Unlock your full potential by mastering the most common Management of Charcot Foot interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Management of Charcot Foot Interview
Q 1. Describe the pathophysiology of Charcot foot.
Charcot foot, also known as neuropathic arthropathy, is a devastating complication primarily affecting individuals with diabetes mellitus and peripheral neuropathy. Its pathophysiology is complex and involves a cascade of events. It begins with loss of protective sensation in the foot due to neuropathy, making patients unaware of injuries. This lack of sensation leads to repeated micro-trauma which goes unnoticed and untreated. The repeated trauma triggers an inflammatory response, characterized by increased blood flow and bone resorption. This leads to the characteristic bone destruction and deformity seen in Charcot foot. Essentially, it’s a process where the body tries to ‘repair’ the repeated micro-injuries inefficiently due to a lack of sensory feedback, resulting in significant bone damage and joint instability. Think of it like repeatedly hitting your knee without realizing it – the inflammation and bone remodeling become destructive instead of reparative.
Q 2. What are the common clinical presentations of Charcot foot?
The clinical presentation of Charcot foot is highly variable but typically progresses through stages. Early stages may present with subtle findings like erythema (redness), edema (swelling), and warmth in the foot. As the condition progresses, significant deformity develops. This can involve joint destruction and instability, leading to rocker-bottom foot, pes cavus (high arch), or valgus/varus deformities (foot turning inward or outward). Patients may experience pain, although this can be inconsistent due to neuropathy. Significant swelling and warmth often persist. Advanced stages manifest with severe deformities, ulceration, and potential for infection, leading to significant functional limitations and risk of amputation.
Imagine a foot that’s become misshapen and unstable, sometimes red and swollen, with a possible open wound. This demonstrates the severity of the condition and the importance of early intervention.
Q 3. Explain the diagnostic methods used to identify Charcot foot.
Diagnosing Charcot foot requires a comprehensive approach combining clinical findings with imaging studies. A detailed history focusing on diabetes, neuropathy, and recent foot trauma is crucial. The physical exam should assess for the characteristic signs mentioned earlier – redness, swelling, warmth, and deformity. However, relying solely on clinical findings can be unreliable due to the variable presentation. Therefore, imaging plays a critical role.
Q 4. Detail the initial management of a suspected Charcot foot case.
Initial management of suspected Charcot foot hinges on immediate offloading to reduce stress on the affected foot and prevent further damage. This typically involves total contact casts (TCC) or specialized offloading footwear. Non-weight bearing is often necessary. Strict glycemic control is paramount for diabetic patients, as hyperglycemia exacerbates the inflammatory process. Careful assessment for infection is crucial, as this is a frequent complication. Analgesics may be used to manage pain. Close monitoring of the foot for any changes is essential. Early referral to a multidisciplinary team including podiatrists, orthopedists, and endocrinologists is highly recommended.
Think of a TCC as a protective cocoon for the foot, allowing it to heal undisturbed. This is a critical first step.
Q 5. How would you differentiate Charcot foot from other foot conditions?
Differentiating Charcot foot from other foot conditions, such as cellulitis, osteomyelitis, or trauma, can be challenging. Clinical presentation can overlap. However, the combination of neuropathy, the presence of characteristic bone changes on imaging (as seen on X-rays), and the often-rapid progression of deformity sets Charcot foot apart. Cellulitis would primarily show soft tissue infection, while osteomyelitis would typically present with localized bone infection but less diffuse bone changes. Trauma would have a clearer history of injury. Imaging studies are crucial for definitive diagnosis.
Q 6. What imaging modalities are essential in Charcot foot diagnosis?
Plain radiographs (X-rays) are essential for assessing bone changes. Early findings may be subtle, with increased density or fragmentation. Later on, severe bone destruction and joint dislocation are evident. Bone scans using technetium-99m can demonstrate increased bone turnover, confirming the active inflammatory process. MRI is useful for evaluating soft tissues and for detecting early changes not seen on X-rays. While CT scans can provide detailed bone anatomy, it’s usually reserved for specific situations.
Q 7. Describe the role of offloading in Charcot foot treatment.
