Cracking a skill-specific interview, like one for Skin and Plantar Fascia Grafting, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Skin and Plantar Fascia Grafting Interview
Q 1. Describe the different types of skin grafts used in reconstructive surgery.
Skin grafts are categorized primarily by the depth of skin harvested. The most common types used in reconstructive surgery include:
- Split-thickness skin grafts (STSG): These grafts involve harvesting only the epidermis and a portion of the dermis. They are thinner, easier to harvest in larger quantities, and heal faster than full-thickness grafts, but they can result in a less aesthetically pleasing outcome.
- Full-thickness skin grafts (FTSG): These grafts include the entire epidermis and dermis. They provide superior cosmetic results, with better color and texture match, but the donor site requires more extensive healing, and the quantity of harvestable graft is limited. FTSGs are often used in areas requiring optimal cosmetic outcomes, such as the face.
- Mesh skin grafts: A variation of STSGs, where the graft is expanded by making incisions in the graft’s surface to increase its surface area. This is useful for covering larger wounds, but it results in a more noticeable scar.
- Composite grafts: These are thicker grafts including epidermis, dermis and even deeper subcutaneous tissues. They are used to replace areas of skin that have more complex structures that are necessary for successful reconstruction (eg. areas that have cartilage and other connective tissues).
The choice of graft depends on several factors, including the size and location of the wound, the patient’s overall health, and the desired cosmetic outcome. For example, a small burn wound on the arm might be treated with an STSG, while a significant facial injury would likely require an FTSG for better aesthetic results.
Q 2. Explain the process of harvesting a split-thickness skin graft.
Harvesting a split-thickness skin graft is a meticulous procedure performed under sterile conditions. The process typically involves:
- Preparation: The donor site, usually a thigh or buttock, is carefully cleaned and prepped. Anesthesia, either local or general, is administered.
- Dermatome use: A dermatome, a specialized instrument, is used to shave the skin to the desired thickness (typically 0.012-0.018 inches). The dermatome’s blade is carefully controlled to ensure an even, consistent thickness of the graft is harvested.
- Graft mesher (if necessary): For larger wounds, a graft mesher might be used to expand the surface area of the harvested graft.
- Graft harvesting: The harvested graft is carefully removed from the donor site and immediately placed on a gauze soaked in sterile saline solution to keep it moist and prevent dehydration.
- Donor Site Management: The donor site is then treated with a pressure dressing and closed with sutures or staples, depending on the depth and size of the harvested tissue.
Throughout the procedure, meticulous attention is paid to prevent damage to the graft and ensure proper hemostasis (control of bleeding) at the donor site.
Q 3. What are the contraindications for skin grafting?
Several factors can contraindicate skin grafting. These include:
- Severe infection: Active infection at the recipient or donor site prevents successful healing and increases the risk of complications.
- Inadequate vascular supply: The recipient site must have sufficient blood flow to support graft survival. Poor blood circulation compromises the graft’s ability to heal.
- Significant nutritional deficiencies: Proper nutrition is crucial for wound healing. Malnutrition can significantly impair healing and increase complications.
- Uncontrolled bleeding: Active bleeding at the recipient site makes it impossible to achieve a secure graft adherence.
- Immunosuppression: Patients with weakened immune systems are at higher risk of infection and graft rejection.
- Certain medications: Some medications can interfere with wound healing, increasing the risk of complications.
A thorough preoperative evaluation is crucial to identify any contraindications and optimize the patient’s chances of a successful outcome. For example, if a patient has a severe infection, treatment of that infection would be required before a skin graft could be attempted. Similarly, if the patient is malnourished, nutritional support would be given to improve their overall health prior to surgery.
Q 4. How do you assess the viability of a skin graft post-operation?
Assessing the viability of a skin graft post-operation is crucial for successful healing. Several methods are used:
- Clinical observation: The graft’s color, texture and capillary refill are observed. A healthy graft typically appears pink and well-perfused within a few days post-operatively.
- Palpation: Gently touching the graft to assess its firmness and adherence. A well-integrated graft will feel firmly attached to the underlying tissue.
- Doppler ultrasound: This technique can assess the blood flow in the graft and detect areas of compromised perfusion. This is a more objective assessment than clinical observation.
