Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Orthotics and Custom Foot Support interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Orthotics and Custom Foot Support Interview
Q 1. Explain the different types of custom foot orthotics and their applications.
Custom foot orthotics are categorized based on their design and intended function. They aren’t a one-size-fits-all solution; the type prescribed depends entirely on the individual’s needs.
- Functional Orthotics: These address biomechanical issues like overpronation (feet rolling inward excessively) or supination (feet rolling outward excessively). They aim to improve foot alignment and reduce stress on joints. Think of them as correcting the mechanics of walking. For example, someone with plantar fasciitis might benefit from a functional orthotic providing medial arch support and heel cushioning.
- Accommodative Orthotics: These focus on cushioning and pressure relief. They’re often used for conditions like diabetic neuropathy (nerve damage in the feet) or rheumatoid arthritis, where pressure points need protection. They might have deep heel cups and extra padding to reduce stress on sensitive areas. A patient with a diabetic ulcer would likely need an accommodative orthotic to prevent further injury.
- Biomechanical Orthotics (Full-Contact Orthotics): These provide comprehensive support covering the entire plantar surface of the foot. They correct biomechanical issues and offer pressure relief simultaneously. This type is typically used for more complex conditions requiring significant correction of foot function. Patients with significant flat feet or multiple foot deformities may need a biomechanical orthotic.
- Rigid Orthotics: Constructed from more durable materials like carbon fiber or graphite, these are designed for individuals needing significant structural support. Often prescribed for severe conditions like Charcot foot. They offer excellent control and stability.
- Semi-rigid Orthotics: Offer a balance between flexibility and support, suitable for patients requiring some structural correction but also needing some flexibility in their footwear.
Q 2. Describe the process of casting and molding for custom orthotics.
Creating custom orthotics begins with a meticulous process. It’s like making a perfect, supportive mold of a sculpture, but the sculpture is your foot!
- Foot Examination and Assessment: The process starts with a thorough examination of the patient’s feet, legs, and gait. This helps determine the appropriate type and design of orthotic.
- Casting: A foam box is typically used to enclose the patient’s foot in a neutral position, ensuring an accurate representation of the foot’s structure. A low-viscosity casting material (typically plaster or foam) is then carefully applied, creating a negative impression of the foot and ankle.
- Model Creation: Once the cast has set, it’s removed, and the material is trimmed. Then, a positive model of the foot is created using a casting material like plaster, hydrostone, or resin. This model is the three-dimensional copy of the patient’s foot.
- Modification and Shaping: The model is modified based on the patient’s biomechanical assessment and the orthotic design. Sections may be added or removed to address specific needs, such as arch support or heel cushioning.
- Shell Fabrication: The model is then used to create the orthotic shell, using a variety of materials (discussed in the next question).
- Covering and Finishing: Once the shell is complete, it’s covered with a softer top material, often leather, foam, or a synthetic material, to improve comfort and durability. Finally, the orthotic undergoes a quality check before being fitted to the patient.
Q 3. What materials are commonly used in the fabrication of custom orthotics, and what are their respective advantages and disadvantages?
The selection of materials significantly impacts the orthotic’s performance, comfort, and longevity. Each material has unique properties making it suitable for certain conditions.
- EVA (Ethylene-vinyl acetate): A common material, EVA is lightweight, shock-absorbent, and relatively inexpensive. However, it’s less durable than other options and may not provide the same level of structural support.
- Polypropylene: A more rigid material, polypropylene offers excellent durability and structural support. It’s frequently used for functional orthotics. Its downside is that it’s less flexible and can be less comfortable initially for some patients.
- Carbon Fiber/Graphite: These high-tech materials offer exceptional strength, lightweight, and stiffness. Perfect for highly active patients or those needing maximum support. However, these come with a higher price tag.
- Leather: Often used for the top cover of the orthotic. Leather is breathable and conforms to the foot well over time. It requires some maintenance to ensure its durability.
- Foam: Provides cushioning and comfort, often used in combination with other materials for additional shock absorption and pressure relief.
The choice of material depends on factors such as patient activity level, foot type, diagnosis, and the budget.
Q 4. How do you assess a patient’s foot biomechanics to determine the appropriate type of orthotic?
Assessing foot biomechanics involves a combination of observation and measurement. It’s a bit like detective work, piecing together clues to understand the foot’s movement.
- Visual Inspection: We observe foot posture, examining for deformities like bunions, hammertoes, or flat feet. We look at alignment of the foot relative to the leg and ankle.
