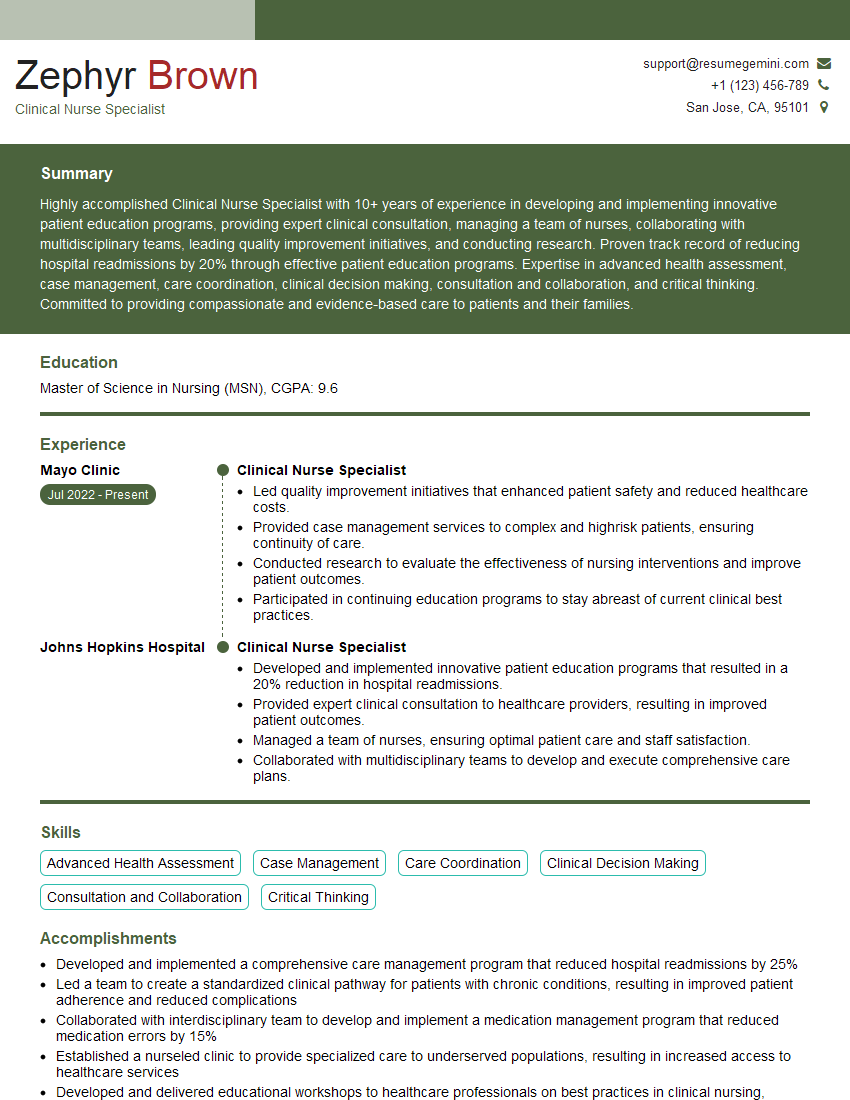
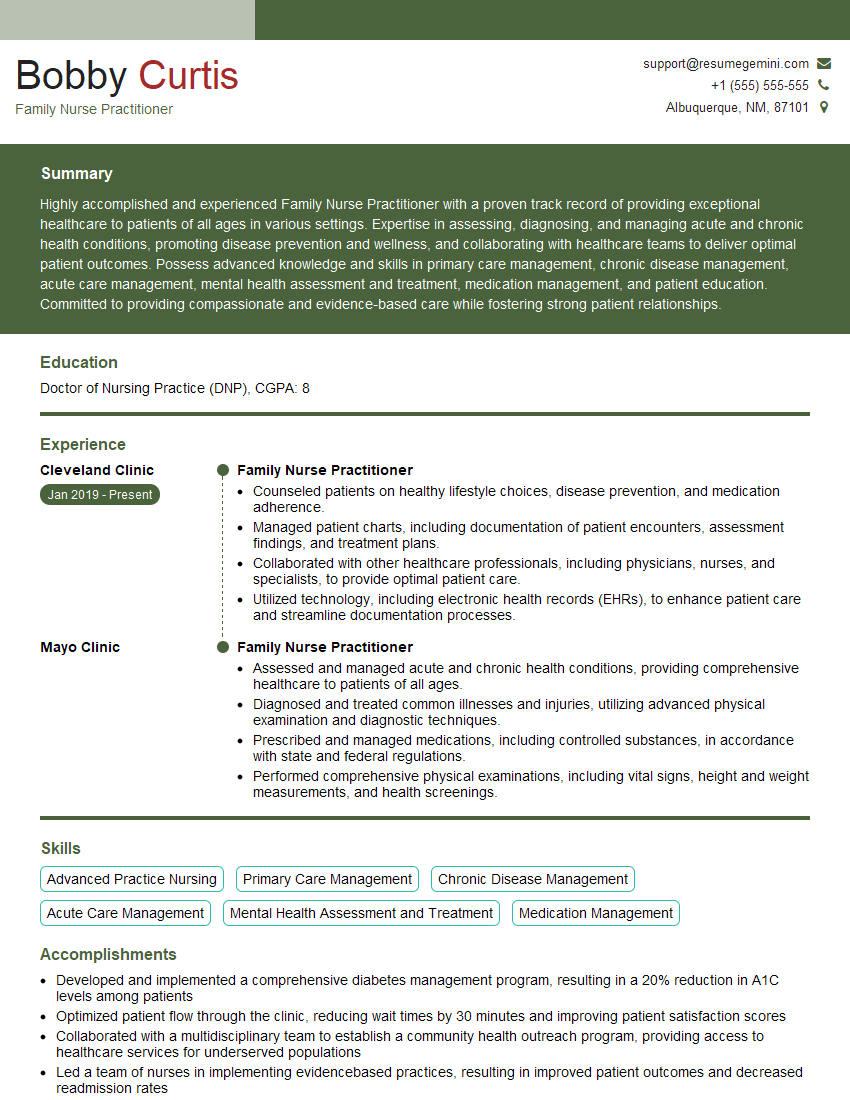
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience with managing various wound types (e.g., lacerations, incisions).
My experience encompasses a broad range of wound types, from simple lacerations to complex incisions. I’ve managed wounds across various anatomical locations and patient demographics. For example, I’ve treated:
- Lacerations: I routinely manage lacerations ranging from minor abrasions to deep, gaping wounds, assessing for nerve, tendon, or vascular damage. Wound cleansing, debridement (removal of dead tissue), and appropriate closure techniques, such as sutures, staples, or adhesives, are essential elements of my approach. I’ve had to adapt my technique based on factors like wound location, depth, and contamination levels.
- Incisions: I’ve extensive experience with post-surgical incision management. This includes monitoring for complications, such as infection, dehiscence, and seroma (fluid accumulation). I tailor my post-op care and suture removal strategies according to the surgical procedure performed, the patient’s medical history, and the healing process. For instance, a post-appendectomy incision requires a different approach than a simple surgical wound closure.
- Chronic wounds: Although not typically addressed with suture removal, I have experience with managing chronic wounds like pressure ulcers or diabetic foot ulcers. These require specialized wound care, addressing factors such as infection control, debridement, and optimizing the moist wound healing environment.
In each case, my approach is individualized, always focusing on minimizing scarring, promoting healing, and preventing infection. Careful documentation is vital in tracking the progress of the wound and its response to treatment.