- Biopsy: In cases of uncertain graft viability, a biopsy can be performed to assess the graft’s cellularity and signs of necrosis (tissue death).
Early detection of graft failure allows for timely intervention, potentially preventing complete graft loss. For example, if a section of the graft shows signs of necrosis, surgical debridement (removal of dead tissue) and potential re-grafting might be necessary.
Q 5. What are the common complications associated with skin grafting?
Skin grafting, while a valuable reconstructive procedure, carries several potential complications:
- Graft failure: This is the most significant complication, often resulting from infection, inadequate blood supply, or hematoma formation.
- Infection: Infection can delay healing, compromise graft viability, and lead to significant morbidity.
- Hematoma: A collection of blood under the graft can compromise blood supply and lead to failure.
- Serosanguinous drainage: Excessive fluid collection under the graft can lift the graft and impair healing.
- Hypertrophic scarring: Excessive scar formation at the recipient or donor site is common but can be managed.
- Contractures: Scar tissue can contract, leading to functional limitations particularly after burns.
- Donor site complications: These can include infection, hematoma, dehiscence (wound opening), and hypertrophic scarring at the donor site.
Careful postoperative care, including diligent wound monitoring, appropriate dressing changes and prompt management of complications are crucial to minimize risks.
Q 6. Discuss the management of donor site complications.
Management of donor site complications depends on the specific problem encountered.
- Infection: Treatment involves wound debridement, intravenous antibiotics, and possibly surgical drainage.
- Hematoma: Small hematomas may resolve spontaneously, while larger ones might require surgical evacuation.
- Dehiscence: Wound opening requires wound closure, often with sutures or skin grafts.
- Hypertrophic scarring: Treatment can involve pressure dressings, silicone sheeting, or steroid injections to minimize scarring.
- Pain management: Analgesics (pain relievers) are used to manage post-operative discomfort at the donor site.
Early recognition and prompt management of complications are essential to minimize their impact on healing and prevent long-term sequelae. For instance, a small hematoma might need observation only, whereas a large one might require immediate surgical intervention to prevent graft failure.
Q 7. Describe the technique for performing a plantar fascia release.
A plantar fascia release is a surgical procedure to relieve plantar fasciitis, a common cause of heel pain. The technique typically involves:
- Anesthesia: Either local or regional anesthesia is used, allowing the patient to remain awake and comfortable during the procedure.
- Incision: A small incision is made over the medial aspect of the heel, typically extending from the medial calcaneal tuberosity (the point of insertion of the plantar fascia on the heel bone).
- Fasciotomy: The plantar fascia is carefully identified and incised using a sharp scalpel. The goal is to release the tension on the fascia without damaging adjacent structures.
- Wound closure: The wound is then carefully closed with dissolvable sutures. A small drain might be placed to minimize the chance of fluid accumulation.
- Post-operative care: The patient is placed in a postoperative boot or splint to immobilize the foot and reduce pain. Physical therapy is frequently recommended to improve flexibility and strength.
Minimally invasive techniques can also be used, often utilizing smaller incisions and specialized instruments to reduce scarring and improve recovery time. The choice of approach depends on the specific clinical scenario and surgeon’s preference.
Q 8. What are the indications for plantar fascia grafting?
Plantar fascia grafting is a surgical procedure indicated for chronic plantar fasciitis cases that haven’t responded to conservative treatments like physical therapy, orthotics, and medications. Specifically, it’s considered when the patient experiences persistent, debilitating heel pain despite these efforts, and imaging (such as MRI or ultrasound) reveals significant plantar fascia tearing or degeneration. In essence, we’re talking about cases where the plantar fascia has failed to heal naturally and is significantly impacting the patient’s quality of life. For example, a patient who has tried six months of physical therapy with minimal pain relief and continues to limp and struggle with daily activities might be a candidate.
The decision to proceed with surgery is made based on a careful assessment of the patient’s history, clinical examination, and imaging results, ensuring surgery is a truly necessary step.
Q 9. What are the different types of grafts used for plantar fascia repair?