Offloading is the cornerstone of Charcot foot treatment. It aims to eliminate weight-bearing stress on the affected foot, allowing the bones to heal and preventing further deformity. Methods include total contact casts (TCCs), custom-molded shoes, crutches, or wheelchairs. The duration of offloading depends on the severity of the disease and the patient’s response to treatment. Proper offloading is essential to prevent further destruction and promote healing. The goal is to provide complete immobilization and protect the injured structures until the inflammatory process subsides and bone healing commences. Careful monitoring is needed to ensure the offloading device remains effective.
Q 8. Explain different types of offloading techniques.
Offloading in Charcot foot aims to relieve pressure from the affected area, preventing further deformity and promoting healing. This is crucial because the neuropathic nature of Charcot foot means patients often don’t feel pain, leading to continued weight-bearing on already damaged bones and joints. Techniques vary depending on the severity and location of the deformity.
- Total Contact Casts (TCCs): These are custom-made casts that distribute pressure evenly across the entire plantar surface of the foot, providing excellent offloading. They’re often the first-line treatment for acute Charcot foot.
- Custom-Molded Shoes and Inserts: These provide targeted pressure relief, accommodating specific foot deformities. They are particularly helpful in the chronic stage or after cast removal for continued support.
- Knee-High Casts (or Below-Knee Casts): These immobilize the entire foot and ankle, preventing movement that could exacerbate the damage. Often used in severe cases or during the acute inflammatory phase.
- Removable Walker Boots: Offer more mobility than casts but still provide significant offloading and support. Useful for the transition phase between cast immobilization and weight-bearing.
- Crutches or Wheelchairs: Non-weight-bearing options are sometimes necessary, especially in the acute phase, to completely eliminate stress on the affected foot.
Choosing the right offloading method depends on individual factors such as the severity of the Charcot arthropathy, the patient’s mobility, and the presence of any concomitant conditions. Regular monitoring and adjustments are essential to ensure optimal offloading and prevent complications.
Q 9. What are the indications for surgical intervention in Charcot foot?
Surgical intervention in Charcot foot is usually reserved for cases that haven’t responded to conservative management, specifically offloading and medical treatment. Indications include:
- Severe Deformity: When significant structural changes cause significant pain, impaired mobility, or risk of ulceration despite optimal offloading.
- Non-Union Fractures: Fractures that fail to heal despite appropriate treatment, leading to instability and pain.
- Recurring Ulcers and Infections: Persistent ulcers or infections that don’t heal despite aggressive local wound care and antibiotics. Surgical debridement may be necessary.
- Progressively worsening Pain: Pain that significantly impacts the patient’s quality of life and doesn’t improve with conservative methods.
- Mechanical Instability: When the foot’s structural integrity is compromised, leading to potential collapse and further damage.
The decision to proceed with surgery should be carefully weighed, considering the risks and potential benefits in the context of the patient’s overall health and functional goals. It’s important to remember that surgery is not a cure-all and often needs to be combined with continued offloading and meticulous wound care.
Q 10. Describe various surgical procedures used in Charcot foot management.
Surgical procedures for Charcot foot are complex and aimed at stabilizing the foot, correcting deformities, and improving functionality. Common procedures include:
- Arthrodesis (Fusion): This involves surgically fusing one or more joints in the foot to provide stability. This is a common procedure, especially for midfoot arthrodesis to correct deformity and prevent collapse.
- Osteotomy: This involves reshaping or realigning bones to correct deformities. This is often used in conjunction with arthrodesis for optimal correction.
- Debridement: This procedure involves removing infected or necrotic tissue to promote healing. Often necessary in cases of ulceration and infection.
- External Fixation: This uses external pins and rods to stabilize fractures and correct deformities. It is particularly useful in situations where internal fixation isn’t feasible.
- Soft Tissue Procedures: These may involve tendon transfers or releases to improve alignment and function.
- Amputation: In severe cases, where conservative and surgical management fail, amputation may be considered as a last resort to prevent further complications and improve the patient’s quality of life.
The specific procedure chosen will depend on the individual’s foot anatomy, the extent and location of the damage, and the overall health of the patient. Post-operative care, including continued offloading and physiotherapy, is crucial for a successful outcome.