Q 17. How do you document the suture removal procedure?
Documentation of suture removal is crucial for maintaining accurate medical records, ensuring continuity of care, and providing a legal record of the procedure. My documentation includes:
- Patient identification: Name, medical record number, date of birth.
- Date and time of suture removal: Precise timing is important for tracking healing progress.
- Location and type of sutures: Detailed description of the wound location (e.g., right upper quadrant abdominal incision) and type of suture material (e.g., 3-0 nylon).
- Number of sutures removed: Accurate count to avoid leaving behind sutures.
- Wound assessment: A thorough description of the wound appearance before and after suture removal. This typically includes assessing wound edges, closure, presence of granulation tissue, and signs of infection. I often use standardized descriptors to ensure consistency across documentation (e.g., ‘well approximated edges’, ‘minimal erythema’).
- Dressing applied (if any): Type and size of dressing used, frequency of dressing changes, and relevant instructions for the patient.
- Post-procedure instructions: Any specific patient instructions given (e.g., wound care, activity limitations, follow-up appointment).
- Physician signature or electronic signature: Verification of the procedure and documentation.
For example, a typical entry might read: “03/15/2024, 10:00 AM: Suture removal performed on a 5-cm right knee laceration closed with 3-0 nylon sutures. All 8 sutures removed without complication. Wound edges well approximated. Sterile dressing applied. Patient instructed on wound care and follow-up appointment scheduled for 03/22/2024. Signed: Dr. Example.“
Q 18. What are the common complications associated with wound healing?