Several graft types are employed in plantar fascia repair. The most common are autografts, where tissue is harvested from the patient’s own body (often the flexor hallucis longus tendon or the peroneus brevis tendon). This minimizes the risk of rejection. Allografts, which are sourced from deceased donors, are another option, though they carry a higher risk of disease transmission and rejection. We also have the option of using synthetic grafts in certain cases, though these are often less successful than autografts in providing long-term durability. Finally, depending on the extent of the damage and the surgeon’s approach, some cases might benefit from a combination of techniques involving the use of a graft in conjunction with other surgical procedures such as fasciotomy or release techniques.
Q 10. How do you select the appropriate graft for a given patient?
Graft selection is a highly individualized process, heavily influenced by several factors. The extent of the plantar fascia damage, as seen on imaging studies, is a primary consideration. A larger tear might necessitate a more substantial graft like a tendon autograft, whereas a smaller, less severe tear may be amenable to a smaller graft or even a combination of surgical approaches, for example, a release procedure in combination with a smaller autograft. The patient’s age, overall health, and activity level also play crucial roles. Younger, more active patients might benefit from the superior longevity of a tendon autograft, even with the longer recovery period. Conversely, an older, less active patient may find an allograft or a smaller autograft more appropriate. The patient’s preference and the surgeon’s expertise are also vital in this decision-making process. We might prioritize an allograft to avoid a second surgical site in patients with co-morbidities affecting wound healing.
Q 11. What are the advantages and disadvantages of autografts versus allografts in plantar fascia repair?
Autografts, due to being taken from the patient’s own body, offer the significant advantage of minimal risk of rejection and disease transmission. They tend to integrate well with the surrounding tissue, leading to better long-term outcomes. However, they require a second surgical site for harvesting the graft, leading to increased discomfort and potential complications at that site. Allografts, on the other hand, eliminate the need for a second surgical site, resulting in a quicker recovery, typically. However, they carry the risk of disease transmission and rejection, although sophisticated screening and processing techniques significantly mitigate this risk. The potential for a longer-term outcome requires careful consideration, where autografts tend to have superior longevity and healing. The final decision hinges on a careful weighing of these advantages and disadvantages in light of the individual patient’s circumstances.
Q 12. Explain the post-operative care for patients undergoing plantar fascia grafting.
Post-operative care is crucial for a successful outcome. Patients are typically placed in a cast or a surgical boot immediately post-op for several weeks to immobilize the foot and allow the graft to heal. Weight-bearing restrictions are strictly enforced during this period, often involving the use of crutches. Regular follow-up appointments are scheduled to monitor healing, manage pain, and assess the graft’s integration. Physical therapy is initiated once sufficient healing has occurred, gradually increasing the range of motion and strength. The use of assistive devices like crutches and a walking boot are crucial in the early stage and gradually decrease with healing and therapist input.
Patients are carefully educated on proper wound care, signs of infection, and pain management strategies. The duration of post-operative rehabilitation varies but can range from several months to over a year depending on the individual patient.
Q 13. How do you manage post-operative pain and infection in plantar fascia graft recipients?
Post-operative pain is typically managed with prescribed analgesics, often a combination of over-the-counter pain relievers and stronger medications for acute pain control. Ice packs and elevation of the foot are also helpful. Infection is a serious concern, and prophylactic antibiotics are often administered. Careful monitoring for signs of infection, such as increased pain, swelling, redness, or purulent discharge, is essential. Any suspicion of infection requires immediate medical attention, often leading to surgical debridement, intravenous antibiotics, and potential graft failure. The goal here is aggressive early intervention.
Q 14. What are the potential long-term complications of plantar fascia grafting?
Long-term complications can include graft failure, recurrent plantar fasciitis, persistent pain, nerve damage, scarring, and limited range of motion. While these complications are not common, they’re important considerations for the patient. Careful patient selection, meticulous surgical technique, and diligent post-operative care help minimize these risks. For example, a patient who returns to high-impact activities too soon is at a greater risk of graft failure. We often have thorough discussions with patients about the realistic expectations for recovery and long-term function, including activity limitations.
Q 15. Describe your experience with different wound closure techniques.