Q 11. What are the potential complications of Charcot foot?
Charcot foot, if not managed appropriately, can lead to several serious complications:
- Progressively worsening deformity: Leading to rocker-bottom foot, severe instability and gait disturbances.
- Recurring ulcers and infections: Due to impaired sensation and compromised blood supply, these can be difficult to treat and potentially lead to osteomyelitis (bone infection).
- Amputation: In cases of severe infection, intractable pain, or failure of other treatments, amputation may be necessary.
- Osteomyelitis (bone infection): A serious infection of the bone that can lead to sepsis (bloodstream infection).
- Joint destruction: Leading to instability and pain.
- Pain: While initially painless due to neuropathy, chronic Charcot foot can become extremely painful due to secondary changes such as inflammation, ulceration, and deformity.
- Reduced mobility and quality of life: The chronic pain and deformity can lead to significant limitations in mobility and daily activities.
Careful management, including diligent offloading, prompt treatment of infections, and regular monitoring, is essential to minimize these risks.
Q 12. How do you manage infections associated with Charcot foot?
Managing infections in Charcot foot requires a multi-pronged approach focusing on prompt diagnosis, aggressive treatment, and prevention of recurrence. The first step is to identify and culture the causative organism to guide antibiotic selection. This might involve wound swabs and possibly bone biopsy.
- Debridement: Surgical removal of infected or necrotic tissue is often crucial. It helps to eliminate the source of infection and allows for better penetration of antibiotics.
- Antibiotic Therapy: This is guided by culture results and usually involves intravenous antibiotics initially. The choice of antibiotic depends on the infecting organism and its sensitivity profile. Duration of therapy needs to be tailored to the response.
- Wound Care: Regular cleaning and dressing changes are essential to prevent further infection and promote healing. This often involves advanced wound care techniques such as negative pressure wound therapy (NPWT).
- Offloading: Continued and effective offloading remains crucial even during treatment of infection to promote healing and prevent re-injury.
- Hyperbaric Oxygen Therapy (HBOT): May be considered in certain situations, particularly for chronic osteomyelitis, to improve tissue oxygenation and enhance healing.
Regular monitoring of the patient’s clinical status and inflammatory markers is necessary to assess the effectiveness of treatment and adjust the approach as needed. Prompt management of infections is vital to prevent serious complications such as sepsis and the need for amputation.
Q 13. Discuss the role of antibiotics in Charcot foot management.
Antibiotics play a vital role in managing infections associated with Charcot foot, particularly osteomyelitis. However, their use must be judicious and guided by microbiological findings whenever possible.
- Empirical Therapy: Before culture results are available, broad-spectrum antibiotics may be started to cover likely pathogens based on local epidemiology.
- Targeted Therapy: Once culture and sensitivity results are available, antibiotics should be tailored to the specific organism and its susceptibility pattern. This is essential for optimal efficacy and minimizing the risk of antibiotic resistance.
- Duration of Therapy: The duration of antibiotic treatment depends on several factors, including the severity of infection, the response to therapy, and the presence of any underlying conditions. It’s often prolonged, sometimes lasting several weeks or even months in severe osteomyelitis.
- Route of Administration: Initially, intravenous antibiotics are typically preferred for severe infections to ensure adequate drug levels. Once the infection is controlled, oral antibiotics may be used if appropriate.
- Combination Therapy: In some cases, combination therapy using multiple antibiotics may be necessary, especially for polymicrobial infections or severe osteomyelitis.
It’s critical to emphasize that antibiotics alone are insufficient. They must be integrated with other crucial management strategies such as surgical debridement, wound care, and offloading to achieve successful infection control and prevent recurrence.
Q 14. What are the long-term management strategies for Charcot foot?
Long-term management of Charcot foot aims to prevent further deformity, protect the foot from injury, and maintain mobility and quality of life. This requires a multidisciplinary approach involving podiatrists, orthotists, and other healthcare professionals.
- Regular Monitoring: Close monitoring for any signs of recurrence, such as increasing pain, swelling, or redness, is vital. Regular foot exams are essential.
