Unlock your full potential by mastering the most common Ankle Arthroscopy interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Ankle Arthroscopy Interview
Q 1. Describe the indications for ankle arthroscopy.
Ankle arthroscopy is indicated when there’s a need to diagnose or treat intra-articular pathology of the ankle joint that is not readily apparent on imaging or through physical examination. It’s a minimally invasive surgical technique offering a superior view of the joint structures compared to open surgery.
- Osteochondral lesions of the talus (OLTs): These are lesions involving both the bone and cartilage of the talus, a common cause of ankle pain and instability.
- Synovitis: Inflammation of the synovial lining of the joint, often caused by arthritis or injury.
- Loose bodies: Fragments of cartilage or bone that float freely within the joint, causing pain and clicking.
- Ankle impingement: Restriction of normal joint movement due to bony spurs or soft tissue lesions.
- Ligament injuries: Certain ligament injuries may benefit from arthroscopic repair or debridement. This is typically reserved for cases where open repair is not possible.
- Debridement of damaged cartilage or bone: Removing damaged tissue to relieve pain and potentially improve joint function.
Essentially, if imaging suggests a problem within the ankle joint and conservative management (rest, ice, physical therapy, medication) has failed, then arthroscopy becomes a viable option. A detailed history and physical examination are crucial in determining the appropriateness of the procedure.
Q 2. What are the contraindications for ankle arthroscopy?
Contraindications to ankle arthroscopy are situations where the procedure’s risks outweigh its potential benefits. These include:
- Severe infection around the ankle: Introducing an arthroscope into an infected joint would exacerbate the infection.
- Extensive skin or soft tissue damage: The incisions required for arthroscopy would further damage compromised tissue.
- Uncontrolled medical conditions: Conditions such as uncontrolled diabetes, heart disease, or bleeding disorders significantly increase surgical risk. Careful assessment and optimization of the patient’s medical condition are critical.
- Unrealistic patient expectations: Arthroscopy may not be able to cure all ankle problems. It is crucial the patient understands the limitations and potential complications of the procedure.
- Severe ankle joint deformity: Severe deformity may make it difficult to visualize and access the joint structures during arthroscopy.
- Extensive prior ankle surgery: Extensive scarring from previous surgery may hinder the placement of portals or obscure visualization of the joint.
A thorough pre-operative evaluation that addresses these issues is crucial to determining whether the patient is a suitable candidate for ankle arthroscopy.
Q 3. Explain the different portals used in ankle arthroscopy.
Several portals, or small incisions, are used in ankle arthroscopy to gain access to different areas within the ankle joint. The specific portals used depend on the pathology being addressed. Common portals include:
- Anteromedial portal: Provides access to the medial gutter and anterior joint.
- Anterolateral portal: Allows visualization of the lateral gutter and anterior joint.
- Posteromedial portal: Offers access to the posterior joint compartment and the medial aspect of the posterior talus.
- Posterolateral portal: Provides access to the posterior joint compartment and the lateral aspect of the posterior talus.
- Distal portal (sometimes used): A more distal portal which may be used to assist in certain procedures.
The surgeon uses a combination of these portals, employing an arthroscope (a small camera) in one and specialized instruments in others to perform the procedure. Fluoroscopy (live X-ray imaging) is often used to guide portal placement and ensure proper instrument positioning within the joint.
Q 4. Detail the steps involved in a typical ankle arthroscopy procedure.
A typical ankle arthroscopy procedure follows these steps:
- Anesthesia: General anesthesia or regional anesthesia (spinal or ankle block) is administered.
- Portal Creation: Small incisions (portals) are made around the ankle joint to insert the arthroscope and instruments.
- Arthroscopy: The arthroscope is inserted to visualize the joint and assess the pathology.
- Diagnostic Arthroscopy: Thorough evaluation of the joint to identify the specific issues present.
- Surgical Intervention: Based on the findings, appropriate surgical techniques are implemented. This may involve debridement of damaged tissue, repair of ligament tears, removal of loose bodies, or other specific procedures.