Wound closure is a critical aspect of my practice, encompassing a range of techniques selected based on the wound’s characteristics and the patient’s overall health. My experience spans primary closure (suturing directly together wound edges), secondary intention (allowing the wound to heal naturally by granulation), and tertiary intention (delayed primary closure, where the wound is left open initially then closed later).
Primary closure: Ideal for clean, well-approximated wounds with minimal tissue loss. This technique offers the quickest healing time but isn’t suitable for all wounds, particularly those at high risk of infection.
Secondary intention: Used for wounds with significant tissue loss or contamination where primary closure isn’t feasible. Healing is slower and results in more scarring, but it’s effective in managing complex wounds. I frequently use this approach with chronic ulcers before considering grafting.
Tertiary intention: A compromise between primary and secondary intention. The wound is initially left open to allow for debridement and infection control, then closed surgically once the wound bed is healthy. This approach is useful for wounds where the risk of infection is initially high.
Skin grafting: A crucial part of my practice, involving the transfer of skin from a donor site to a recipient site (the wound). This is essential for wounds that won’t close by other methods due to tissue loss or damage.
The choice of closure technique requires careful consideration of numerous factors including wound depth, location, contamination, vascularity, and patient factors like comorbidities (such as diabetes which can impair healing).
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you assess a patient’s suitability for skin or plantar fascia grafting?
Assessing patient suitability for skin or plantar fascia grafting involves a thorough evaluation of several factors. It’s not a one-size-fits-all approach. First, the wound itself needs detailed assessment: its size, depth, location, presence of infection or foreign bodies, and the quality of surrounding tissue. I examine the wound bed for viable granulation tissue, eschar (dead tissue), and signs of infection.
Beyond the wound, I look at systemic factors. Conditions like diabetes, peripheral vascular disease (PVD), and immunosuppression significantly impact healing and graft survival. A patient with poorly controlled diabetes, for instance, may have impaired blood supply to the wound, reducing the chances of graft success. Similarly, PVD can compromise blood flow to both the graft and recipient site.
I also assess the patient’s overall health, including nutritional status, smoking history, and medications. Nutritional deficiencies can hinder healing, and smoking decreases blood flow, impacting graft take. A pre-operative assessment including blood tests and possibly imaging (discussed in the next question) helps ensure optimal conditions.
Finally, I discuss expectations and potential complications openly and honestly with the patient, ensuring they understand the procedure, recovery, and potential risks.
Q 17. What imaging modalities do you utilize to assess skin and plantar fascia defects?
Imaging plays a crucial role in assessing skin and plantar fascia defects before and after grafting. The choice of modality depends on the specific clinical question.
Ultrasound: A useful non-invasive tool to evaluate the depth and extent of soft tissue defects, assess blood flow to the wound bed (particularly important in PVD), and monitor graft thickness and integration. It’s relatively inexpensive and readily available.
Magnetic Resonance Imaging (MRI): Provides detailed anatomical information, particularly helpful in assessing the plantar fascia’s integrity and the extent of damage in plantar fascia defects. MRI is superior to ultrasound for detailed assessment of soft tissue structures and bone involvement.
Computed Tomography (CT): Less commonly used for superficial defects, but valuable if there is suspected bone involvement or foreign bodies within the wound.
For example, in a patient with a suspected deep plantar fascia tear, MRI would provide a precise assessment of the tear’s extent, guiding treatment decisions. Ultrasound would be helpful to monitor vascularity of the wound and track healing over time. The combination of imaging techniques often provides the most comprehensive evaluation.
Q 18. Discuss your experience with different types of dressings and their applications in wound healing.
Selecting the right dressing is crucial for optimal wound healing. My experience encompasses a wide array of dressings, each with specific properties and applications.
Hydrocolloids: These are self-adhesive dressings that maintain a moist wound environment, promoting autolytic debridement (the body’s natural removal of dead tissue). They are useful for partial-thickness wounds and help to reduce pain.
Hydrogels: Water-based dressings that provide moisture and hydration to the wound bed. They are particularly beneficial for dry, necrotic wounds and can help with pain management.
Alginates: Derived from seaweed, these dressings are highly absorbent and effective in managing wounds with heavy exudate (fluid). They are frequently used for wounds with significant drainage.