- Continued Offloading: Even after the acute phase, continued pressure relief is often necessary. This might involve custom-made shoes, inserts, or other assistive devices.
- Wound Care: Careful management of any existing wounds or ulcers is crucial to prevent infection and promote healing.
- Diabetes Management (if applicable): For patients with diabetes, maintaining optimal glycemic control is critical to prevent recurrence and complications.
- Physiotherapy: Regular physiotherapy may help to improve range of motion, strength, and function. Exercises are tailored to the patient’s specific needs and level of mobility.
- Patient Education: Patient education is vital. Patients need to be well-informed about their condition, management strategies, and how to recognize warning signs of recurrence.
- Regular Follow-up: Regular follow-up appointments with the healthcare team are essential to monitor progress, assess for complications, and make necessary adjustments to the management plan.
Long-term management of Charcot foot is a marathon, not a sprint. It requires dedication, collaboration, and continuous vigilance to ensure the patient maintains a reasonable quality of life.
Q 15. How do you assess the success of Charcot foot treatment?
Assessing the success of Charcot foot treatment is multifaceted and depends on several factors. We don’t just look at the absence of pain; we consider the overall functional outcome and prevention of future complications. A successful outcome involves achieving ulcer healing, preventing infection, minimizing deformity, and restoring as much mobility and function as possible. This is often assessed through clinical examination, imaging (X-rays, MRI), patient-reported outcome measures (like the Foot Function Index), and monitoring for recurrence.
For example, a successful outcome might be seen in a patient who presented with a severely deformed foot and an ulcer, but after treatment, healed the ulcer, experienced a reduction in pain, and regained the ability to ambulate with minimal assistance using appropriate footwear. Conversely, continued deformity, recurrent ulcers, or persistent pain despite treatment would indicate a less successful outcome.
Career Expert Tips:
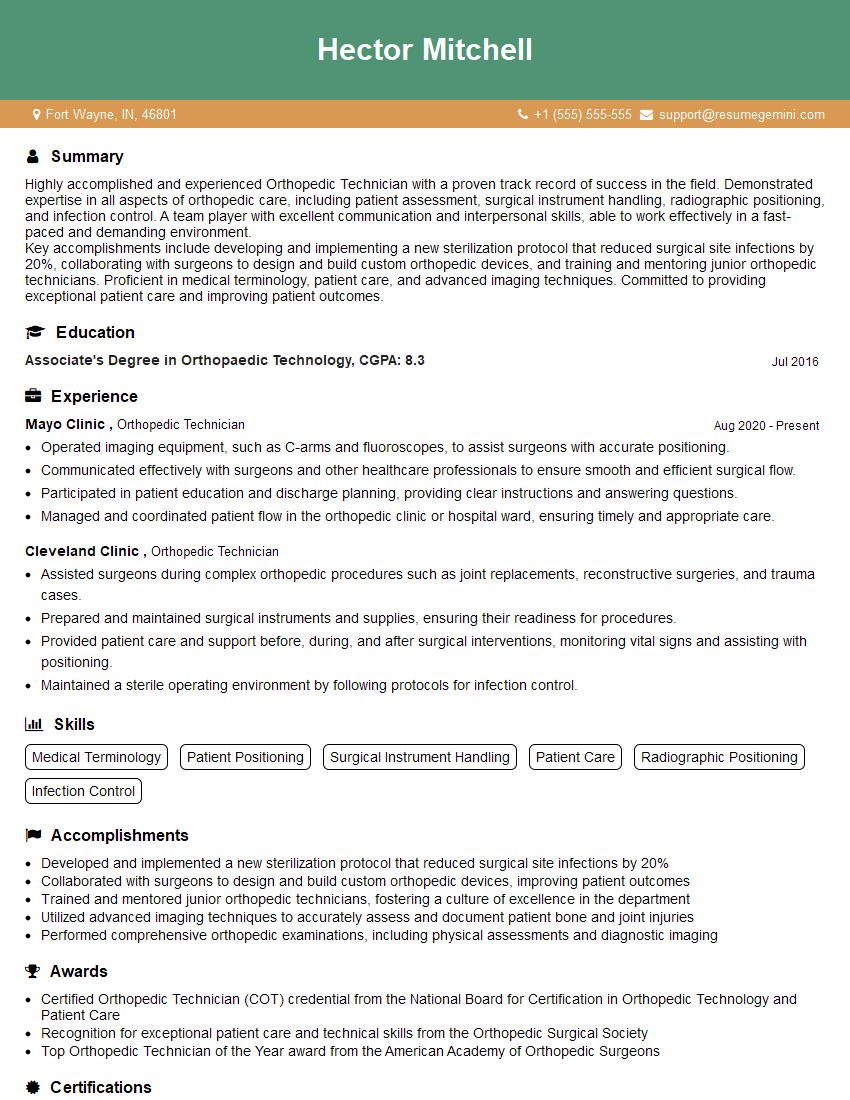
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain the role of patient education in managing Charcot foot.