- Irrigation and Lavage: The joint is thoroughly irrigated to remove any debris or blood.
- Closure: The portals are closed with sutures or steri-strips.
- Postoperative Care: A protective dressing is applied, and the patient is given instructions for post-operative care, including pain management, weight-bearing restrictions, and physical therapy.
The entire procedure typically takes between 30-90 minutes, depending on the complexity of the case.
Q 5. How do you diagnose an ankle impingement?
Diagnosing ankle impingement involves a combination of techniques. It is a condition of restricted joint movement often involving bony spurs, loose bodies, or ligament instability.
- Patient History: A detailed history, including the onset, nature, and location of the pain, is crucial. Pain often worsens with activity and specific range of motion. A ‘catching’ or locking sensation may be described.
- Physical Examination: This involves assessing the range of motion, palpating for tenderness, and performing special tests to assess ligament stability. A limited range of motion, particularly dorsiflexion (pointing toes upward), or plantarflexion (pointing toes downward) is often noted.
- Imaging: X-rays can reveal bony spurs or other bony abnormalities. MRI provides a detailed view of the soft tissues and is highly valuable in detecting ligament injuries or other soft tissue lesions. CT scans may be used for better evaluation of bony structures.
- Arthroscopy (diagnostic): In many cases, arthroscopy is used to confirm the diagnosis and assess the extent of the impingement. Direct visualization of the structures within the ankle allows the surgeon to accurately identify the source of impingement.
Sometimes, a combination of clinical findings and imaging is sufficient for a diagnosis; however, arthroscopy may be necessary to confirm the diagnosis and to simultaneously address the pathology.
Q 6. What are the common pathologies treated with ankle arthroscopy?
Ankle arthroscopy is used to treat a variety of pathologies, including:
- Osteochondral lesions of the talus (OLTs): These lesions are treated through debridement, microfracture, or autologous chondrocyte implantation (ACI).
- Synovitis: Arthroscopy allows for direct visualization and treatment of synovitis, often through debridement or synovectomy.
- Loose bodies: These can be easily removed arthroscopically.
- Ankle impingement: Arthroscopy is used to remove bony spurs or address soft tissue lesions causing impingement.
- Ligament injuries: Certain ligament injuries, particularly those involving the anterior talofibular ligament (ATFL), may be addressed arthroscopically in select cases.
- Debridement of damaged articular cartilage: This can be performed to alleviate pain and improve joint function. In some instances, cartilage repair techniques such as microfracture may also be implemented.
- Ganglion cysts: Removal of ganglion cysts within or adjacent to the ankle joint.
The choice of treatment depends on the specific pathology and the surgeon’s assessment of the patient’s condition.
Q 7. Describe the surgical techniques for treating osteochondral lesions of the talus.
Surgical techniques for treating osteochondral lesions of the talus (OLTs) during ankle arthroscopy depend on the size, location, and severity of the lesion. Common techniques include:
- Debridement: This involves removing loose or damaged cartilage fragments. This is appropriate for smaller lesions that aren’t deep and may provide short term relief.
- Microfracture: This technique creates small fractures in the subchondral bone (beneath the cartilage) to stimulate bleeding and the formation of new cartilage. This is best suited for smaller, relatively superficial lesions.
- Autologous Chondrocyte Implantation (ACI): This involves harvesting healthy cartilage cells from a non-weight-bearing area of the patient’s knee, growing them in a laboratory, and then reimplanting them into the lesion. This is a more complex procedure suitable for larger, deeper lesions where a more robust, cartilage-like repair is desired.
- Osteochondral autograft transplantation (OAT): This involves harvesting a plug of healthy bone and cartilage from a non-weight-bearing area, usually the knee, and then transferring it to the site of the OLT to fill the defect. This technique is also suitable for larger lesions but may involve a more significant surgical procedure.
The choice of technique is individualized based on the patient’s age, activity level, lesion size, location, and the surgeon’s preference. The goal is to restore articular surface congruity and alleviate pain, thereby improving joint function.
Q 8. How do you manage a syndesmotic injury during ankle arthroscopy?