Foams: Absorbent dressings that can manage moderate to heavy exudate. They are available in various thicknesses, allowing for customization based on the wound’s drainage.
Transparent films: These allow for visualization of the wound bed while maintaining a moist environment. They are ideal for wounds with minimal exudate and are often used in the later stages of healing.
The choice of dressing depends on the stage of wound healing, the amount of exudate, the presence of infection, and the patient’s comfort. For example, a newly grafted wound might initially require a thin, transparent film to allow visualization and protect the graft. Later, a more absorbent dressing might be necessary depending on the level of exudate.
Q 19. How do you manage a dehisced wound after skin grafting?
Wound dehiscence after skin grafting, where the grafted skin separates from the wound bed, is a serious complication that requires prompt and decisive action. The immediate management focuses on preventing further damage and promoting reattachment or secondary healing.
Immediate Steps:
Gentle Wound Cleansing: The wound is carefully cleansed with saline solution to remove any debris or exudate.
Assessment of the Extent of Dehiscence: A thorough assessment determines the area of separation and the viability of the separated skin graft.
Debridement (if necessary): Any non-viable tissue is carefully debrided, to remove the necrotic tissue and leave a clean wound base.
Re-approximation (if possible): If the graft is still viable and the separation is minimal, gentle re-approximation of the graft to the wound bed may be attempted, using sutures or adhesive materials, accompanied by appropriate dressings to maintain pressure and prevent further separation.
Dressing Selection: A suitable dressing is applied to protect the wound, maintain a moist environment, and promote re-epithelialization. The choice depends on the wound’s characteristics and the presence of exudate (e.g., alginates for high exudate).
Subsequent Management:
Post-operative management involves regular wound assessments, and dressing changes, potential application of growth factors, and close monitoring for signs of infection. In cases where re-approximation is not successful, secondary intention healing will be allowed to occur. This process is often monitored by regular follow up appointments.
Prevention is key, with meticulous surgical technique and meticulous post-operative care playing an important role in minimizing the risk of dehiscence.
Q 20. Describe your experience with the use of growth factors in wound healing.
Growth factors have emerged as valuable tools to enhance wound healing, and I’ve had positive experiences integrating them into my practice. Growth factors are naturally occurring proteins that stimulate cellular proliferation and differentiation, crucial for tissue regeneration.
Types and Applications:
Platelet-derived growth factor (PDGF): Stimulates cell migration and proliferation, useful in chronic wounds with impaired healing.
Transforming growth factor-beta (TGF-β): Promotes collagen synthesis and tissue remodeling, helpful in improving the quality of scar tissue.
Fibroblast growth factor (FGF): Stimulates angiogenesis (blood vessel formation) and cell proliferation, crucial for graft survival.
Clinical Experience: I have used growth factors topically in various forms, including gels and creams, especially in recalcitrant wounds or in patients with impaired healing due to comorbidities such as diabetes. It’s important to note that growth factors are not a universal solution and their efficacy can vary depending on the wound type and the patient’s overall health. The decision to incorporate growth factors is made on a case-by-case basis after careful consideration of the wound and the patient’s condition.
In some cases, I have incorporated growth factors into the procedure itself, introducing them into the graft site to enhance integration and accelerate healing.
Q 21. Explain your understanding of the biological principles of skin and plantar fascia regeneration.
Understanding the biological principles of skin and plantar fascia regeneration is fundamental to successful grafting and wound management. Skin regeneration involves a complex interplay of various cell types and signaling pathways.
Skin Regeneration:
The process begins with hemostasis (blood clotting) followed by inflammation, where immune cells remove debris and prepare the wound bed. Keratinocytes (skin cells) migrate from the wound edges, and fibroblasts synthesize collagen to form new tissue. Angiogenesis (new blood vessel formation) is critical to provide nutrients and oxygen to the healing tissue. Finally, remodeling occurs, with collagen reorganization and scar tissue formation.
Plantar Fascia Regeneration:
Plantar fascia regeneration is significantly more challenging due to its limited blood supply and relatively low cellular turnover. Healing primarily involves scar tissue formation rather than complete regeneration of the original tissue. The limited regenerative capacity explains the persistence of pain and dysfunction in some patients after plantar fascia injuries. This limited regeneration capacity is why surgical procedures such as grafting may not completely restore the original function of the plantar fascia.