Patient education is paramount in Charcot foot management. It’s the cornerstone of preventing recurrence. Patients need to understand the condition, its risks, and their role in managing it. This includes detailed explanations about the disease process, the importance of meticulous foot care (regular inspection, proper hygiene, avoiding trauma), and the adherence to prescribed treatment protocols.
- Understanding the condition: Patients should understand that Charcot foot is a serious complication of diabetes and neuropathy, leading to bone destruction and deformity.
- Foot care: Daily foot inspection, proper hygiene, and the use of appropriate footwear are crucial to prevent further injury.
- Medication adherence: Patients must understand the importance of adhering to their prescribed medication regimen, including any pain management, antibiotics, or medications for glycemic control.
- Offloading: The importance of offloading pressure from the affected area through specialized footwear, crutches, or other devices must be emphasized.
Think of it like this: giving a patient a detailed instruction manual for their foot’s ‘care and maintenance.’ Without this understanding, even the best medical intervention might be undermined by poor patient compliance.
Q 17. Describe the importance of multidisciplinary care in Charcot foot management.
Multidisciplinary care is essential for optimal Charcot foot management. No single specialist can address all the complexities of this condition. A successful treatment plan requires a coordinated effort between various healthcare professionals.
- Endocrinologist: To manage diabetes and optimize glycemic control.
- Podiatrist: For specialized foot care, wound management, and custom orthotics.
- Orthopedic surgeon: May be involved in surgical intervention for severe deformities or non-healing wounds.
- Infectious disease specialist: To manage infections, which are a common and serious complication.
- Physical therapist: For rehabilitation, improving mobility, and strengthening exercises.
- Diabetic educator: To provide comprehensive education about diabetes management.
For example, if a patient develops an infection, the podiatrist would manage the wound, while the infectious disease specialist would prescribe appropriate antibiotics. The coordinated efforts of this team increase the chances of achieving a successful outcome.
Q 18. How do you involve the patient and their family in the treatment plan?
Involving the patient and their family is crucial for successful management. This requires open communication and shared decision-making. We need to empower the patient to actively participate in their care.
- Shared decision-making: We explain treatment options, risks, and benefits, allowing patients to choose the approach that best fits their preferences and lifestyle.
- Education and support: We provide comprehensive education and resources to the patient and their family, ensuring they understand the disease process, treatment plan, and potential complications.
- Family involvement: The family plays a crucial role in supporting the patient’s adherence to the treatment plan and in monitoring for any warning signs.
- Regular follow-up: Regular follow-up appointments provide an opportunity to assess progress, address concerns, and adjust the treatment plan as needed.
Imagine a scenario where a patient struggles with self-care due to vision impairment. Involving their family allows for assistance with daily foot care, ensuring the patient adheres to the prescribed regimen.
Q 19. What are the risk factors for developing Charcot foot?
Several factors increase the risk of developing Charcot foot. The most significant risk factor is diabetes, particularly poorly controlled diabetes with peripheral neuropathy. Other contributing factors include:
- Peripheral neuropathy: Loss of sensation in the feet makes it difficult to detect injuries and protect the feet from further damage.
- Poor glycemic control: High blood sugar levels contribute to nerve damage and impaired immune function, increasing susceptibility to infections.
- Vascular disease: Reduced blood flow to the feet impairs healing and increases the risk of infections.
