Unlock your full potential by mastering the most common Orthotics and Arch Supports Prescription interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Orthotics and Arch Supports Prescription Interview
Q 1. What are the different types of arch supports available?
Arch supports, or orthotics, come in various types, broadly categorized as prefabricated and custom. Prefabricated orthotics are readily available over-the-counter in pharmacies and shoe stores. They offer various levels of arch support and cushioning but lack the personalized fit of custom orthotics. Custom orthotics, on the other hand, are individually designed and crafted to address a patient’s specific foot structure and biomechanical needs.
- Full-length orthotics: These cover the entire sole of the foot, providing comprehensive support from heel to toe.
- 3/4 length orthotics: These extend from the heel to the metatarsal heads, offering support to the arch and midfoot, suitable for those with less severe foot conditions.
- Heel cups: Primarily designed to provide heel support and cushioning, often used for plantar fasciitis.
- Arch wedges: These simple devices provide added lift under the arch and can be inserted into existing shoes.
- Partial orthotics: Custom-made but address only specific regions of the foot, like the metatarsals, for issues such as metatarsalgia.
The choice depends heavily on the severity and nature of the foot problem.
Q 2. Explain the biomechanics of the foot and ankle.
The foot and ankle are complex structures with intricate biomechanics. Imagine a sophisticated suspension system! The bones, muscles, ligaments, and tendons all work together to provide stability, mobility, and shock absorption during movement. The subtalar joint, located between the heel bone (calcaneus) and talus, allows for inversion and eversion (rolling the foot inward and outward). The midtarsal joint contributes to pronation and supination (the foot’s rolling motion).
During gait (walking), the foot goes through a sequence: heel strike, midstance, push-off. Pronation, the inward rolling of the foot, is crucial for shock absorption. Excessive pronation, however, can lead to various problems. Supination, the outward rolling, is equally important for balance and stability. An imbalance in these motions can affect the entire kinetic chain, leading to pain in the knees, hips, and even back.
Q 3. How do you assess a patient’s need for orthotics?
Assessing a patient’s need for orthotics is a multi-step process. It starts with a comprehensive history taking, where I delve into the patient’s medical history, current symptoms, activities, and shoe wear patterns. Then a thorough physical examination follows, which includes observing their gait (walking style), assessing range of motion in the ankles and feet, palpating for tenderness or abnormalities, and checking for deformities like flat feet or high arches.
I also utilize specialized tools like a foot pressure plate to quantitatively analyze pressure distribution and identify areas of increased stress. This data, combined with the clinical examination, helps pinpoint the underlying cause of their discomfort and determine the appropriate level of support required. For instance, a patient with plantar fasciitis might benefit from heel support and arch support, while someone with excessive pronation might need a more substantial orthotic device to control the foot’s rolling motion.
Q 4. Describe the process of taking a plaster cast for custom orthotics.
Creating a plaster cast for custom orthotics is a precise procedure. First, the patient’s foot is thoroughly cleaned and prepared. A foam or cotton padding material is placed around the foot and lower leg to provide comfort and create a smooth surface for the cast. Then, the plaster bandages (or modern alternatives like foam or other materials) are carefully applied, starting from the toes and working up to the lower leg. The cast needs to encompass the entire foot and slightly below the ankle. It’s crucial to maintain proper alignment during the casting process.
The plaster is allowed to fully harden, usually within 15-20 minutes. The cast is then carefully removed and inspected to ensure its integrity. It provides a three-dimensional model of the patient’s foot which acts as a positive mold for creating the orthotic devices.
Q 5. What materials are commonly used in orthotic fabrication?
Orthotic fabrication utilizes a variety of materials, each with unique properties:
- Polypropylene: A rigid, durable, and lightweight plastic, commonly used for the base of many orthotics. It offers good support and is easy to mold.
- EVA (Ethylene-vinyl acetate): A cushioning foam material frequently used as a shock-absorbing layer within the orthotic or as a top cover layer.
- Carbon fiber: A high-strength, lightweight material incorporated to provide additional support and stiffness, often used in high-performance orthotics for athletes or individuals with significant instability.
- Leather: Used for the top cover of some orthotics. Offers breathability but is less durable than other materials.
- Cork: A natural, shock-absorbing material sometimes used for cushioning, particularly in softer custom orthotics.
The choice of material greatly affects the orthotic’s overall characteristics, and the best material depends on many factors, such as the individual’s weight, activity level, and foot condition.
Q 6. How do you select the appropriate material for a specific patient’s needs?
Material selection is crucial for orthotic success. It’s tailored to the patient’s specific needs and the type of support required. For instance, a highly active individual with significant pronation might require a rigid polypropylene base for stability and control, combined with a layer of EVA for shock absorption. A less active individual with mild plantar fasciitis might benefit from a softer, more flexible material, like EVA, or a combination of cork and leather for comfort and cushioning.