- Palpation: We feel the foot for areas of tenderness, muscle tightness, or bone prominence. This helps identify areas of potential stress or inflammation.
- Range of Motion Assessment: We assess the flexibility and mobility of the foot and ankle joints. Restricted movement can indicate underlying problems.
- Gait Analysis (discussed further in the next question): Observing the patient’s walking pattern reveals crucial information about their biomechanics, such as pronation or supination.
- Foot Posture Index (FPI): This is a quantitative assessment of foot posture, providing a numerical score that helps standardize assessment and tracking of changes over time.
- Weight-Bearing Footprints: Plantography shows pressure distribution and can identify areas of excessive pressure.
This comprehensive assessment enables us to determine if the patient needs orthotics, the type required (functional, accommodative, etc.), and the specific design features needed, such as arch support, heel cushioning, or metatarsal pads.
Q 5. Discuss the role of gait analysis in orthotic prescription.
Gait analysis plays a crucial role in accurately prescribing orthotics. It’s like watching a film of someone walking and analyzing each frame to spot potential problems.
Through gait analysis (which can include visual observation, video recording, and more advanced methods like pressure plate analysis and motion capture), we assess:
- Stance Phase: We observe how the foot contacts the ground and the weight distribution across the foot. This highlights areas of excessive stress.
- Swing Phase: We examine the leg’s movement during the swing phase to identify any compensations or abnormalities that might be contributing to foot problems.
- Step Length and Cadence: These parameters help determine the overall efficiency and effectiveness of gait.
- Pronation and Supination: Gait analysis helps quantify the degree of pronation or supination, critical information for designing functional orthotics.
By carefully studying gait, we can identify the underlying causes of foot problems and design orthotics that effectively correct biomechanical imbalances, ultimately improving gait and reducing pain.
Q 6. Explain the concept of pressure relief in orthotic design.
Pressure relief in orthotic design is crucial for protecting sensitive areas of the foot and preventing injuries. Imagine distributing the weight of your body evenly instead of concentrating it in one spot.
We achieve pressure relief through several strategies:
- Heel Cushioning: A deep heel cup helps distribute pressure across a larger surface area, reducing stress on the heel. This is vital for patients with heel pain or plantar fasciitis.
- Metatarsal Pads: These pads relieve pressure on the ball of the foot, benefiting patients with metatarsalgia (pain in the ball of the foot).
- Material Selection: Selecting cushioning materials like EVA foam helps absorb impact and distribute pressure more evenly.
- Accommodation for Deformities: For patients with foot deformities (like bunions or hammertoes), orthotics are designed to accommodate the deformity and reduce pressure on the affected area.
Careful consideration of pressure distribution is fundamental to successful orthotic design, ensuring patient comfort and preventing further injury.
Q 7. How do you address common complications associated with orthotic use, such as skin irritation or discomfort?
Although custom orthotics are designed to improve comfort, some complications can occur. Proactive measures are key to avoid these issues.
- Skin Irritation: This is a common problem, often caused by friction or pressure points. We address this by ensuring proper fitting, using breathable materials (like leather), and recommending the use of lubricating powders or creams to reduce friction.
- Discomfort: Initial discomfort is sometimes experienced as the foot adjusts to the orthotic. We advise a gradual introduction of orthotic use, starting with short periods and gradually increasing the wear time. Padding or modifications can be implemented if necessary.
- Calluses and Blisters: These often arise from excessive pressure or friction. We identify and address pressure points by adjusting the orthotic or using specialized padding materials.
- Nail Problems: Improperly fitting orthotics may put pressure on nails, leading to ingrown toenails or other problems. Regular monitoring and adjustments are important to avoid this.
Regular follow-up appointments allow for adjustments and monitoring. Open communication between patient and clinician is crucial to address any complications promptly and effectively.
Q 8. What are the key differences between accommodative, supportive, and corrective orthotics?
Orthotics are categorized into accommodative, supportive, and corrective types, each serving a distinct purpose in managing foot and lower limb conditions. Think of them as addressing different levels of foot problem severity.
- Accommodative orthotics primarily aim to reduce pressure and friction on specific areas of the foot. They’re like cushions, providing relief from painful conditions like plantar fasciitis or diabetic foot ulcers. They might incorporate deep heel cups for shock absorption or metatarsal pads to alleviate pressure on the ball of the foot. For example, a patient with a bunion might benefit from a device that creates space around the prominent bone.
- Supportive orthotics offer more substantial structural support to the foot and ankle. They improve the overall alignment and stability of the foot, often mitigating issues caused by flat feet or excessive pronation. Imagine them as adding structure and support to a poorly built foundation. These orthotics may include a substantial medial arch support and a firm heel counter to help control foot motion.