- History of previous Charcot arthropathy: Patients with a history of Charcot foot in one foot are at higher risk of developing it in the other foot.
- Alcohol abuse: Can contribute to peripheral neuropathy and worsen diabetic control.
- Certain medications: Some medications can affect blood flow or nerve function.
For instance, a patient with long-standing, poorly managed diabetes and significant peripheral neuropathy is at considerably higher risk than someone with well-controlled diabetes and normal sensation.
Q 20. Describe the role of glycemic control in preventing Charcot foot.
Glycemic control plays a vital role in preventing Charcot foot. Maintaining optimal blood sugar levels is crucial for protecting nerves and blood vessels in the feet. Poorly controlled diabetes leads to neuropathy and vascular disease, both of which are major risk factors for Charcot foot.
Tight glycemic control, achieved through lifestyle modifications (diet, exercise) and medication (insulin, oral hypoglycemics) as needed, can significantly reduce the risk. Regular monitoring of blood glucose levels, HbA1c tests, and assessment of neuropathy are essential. The goal is to keep blood sugar levels within the target range recommended by the patient’s healthcare provider to minimize the risk of complications like Charcot foot.
Consider it like this: blood sugar is fuel for the body. Too much fuel (hyperglycemia) damages the engine (nerves and blood vessels). Maintaining optimal fuel levels protects the engine from damage and decreases the risk of breakdown (Charcot foot).
Q 21. What are the common causes of Charcot foot recurrence?
Charcot foot recurrence can be a significant challenge. Several factors contribute to this:
- Inadequate offloading: Failure to adequately protect the foot from weight-bearing stress after the initial episode is a major cause of recurrence.
- Poor glycemic control: Persistent hyperglycemia continues to damage nerves and blood vessels, increasing vulnerability.
- Non-compliance with foot care instructions: Neglecting foot hygiene, ignoring minor injuries, or wearing inappropriate footwear can lead to recurrence.
- Underlying vascular disease: Impaired blood flow to the foot hinders healing and increases the risk of infections.
- Continued peripheral neuropathy: Loss of sensation prevents early detection of injuries and increases the risk of repeated trauma.
For instance, a patient who doesn’t consistently wear their prescribed offloading footwear after an initial episode might experience a recurrence due to repeated stress on the affected area. Careful attention to all of these factors is crucial in preventing a recurrence.
Q 22. How would you prevent Charcot foot recurrence?
Preventing Charcot foot recurrence hinges on meticulous management of the underlying condition, typically diabetes. This is a multi-faceted approach focusing on tight glycemic control, regular foot exams, and proactive management of neuropathy and vascular disease.
- Optimal Glucose Control: Maintaining HbA1c levels below 7% is crucial in reducing the risk of neuroischemic damage that predisposes to Charcot foot. We work closely with endocrinologists to achieve this.
- Neuropathy Management: Addressing diabetic neuropathy through medication and lifestyle changes (e.g., avoiding barefoot walking) is critical. Pain is often absent in the early stages of Charcot foot, and this makes neuropathy management particularly vital.
- Vascular Assessment and Management: Regular assessments of peripheral arterial disease (PAD) are essential. We might employ ankle-brachial index (ABI) measurements and, if necessary, refer patients for vascular surgery or interventional radiology to improve blood flow.
- Offloading and Protective Footwear: Even after the acute phase, custom-made footwear or offloading devices remain critical to prevent weight-bearing stress on affected areas and minimize recurrence. This might involve specialized shoes, inserts, or crutches.
- Patient Education: Educating patients about self-foot care, including daily inspection, proper footwear, and immediate attention to any foot injury, is paramount in preventing recurrence.
Think of it like this: we’re not just treating the broken bone (the Charcot foot itself), we’re addressing the underlying disease process to prevent future breaks. It’s a holistic approach to patient care.
Q 23. What are the most common complications following Charcot foot surgery?
Complications following Charcot foot surgery are unfortunately common and can be serious. They include:
- Infection: Surgical sites are vulnerable, especially in patients with compromised immunity. We use prophylactic antibiotics and rigorous sterile techniques to minimize this risk.
- Nonunion: The fracture may not heal properly, requiring further surgery, such as bone grafting or external fixation.