Managing a syndesmotic injury (injury to the ligaments connecting the tibia and fibula) during ankle arthroscopy requires a careful and systematic approach. It’s crucial to remember that arthroscopy itself isn’t always sufficient for syndesmotic repair; often, it plays a diagnostic and adjunctive role.
Initial Assessment: The arthroscope allows for direct visualization of the syndesmosis. We look for signs of widening, instability, and ligamentous disruption. Intra-operative fluoroscopy (discussed later) is essential here to confirm the findings.
Arthroscopic Management (Limited): If the injury is minimal, such as a small tear, we might perform debridement of any loose fragments or inflamed tissue within the joint. This can sometimes improve stability.
Open Surgical Repair: However, most significant syndesmotic injuries require open surgical repair. This is because arthroscopic techniques can’t provide the necessary fixation strength for a stable repair. Arthroscopy can guide the surgeon in positioning the open incisions, but the actual repair is performed using screws and plates externally.
Example: Imagine trying to fix a broken chair leg with only a tiny needle. You might be able to clean it up a bit, but you can’t create a strong, stable repair. Open surgery is like using strong screws and glue for a proper fix.
Q 9. What are the potential complications of ankle arthroscopy?
Ankle arthroscopy, while minimally invasive, carries potential complications. These can be broadly categorized into:
- Infections: A risk with any surgical procedure, meticulously following sterile technique is paramount to minimize this. Post-op antibiotics are usually prescribed.
- Stiffness: Scar tissue formation can lead to limited range of motion. Physical therapy plays a crucial role in mitigating this.
- Complex Regional Pain Syndrome (CRPS): A rare but debilitating condition characterized by chronic pain, swelling, and changes in skin color and temperature. Early recognition and management are key.
- Nerve Injury: The proximity of nerves in the ankle region makes nerve damage a possibility, though less frequent with experienced surgeons. Careful surgical technique helps minimize this.
- Recurrence of the original problem: This is particularly true for articular cartilage damage that wasn’t fully addressed during surgery. Careful planning and surgical precision are vital.
- Deep Vein Thrombosis (DVT) or Pulmonary Embolism (PE): These are rare but serious risks associated with any surgery, necessitating appropriate prophylactic measures.
- Wound Healing Complications: Problems like delayed healing or infection can occur, which necessitate additional management.
Thorough patient selection, meticulous surgical technique, and a comprehensive postoperative plan are crucial for minimizing these risks.
Q 10. How do you assess the stability of the ankle joint during arthroscopy?
Assessing ankle joint stability during arthroscopy involves a combination of visual inspection and stress testing.
Visual Inspection: The arthroscope allows for direct visualization of the articular cartilage, ligaments, and joint capsule. We look for any evidence of injury or damage to these structures.
Stress Testing: While the joint is under direct visualization, we apply controlled stress to the ankle. This involves manipulating the ankle in various directions (dorsiflexion, plantarflexion, inversion, eversion) to assess the integrity of the ligaments.
Intraoperative Fluoroscopy: This is invaluable in providing additional information regarding joint stability. Fluoroscopic images show the alignment and relationship between the bones, aiding in the assessment of ligamentous injury (as discussed later).
Example: Imagine checking the stability of a table leg. You visually inspect it for cracks, then manually try to move it to see how firmly it’s connected to the tabletop. Similarly, during arthroscopy, we combine visual inspection with manual stress testing to assess the joint’s stability.
Q 11. Discuss the post-operative management of an ankle arthroscopy patient.
Post-operative management of an ankle arthroscopy patient is crucial for optimal recovery and minimizing complications.
Immediate Post-op: This includes pain management (often with ice and analgesics), elevation of the leg to reduce swelling, and assessment of the surgical site for signs of infection or excessive bleeding.
Early Post-op (Days 1-7): Patients are typically mobilized with partial weight-bearing (as per surgeon’s instructions), and physical therapy is initiated to improve range of motion and reduce swelling. Wound care is essential during this period.