- Corrective orthotics are designed to actively modify foot mechanics and posture. These are more sophisticated and actively change how the foot functions. They’re used for more severe conditions, addressing problems such as forefoot varus (inward turning of the forefoot) or pes cavus (high arch). These orthotics often have features like a wedge to adjust the position of the foot or an extended medial post to help control pronation. It’s like a building renovation – a major change to improve functionality and reduce structural issues.
Q 9. Describe your experience with various orthotic materials, including plastics, foams, and carbon fiber.
My experience spans a wide range of orthotic materials, each with its own unique properties and applications. The choice of material depends heavily on the patient’s needs, activity level, and the specific condition being addressed.
- Plastics: Thermoplastic materials like polypropylene and polyethylene are widely used due to their durability, moldability, and ability to provide excellent support. They are often used in corrective orthotics where precise control of foot mechanics is crucial. I frequently use these for patients with significant structural deformities.
- Foams: Ethylene vinyl acetate (EVA) and polyurethane foams offer cushioning and comfort, often incorporated in accommodative orthotics. They’re lightweight and readily adaptable for partial foot coverings or for use within a shoe. These are good for patients with mild conditions or those who prioritize comfort over rigid support.
- Carbon fiber: This advanced material provides exceptional strength and stiffness while remaining relatively lightweight. It’s primarily used in high-performance orthotics for athletes or individuals with significant biomechanical needs who require maximum support and shock absorption. I’ve successfully used this for runners with plantar fasciitis, reducing pain and improving performance.
Selecting the right material involves a careful assessment of the patient’s condition, lifestyle, and functional goals. For instance, a high-impact athlete might benefit from carbon fiber, while a sedentary individual with plantar fasciitis might be better suited to a softer foam material.
Q 10. How do you ensure proper fit and function of a custom orthotic?
Ensuring proper fit and function is paramount. It involves a multi-step process starting with a thorough assessment.
- Detailed assessment: This includes a comprehensive patient history, gait analysis (observing their walking pattern), range of motion tests, and palpation of the feet to identify areas of pressure, pain, or deformity. This helps to pinpoint the underlying biomechanical issue.
- Casting (if applicable): Accurate casting is critical for custom orthotics. This captures the precise shape of the foot and ankle to create a perfectly fitting device. I use various methods, including foam box and plaster of Paris (detailed in the following answer).
- Modification & Adjustments: After initial fabrication, the orthotic undergoes modifications to fine-tune the fit and address any identified pressure points. This often involves using grinders, files, and heat to refine the shape and enhance comfort.
- Trial and Evaluation: Patients are fitted with the orthotics, and their gait and comfort are observed. Any necessary adjustments are made based on feedback from the patient and my clinical observations. This is an iterative process, allowing for optimization.
- Patient education: This is critical. The patient is educated on how to properly wear and care for the orthotics, including appropriate footwear and hygiene.
This iterative approach ensures the final product effectively addresses the patient’s needs and maximizes its benefit.
Q 11. Explain your understanding of the biomechanical principles underlying orthotic design.
Biomechanical principles are fundamental to orthotic design. We aim to influence the forces and movements acting on the foot and lower limb to improve function and reduce pain.
- Foot and ankle kinematics: Understanding the movement of the foot and ankle during the gait cycle (walking) is essential. We analyze pronation (inward rolling) and supination (outward rolling) to determine the optimal level of control needed.
- Force distribution: Orthotics help redistribute weight and pressure across the foot, relieving stress on areas such as the heel, arch, or metatarsal heads. This is particularly crucial in conditions like plantar fasciitis or diabetic foot ulcers.
- Muscle activation: Orthotics can influence muscle activation patterns, potentially improving muscle efficiency and reducing strain. This relates to how the orthotic supports the foot and how that influences the muscles controlling the lower leg and foot.
- Joint alignment: By influencing the alignment of joints like the ankle and subtalar (ankle bone) joint, we can improve overall lower limb mechanics and potentially alleviate pain and dysfunction originating higher up in the leg.
For example, a patient with excessive pronation might benefit from an orthotic that provides medial arch support to control the inward rolling of the foot during gait.
Q 12. Describe your experience with different casting methods (e.g., foam box, plaster of Paris).
I have extensive experience with various casting methods. The choice of method depends on factors like patient comfort and the level of detail required.
- Foam box method: This is a simpler, faster technique, often used for less complex cases. A patient’s foot is immersed in a foam material, which shapes around the foot, providing a mold. It’s quick, comfortable, and good for basic accommodative orthotics. However, it’s less precise than plaster casting.