Clinical Implications: This knowledge informs my approach to managing wounds and choosing appropriate techniques. For example, optimizing blood supply to the wound bed is crucial for successful skin grafting, ensuring adequate cell migration, proliferation, and tissue regeneration. Understanding the limitations of plantar fascia regeneration helps in managing patient expectations, tailoring treatment plans, and focusing on pain management and functional restoration.
Q 22. How do you address patient concerns and expectations regarding grafting procedures?
Addressing patient concerns and expectations regarding grafting procedures is paramount. It begins with a thorough pre-operative consultation where I explain the procedure in clear, simple terms, avoiding overly technical jargon. I discuss the potential benefits, risks, and limitations of the grafting procedure, including the possibility of complications like infection, scarring, and graft failure. I use visual aids such as photographs and diagrams to illustrate the process and expected outcomes. Realistic expectations are crucial. For example, I explain that while we aim for optimal cosmetic results, perfect matching of skin tone and texture isn’t always possible, particularly with larger grafts or in areas with significant skin damage. I encourage patients to ask questions and address any anxieties they might have, emphasizing open communication throughout the entire process. Post-operatively, I maintain regular follow-up appointments to monitor healing progress, address concerns, and provide reassurance.
For instance, a patient anticipating a skin graft for a burn injury might have concerns about pain management, scarring, and the length of the recovery period. I explain the pain management protocol, the type of scarring expected (hypertrophic vs. atrophic), and the typical rehabilitation timeline. By managing expectations and fostering trust, I ensure the patient feels informed and empowered throughout their treatment journey.
Q 23. Describe a challenging case involving skin or plantar fascia grafting and how you overcame it.
One particularly challenging case involved a patient with a large, deep plantar fascia defect following a severe laceration. The wound was heavily contaminated, delaying the primary grafting procedure and increasing the risk of infection. The patient also suffered from diabetes, significantly compromising wound healing. Initially, the standard autologous plantar fascia graft was deemed unsuitable due to the extensive damage. We needed to achieve primary wound closure while maintaining functionality. We opted for a two-stage approach: First, we aggressively debrided the wound, addressing the contamination and establishing a healthy wound bed. This was followed by a period of negative pressure wound therapy (NPWT) to promote granulation tissue formation. After several weeks, once a sufficient amount of healthy granulation tissue had formed, we performed a split-thickness skin graft to cover the wound. This approach minimized the risk of graft failure and allowed for proper healing despite the patient’s underlying condition. Post-operatively, strict glycemic control and meticulous wound care were crucial to ensure successful outcome. Regular follow-ups and adjustments to the treatment plan as needed were vital in this case. Ultimately, the patient achieved satisfactory healing, though with a noticeable scar. This case highlighted the importance of adaptive treatment planning based on the patient’s specific circumstances and careful wound management.
Q 24. What are the ethical considerations in selecting patients for grafting procedures?
Ethical considerations in selecting patients for grafting procedures are paramount. The primary ethical principle is beneficence – ensuring that the procedure offers a net benefit to the patient, outweighing potential risks. This necessitates a thorough assessment of the patient’s overall health, including comorbidities such as diabetes, cardiovascular disease, and autoimmune conditions, which could affect healing and increase the risk of complications. Autonomy, the patient’s right to make informed decisions, is another crucial consideration. This involves providing patients with all the necessary information about the procedure, including benefits, risks, and alternatives, to allow them to make a fully informed choice. Justice requires equitable access to grafting procedures regardless of socioeconomic status or other demographic factors. Resources should be allocated fairly and transparently. Furthermore, the principle of non-maleficence requires that the procedure is not performed if the risks clearly outweigh the potential benefits. In cases with limited resources, prioritizing those patients who have the greatest chance of successful outcome and improved quality of life is ethically justifiable, however, careful evaluation and consideration of all patient needs are fundamental.
Q 25. What advancements in skin and plantar fascia grafting techniques have you observed recently?