Wound healing complications can range from minor inconveniences to life-threatening issues. Common complications include:
- Infection: A common complication, characterized by signs like redness, swelling, warmth, pain, and purulent drainage. Untreated infections can lead to sepsis.
- Dehiscence: Partial or complete separation of wound edges, often due to tension on the wound, infection, or poor healing.
- Evisceration: Protrusion of internal organs through a dehisced wound. This is a surgical emergency.
- Hematoma: Collection of blood beneath the skin, often due to bleeding from disrupted blood vessels.
- Seromas: Collection of serous fluid (clear fluid) under the skin.
- Hypertrophic scars: Raised, red scars that extend beyond the original wound boundaries.
- Keloid scars: Overgrown scars that extend far beyond the original wound and often cause cosmetic concerns.
- Wound contractures: Excessive tightening of the wound, causing restricted movement.
Risk factors for these complications include diabetes, obesity, smoking, poor nutrition, immunosuppression, and inadequate wound care.
Q 19. How do you identify and manage a wound infection?
Identifying and managing a wound infection requires a systematic approach. Key signs and symptoms include:
- Increased pain: Pain that is disproportionate to the expected level of healing.
- Erythema (redness): Significant redness extending beyond the original wound boundaries.
- Swelling: Increased swelling or induration (hardening) around the wound.
- Warmth: Local warmth to the touch compared to surrounding tissues.
- Purulent drainage (pus): Yellowish-green or other discolored discharge from the wound.
- Fever and chills: Systemic signs of infection indicating a more serious situation.
Management strategies include:
- Wound culture and sensitivity testing: To identify the causative organism and guide appropriate antibiotic therapy.
- Antibiotic treatment: Prescribing appropriate antibiotics based on culture results and clinical judgment.
- Debridement: Removal of necrotic (dead) tissue and foreign material to reduce bacterial load.
- Wound irrigation: Washing the wound with sterile saline to remove debris and bacteria.
- Dressing changes: Frequent dressing changes with appropriate wound dressings that promote moist wound healing and prevent further contamination.
- Pain management: Addressing pain with analgesics as needed.
Severe infections might require hospitalization and intravenous antibiotics.
Q 20. Explain the principles of aseptic technique in wound care.
Aseptic technique in wound care is paramount in preventing infection. The goal is to create a sterile environment during wound management to minimize the introduction of microorganisms. Key principles include:
- Hand hygiene: Thorough handwashing with soap and water or the use of an alcohol-based hand rub before and after each wound care procedure.
- Protective barriers: Wearing gloves, gowns, and masks when necessary to prevent contamination. Gowns are especially crucial if you expect wound drainage.
- Sterile instruments and supplies: Using sterile instruments, dressings, and solutions for wound care. Instruments are often sterilized using autoclaves or gas sterilization techniques.
- Preparation of the wound site: Cleaning the wound site with antiseptic solutions such as povidone-iodine or chlorhexidine to reduce the bacterial load. This is often done in a concentric outward circular pattern to minimize cross-contamination.
- Proper disposal of contaminated materials: Disposing of all used materials in appropriate containers to prevent the spread of infection.
- Maintaining a sterile field: Keeping a clean and organized workspace to prevent contamination of instruments and supplies.
Imagine preparing a surgical site as preparing a very delicate dish – every precaution is taken to prevent contamination. The same diligence should be applied to wound care.
Q 21. How do you select the appropriate wound dressing for a specific wound?
Selecting the appropriate wound dressing is crucial for optimal wound healing. The choice depends on several factors:
- Type of wound: Acute wounds (surgical incisions, lacerations) heal differently than chronic wounds (pressure ulcers, diabetic foot ulcers). Acute wounds often require simple dressings to protect the wound, whereas chronic wounds may require dressings to promote debridement, manage drainage, or maintain a moist wound environment.
- Wound size and depth: Larger and deeper wounds might require larger dressings or specialized dressings that conform to the wound bed.
- Amount of drainage: Highly draining wounds require dressings that can absorb large amounts of fluid, such as alginate dressings or superabsorbent foam dressings.
- Wound bed characteristics: The presence of necrotic tissue (dead tissue), granulation tissue, or eschar (dry, black tissue) will influence dressing choice. For instance, dressings that facilitate autolytic debridement (body’s natural process of removing dead tissue) might be preferred for wounds with necrotic tissue.
- Patient factors: Patient allergies, skin sensitivity, and cost considerations will also factor into the selection.