- Plaster of Paris method: This traditional method uses plaster bandages to create a highly detailed and accurate cast of the foot. It’s used when greater precision is necessary, for example in cases requiring corrective orthotics where precise alignment is crucial. While more time-consuming, it offers superior detail and captures the subtle anatomy of the foot more effectively.
Each method has its advantages and limitations. The foam box is great for speed and patient comfort, while plaster of Paris provides the detail required for intricate corrective devices. I select the method based on the individual patient’s needs and the complexity of the orthotic required.
Q 13. How do you modify an orthotic to improve its fit or function?
Modifying an orthotic to improve fit or function is a common practice. It requires a keen eye for detail and a good understanding of biomechanics.
- Grinding and filing: Excess material is carefully removed using grinders and files to refine the shape and address pressure points. This is a precise process, needing to be done slowly and carefully to avoid weakening the device.
- Heat molding: Thermoplastic materials can be reshaped using heat guns. This allows for adjustments to the arch height, heel cup depth, or overall shape of the orthotic. This requires experience to avoid damaging the material.
- Adding and removing components: Components like metatarsal pads, heel wedges, or medial posts can be added or removed to fine-tune the support and pressure relief provided by the device. This is done based on patient feedback and ongoing assessment.
For example, a patient might report discomfort under the metatarsal heads. I would then carefully grind down the material in that area to reduce pressure. Alternatively, if a patient requires more arch support, I might add a medial post to the orthotic.
Q 14. Explain your experience with different types of footwear and their impact on orthotic effectiveness.
Footwear plays a crucial role in the effectiveness of orthotics. The shoe must be compatible with the orthotic to ensure proper function and prevent discomfort.
- Shoe type: The height and stiffness of the shoe’s heel counter influence orthotic performance. A shoe with a stiff heel counter provides more support, complementing the function of a supportive orthotic. Conversely, a flexible shoe might undermine the structural support offered by a corrective orthotic. Shoes with adequate depth are also essential, providing space for the orthotic to sit properly.
- Shoe materials: Flexible and breathable materials help reduce heat and moisture build-up, improving comfort for the patient. Rigid shoes, while helpful for certain types of orthotics, can put unnecessary stress if not matched to the needs.
- Shoe size and fit: The shoe should be appropriately sized to accommodate the orthotic without excessive pressure or restriction. A well-fitting shoe complements the orthotic, ensuring proper alignment and function.
For instance, a patient with a rigid orthotic will need a shoe with enough depth and a sturdy heel counter. Ignoring the shoe’s role can greatly compromise the orthotic’s effectiveness and lead to patient dissatisfaction.
Q 15. How do you communicate effectively with patients about their orthotic needs and treatment plan?
Effective communication with patients is paramount in orthotics. I begin by actively listening to their concerns and understanding their lifestyle, activity levels, and pain descriptions. I then explain their diagnosis in clear, non-medical terms, avoiding jargon. Using visual aids like anatomical diagrams or 3D models can significantly enhance understanding. I collaboratively develop a treatment plan, explaining the purpose and benefits of each component, including the type of orthotic recommended, the materials used, and the expected timeline for improvement. I encourage questions throughout the process and ensure the patient feels empowered and informed.
For example, if a patient presents with plantar fasciitis, I wouldn’t just say, ‘You need a custom foot orthotic.’ Instead, I’d explain that plantar fasciitis is an inflammation of the plantar fascia (showing them an image), and that the orthotic will help support the arch, reduce strain on the fascia, and alleviate pain. We’d discuss their daily activities – are they a runner? Do they stand for long periods? – to tailor the orthotic to their specific needs.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience with patient education related to orthotic use and care.
Patient education is an integral part of successful orthotic therapy. I provide detailed instructions on how to properly wear and care for their orthotics, emphasizing hygiene and proper cleaning methods. I explain the importance of gradually increasing wear time to allow for adaptation and demonstrate the correct placement of the orthotic within the shoe. I also educate patients on recognizing signs of irritation or discomfort and encourage them to contact me immediately if any issues arise. I frequently use handouts with clear instructions and diagrams to reinforce key points. I often schedule follow-up appointments to monitor progress, address any concerns, and make any necessary adjustments to ensure a comfortable fit and optimal therapeutic effect.
For instance, I might provide a patient with a handout depicting the proper way to clean their orthotics, including the recommended cleaning solutions and drying methods. I will also explain the potential need for shoe modifications to accommodate the orthotics.