- Malunion: The bone may heal in an incorrect position, leading to deformity and functional impairment. Careful postoperative casting and bracing are crucial to prevent this.
- Delayed Wound Healing: Especially in diabetic patients with poor circulation, wound healing can be significantly delayed, increasing the risk of infection.
- Hardware Complications: If implants are used, there’s a risk of loosening, breakage, or infection of the hardware, necessitating revision surgery.
- Recurrence of Charcot Arthropathy: Even with surgery, the underlying disease process continues, and recurrence is possible if the underlying diabetes and neuropathy are not well managed.
Managing these complications requires a multidisciplinary approach involving surgeons, infectious disease specialists, podiatrists, and diabetes care teams. Postoperative monitoring is rigorous, and we adjust treatment plans as needed to optimize outcomes.
Q 24. What are the challenges associated with treating Charcot foot in specific patient populations (e.g., elderly, diabetics with comorbidities)?
Treating Charcot foot in specific populations presents unique challenges:
- Elderly Patients: They often have reduced bone healing capacity and increased fragility, making surgical interventions more risky. Non-surgical approaches might be prioritized, emphasizing offloading and meticulous wound care. We also need to consider their overall health and functional status when deciding on a treatment strategy.
- Diabetics with Comorbidities: Patients with cardiovascular disease, renal failure, or neuropathy pose significant challenges. These comorbidities increase surgical risk and impair healing. We need to carefully balance the benefits and risks of different treatments and frequently involve specialists in cardiology, nephrology, and pain management.
For example, an elderly patient with severe cardiovascular disease might benefit more from a conservative approach focused on offloading and meticulous wound care, avoiding the added stress of surgery. Conversely, a younger, healthier patient might be a good candidate for surgical intervention to correct severe deformity.
Q 25. What is the role of Total Contact Cast (TCC) in Charcot foot management?
The Total Contact Cast (TCC) is a cornerstone of non-surgical Charcot foot management. It’s a custom-made cast that distributes weight evenly across the entire plantar surface of the foot, thereby minimizing stress on the affected areas and promoting healing.
- Offloading: The key function is to provide complete offloading of the affected joints, reducing inflammation and promoting healing.
- Immobilization: The cast immobilizes the foot and ankle, preventing further damage from weight-bearing and movement.
- Early Intervention: TCC is typically applied early in the course of Charcot arthropathy, ideally within the first few weeks of symptom onset, preventing severe deformities.
- Monitoring: The TCC allows for regular monitoring of the foot, allowing for early detection of any complications like pressure sores or infections.
Think of a TCC as a protective ‘hug’ for the injured foot, preventing further damage and allowing the underlying bones to heal. It’s a crucial tool in the arsenal of Charcot foot management.
Q 26. Compare and contrast different types of footwear suitable for Charcot foot patients.
Footwear choices for Charcot foot patients are crucial for long-term management. The goal is to distribute pressure evenly and protect the foot from further injury. Options include:
- Custom-Molded Shoes: These shoes are made to the exact specifications of the patient’s foot, accommodating any deformities and providing optimal pressure distribution. They’re usually the gold standard for long-term management.
- Extra-Depth Shoes: These provide ample space to accommodate foot swelling and deformities, offering better comfort and protection than standard shoes.
- Diabetic Shoes: While not always appropriate for all Charcot foot patients, they offer extra cushioning and support that can improve comfort and help offload weight, particularly if the patient also has diabetes.
- Orthoses (Insoles): Custom or prefabricated orthoses can be used in conjunction with shoes to provide additional support and offloading. They can be particularly helpful for managing localized pressure points.
The choice depends on the severity of the deformity, the patient’s activity level, and their overall foot health. For severe deformities, custom-molded shoes are often necessary, while for milder cases, extra-depth shoes or well-fitted shoes with orthoses might suffice.
Q 27. How do you monitor the progress of a patient with Charcot foot?
Monitoring Charcot foot progress requires a multi-pronged approach. We use a combination of clinical exams, imaging, and patient-reported outcomes.
- Clinical Examination: This includes assessing swelling, redness, warmth, pain, and range of motion. We look for any signs of infection or worsening deformity.