Intermediate Post-op (Weeks 2-6): Progressive weight-bearing and range-of-motion exercises are continued. Physical therapy focuses on strengthening and regaining functional mobility.
Later Post-op (Weeks 6+): Further strengthening and proprioceptive (balance) exercises are incorporated. Return to sports or other activities is gradual and depends on the patient’s progress and the nature of the surgery.
Patient Education: Clear communication with the patient about pain management, expected recovery timeline, signs of complications (infection, excessive swelling, persistent pain), and adherence to the prescribed physical therapy regimen is crucial.
Q 12. What are the different types of ankle arthroscopy instruments?
Ankle arthroscopy utilizes a variety of specialized instruments designed for precise manipulation within the confined space of the ankle joint. These include:
- Arthroscope: A slender, telescope-like instrument with a camera and light source that provides visualization of the joint’s interior.
- Shavers: Used to remove damaged cartilage, loose bodies, and inflamed tissue.
- Forceps: Various sizes and shapes, used for grasping and manipulating tissue.
- Probes: Used to explore the joint and assess the extent of injuries.
- Scissors: For cutting and trimming tissue.
- Cannulas: Introduce irrigation fluid and provide access to the joint.
- Suction Devices: Remove debris and blood from the operative field.
The specific instruments used depend on the nature of the surgical procedure.
Q 13. Explain the use of fluoroscopy during ankle arthroscopy.
Fluoroscopy is a real-time X-ray imaging technique used during ankle arthroscopy to provide a dynamic view of the joint’s anatomy. It’s invaluable in several aspects:
- Accurate Instrument Placement: Ensures instruments are placed in the correct anatomical location, minimizing the risk of iatrogenic injury to important structures.
- Assessment of Reduction: When addressing fractures or dislocations, fluoroscopy verifies the proper alignment of the bones post-reduction.
- Assessment of Ligamentous Injuries: Provides clear visualization of the syndesmosis or other ligaments to assess the extent of injury or stability.
- Implant Placement: Allows for accurate placement of screws or other implants during certain procedures.
Example: Imagine trying to assemble a complex jigsaw puzzle in the dark. Fluoroscopy is like turning on a light; it illuminates the anatomy, allowing for precise and safe manipulation of the instruments within the ankle joint.
Q 14. How do you manage intraoperative bleeding during ankle arthroscopy?
Intraoperative bleeding during ankle arthroscopy is usually minimal due to the minimally invasive nature of the procedure and the use of tourniquets. However, if bleeding occurs, several strategies are employed:
- Pressure: Direct pressure on the bleeding site with a sponge or other instrument can often control minor bleeding.
- Irrigation: Using copious amounts of irrigation fluid washes away blood and improves visibility. This also helps dilute any clotting factors.
- Electrocautery: For pinpoint bleeding sources, electrocautery can be used to seal off small blood vessels. This is used cautiously to avoid damage to surrounding tissues.
- Suture Ligation: In rare cases where bleeding is significant and cannot be controlled by the above methods, surgical ligation of the bleeding vessel may be required.
Prevention is key. Maintaining adequate hemostasis during the procedure by careful dissection and use of appropriate surgical techniques reduces the need for these more advanced methods.
Q 15. How do you differentiate between a ligamentous injury and a cartilage lesion on arthroscopy?
Differentiating between a ligamentous injury and a cartilage lesion during ankle arthroscopy relies on a combination of visual inspection and understanding of anatomical structures. Ligamentous injuries often present as tears, fraying, or stretching of the ligament fibers. We look for irregularities in the ligament’s normal smooth, glistening appearance. These tears can be partial or complete. We might see hemorrhage or inflammation surrounding the injured ligament. Cartilage lesions, on the other hand, manifest as changes in the cartilage’s surface. This could include fibrillation (roughening), fissuring (cracks), or full-thickness defects (loss of cartilage). The color of the cartilage can also be an indicator; normal cartilage is pearly white, while damaged cartilage might appear dull, yellow, or even red if inflamed. We use specialized arthroscopic probes and instruments to assess the depth and extent of both ligament and cartilage injuries. For example, a significant lateral ankle sprain might show a clear tear in the anterior talofibular ligament (ATFL), easily distinguishable from a localized area of cartilage fibrillation on the talus. Careful assessment, aided by high-definition imaging and the surgeon’s experience, is crucial for accurate diagnosis.
