Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Ingrown Toenails Treatment interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Ingrown Toenails Treatment Interview
Q 1. Describe the different methods for treating ingrown toenails.
Ingrown toenail treatment varies depending on the severity. Mild cases often respond well to conservative management at home. More severe cases may require professional intervention.
- Conservative Management: This involves soaking the foot in warm, soapy water several times a day to soften the skin and nail. Gently lifting the ingrown portion of the nail away from the skin using a cotton thread or small piece of gauze can also provide relief. Over-the-counter pain relievers like ibuprofen can help manage discomfort. Proper nail trimming – cutting straight across and not too short – is crucial for prevention.
- Partial Nail Avulsion: A minor surgical procedure where a portion of the ingrown nail is removed. This is done under local anesthesia to minimize discomfort. A small section of the nail matrix (the area where the nail grows from) may also be removed to prevent recurrence. This procedure is relatively straightforward and usually only takes about 15-20 minutes.
- Complete Nail Avulsion: This involves removing the entire toenail. It’s usually reserved for severe cases where infection is present or conservative measures have failed. The procedure is performed under local anesthesia and may involve removing a portion of the nail matrix to reduce the chances of the nail growing back ingrown. Post-operative care involves keeping the area clean and dry to promote healing.
- Chemical Cauterization (Phenol): This technique uses phenol, a chemical, to destroy a portion of the nail matrix. It is less invasive than nail avulsion but may require multiple sessions for complete treatment.
The choice of treatment method depends on individual factors like the severity of the ingrown toenail, the presence of infection, and the patient’s overall health.
Q 2. Explain the procedure for partial or complete nail avulsion.
Nail avulsion, whether partial or complete, is a minor surgical procedure performed by a podiatrist or other qualified healthcare professional. It’s crucial to remember that this should only be done in a sterile environment to minimize the risk of infection.
Partial Nail Avulsion:
- Local Anesthesia: The area around the toenail is numbed using a local anesthetic injection. This ensures the patient is comfortable during the procedure.
- Nail Removal: A small portion of the ingrown nail is carefully removed using surgical instruments. The procedure is precise to avoid damaging the surrounding skin and tissue.
- Matrixectomy (Optional): In some cases, a small portion of the nail matrix (the root of the nail) may be removed to prevent regrowth of the ingrown portion. Different techniques are used, including chemical matrixectomy using phenol or surgical excision.
- Wound Care: The wound is cleaned and dressed to promote healing and prevent infection.
Complete Nail Avulsion: This procedure follows a similar sequence but involves removing the entire toenail. A larger section of the nail matrix may also be removed. Post-operative care is more extensive, requiring regular dressing changes and monitoring for signs of infection.
Proper postoperative care, including keeping the wound clean and dry and using prescribed antibiotics if necessary, is essential for a successful outcome.
Q 3. What are the common causes of ingrown toenails?
Ingrown toenails are a common problem with several contributing factors. Improper nail trimming is a leading cause, as cutting the nails too short or curving the edges can make the nail grow into the surrounding skin. Other factors include:
- Tight-fitting shoes: Shoes that put pressure on the toenails can force the nail to curve and grow into the skin.
- Trauma: Injuries to the toenail, such as stubbing your toe, can cause the nail to grow abnormally.
- Genetics: Some people are genetically predisposed to ingrown toenails due to the shape of their nails or nail beds.
- Underlying medical conditions: Conditions like fungal infections, psoriasis, and peripheral vascular disease can increase the risk of ingrown toenails.
- Improper foot hygiene: Poor hygiene can increase the risk of infection in an already ingrown nail.
Understanding these causes helps in implementing preventive measures like wearing properly fitted shoes and adopting correct nail-cutting techniques.
Q 4. How do you differentiate between an ingrown toenail and other foot conditions?
Differentiating an ingrown toenail from other foot conditions requires careful examination. Key characteristics of an ingrown toenail include:
- Pain and tenderness: The affected area is typically painful, especially when pressure is applied.
- Redness and swelling: The skin around the ingrown nail is often red and swollen, potentially indicating infection.
- Ingrown nail edge: A visible portion of the nail edge is embedded into the surrounding skin.
- Pus or discharge (in advanced cases): Severe infections may produce pus or discharge from the affected area.