Q 17. How do you manage patient expectations regarding orthotic outcomes?
Managing patient expectations is crucial to prevent disappointment. I strive to be realistic and transparent about the potential outcomes of orthotic treatment. I explain that while orthotics can significantly improve symptoms, they are not a cure-all. The timeframe for improvement varies depending on the individual’s condition, the severity of the problem, and their adherence to the treatment plan. I discuss potential limitations and alternative treatment options if necessary. I ensure the patient understands that consistent use of the orthotic is essential for achieving the best results. Open communication and regular follow-up appointments help to monitor progress and adjust expectations as needed.
For example, a patient with severe arthritis might not experience complete pain relief, but we can aim for a significant reduction in pain and improved mobility. I will clearly articulate these realistic goals during our initial consultation.
Q 18. Describe your experience with different types of foot pathologies and their corresponding orthotic interventions.
My experience encompasses a wide range of foot pathologies. For example, I’ve worked with patients suffering from plantar fasciitis, where custom orthotics with medial arch support and heel cushioning are often prescribed. Pes cavus (high arches) requires orthotics that address excessive pronation and provide cushioning and metatarsal support. Patients with pes planus (flat feet) benefit from orthotics that provide arch support and control excessive pronation to prevent further complications. I’ve also treated diabetic patients, focusing on pressure relief and preventing ulcer formation, often utilizing specialized materials and designs. Additionally, I have experience with rheumatoid arthritis, where orthotics can help improve joint stability and reduce pain. The choice of orthotic design and materials are tailored to each specific pathology and the patient’s individual needs and activity level.
Q 19. How do you measure and document relevant patient data for orthotic prescription?
Accurate measurement and documentation are fundamental for successful orthotic prescription. I use a combination of static and dynamic measurements. Static measurements include using a plantigrade foot assessment, measuring foot length, width, arch height, and heel characteristics. Dynamic measurements involve observing the patient’s gait and foot function, assessing weight-bearing posture and range of motion. I utilize specialized tools like footprint scanners and goniometers for precise data collection. This information, along with the patient’s medical history and lifestyle factors, is meticulously documented in the patient’s chart, including digital images and videos of gait analysis. This comprehensive data ensures the orthotic design accurately addresses the patient’s unique biomechanical needs.
Q 20. Describe your understanding of the regulatory requirements related to orthotics fabrication and fitting.
I am well-versed in the regulatory requirements for orthotic fabrication and fitting. This includes adhering to infection control protocols, maintaining accurate patient records, ensuring proper sterilization techniques, and following all relevant health and safety regulations, which vary based on the country and state. I understand the importance of maintaining appropriate documentation for insurance billing and complying with medical device regulations, such as those related to material safety and labeling requirements. Continuing professional development keeps me updated on the latest regulations and best practices.
Q 21. Explain your experience with CAD/CAM technology in orthotics design and fabrication.
I have extensive experience with CAD/CAM (Computer-Aided Design/Computer-Aided Manufacturing) technology in orthotics. This technology allows for precise and efficient design and fabrication of custom orthotics. I utilize 3D scanning systems to capture detailed anatomical data, which is then used to create a digital model of the patient’s foot. This model is used to design the orthotic, considering factors like pressure distribution, arch support, and heel cushioning. The design is then transmitted to a milling machine for automated fabrication, resulting in a highly accurate and personalized orthotic. CAD/CAM significantly improves efficiency, accuracy, and consistency compared to traditional methods, leading to superior patient outcomes.
For example, CAD/CAM allows me to precisely adjust the shell thickness in specific areas of the orthotic based on pressure mapping data to optimize pressure relief for a patient with diabetic neuropathy.
Q 22. Describe your proficiency in using various orthotic design software.
My proficiency in orthotic design software spans several leading platforms. I’m highly skilled in using CAD/CAM software such as Paramount, Orthotic Pro, and Easy Ortho. These programs allow me to create precise 3D models of orthotics, ensuring accurate fit and function. I’m comfortable with all aspects of the software, from initial patient data capture and model creation to generating milling instructions for fabrication. For example, I recently used Paramount to design a custom foot orthotic for a patient with severe plantar fasciitis, incorporating specific pressure relief zones identified during a gait analysis. The software’s ability to simulate pressure distribution allowed for precise adjustments before fabrication, ultimately leading to a more effective and comfortable orthotic for the patient.
Beyond 3D modeling, I’m also proficient in using software for generating reports and documenting the orthotic design process. This is crucial for maintaining accurate patient records and facilitating communication with other healthcare professionals.