Career Expert Tips:
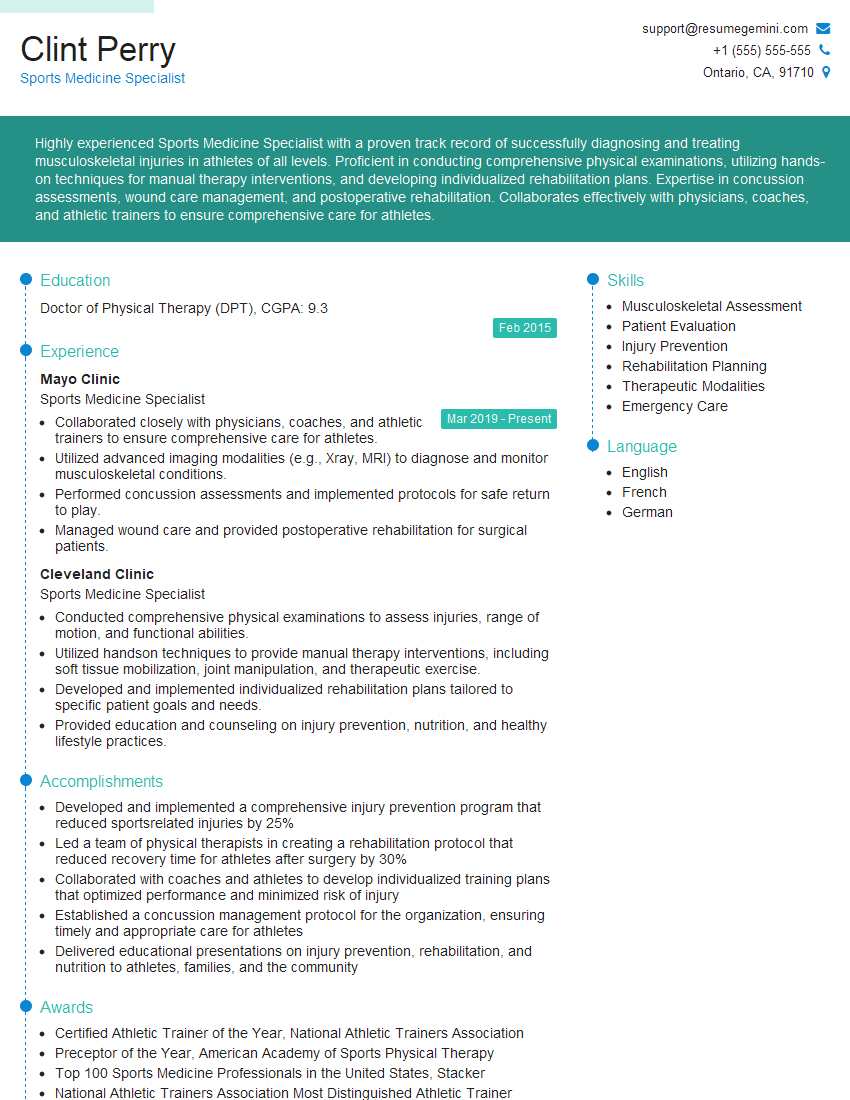
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe the rehabilitation protocol following ankle arthroscopy.
Rehabilitation after ankle arthroscopy is crucial for a successful outcome. The protocol is highly individualized and depends on the nature and extent of the surgery. Initially, the focus is on pain control and reducing swelling. This often involves elevation of the leg, ice application, and possibly medication. Early mobilization is encouraged to prevent stiffness, starting with simple range-of-motion exercises. Weight-bearing is gradually progressed as tolerated, often using crutches initially. Physical therapy plays a vital role, incorporating strengthening exercises for the ankle and surrounding muscles. Proprioceptive training – exercises that improve balance and coordination – is also essential. The patient might start with simple exercises like toe raises and ankle pumps, gradually progressing to more challenging activities, such as balance board exercises and agility drills. The duration of rehabilitation varies, but patients typically see significant improvement within several weeks. Return to sports or strenuous activities is determined on a case-by-case basis, typically after achieving full strength and stability.