Recent advancements in skin and plantar fascia grafting techniques include the widespread adoption of acellular dermal matrices (ADMs) as graft substitutes. These bioscaffolds promote tissue regeneration and can reduce donor site morbidity associated with autografts. We are also seeing increased use of minimally invasive surgical techniques, such as robotic surgery, to improve precision and reduce trauma during harvesting and grafting. Furthermore, there are ongoing research efforts focusing on stem cell therapies and tissue engineering, aiming to create bioengineered skin and fascia grafts with improved healing potential and cosmetic outcomes. Advances in imaging techniques, such as high-resolution ultrasound and 3D imaging, facilitate more accurate assessment of wound depth and tissue characteristics, leading to more precise graft design and placement. These innovations constantly enhance our ability to provide improved outcomes for patients.
Q 26. Describe your familiarity with relevant surgical instruments and equipment.
My familiarity with surgical instruments and equipment used in skin and plantar fascia grafting is comprehensive. This includes various types of scalpel blades, scissors, forceps (including Adson, Brown-Adson, and toothed forceps), skin hooks, dermatomes (for harvesting split-thickness skin grafts), and specialized instruments for fascia harvesting. I am proficient in using surgical lasers for precise excision and hemostasis, and various types of suture materials for graft fixation. I am also experienced with the utilization and maintenance of advanced equipment, such as surgical microscopes for microsurgical grafting techniques, operating tables with adjustable positioning capabilities, and negative pressure wound therapy (NPWT) systems. Understanding the nuances of each instrument and its appropriate application is critical for minimizing surgical trauma and maximizing graft success.
Q 27. How do you maintain a sterile field during grafting procedures?
Maintaining a sterile field during grafting procedures is of utmost importance to prevent infection. We adhere to strict aseptic techniques throughout the procedure, beginning with thorough handwashing and the use of sterile gloves, gowns, and drapes. The surgical site is meticulously prepared with antiseptic solutions. All instruments and equipment are sterilized prior to use. During the procedure, we maintain a meticulous sterile field, avoiding unnecessary movement or contact with unsterile items. A dedicated surgical team, all adhering to sterile protocols, is essential. Any potential breaches in sterility are immediately addressed. A continuous monitoring of the sterile field is undertaken throughout the procedure. For instance, we use sterile drapes to isolate the surgical field and prevent contamination from adjacent areas. The air quality in the operating room is maintained through filtration systems. These measures ensure an environment conducive to minimizing the risk of surgical site infection, a major concern following grafting procedures.
Q 28. What are your strategies for minimizing scarring after grafting?
Minimizing scarring after grafting involves a multifaceted approach that begins even before the surgery. Careful surgical technique, including precise wound closure and minimizing tension on the graft, plays a crucial role. Post-operatively, appropriate dressings and wound care are essential. We often use compression dressings to reduce swelling and improve graft adherence. The use of silicone gels or sheets can help to reduce hypertrophic scarring. In some cases, we might employ intralesional steroid injections to soften scar tissue. Patient education about proper sun protection after the procedure is critical, as UV exposure can worsen scarring. Early mobilization and physiotherapy can improve function and reduce contractures. For instance, after a plantar fascia graft, early range of motion exercises are crucial to maintain flexibility and prevent stiffness. In certain cases, we may utilize laser therapy or other advanced techniques to improve the cosmetic appearance of the scar over time. A multidisciplinary approach, often including dermatologists and physiotherapists, often provides optimal results.
Key Topics to Learn for Skin and Plantar Fascia Grafting Interview
- Wound Assessment and Selection Criteria: Understanding the ideal patient and wound characteristics for successful grafting procedures. This includes evaluating wound bed preparation, infection control, and overall patient health.
- Graft Harvest Techniques: Mastering the different techniques for harvesting skin and plantar fascia grafts, including split-thickness skin grafts, full-thickness skin grafts, and the nuances of plantar fascia harvesting. Consider the advantages and disadvantages of each.
- Graft Preparation and Handling: Understanding the meticulous process of preparing the graft for implantation, ensuring its viability and maximizing its chances of successful integration.
- Graft Application and Fixation: Understanding various methods for applying and securing the graft to the recipient site, including the importance of appropriate tension and immobilization techniques.
- Post-Operative Care and Management: Understanding the critical role of post-operative care in ensuring graft survival and patient recovery, including wound dressing techniques, pain management, and potential complications.