Patients with high arches will likely need materials that provide more arch support and stability. Similarly, patients with flat feet or excessive pronation will benefit from stiffer, more supportive materials. A lightweight material will be advantageous for someone who is very active or an athlete. The material’s durability, breathability, and weight are also considered, balancing performance and comfort.
Q 7. Explain the difference between prefabricated and custom orthotics.
Prefabricated and custom orthotics differ significantly in their design, fitting, and effectiveness. Prefabricated orthotics are mass-produced, ‘one-size-fits-most’ devices available over the counter. They offer general support but may not address individual foot abnormalities precisely. They are often a good starting point for minor foot pain or discomfort or for a trial period before committing to custom orthotics.
Custom orthotics are individually designed and manufactured based on a detailed assessment of the patient’s feet and biomechanics. They provide a precise fit, addressing specific needs and anatomical variations. While more costly, they are far more effective in managing complex foot conditions. Think of prefabricated orthotics as ready-to-wear clothing—comfortable for many, but not tailored. Custom orthotics are akin to bespoke tailoring—precisely crafted for individual needs, providing optimal comfort and support.
Q 8. What are the common indications for orthotic prescription?
Orthotics are prescribed for a wide range of conditions affecting the feet, ankles, and lower extremities. The goal is to improve biomechanics, alleviate pain, and correct deformities. Common indications include:
- Pes planus (flat feet): Orthotics help support the arch and improve foot stability, reducing strain on the ankles, knees, hips, and lower back.
- Pes cavus (high arches): These can lead to metatarsalgia (pain in the ball of the foot) and other issues; orthotics help redistribute pressure and reduce pain.
- Plantar fasciitis: Orthotics provide arch support and cushioning, reducing strain on the plantar fascia, the thick band of tissue on the bottom of the foot.
- Metatarsalgia: Orthotics can redistribute pressure away from painful metatarsal heads.
- Heel spurs: While not directly treating the spur itself, orthotics can help manage associated pain by reducing strain on the heel.
- Bunions (hallux valgus): Orthotics can help alleviate pain and pressure on the bunion.
- Knee pain (related to foot biomechanics): Improper foot mechanics can contribute to knee pain. Orthotics can help correct these mechanics.
- Lower back pain (related to foot biomechanics): Similar to knee pain, foot biomechanics directly affect the entire kinetic chain, and orthotics can positively impact lower back pain.
- Diabetic foot complications: Orthotics can help prevent foot ulcers and reduce pressure on areas with decreased sensation.
Essentially, if a patient is experiencing pain or discomfort due to foot or leg biomechanical issues, an orthotic evaluation is often warranted.
Q 9. What are the contraindications for orthotic use?
While orthotics are generally well-tolerated, there are some contraindications. These are situations where orthotics might not be beneficial or could even be harmful. These include:
- Severe peripheral arterial disease (PAD): Reduced blood flow to the feet can make it difficult for wounds to heal, and ill-fitting orthotics can increase the risk of ulceration.
- Severe neurological conditions: Patients with decreased sensation in their feet may not be able to detect problems with orthotic fit, increasing the risk of skin breakdown and injury.
- Active infection or significant inflammation: Orthotics can exacerbate these conditions.
- Certain skin conditions: Conditions that make the skin fragile, like severe eczema, can be irritated by orthotics.
- Uncontrolled edema (swelling): Orthotics may restrict blood flow and worsen swelling. The edema needs to be addressed first.
- Patient non-compliance: If a patient is unwilling or unable to wear the orthotics as prescribed, they won’t be effective.
A thorough patient history and physical examination are crucial to identify these contraindications before prescribing orthotics.
Q 10. How do you address patient concerns and questions about orthotics?
Addressing patient concerns is crucial for successful orthotic therapy. I always start by actively listening to their concerns, validating their feelings, and explaining the rationale behind the orthotic prescription in clear, non-technical terms. I use visual aids like diagrams and models to illustrate how the orthotics will work. I answer all their questions patiently and thoroughly, creating a safe space for them to express doubts or worries. For example, if a patient is concerned about the cost, I’ll discuss different payment options and explore if there are any financial assistance programs available. If they are worried about comfort, I’ll explain the break-in period and strategies for managing any discomfort. Building a strong doctor-patient relationship based on trust and understanding is paramount.
Q 11. Describe the process of fitting and adjusting orthotics.