Q 17. What are the advantages and disadvantages of ankle arthroscopy compared to open surgery?
Ankle arthroscopy offers several advantages over open surgery. It’s minimally invasive, resulting in smaller incisions, less pain, reduced scarring, faster recovery times, and a shorter hospital stay. It also provides excellent visualization of the joint, allowing for precise diagnosis and treatment. Open surgery, while sometimes necessary for complex cases, involves a larger incision, greater tissue disruption, longer recovery, and a higher risk of complications like infection and stiffness. However, arthroscopy may not be suitable for all conditions, particularly those requiring extensive joint reconstruction or significant bone work. For example, a large osteochondral defect might necessitate open surgery for optimal repair. The choice between arthroscopy and open surgery depends on the specific clinical scenario and the surgeon’s judgment.
Q 18. How do you address post-operative infection after ankle arthroscopy?
Post-operative infection after ankle arthroscopy, while rare, is a serious complication. Management involves prompt diagnosis and aggressive treatment. Early signs might include increased pain, swelling, redness, warmth around the incision, and fever. Laboratory tests, including blood cultures, may be performed to identify the infecting organism. Treatment typically involves intravenous antibiotics, tailored to the specific bacteria identified. In some cases, surgical debridement (removal of infected tissue) might be necessary. The goal is to eradicate the infection and prevent further spread. Close monitoring of the patient is crucial throughout the treatment process, including regular wound care and follow-up appointments. Prevention strategies include meticulous surgical technique, proper sterilization of instruments, and antibiotic prophylaxis (preventative antibiotics) in high-risk patients.
Q 19. What are the common causes of failure after ankle arthroscopy?
Failure after ankle arthroscopy can stem from various factors. Incomplete lesion repair, either in cartilage or ligaments, is a common cause. This may result from inadequate surgical technique or the inherent limitations of arthroscopic repair. Persistent inflammation or instability can also lead to poor outcomes. Sometimes, pre-existing conditions or co-morbidities might negatively affect healing. For instance, patients with underlying arthritis or poor blood supply might experience less satisfactory results. Patient non-compliance with the rehabilitation protocol can also contribute to failure, as inadequate exercise or improper weight-bearing can hinder recovery. Finally, an inaccurate diagnosis leading to inappropriate surgical intervention can result in a less-than-optimal outcome.
Q 20. How do you manage a persistent pain after ankle arthroscopy?
Managing persistent pain after ankle arthroscopy necessitates a thorough evaluation to determine the underlying cause. It’s important to differentiate between pain related to the surgical procedure itself and pain arising from other sources, such as pre-existing conditions. A detailed history, physical examination, imaging studies (X-rays, MRI), and nerve conduction studies might be necessary. Management strategies include medication, physical therapy, injections (such as corticosteroids or local anesthetics), and occasionally further surgical intervention. If the pain is due to instability, addressing this might require additional procedures like ligament reconstruction. If nerve irritation is the problem, targeted treatment focusing on the nerves might be appropriate. The goal is to identify the source of pain and implement targeted treatment to alleviate the symptoms and improve function.
Q 21. Describe your experience with different types of ankle implants used in arthroscopy.
My experience encompasses various ankle implants used in arthroscopy, though they are not as frequently used as in other joints like the knee or hip. We primarily utilize implants for the repair of osteochondral lesions (damage to both bone and cartilage). These can range from small, bioabsorbable implants for filling small defects to larger, more complex implants designed to integrate with the bone and provide structural support. I have experience with various materials, including synthetic materials and those derived from the patient’s own bone marrow. The choice of implant depends on factors such as the size and location of the lesion, the patient’s age and activity level, and the surgeon’s preference. The goal is to choose an implant that provides appropriate support, stimulates healing, and minimizes the risk of complications. Successful implantation requires precise placement and secure fixation to ensure stability and long-term integration. Careful postoperative management, including appropriate weight-bearing and rehabilitation, is crucial for optimal results.