- Radiographic Imaging: Serial X-rays are crucial for monitoring fracture healing, joint destruction, and assessing the effectiveness of treatment. We look for changes in bone density, alignment, and joint space.
- Weight-Bearing Status: We monitor the patient’s ability to bear weight and their progress towards regaining weight-bearing capacity. This may involve using scales or gait analysis.
- Patient-Reported Outcomes: We assess the patient’s pain levels, functional ability (e.g., walking distance), and overall quality of life. Standard questionnaires can help track these changes over time.
By combining these methods, we obtain a holistic picture of the patient’s progress and adjust treatment as needed. Regular follow-up appointments are crucial to ensure early detection of complications and optimize outcomes.
Q 28. Describe a case scenario where you had to manage a complicated case of Charcot foot and explain your approach.
I recall a patient, a 68-year-old male with poorly controlled type 2 diabetes and peripheral neuropathy who presented with a severe Charcot midfoot deformity. He had significant inflammation, swelling, and pain. Initial X-rays showed extensive bone destruction and joint dislocation.
My approach was multi-faceted:
- Immediate Offloading: We initiated total contact casting (TCC) to completely offload the affected foot, reducing inflammation and preventing further damage.
- Intensive Glycemic Control: We collaborated with the endocrinology team to optimize his blood sugar control, aiming for an HbA1c below 7%.
- Infection Control: Given his diabetic neuropathy, we closely monitored him for any signs of infection, and administered prophylactic antibiotics.
- Surgical Intervention: After several weeks of non-surgical management, the inflammation subsided, but the severe deformity persisted. We then proceeded with corrective osteotomy and arthrodesis to stabilize the foot and correct the deformity. The surgical approach was tailored to preserve as much of the foot as possible while ensuring stability.
- Post-Operative Management: He was placed in a post-operative cast and then progressed to a custom-made orthosis for long-term management. We continued to monitor for complications, adjust medications as needed, and emphasize regular blood glucose monitoring and foot care.
This case highlighted the importance of a multidisciplinary approach and the need to balance aggressive early intervention with careful consideration of the patient’s overall health status and comorbidities. Long-term follow-up is essential to monitor for complications and ensure adherence to the treatment plan, preventing recurrence.
Key Topics to Learn for Management of Charcot Foot Interview
- Pathophysiology of Charcot Foot: Understand the underlying mechanisms of bone destruction, joint instability, and soft tissue involvement in Charcot neuroarthropathy. Consider the role of neuropathy and vascular compromise.
- Clinical Presentation and Diagnosis: Be prepared to discuss the typical signs and symptoms, diagnostic imaging (X-ray, MRI, CT), and the importance of early detection and differentiation from other foot pathologies.
- Non-surgical Management: Detail your knowledge of offloading techniques (e.g., total contact casts, custom-molded footwear), wound care protocols, and the management of infection. Include practical considerations like patient education and compliance.
- Surgical Management: Discuss the indications, techniques, and potential complications of surgical interventions such as arthrodesis, osteotomy, and amputation. Explain your decision-making process in selecting appropriate surgical approaches.
- Rehabilitation and Prognosis: Outline the importance of physical therapy, bracing, and patient education in long-term management. Understand factors influencing patient outcomes and the potential for recurrence.
- Complications and their Management: Be ready to discuss common complications such as infection, ulceration, non-union, and amputation. Explain how you would manage these scenarios effectively.
- Multidisciplinary Approach: Highlight the collaborative nature of Charcot foot management, including the roles of podiatrists, endocrinologists, vascular surgeons, and other specialists. Explain your experience and understanding of team-based care.
Next Steps
Mastering the management of Charcot foot significantly enhances your career prospects in podiatry, orthopedics, and related fields. It demonstrates a high level of specialized knowledge and expertise, making you a highly desirable candidate. To further strengthen your job application, create an ATS-friendly resume that highlights your relevant skills and experience. ResumeGemini is a trusted resource for building professional resumes, and we provide examples of resumes tailored to Management of Charcot Foot to help you showcase your qualifications effectively. Investing time in crafting a strong resume will significantly increase your chances of securing your dream position.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.