Fitting and adjusting orthotics is a multi-step process that requires skill and experience. It begins with a thorough biomechanical evaluation, including gait analysis and assessment of foot structure. Then, a custom or prefabricated orthotic is selected based on the patient’s needs. Next, the orthotic is fitted to the patient’s foot, ensuring proper alignment and comfort. This often involves adjustments to accommodate the foot’s unique shape and biomechanics. A series of follow-up appointments are scheduled for adjustments based on the patient’s feedback and ongoing assessment. We typically evaluate:
- Pressure points: Are there areas of excessive pressure that need padding or modifications?
- Range of motion: Does the orthotic restrict the patient’s ankle or foot movement excessively?
- Comfort: Is the orthotic generally comfortable during activities?
- Effectiveness: Is it effectively addressing the patient’s pain or biomechanical issue?
Adjustments might involve modifying the shell, adding padding, or changing the heel height. The goal is to achieve optimal comfort and effectiveness.
Q 12. How do you educate patients on proper orthotic care and maintenance?
Patient education is crucial for long-term success. I provide clear instructions on how to care for and maintain their orthotics. This includes:
- Cleaning: Regular cleaning with mild soap and water to prevent the build-up of sweat and debris.
- Drying: Allowing the orthotics to air dry completely to prevent mold and mildew growth.
- Storage: Storing them in a clean, dry place to maintain their shape and integrity.
- Inspection: Regularly checking for any signs of wear and tear and reporting any issues promptly.
- Break-in period: Emphasizing that there will be a break-in period where discomfort is possible, and offering strategies for comfort like gradual use or using appropriate socks.
I also advise patients on appropriate footwear choices that complement their orthotics and provide written instructions to reinforce the verbal information.
Q 13. What are the common complications associated with orthotic use?
While generally safe, complications can arise from orthotic use. These are usually related to improper fitting or patient non-compliance:
- Skin irritation or breakdown: This can occur due to pressure points or friction. Proper fitting and padding can help prevent this.
- Increased pain: If the orthotics are ill-fitting or inappropriate for the condition, they can exacerbate pain instead of alleviating it. This is why a thorough evaluation is so important.
- Calluses or corns: These can develop due to excessive pressure in specific areas.
- Nail problems: Improper fitting can compress the toenails.
- Leg cramps: In some instances, orthotics might change muscle activation and cause leg cramps initially, which usually resolve with adjustments or adaptation.
Regular follow-up appointments are vital to identify and address these complications promptly.
Q 14. How do you troubleshoot common problems with orthotic fitting?
Troubleshooting fitting issues involves a systematic approach. I start by assessing the patient’s complaints and re-evaluating the initial biomechanical assessment. Common problems include:
- Painful pressure points: This usually requires adding padding or modifying the orthotic shell to redistribute pressure.
- Restricted range of motion: The orthotic might need to be adjusted to allow for more natural movement.
- Lack of effectiveness: This might indicate that the initial diagnosis or orthotic prescription was incorrect. A reevaluation might be needed, or a different type of orthotic may be required.
- Poor comfort: This might be due to material incompatibility, improper break-in, or ill-fitting footwear. Addressing these factors is crucial.
I use a combination of observation, palpation, and patient feedback to identify the problem and develop appropriate solutions. Sometimes, a custom orthotic modification is necessary, while other times, simply adjusting footwear or providing additional patient education is sufficient.
Q 15. What are the latest advancements in orthotic technology?
Recent advancements in orthotic technology are revolutionizing how we address biomechanical foot and lower limb issues. Key innovations include:
- 3D Scanning and CAD/CAM Manufacturing: This allows for highly accurate, customized orthotics produced with greater precision and efficiency than traditional methods. The process minimizes errors and ensures a better fit.
- Smart Orthotics: Incorporating sensors and microprocessors, these devices can monitor gait parameters, pressure distribution, and even activity levels, providing valuable data for clinicians and patients. This allows for objective assessment of treatment efficacy and potential adjustments.
- Advanced Materials: Lighter, stronger, and more breathable materials like carbon fiber composites, thermoplastic polymers, and memory foams are being used to create more comfortable and durable orthotics. These materials cater to a wide range of patient needs and activities.
- Bioprinting: While still in its early stages, bioprinting holds immense potential for creating personalized orthotics with customized biomechanical properties, potentially even incorporating regenerative medicine approaches.
- Improved Design Software: Sophisticated software allows for intricate design modifications, incorporating complex biomechanical principles and patient-specific anatomical details for optimized support.
These advancements ultimately lead to improved patient comfort, better functional outcomes, and more efficient manufacturing processes.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you stay up-to-date with the latest research and best practices in orthotics?
Staying current in the dynamic field of orthotics requires a multi-faceted approach. I actively participate in:
- Professional Organizations: Membership in organizations like the American Academy of Orthopaedic Surgeons (AAOS) and the American Orthotic and Prosthetic Association (AOPA) provides access to continuing education courses, journals, and networking opportunities with leading experts.