Q 23. How do you stay current with the latest advancements in orthotics and prosthetic technology?
Staying current in the rapidly evolving field of orthotics and prosthetics requires a multifaceted approach. I actively participate in professional development activities, including attending conferences like the American Academy of Orthopaedic Surgeons (AAOS) annual meeting and the American Orthotic & Prosthetic Association (AOPA) conferences. These events provide valuable insights into the latest research, technologies, and treatment protocols.
Further, I regularly subscribe to and read leading journals in the field, such as the Journal of Orthopaedic Research and Prosthetics and Orthotics International. This keeps me updated on cutting-edge research and clinical trials. I also actively participate in online professional communities and forums, engaging in discussions and knowledge sharing with colleagues across the globe. This constant engagement ensures I’m always on the forefront of advancements and best practices within my profession.
Q 24. How do you handle situations where a patient experiences unexpected complications with their orthotic?
When a patient experiences unexpected complications with their orthotic, my approach is systematic and patient-centered. The first step involves a thorough reassessment of the patient, including a detailed interview about the nature and onset of the problem. I then conduct a physical examination of the patient’s feet, gait, and any areas of concern highlighted by the patient. This might involve observing their gait using video analysis or employing pressure mapping systems to visualize pressure distribution under the foot.
Based on this reassessment, I determine the cause of the complication. It could be due to an ill-fitting orthotic, an unexpected change in the patient’s condition, or even a simple adjustment needed. For example, a patient might experience increased pain due to a too-rigid shell or inadequate cushioning. In such cases, I might modify the orthotic by adjusting the shell’s rigidity, adding more cushioning, or altering the alignment. In more complex situations, I liaise closely with the referring physician or other members of the healthcare team to determine the best course of action, which might include further imaging or referral to a specialist.
Q 25. Describe your experience with working collaboratively with other healthcare professionals (e.g., podiatrists, physical therapists).
Collaborative teamwork is essential in orthotics. I regularly work with podiatrists, physical therapists, and other healthcare professionals to provide comprehensive patient care. For instance, I often collaborate with podiatrists to obtain detailed medical history, diagnoses, and treatment plans before designing orthotics. This ensures the orthotics align perfectly with the overall treatment strategy.
With physical therapists, the collaboration focuses on rehabilitation and functional outcomes. I’ll discuss the patient’s progress and adjust the orthotic design as needed based on their input and the patient’s response to therapy. I always prioritize clear and effective communication, using shared patient portals or regular meetings to ensure that everyone remains informed and works towards the same goal: optimal patient recovery and well-being. This collaborative approach helps to improve patient outcomes and achieve better treatment success.
Q 26. Explain your process for troubleshooting and resolving issues with custom orthotics.
Troubleshooting custom orthotics involves a systematic process. First, I carefully listen to the patient’s description of the problem, noting the exact location, intensity, and timing of any discomfort or functional limitations. I then visually inspect the orthotic for any signs of wear, tear, or structural issues. This might include checking for cracks in the shell, delamination of materials, or misalignment of components.
Next, I conduct a thorough biomechanical evaluation of the patient, often using gait analysis tools to identify any movement compensations or gait abnormalities that may contribute to the problem. This may involve observation of the patient’s gait pattern and pressure mapping to determine if any areas experience excessive pressure. Finally, based on the assessment, I implement corrective measures, which could range from simple adjustments like minor modifications to the orthotic shell or cushioning, to a complete redesign if necessary. Throughout this process, I maintain clear communication with the patient and referring clinician to ensure they are informed and actively participate in the problem-solving process.
Q 27. Describe your experience with selecting and utilizing appropriate tools and equipment for orthotics fabrication.
My experience with orthotics fabrication equipment is extensive. I’m proficient in using various tools and technologies, including vacuum forming machines, milling machines (both computer-numeric control (CNC) and manual), casting materials (plaster, foam), and various finishing tools like grinders, sanders, and heat guns. I am familiar with selecting appropriate materials based on the patient’s needs and the type of orthotic being fabricated, taking into consideration factors like material stiffness, durability, and patient comfort. For instance, for a high-impact orthotic for an athlete, I might choose a more durable and stiffer material, while for a patient with sensitive skin, I would opt for a softer, more comfortable material.
I’m also skilled in using hand tools for precise adjustments and refinements, ensuring a perfect fit and customized support. Safety is always a priority, and I strictly adhere to all safety protocols and regulations when using these tools and equipment. Regular maintenance and calibration of the equipment are essential aspects of my workflow, to ensure accuracy and optimal performance.
Q 28. How do you ensure the quality and accuracy of your orthotic designs and fabrications?