Other foot conditions that may cause similar symptoms include:
- Paronychia: An infection of the skin around the nail.
- Fungal nail infection (Onychomycosis): A fungal infection that can thicken and discolour the nail, sometimes leading to pain and inflammation.
- Psoriasis: This can also affect nails and cause similar pain, redness, and inflammation.
A podiatrist can accurately diagnose the condition through a thorough examination, considering the patient’s medical history and the symptoms presented. A visual inspection of the affected area, along with any accompanying symptoms, usually provides a definitive diagnosis.
Q 5. What are the potential complications of an untreated ingrown toenail?
Untreated ingrown toenails can lead to several complications, ranging from minor discomfort to serious health issues. These complications include:
- Infection: Bacteria can easily invade the affected area, causing a painful infection that may require antibiotics or surgical drainage. In severe cases, it could spread to other parts of the foot or body.
- Cellulitis: An infection of the deeper skin layers that can cause significant swelling, redness, and pain.
- Abscess formation: A collection of pus may form under the skin, requiring surgical incision and drainage.
- Lymphangitis: Inflammation of the lymphatic vessels, appearing as red streaks running up the leg from the infected area.
- Osteomyelitis: In rare cases, the infection can spread to the bone, resulting in a serious bone infection.
- Chronic pain: Repeated ingrown toenails can lead to chronic pain and discomfort.
Early treatment can significantly reduce the risk of these complications. Any signs of infection like increased pain, swelling, redness, or pus should prompt a visit to a healthcare professional.
Q 6. Explain your approach to managing pain associated with ingrown toenails.
Pain management for ingrown toenails is a critical aspect of treatment. My approach is multifaceted and tailored to the individual’s pain level and the severity of the condition.
- Conservative Measures: For mild cases, I advise patients to soak their feet in warm water, keep the area clean and dry, and use over-the-counter pain relievers such as ibuprofen or acetaminophen. Gently lifting the ingrown nail edge with cotton is also sometimes helpful.
- Local Anesthesia: For more severe cases requiring procedures like partial or complete nail avulsion, I administer local anesthesia to numb the affected area. This makes the procedure virtually painless.
- Prescription Medications: In cases of severe pain or infection, I may prescribe stronger pain medications or antibiotics to manage the symptoms and combat infection.
- Wound Care: After a procedure, meticulous wound care is essential to minimize pain and promote healing. Regular dressing changes and cleaning of the wound are crucial.
The goal is to provide effective pain relief while addressing the underlying cause of the ingrown toenail. I prioritize patient comfort and discuss appropriate pain management options to ensure a positive experience.
Q 7. Describe your experience with using different types of local anesthesia for ingrown toenail procedures.
My experience encompasses various types of local anesthetics used in ingrown toenail procedures. The choice of anesthetic depends on factors like the patient’s medical history, the extent of the procedure, and the patient’s preferences.
- Lidocaine: This is a widely used, commonly preferred and well-tolerated local anesthetic, often injected in a dilute solution to provide adequate numbness. Its effectiveness and relative safety make it a suitable choice for most procedures.
- Bupivacaine: A longer-acting anesthetic than lidocaine, bupivacaine can provide prolonged pain relief, particularly beneficial for post-procedure comfort. However, it may have a slightly slower onset of action.
- Combination Anesthetics: Some procedures may benefit from a combination of local anesthetics to leverage their different properties and achieve optimal pain control.
I always prioritize patient safety and carefully assess any allergies or contraindications before administering anesthesia. The injection technique itself is important to minimize discomfort and ensure complete numbing. I use small-gauge needles and inject slowly, paying close attention to the patient’s feedback during the process. Post-injection care instructions are always provided to the patient.
Q 8. How do you counsel patients on post-operative care for ingrown toenail surgery?