For instance, a simple surgical incision might be dressed with a simple non-adherent dressing to protect it and allow for observation. A pressure ulcer, however, might require a complex dressing regimen involving a combination of alginate, foam, and gauze dressings depending on its stage and the amount of exudate.
Q 22. Describe your experience with negative pressure wound therapy.
Negative pressure wound therapy (NPWT), also known as vacuum-assisted closure (VAC) therapy, is a technique used to promote healing in chronic and acute wounds that are not healing properly. It involves applying a sealed dressing to the wound, connected to a vacuum pump that gently removes excess fluid, bacteria, and debris. This creates a moist wound environment that stimulates cell growth and granulation tissue formation.
My experience with NPWT spans several years and includes managing a wide variety of wounds, from post-surgical incision sites to diabetic ulcers and pressure sores. I’ve found it particularly effective in situations where traditional wound dressings were insufficient in promoting healing. For instance, I successfully used NPWT on a patient with a large, infected leg ulcer that had resisted other treatments for months. The NPWT significantly reduced the infection, promoted granulation tissue formation, and eventually allowed the wound to close. I am proficient in selecting the appropriate NPWT settings and dressings based on the individual patient’s needs and the type of wound. Regular monitoring of the wound bed and adjusting the pressure settings are key components of successful NPWT management.
Q 23. What are the signs and symptoms of a wound hematoma?
A wound hematoma is a collection of blood outside of blood vessels, forming a bruise or lump near a wound. Think of it like a localized internal bleeding within the tissue surrounding the wound.
- Signs: A noticeable swelling or mass near the wound site, often fluctuant (meaning you can feel a wave of fluid beneath the skin).
- Symptoms: Pain, tenderness, discoloration (often bluish or purplish), potential for increased pressure and discomfort in the affected area. In severe cases, a hematoma can cause significant pressure on nearby structures and compromise circulation.
The severity of signs and symptoms varies depending on the size and location of the hematoma. Small hematomas may resolve on their own, but larger ones often require medical intervention.
Q 24. How do you handle a patient who experiences discomfort during suture removal?
Patient discomfort during suture removal is common, and managing it is crucial for a positive patient experience. I always begin by explaining the procedure clearly and reassuring the patient.
- Pain Management: I offer topical anesthetic creams or sprays to numb the area beforehand. This significantly reduces discomfort. In some cases, a local anesthetic injection might be needed for more extensive or sensitive areas.
- Gentle Technique: I use sharp, sterile scissors and forceps. I work slowly and deliberately, cutting the suture as close to the skin as possible and gently pulling the suture out, avoiding jerking movements that could cause pain or tearing.
- Distraction Techniques: Engaging the patient in conversation or allowing them to focus on something else can help to distract them from the sensation.
- Breaks: If the patient experiences significant pain, I break the procedure into smaller steps with rest periods in between.
The key is to be empathetic, communicate effectively, and adjust the approach based on the patient’s response. A patient’s comfort is my top priority.
Q 25. Explain the difference between absorbable and non-absorbable sutures.
The main difference between absorbable and non-absorbable sutures lies in their behavior within the body.
- Absorbable sutures: These sutures are gradually broken down and absorbed by the body’s enzymes over time. Common materials include catgut (made from collagen) and synthetic polymers like polyglycolic acid (PGA) and polylactic acid (PLA). They are typically used for internal stitches or in situations where removing sutures is difficult or undesirable.
- Non-absorbable sutures: These sutures remain in the body indefinitely unless surgically removed. They are made from materials like nylon, polypropylene, silk, or stainless steel. They are usually preferred for skin closure because their strength is needed for wound support while it heals.
Choosing between absorbable and non-absorbable sutures depends on several factors, including the wound location, tissue type, and the surgeon’s preference. The surgeon makes the initial suture selection based on patient condition, wound characteristics and surgical strategy. I often consult with surgeons before making a decision on suture removal and care.
Q 26. How do you manage a wound that is not healing properly?
Managing a wound that’s not healing properly requires a systematic approach, starting with a thorough assessment.
- Assessment: This involves evaluating the wound size, depth, appearance (color, presence of exudate), and surrounding tissue. Factors like diabetes, vascular disease, and infection need to be considered.
- Debridement: Removal of dead or infected tissue from the wound is often essential to promote healing. This can be done surgically, enzymatically, or using autolytic methods (the body’s own mechanisms).
- Infection Control: If infection is present, appropriate antibiotics must be administered. This is often guided by culture results.
- Wound Dressings: Selecting the appropriate dressing is crucial to maintain a moist wound environment, prevent infection, and manage excess exudate. Different dressings are used depending on the wound type and stage of healing.