Q 22. Discuss the role of advanced imaging (MRI, CT) in planning ankle arthroscopy.
Advanced imaging, specifically MRI and CT scans, plays a crucial role in pre-operative planning for ankle arthroscopy. These modalities provide detailed anatomical information, far exceeding what a physical exam can offer. They are essential for identifying the precise location and nature of intra-articular pathology.
- MRI: Offers excellent soft tissue contrast, allowing visualization of ligamentous injuries (like anterior talofibular ligament tears), cartilage lesions (osteochondral defects), synovitis, and bone bruises. It’s particularly useful in detecting subtle injuries often missed on X-ray.
- CT: Provides superior bone detail, allowing for accurate assessment of fractures, osteophytes (bone spurs), and loose bodies within the joint. 3D CT reconstructions can be particularly helpful in complex cases.
For example, an MRI might reveal a significant cartilage defect in the talus, guiding the arthroscopic approach and the need for potential cartilage repair procedures during the surgery. A CT scan might show a small loose body that needs to be removed. By combining the information from both MRI and CT, we can develop a highly tailored surgical plan, improving the chances of a successful outcome and reducing intraoperative surprises.
Q 23. How do you counsel patients about the risks and benefits of ankle arthroscopy?
Counseling patients about ankle arthroscopy involves a thorough discussion of both the potential benefits and risks. I always emphasize that it’s a minimally invasive procedure, but it’s still surgery with inherent risks.
- Benefits: I explain how it can alleviate pain, improve range of motion, and potentially avoid more extensive open surgery. I use relatable examples, like comparing the smaller incisions to keyhole surgery, highlighting quicker recovery times and reduced scarring.
- Risks: I clearly outline potential complications, including infection, nerve injury, stiffness, persistent pain, and the possibility that the surgery may not fully resolve the problem. I explain the likelihood of these risks, emphasizing that they are rare but possible. I also discuss the need for post-operative physiotherapy and rehabilitation.
The conversation is tailored to the individual patient’s specific situation and concerns. For instance, a younger, active patient might have different priorities and risk tolerance than an older patient. Transparency and open communication build trust and ensure informed consent.
Q 24. Describe a challenging case you encountered during ankle arthroscopy and how you handled it.
One challenging case involved a patient with a complex ankle fracture and significant ligamentous instability that had been poorly managed initially. The patient presented with persistent pain and limited mobility, despite previous attempts at conservative treatment. The post-traumatic arthritis was severe, and significant scarring made the arthroscopic approach significantly more difficult.
The challenge was navigating the dense scar tissue to gain adequate visualization of the joint while minimizing further trauma. I employed specialized instruments and techniques, including the use of a wider-angle arthroscope and meticulous dissection under direct visualization. We successfully debrided the damaged cartilage and repaired the ligaments, restoring joint congruity. Post-operative rehabilitation was crucial, and the patient gradually regained a good level of function.
This case highlighted the importance of careful pre-operative planning, the need for specialized instrumentation, and the value of adapting surgical techniques to overcome intra-operative challenges.
Q 25. What are the latest advancements in ankle arthroscopy techniques?
Recent advancements in ankle arthroscopy include:
- Improved instrumentation: Smaller, more precise instruments allow for less invasive procedures and improved visualization in challenging anatomical areas.
- Enhanced visualization techniques: High-definition arthroscopy and specialized lenses provide clearer images, allowing surgeons to identify and address pathology with greater accuracy.
- Minimally invasive cartilage repair techniques: Techniques like microfracture, autologous chondrocyte implantation (ACI), and osteochondral autograft transfer system (OATS) are becoming increasingly refined and are often performed arthroscopically.
- 3D-printed implants and surgical guides: These technologies offer improved accuracy and personalization in procedures like ligament reconstruction.