Post-operative care for ingrown toenail surgery is crucial for preventing complications and ensuring proper healing. My counseling emphasizes meticulous cleanliness and careful nail trimming. I instruct patients to keep the surgical site clean and dry, often recommending gentle washing with soap and water twice daily, followed by patting the area dry. Soaking the foot isn’t usually recommended unless explicitly instructed. I advise against using harsh soaps or lotions, which could irritate the sensitive skin. Patients are given detailed instructions on how to properly trim their nails straight across, avoiding digging into the corners, a common cause of recurrence. Pain management is addressed, providing guidance on over-the-counter pain relievers like ibuprofen or acetaminophen. We discuss the importance of keeping the affected toe elevated to reduce swelling and discomfort. Finally, I schedule a follow-up appointment to monitor healing progress and address any potential concerns. For example, I’ll often show patients the correct nail trimming technique using a visual aid. If there is significant swelling, I’ll advise them on how to use ice packs appropriately. Each patient receives a detailed, written care plan to reinforce the verbal instructions.
Q 9. What are the signs and symptoms of an infected ingrown toenail?
An infected ingrown toenail presents with several telltale signs and symptoms. The most obvious is significant pain, often throbbing and pulsating, localized around the affected nail edge. The area will typically be red, swollen, and warm to the touch. You’ll often see pus or a yellowish-white discharge. Sometimes there’s a noticeable change in skin color, with potential darkening of the skin adjacent to the nail. The toe may feel tender to the touch, and walking might become increasingly painful. In severe cases, fever, chills, or red streaks extending up the leg can indicate a more serious systemic infection requiring immediate medical attention. Think of it like this: the milder symptoms are like a low-grade warning, while the more severe symptoms are a full-blown alarm demanding immediate action.
Q 10. How do you manage an infected ingrown toenail?
Managing an infected ingrown toenail involves a multi-pronged approach. The first step is a thorough assessment of the infection’s severity. Mild infections can sometimes be managed conservatively with soaking, cleaning, and appropriate topical antibiotic creams. I frequently prescribe a course of oral antibiotics to tackle a systemic infection. Proper wound care is essential, which includes keeping the area clean and dry, regularly changing any dressings, and using appropriate antiseptic solutions. In cases of significant infection or the presence of pus, surgical debridement might be necessary. This procedure involves removing the infected portion of the nail, relieving pressure, and allowing drainage. If there’s evidence of cellulitis or systemic infection, immediate referral to a specialist might be required for intravenous antibiotics. The goal is to eradicate the infection, prevent its spread, and alleviate the patient’s pain and discomfort. Regular monitoring of the affected toe is critical during the treatment process.
Q 11. What are the different types of topical and oral antibiotics used for ingrown toenail infections?
The choice of topical and oral antibiotics for ingrown toenail infections depends on the severity of the infection and the patient’s medical history. Topical antibiotics commonly used include bacitracin and mupirocin ointments. These are applied directly to the affected area to control local infection. For oral antibiotics, I might prescribe amoxicillin-clavulanate, cephalexin, or clindamycin, depending on the pathogen suspected and the patient’s allergies. The selection process involves considering the patient’s allergies, previous antibiotic use, and the potential for drug interactions. For example, a patient with a penicillin allergy would not be prescribed amoxicillin-clavulanate. Always ensuring the correct dosage and duration of treatment is paramount. The decision about which antibiotic to use is tailored to each patient and the specifics of their case.
Q 12. Discuss your experience with conservative management of ingrown toenails.
Conservative management of ingrown toenails is my first line of defense when dealing with uncomplicated cases. This approach focuses on alleviating pain and promoting healing without surgical intervention. It typically starts with meticulous cleansing of the affected area using warm water and mild soap. Soaking the toe in warm Epsom salt water multiple times a day helps to soften the nail and reduce inflammation. Gentle elevation of the affected limb also minimizes swelling. I then use a cotton wisp or a small piece of sterile gauze to lift the ingrown edge of the nail away from the surrounding skin, thus relieving pressure. This technique often requires repeated adjustments and ongoing care from the patient at home. Topical antibiotic creams are frequently applied to help prevent infection. In cases where the pressure is substantial, I will also trim back the sharp edge of the ingrown nail with proper instruments. The success rate of conservative management depends on the severity of the ingrown toenail and the patient’s diligence in following home care instructions. However, it’s crucial to emphasize that if conservative measures fail to improve the condition, surgical intervention is necessary.
Q 13. Explain your approach to managing recurrent ingrown toenails.