Quality and accuracy are paramount in orthotic design and fabrication. I adhere to strict quality control measures at every stage of the process. This starts with accurate measurements and casting of the patient’s foot. We use precise casting techniques to capture accurate foot shape and avoid potential errors in the final orthotic. I meticulously inspect the 3D model generated by the CAD/CAM software, verifying that it accurately reflects the patient’s foot anatomy and the design specifications. This inspection often involves comparing the digital model to the original cast.
During fabrication, I closely monitor the milling process to ensure that the final orthotic conforms precisely to the digital model. After fabrication, I conduct a thorough quality check of the finished orthotic, examining it for any imperfections, misalignments, or inconsistencies before it’s delivered to the patient. I maintain detailed records of every step of the process, including materials used and any modifications made. This comprehensive approach to quality control ensures that each orthotic is not only functional but also safe, comfortable, and meets the highest standards of quality.
Key Topics to Learn for Orthotics and Custom Foot Support Interview
- Biomechanics of the Foot and Ankle: Understanding gait analysis, pressure distribution, and common foot pathologies (e.g., plantar fasciitis, bunions, pes planus).
- Orthotic Design Principles: Knowledge of materials (e.g., plastics, foams, carbon fiber), fabrication techniques (e.g., casting, molding, CAD/CAM), and design considerations for different pathologies.
- Clinical Assessment and Patient Interaction: Mastering techniques for thorough patient evaluation, including history taking, physical examination, and communication skills to effectively understand patient needs and expectations.