- Complications and their Management: Identifying potential complications such as graft failure, infection, hematoma, and seroma. Develop a clear understanding of their prevention and management strategies.
- Ancillary Procedures: Understanding the role of other surgical procedures that may accompany skin and plantar fascia grafting, such as debridement or tendon repair.
- Advances in Skin and Plantar Fascia Grafting: Staying current with the latest advancements in techniques, materials, and technologies used in skin and plantar fascia grafting.
Next Steps
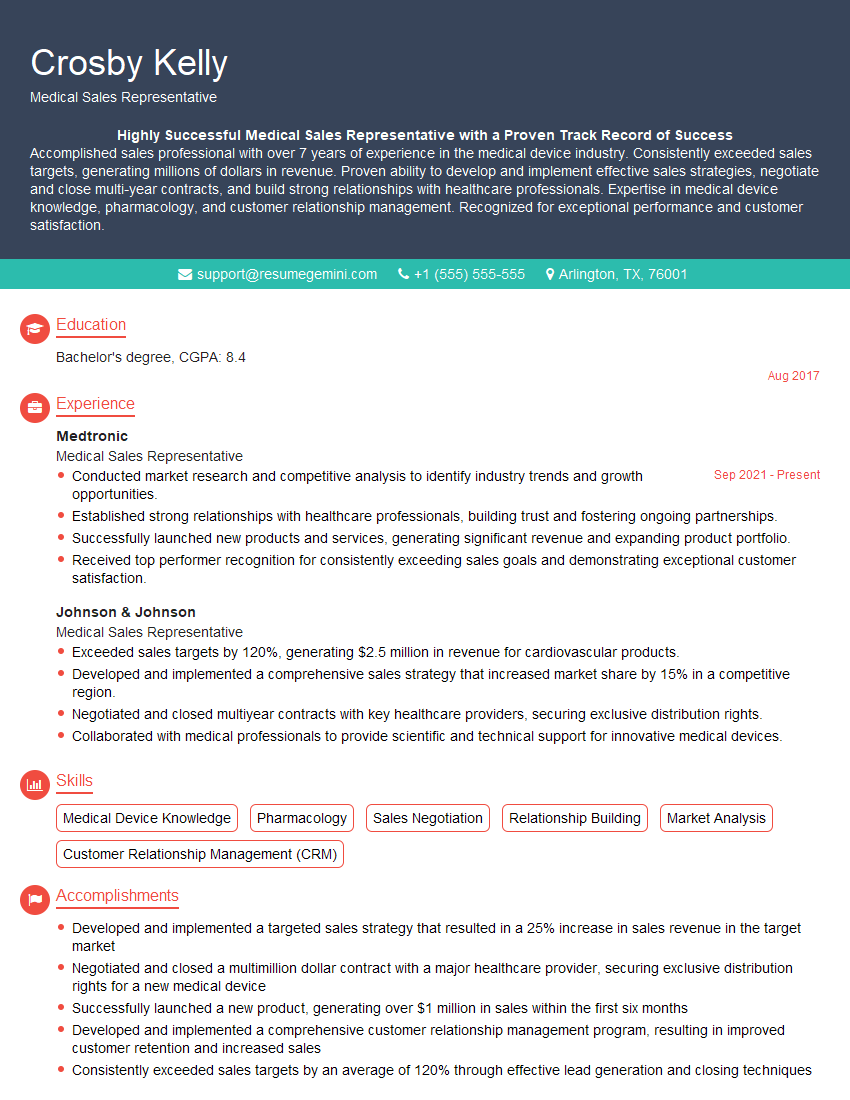
Mastering Skin and Plantar Fascia Grafting techniques significantly enhances your career prospects in reconstructive surgery and related fields. It demonstrates a high level of surgical skill and expertise, opening doors to advanced positions and research opportunities. To maximize your chances of landing your dream job, a well-crafted, ATS-friendly resume is crucial. ResumeGemini is a trusted resource to help you build a professional resume that highlights your skills and experience effectively. ResumeGemini provides examples of resumes tailored to Skin and Plantar Fascia Grafting to help guide you in creating a compelling application that showcases your qualifications.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.