Recurrent ingrown toenails are a frustrating problem for both the patient and the clinician. My approach focuses on identifying and addressing the underlying cause, which is often improper nail trimming. I provide extensive patient education on correct nail trimming techniques, emphasizing trimming straight across and avoiding rounding the corners. In many cases, I recommend regular professional nail trimming to ensure the correct technique is maintained. For patients with persistent recurrence, I may suggest a partial or total nail avulsion, a surgical procedure where a portion or all of the affected nail is removed. In some instances, a chemical matrixectomy using phenol injection is also a viable option. This helps destroy the nail matrix, the part responsible for nail growth, reducing the chances of recurrence. The choice of management for recurrent ingrown toenails is individualised and depends on the severity of the recurrence and the patient’s preferences. Post-operative care and patient education are crucial to prevent future problems.
Q 14. Describe the procedure for applying a phenol injection to treat ingrown toenails.
Phenol injection is a minimally invasive procedure used to treat recurrent ingrown toenails. The procedure begins with thorough cleaning and sterilization of the affected area. Local anesthesia is administered to numb the region around the nail matrix. A small gauge needle is then used to inject a precise amount of phenol solution directly into the nail matrix, aiming to destroy the tissue responsible for nail growth in the affected area. The amount of phenol and the injection technique are carefully considered, ensuring that the surrounding tissue is not damaged. After the injection, the area is covered with a sterile dressing. Patients are instructed on post-operative care, which typically involves keeping the area clean and dry and avoiding activities that put undue pressure on the toe. The procedure is generally well-tolerated; however, some discomfort and mild swelling are expected. The treatment can reduce or eliminate the nail’s regrowth in the area where it was previously ingrown, mitigating future recurrences. The success of the procedure and the eventual healing are monitored through regular follow-up visits.
Q 15. What is your experience with using chemical cauterization for ingrown toenail treatment?
Chemical cauterization, using agents like phenol or silver nitrate, is a technique I’ve employed in managing ingrown toenails, particularly in cases of recurring ingrowth or when the nail is severely embedded. It involves carefully applying the chemical to the nail matrix (the area where the nail grows from), aiming to destroy the part of the matrix causing the ingrowth. This effectively slows or stops the growth of the offending portion of the nail.
My experience shows that it’s a minimally invasive procedure, typically performed in the office under local anesthesia. It’s particularly useful in avoiding the need for more extensive surgery, especially for patients who are high-risk or have a preference for less invasive options. However, it’s crucial to manage expectations; while often effective, it’s not a guaranteed cure, and multiple treatments might be necessary. Proper technique is essential to avoid damaging surrounding tissue, and I always meticulously assess the patient’s overall health and suitability before proceeding.
For example, I recently used phenol cauterization on a patient with a chronically ingrown toenail who had previously undergone surgery with unsatisfactory results. The procedure was well-tolerated, and the patient experienced a significant reduction in pain and discomfort. Follow-up care included regular nail trimming and keeping the area clean to minimize the risk of infection.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience with the use of nail splints or braces.
Nail splints or braces are another valuable tool in my arsenal for treating ingrown toenails. These devices gently lift the edge of the ingrown nail away from the surrounding soft tissue, allowing the skin to heal. They’re particularly useful in less severe cases or as an adjunct to other treatments. The splints are usually made of thin, flexible materials and are bonded to the nail plate.
In my practice, I’ve found that nail splints are an excellent conservative management option, offering a non-surgical approach with minimal discomfort. Patients generally find them comfortable and easy to use. I explain the proper application and aftercare, emphasizing the importance of keeping the splint clean and dry.
For instance, I recently fitted a young patient with a minor ingrown toenail with a temporary nail splint. Within a few weeks, the nail had grown out correctly, and the inflammation resolved completely. It was a simple, effective solution that avoided the need for surgery.
Q 17. How do you assess the patient’s suitability for conservative versus surgical treatment?
Assessing patient suitability for conservative versus surgical treatment hinges on several factors. I consider the severity of the ingrowth, the presence of infection, the patient’s overall health, and their preferences.
- Mild ingrown toenails, with minimal inflammation and pain, often respond well to conservative measures like nail trimming, soaking, and the use of splints.
- Severe cases with significant inflammation, infection (signs like purulent discharge, redness, swelling, increased warmth, or pain), or recurrent ingrowths may necessitate surgical intervention, such as partial nail avulsion or matrixectomy.