- Conferences and Workshops: Attending conferences and workshops allows me to learn about the latest research findings, new technologies, and best practices directly from researchers and clinicians.
- Peer-Reviewed Journals: Regularly reviewing articles in journals like the Journal of the American Podiatric Medical Association (JAPMA) and Clinical Biomechanics keeps me updated on the latest scientific evidence supporting orthotic interventions.
- Online Resources and Databases: I utilize online databases like PubMed and Google Scholar to access research articles and stay informed about emerging trends and technologies.
- Mentorship and Collaboration: Engaging with experienced colleagues and mentors through professional networks fosters collaboration and knowledge sharing.
This combination of active participation and continuous learning ensures that I apply the most up-to-date, evidence-based practices in my clinical work.
Q 17. Describe your experience with different orthotic designs (e.g., UCBL, medial longitudinal arch support).
My experience encompasses a wide range of orthotic designs, each tailored to specific biomechanical needs. I have extensive experience with:
- UCBL (University of California, Biomechanics Laboratory) Orthotics: These custom-made orthotics are known for their comprehensive approach to addressing foot and ankle biomechanics. They often incorporate features like medial longitudinal arch support, metatarsal pads, and heel cups to correct pronation or supination, and manage various foot conditions. I’ve found them particularly effective for patients with complex needs.
- Medial Longitudinal Arch Support: These are crucial for supporting the arch of the foot, and I use various designs depending on the patient’s specific needs. Some are incorporated into custom-made orthotics, while others are readily available as off-the-shelf supports. The design often involves a raised medial arch to improve support and reduce stress on the plantar fascia.
- Other Designs: I’ve worked extensively with other designs including functional foot orthoses, accommodative orthotics, and those addressing specific conditions like hallux valgus, pes cavus, and pes planus. My approach always prioritizes selecting the most appropriate design based on a thorough biomechanical evaluation and the patient’s individual needs.
Selecting the right design often requires careful consideration of the patient’s condition, activity level, and personal preferences to create a functional and comfortable solution.
Q 18. How do you incorporate patient preferences into the orthotic prescription process?
Incorporating patient preferences is paramount for successful orthotic prescription. A successful orthotic is not just biomechanically sound, but also comfortable and acceptable to the patient for daily use. I achieve this through:
- Open Communication: I begin by having an open discussion with the patient about their lifestyle, activity level, footwear preferences, and any concerns or expectations they have regarding the orthotics.
- Education: I explain the biomechanical principles underlying the recommended orthotic design and how it will address their specific condition. This ensures informed consent and empowers patients to be active participants in the treatment process.
- Customization Options: I offer various choices in materials, colors, and styles whenever possible, allowing patients to personalize their orthotics and enhance their comfort and acceptance. This includes choices regarding the type of cushioning, the level of support, and the style of the orthotic.
- Trial and Adjustment: I provide opportunities for patients to trial the orthotics and provide feedback, allowing for adjustments to be made to ensure optimal fit and comfort before finalization.
By prioritizing patient-centered care, we create a positive experience and increase the likelihood of adherence to the treatment plan. A comfortable, patient-approved orthotic is much more likely to be used correctly and produce the desired outcome.
Q 19. How do you manage patients with specific foot conditions (e.g., plantar fasciitis, flat feet, high arches)?
Managing patients with specific foot conditions requires a personalized approach that considers the unique presentation of each case. Here’s how I approach some common conditions:
- Plantar Fasciitis: Treatment typically involves orthotics with a deep heel cup to support the plantar fascia and reduce stress on the heel. Custom-made orthotics often incorporate medial arch support to reduce excessive pronation. Night splints may also be recommended.
- Flat Feet (Pes Planus): Orthotics for flat feet usually involve medial longitudinal arch support to provide structural support and correct excessive pronation. Custom-made orthotics are often more effective than off-the-shelf options, as they can be precisely molded to the individual’s foot shape and biomechanics.
- High Arches (Pes Cavus): Patients with high arches often benefit from orthotics that provide metatarsal support and cushioning to reduce pressure on the forefoot and improve comfort. Custom-made orthotics are frequently used to address the specific biomechanical imbalances present in pes cavus.
Beyond orthotics, treatment often involves other modalities such as stretching exercises, icing, and anti-inflammatory medications. Each patient’s treatment plan is individualized based on their specific presentation, activity level, and response to treatment.
Q 20. What is your experience with different casting methods?
I have extensive experience with various casting methods for orthotic fabrication, each with its advantages and disadvantages:
- Traditional Plaster Casting: This method provides excellent detail and accuracy but can be time-consuming and less comfortable for the patient. It requires skilled technique to obtain a precise cast.