- Robotic-assisted arthroscopy: This offers improved precision and potentially reduced invasiveness, but its wider adoption is still ongoing.
These advancements lead to improved surgical outcomes, faster recovery times, and reduced complications. They demonstrate the ongoing evolution of the field towards minimally invasive and patient-centered care.
Q 26. How do you stay current with the latest research and advancements in ankle arthroscopy?
Staying current in ankle arthroscopy requires a multi-faceted approach.
- Active participation in professional organizations: Membership in organizations like the American Academy of Orthopaedic Surgeons (AAOS) and attendance at national and international conferences provide access to the latest research and techniques.
- Review of peer-reviewed journals: Regularly reviewing leading orthopaedic journals, such as the Journal of Bone and Joint Surgery and the American Journal of Sports Medicine, keeps me abreast of current research.
- Continuing medical education (CME): I actively seek out relevant CME courses and workshops to enhance my skills and knowledge base. This includes hands-on workshops focusing on new surgical techniques and instrumentation.
- Collaboration with colleagues: Engaging in discussions and case presentations with other ankle arthroscopy specialists facilitates knowledge exchange and the sharing of best practices.
This continuous learning process ensures that I provide my patients with the best possible care using the most current and evidence-based techniques.
Q 27. What are your strengths and weaknesses as an Ankle Arthroscopy surgeon?
My strengths lie in my meticulous surgical technique, my commitment to patient education and communication, and my ability to adapt to challenging surgical situations. I’m detail-oriented and strive for excellence in every procedure. I’m also known for a thorough and patient approach to consultations.
One area for improvement is my delegation skills. As a highly involved surgeon, I sometimes find it challenging to fully delegate tasks to the surgical team. I am actively working on improving this aspect by employing clear communication protocols and enhancing trust within the team.
Q 28. What are your long-term career goals in the field of ankle arthroscopy?
My long-term career goals include continued refinement of my surgical skills in ankle arthroscopy, particularly in complex revision cases and the implementation of newer technologies. I also aspire to contribute to the advancement of the field through research and mentoring of junior surgeons. I’m interested in exploring opportunities for leadership within the orthopaedic community, potentially contributing to surgical guidelines and educational initiatives. Ultimately, I aim to become a recognized leader and innovator in the field of ankle arthroscopy.
Key Topics to Learn for Ankle Arthroscopy Interview
- Ankle Anatomy & Biomechanics: Thorough understanding of ligaments, tendons, bones, and their interplay during movement. Consider the implications of variations in anatomy.
- Arthroscopic Techniques: Mastery of portals, instrumentation, and specific procedures like debridement, repair, and reconstruction. Practice explaining your approach to different scenarios.
- Diagnosis & Imaging: Interpreting X-rays, MRI, and CT scans to identify pathologies requiring arthroscopic intervention. Discuss differential diagnoses and the role of clinical examination.
- Surgical Planning & Decision-Making: Explain your decision-making process for selecting the appropriate surgical approach based on patient history, imaging findings, and clinical presentation. Include a discussion of limitations and potential complications.
- Post-Operative Care & Rehabilitation: Outline the post-operative management including pain control, immobilization, and rehabilitation protocols. Discuss expected recovery timelines and potential complications.
- Complications & Management: Identify potential intraoperative and postoperative complications (e.g., infection, nerve injury, stiffness). Describe your approach to managing these complications.
- Current Research & Trends: Stay updated on the latest advancements in ankle arthroscopy techniques, instrumentation, and rehabilitation strategies. Demonstrate your commitment to continuous learning.
- Ethical Considerations & Patient Communication: Discuss the importance of informed consent, shared decision-making, and managing patient expectations.
Next Steps
Mastering ankle arthroscopy is crucial for advancing your career in orthopedic surgery and showcasing your expertise in minimally invasive techniques. A strong resume is your first impression – make it count! An ATS-friendly resume increases your chances of getting noticed by recruiters. ResumeGemini is a trusted resource to help you build a professional and impactful resume that highlights your skills and experience. Examples of resumes tailored to Ankle Arthroscopy are provided to guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.