- Optimizing Systemic Factors: Addressing underlying conditions such as diabetes, poor circulation, and malnutrition can significantly improve wound healing. This may involve managing blood sugar levels, improving vascular health, or nutritional support.
- Advanced Therapies: In some cases, more advanced therapies like NPWT, hyperbaric oxygen therapy, or skin grafts may be necessary.
Often, non-healing wounds require a multidisciplinary approach involving a surgeon, wound care specialist, and other healthcare professionals.
Q 27. Describe your experience with different types of wound closure techniques.
I have experience with a range of wound closure techniques, each appropriate for different situations and wound types.
- Sutures: The most common method, involving stitching the wound edges together. The type of suture used (absorbable or non-absorbable, material and size) varies based on the wound and location.
- Staples: Metal staples are sometimes used for larger wounds, particularly in areas where tension is high, such as scalp wounds. They provide quick closure but require removal.
- Surgical Tape (Steri-Strips): Used for smaller, superficial wounds with minimal tension. These are adhesive strips that hold the wound edges together, leaving no marks.
- Adhesive Tissue Sealants: These are liquid or spray-on adhesives used to close wounds, especially smaller ones or those difficult to suture. They’re often used in conjunction with other methods.
- Wound Vacuum Assisted Closure (NPWT): As mentioned earlier, NPWT aids wound healing by removing exudate and promoting granulation, contributing to improved closure.
The choice of technique is dictated by many factors including the wound size, location, depth, type and condition of the surrounding tissues, and the overall health of the patient. The selection is usually done in collaboration with the surgeon.
Q 28. What are the legal and ethical considerations related to suture removal and wound care?
Legal and ethical considerations related to suture removal and wound care are paramount.
- Informed Consent: Before any procedure, the patient must provide informed consent, meaning they understand the procedure, risks, and benefits. This applies to suture removal as well as wound care treatment plans.
- Infection Control: Maintaining strict adherence to sterile techniques is crucial to prevent infections. Failure to do so can result in legal repercussions.
- Documentation: Detailed and accurate documentation is essential. This includes recording the procedure details, the patient’s response, and any complications encountered. Good documentation protects the healthcare professional.
- Confidentiality: Maintaining patient confidentiality is a legal and ethical obligation. Patient information must be handled according to HIPAA regulations or equivalent.
- Competence: Performing procedures within the scope of one’s training and competence is essential. Undertaking procedures beyond one’s capabilities could lead to legal consequences.
- Pain Management: Providing adequate pain relief during procedures is a critical ethical consideration. Neglecting pain management can lead to ethical and legal issues.
Ethical and legal compliance is fundamental to the practice of suture removal and wound care. It ensures the safety and well-being of the patient and protects the healthcare provider.
Key Topics to Learn for Suture Removal and Wound Care Interview
- Aseptic Technique: Understanding and applying principles of sterile technique to prevent infection during suture removal and wound care.
- Suture Types and Properties: Knowing the characteristics of different suture materials (absorbable vs. non-absorbable, strength, etc.) and their appropriate applications.
- Suture Removal Techniques: Mastering the proper steps for removing sutures, including cutting and removing the suture without causing trauma to the wound.
- Wound Assessment: Accurately evaluating wound healing, identifying signs of infection (redness, swelling, drainage), and determining appropriate next steps.
- Wound Dressing Selection and Application: Choosing the right type of dressing based on wound type and stage of healing, and applying it correctly to promote healing and protect the wound.
- Patient Education: Explaining post-operative care instructions to patients, including signs of complications and when to seek medical attention.
- Complication Recognition and Management: Identifying potential complications such as infection, dehiscence, or hematoma, and knowing appropriate response protocols.
- Legal and Ethical Considerations: Understanding relevant regulations and ethical guidelines related to patient care and documentation.
- Practical Application: Scenario-based problem-solving: Imagine different wound types (e.g., lacerations, surgical incisions) and practice your approach to assessment, suture removal, and wound care.
Next Steps
Mastering Suture Removal and Wound Care is crucial for career advancement in healthcare. A strong understanding of these procedures demonstrates competence and professionalism, opening doors to diverse opportunities and potentially higher salaries. To maximize your job prospects, crafting an ATS-friendly resume is essential. ResumeGemini is a trusted resource to help you build a professional and impactful resume that highlights your skills and experience effectively. We offer examples of resumes tailored to Suture Removal and Wound Care to help you get started. Invest time in crafting a compelling resume – it’s your first impression on potential employers.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.