- Foam Box Casting: A faster and more comfortable method, foam box casting utilizes foam material to create a cast of the patient’s foot. It is often used for less complex orthotics but may lack the detail of plaster casting.
- Digital Scanning: This modern technique uses 3D scanners to create a digital model of the foot, eliminating the need for traditional casting entirely. It offers superior accuracy, speed, and comfort for the patient and simplifies the manufacturing process.
My choice of casting method is determined by factors including the complexity of the orthotic, the patient’s comfort level, and the availability of resources and technology. I often explain the advantages and disadvantages of each method to the patient to ensure they are comfortable with the chosen approach.
Q 21. Describe your experience with CAD/CAM technology in orthotics.
CAD/CAM (Computer-Aided Design/Computer-Aided Manufacturing) technology has significantly improved the accuracy, efficiency, and customization of orthotic fabrication. My experience with this technology includes:
- Digital Model Creation: Using 3D scanning or digital impressions, we create a highly accurate 3D model of the patient’s foot. This model serves as the basis for the orthotic design.
- Design Software: Specialized software allows for precise design modifications, incorporating the patient’s specific biomechanical needs and anatomical features. We can adjust various parameters like shell thickness, arch height, and heel cup depth to optimize the orthotic’s function.
- CNC Milling: Once the design is finalized, the digital model is sent to a CNC (Computer Numerical Control) milling machine, which precisely carves the orthotic from a block of material. This ensures consistent quality and accuracy in the final product.
- Finishing and Refinement: After milling, the orthotic undergoes finishing and refinement processes, ensuring a smooth and comfortable fit. This may include trimming, sanding, and adding cushioning layers.
CAD/CAM technology allows for a much more precise and customized orthotic than traditional methods, leading to improved patient outcomes and overall satisfaction. It also streamlines the manufacturing process, improving efficiency and reducing turnaround time.
Q 22. What is your experience with 3D printed orthotics?
My experience with 3D printed orthotics is extensive. I’ve found them to be a game-changer in custom orthotic fabrication. The technology allows for a level of precision and customization previously unattainable with traditional methods. For example, we can create orthotics with intricate designs to address highly specific biomechanical needs, such as accommodating complex deformities or incorporating pressure-relieving features in very targeted areas. I use CAD software to design the orthotics based on patient-specific data from pressure mapping and physical assessments. The 3D printing process allows for rapid prototyping, enabling us to iterate on designs and fine-tune the orthotics until we achieve the optimal fit and function. This significantly reduces turnaround time for patients compared to traditional methods. Furthermore, 3D printing allows us to use a wider range of materials with different properties (e.g., flexibility, density), tailored to each patient’s unique needs and activity level. The process also enables the creation of orthotics with features that would be impossible to achieve through traditional casting methods.
Q 23. How do you measure foot angles (e.g., heel valgus, forefoot varus)?
Measuring foot angles like heel valgus and forefoot varus requires a systematic approach. I begin with a thorough visual inspection to identify any obvious deformities. Then, I use a combination of tools, including a goniometer and plumb line. The goniometer measures the angle between two bones, for example, the angle of the heel relative to the lower leg to assess heel valgus (outward turning of the heel) or the angle of the forefoot relative to the rearfoot to assess forefoot varus (inward turning of the forefoot). The plumb line helps to assess the alignment of the lower limb, providing an overall picture of the limb’s alignment in relation to the center of gravity. We hang the plumb line from the anterior superior iliac spine (ASIS), and the ideal position is to have it hang directly through the middle of the patella, ankle, and foot. Deviations from this line can indicate underlying biomechanical problems. Footprint analysis using a podoscope or weight-bearing radiographs can further help quantify these angles and support the clinical assessment.
Q 24. Explain your understanding of pressure mapping and its role in orthotic prescription.
Pressure mapping is a crucial diagnostic tool in orthotic prescription. It provides a quantitative assessment of plantar pressure distribution during weight-bearing. Using a pressure mapping system, we capture a detailed picture of how pressure is distributed across the plantar surface of the foot. Areas of high pressure, which can indicate areas prone to breakdown or pain, are readily identified. This information is indispensable in designing orthotics that effectively redistribute pressure and reduce stress on problematic areas. For example, if a patient presents with plantar fasciitis, pressure mapping can pinpoint the exact location of high pressure under the heel, guiding the design of the orthotic’s heel cup to provide optimal support and cushioning in that specific area. This ensures the orthotic will be targeted and effective, reducing trial and error and improving patient outcomes.
Q 25. How do you assess the effectiveness of an orthotic prescription?