- Custom vs. Pre-fabricated Orthotics: Understanding the indications and contraindications for each type, and the advantages and disadvantages of various materials and designs.
- Practical Application: Ability to explain the process of creating custom orthotics, from initial assessment to final fitting and follow-up care, including adjustments and modifications.
- Problem-solving and Troubleshooting: Demonstrating the ability to identify and address common challenges encountered during orthotic fabrication and fitting, such as pressure points, discomfort, and inadequate support.
- Rehabilitation and Therapeutic Interventions: Understanding the role of orthotics in conjunction with other therapies, such as physical therapy and exercise, to improve patient outcomes.
- Legal and Ethical Considerations: Familiarity with relevant regulations, documentation requirements, and ethical practices within the field.
Next Steps
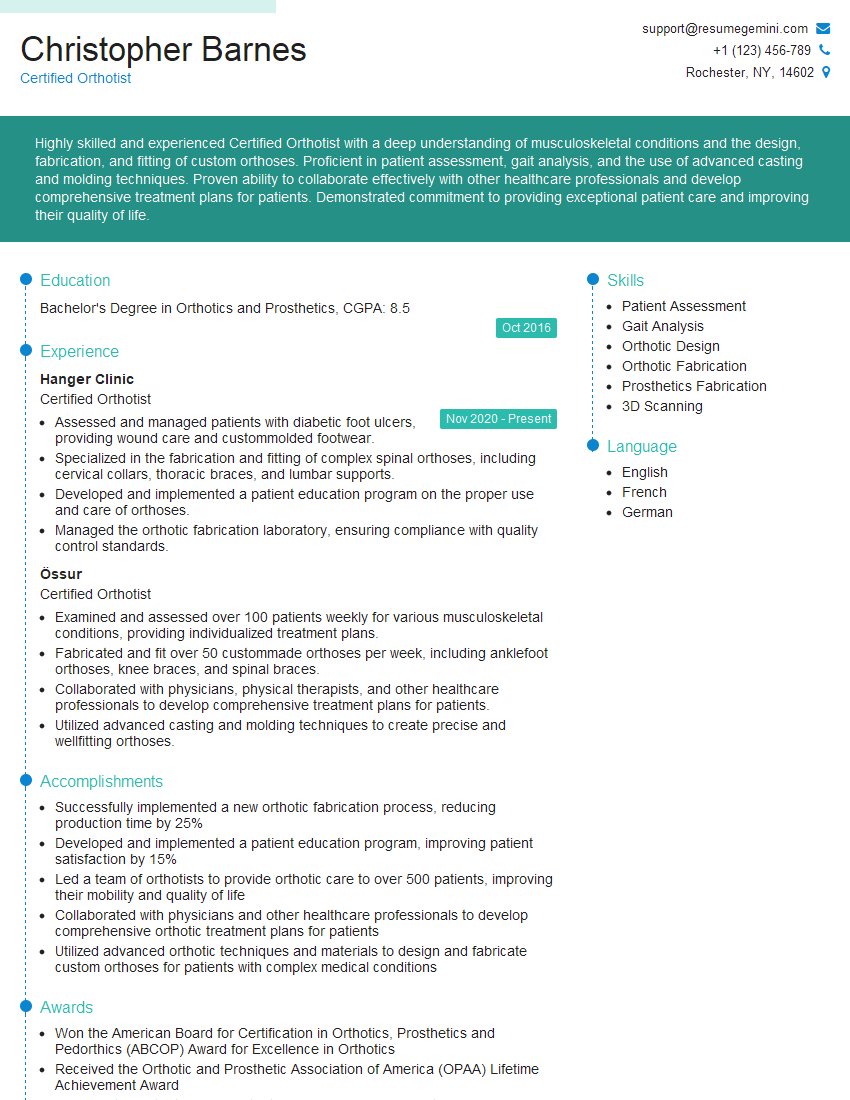
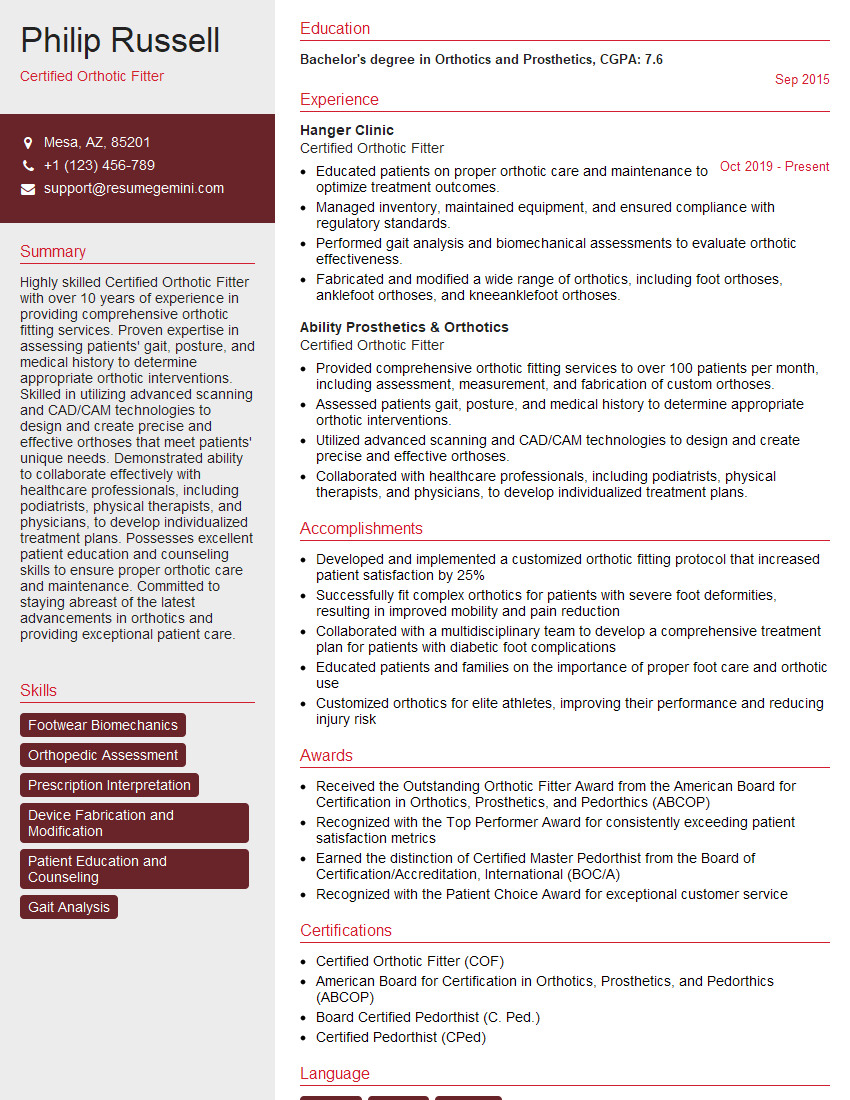
Mastering Orthotics and Custom Foot Support is crucial for a successful and rewarding career. A strong understanding of these principles will significantly enhance your value to any employer and open doors to diverse and challenging opportunities. To maximize your job prospects, it’s vital to present your skills and experience effectively. Creating an ATS-friendly resume is essential for getting your application noticed by potential employers. ResumeGemini is a trusted resource to help you build a professional and impactful resume, tailored to highlight your qualifications. Examples of resumes specifically designed for Orthotics and Custom Foot Support professionals are available through ResumeGemini, helping you stand out from the competition.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.