Assessing the effectiveness of an orthotic prescription involves a multi-faceted approach. We start by reassessing the patient’s symptoms. Has their pain reduced? Has their gait improved? We also perform a clinical examination, checking for any changes in foot posture, range of motion, and muscle strength. We may repeat pressure mapping to determine if pressure distribution has improved. Patient feedback is crucial; we ask them about their experience with the orthotics in terms of comfort, functionality and any lingering pain. We also consider their activity levels and how well they are tolerating the orthotics during daily activities. Sometimes, functional assessments, such as gait analysis, might be employed to objectively measure improvements in gait parameters. If the orthotics aren’t working as intended, we might modify the design, consider a different material, or even explore alternative treatment options.
Q 26. What are the ethical considerations in orthotics prescription?
Ethical considerations in orthotic prescription are paramount. We must ensure the prescription is medically necessary and that the patient fully understands the benefits and risks involved. This includes being transparent about costs and any potential limitations. We must avoid prescribing unnecessary orthotics purely for profit. It’s also crucial to respect patient autonomy, allowing them to participate actively in decision-making. Maintaining confidentiality is vital, as is providing informed consent before any treatment. If there is any conflict of interest, such as a financial incentive for recommending a specific product, it must be disclosed. We need to provide ethical and evidence-based recommendations and avoid using unsubstantiated claims or misleading patients into making choices that might not be in their best interest.
Q 27. How do you handle situations where a patient is non-compliant with orthotic use?
Non-compliance with orthotic use is a common challenge. First, I explore the reasons for non-compliance through open communication. Are they uncomfortable? Do they find them cumbersome? Are there practical challenges in using them? Understanding their concerns helps address them appropriately. This might involve adjusting the orthotics, providing alternative options, suggesting methods to improve comfort, or offering educational resources about the importance of consistent use. In some cases, involving a therapist to aid in adaptation and motivation might be beneficial. I also reiterate the treatment goals and how the orthotics contribute to achieving them. If the underlying cause of the pain has improved significantly, we can explore a gradual reduction in orthotic usage, making the transition less daunting. Collaboration with the patient is key to overcoming compliance issues and improving the success rate of orthotic therapy.
Q 28. Describe your experience collaborating with other healthcare professionals (e.g., podiatrists, physical therapists).
Collaboration with other healthcare professionals is essential for optimal patient care. I regularly work with podiatrists, physical therapists, and physicians. For example, I might collaborate with a podiatrist on cases involving diabetic foot ulcers, where managing pressure distribution is critical for wound healing. Physical therapists often help patients develop exercises to enhance their strength and improve biomechanics, complementary to orthotic therapy. Collaboration with physicians is particularly valuable when managing patients with systemic conditions that impact foot health, such as rheumatoid arthritis or diabetes. This collaborative approach ensures a holistic approach to patient care, integrating different perspectives and expertise for the best possible outcomes. We often share information through electronic health records or in direct consultations to ensure everyone is aligned on the treatment plan and its progression.
Key Topics to Learn for Orthotics and Arch Supports Prescription Interview
- Biomechanics of the Foot and Ankle: Understanding gait analysis, plantar pressure distribution, and common foot deformities (e.g., pes planus, cavus foot).
- Types of Orthotic Devices: Familiarize yourself with various orthotic designs (e.g., accommodative, functional, corrective), materials, and manufacturing processes.
- Patient Assessment and Examination: Master the techniques for conducting thorough patient history taking, physical examinations, and identifying appropriate treatment plans.
- Prescription Writing and Communication: Learn to effectively communicate your findings and recommendations to other healthcare professionals (e.g., physicians, physical therapists) through clear and concise prescriptions.
- Practical Application of Orthotics: Understand how to properly fit and adjust orthotics, addressing common patient issues such as pain, discomfort, and skin irritation.
- Casting and Modeling Techniques: Gain proficiency in taking accurate foot impressions and constructing custom orthotics using various materials and methods.
- Rehabilitation and Patient Education: Develop strategies for educating patients on proper orthotic use, care, and follow-up appointments.
- Legal and Ethical Considerations: Understand the implications of prescribing orthotics and adhering to professional standards of practice.
- Common Foot Conditions and Their Treatment: Develop expertise in diagnosing and managing common foot and ankle pathologies that benefit from orthotic intervention (e.g., plantar fasciitis, metatarsalgia, hallux valgus).
- Advanced Orthotic Concepts: Explore topics such as biomechanical principles, custom orthotic design software, and emerging technologies in orthotics.
Next Steps
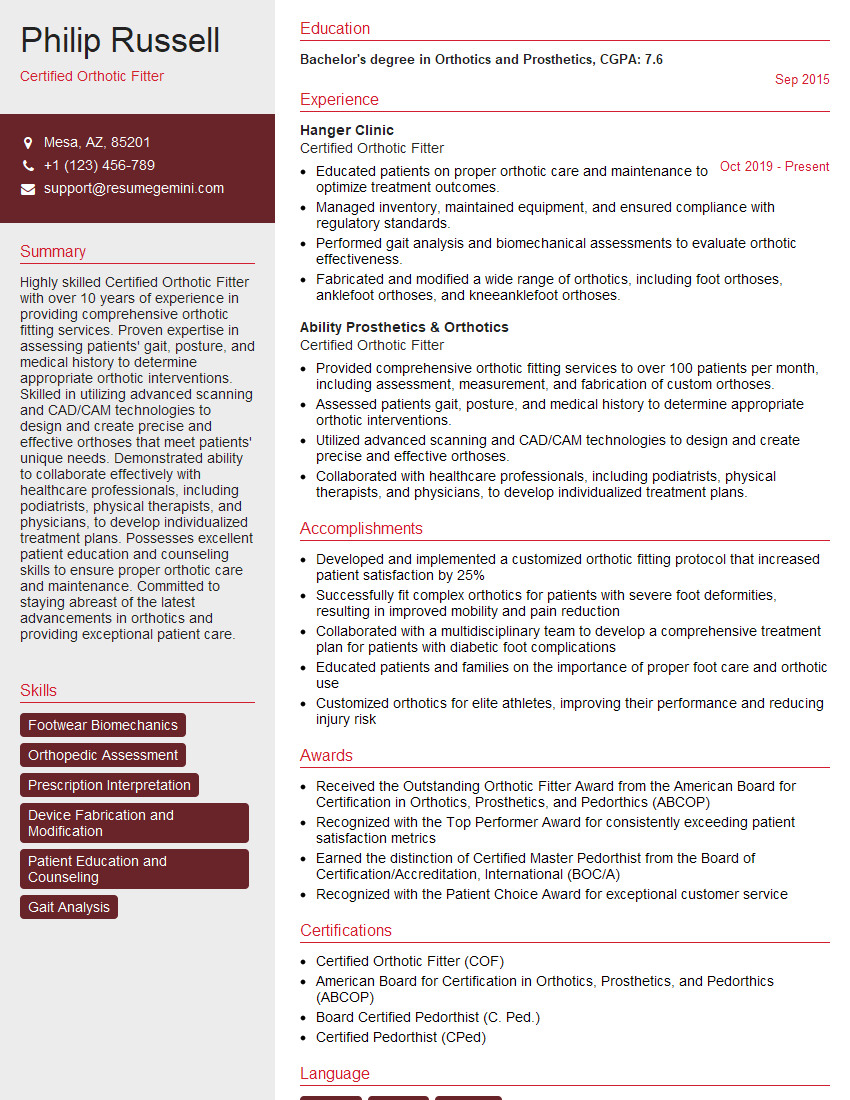
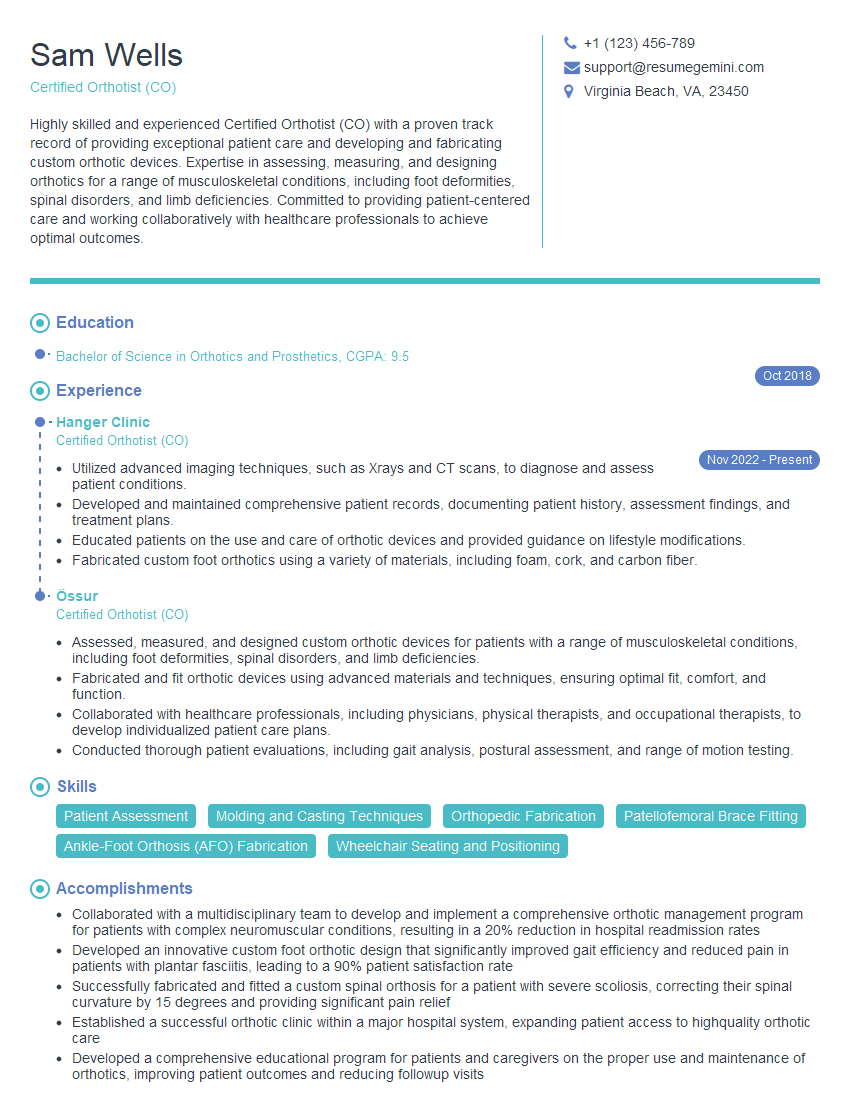
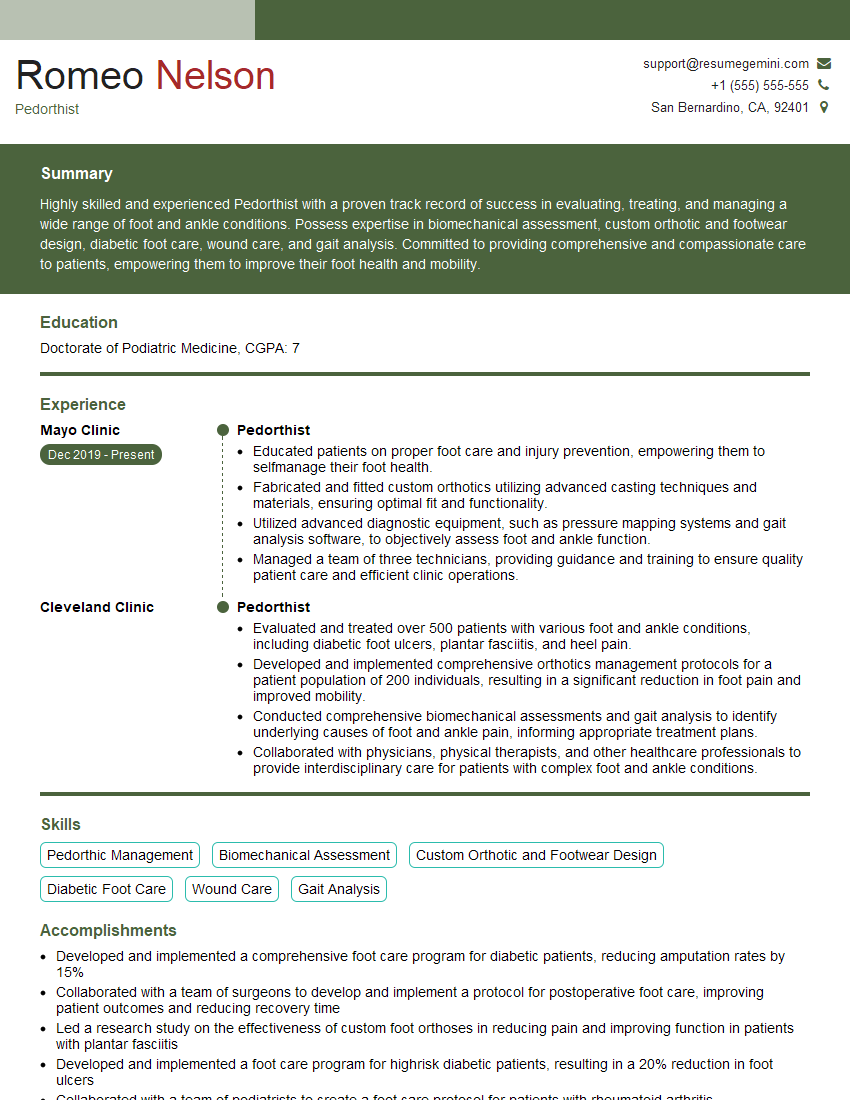
Mastering Orthotics and Arch Supports Prescription is crucial for career advancement in this specialized field. A strong understanding of these concepts will significantly improve your interview performance and demonstrate your expertise to potential employers. To enhance your job prospects, focus on creating an ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource to help you build a professional and impactful resume. They offer examples of resumes tailored specifically to Orthotics and Arch Supports Prescription professionals, providing you with a valuable head start in your job search.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.