- Patient-specific factors such as diabetes, peripheral vascular disease, or immunocompromise significantly impact treatment decisions, often favoring conservative approaches to mitigate risks.
I engage patients in a thorough discussion, explaining the risks and benefits of each approach before making a joint decision. It’s essential for them to understand their role in successful treatment, including meticulous foot care and follow-up appointments.
Q 18. What are the contraindications for surgical removal of an ingrown toenail?
Several contraindications exist for surgical removal of an ingrown toenail. These include:
- Poor peripheral circulation: Patients with severe peripheral artery disease (PAD) are at increased risk of poor wound healing and infection post-surgery.
- Uncontrolled diabetes: High blood glucose levels impair wound healing and increase the risk of infection. Optimal diabetic control is crucial before considering surgery.
- Active infection: Surgery is generally postponed until the infection is adequately controlled with antibiotics.
- Bleeding disorders: Patients with clotting disorders need careful evaluation and management before undergoing any procedure.
- Immunocompromised states: Patients with weakened immune systems are at a higher risk of complications post-surgery.
I always perform a thorough medical history review and physical examination to identify any of these contraindications before planning any surgical intervention. Patient safety is my highest priority, and surgery is only recommended when the benefits outweigh the risks significantly.
Q 19. How do you manage complications following ingrown toenail surgery?
Managing complications following ingrown toenail surgery is crucial. Potential complications include infection, bleeding, pain, and recurrence.
Post-operative care typically includes:
- Pain management: Prescribing analgesics to control post-operative pain.
- Wound care: Providing detailed instructions for keeping the wound clean and dry, regularly changing dressings, and monitoring for signs of infection.
- Infection control: Prescribing antibiotics if an infection develops.
- Regular follow-up: Scheduling follow-up appointments to monitor healing progress and address any issues promptly.
For example, if a patient develops signs of infection such as increased pain, swelling, redness, or pus, I would immediately prescribe antibiotics, possibly perform wound debridement if necessary, and closely monitor the situation. Early intervention is key in preventing more severe complications.
Q 20. What is your experience with managing patients with diabetes who have ingrown toenails?
Managing ingrown toenails in patients with diabetes requires a particularly cautious approach. Diabetic patients have impaired wound healing and are at a higher risk of infection.
My approach emphasizes:
- Meticulous foot care education: Patients must be thoroughly educated on proper foot hygiene and daily inspection for any signs of injury or infection.
- Conservative treatment preference: I typically prefer conservative management techniques such as nail trimming, soaking, and splints whenever possible, to minimize the risk of complications.
- Strict glycemic control: Optimal blood glucose levels are crucial for wound healing. Close collaboration with the patient’s primary care physician or endocrinologist is vital.
- Prompt attention to any signs of infection: Even minor signs of infection must be addressed immediately with appropriate antibiotic therapy and, if necessary, surgical debridement.
For instance, a diabetic patient with a mildly ingrown toenail would receive detailed instructions on foot care and would be closely monitored for any signs of infection. I would only consider surgical intervention as a last resort after careful assessment and in close consultation with their primary care physician to ensure optimal blood glucose levels.
Q 21. What specific knowledge do you have regarding fungal infections related to ingrown toenails?
Fungal infections, such as onychomycosis (nail fungus), can complicate ingrown toenails. The presence of a fungal infection can impair nail health, making it more brittle and prone to ingrowth. Additionally, the presence of a compromised nail can create an environment conducive to fungal growth.
My approach involves:
- Proper diagnosis: Differentiating fungal infection from other nail conditions through clinical examination and potentially laboratory testing (e.g., KOH preparation or fungal culture).
- Treatment of the fungal infection: Using appropriate antifungal medications, either topical or oral, depending on the severity and extent of the infection. Treatment duration is typically longer than for uncomplicated onychomycosis.
- Addressing the ingrown nail: Managing the ingrown nail itself with conservative or surgical methods, once the fungal infection is under control.
For example, a patient presenting with an ingrown toenail and visible signs of onychomycosis (thickened, discolored nail) would first undergo treatment for the fungal infection. Only after significant improvement in the nail’s condition would I proceed with addressing the ingrown toenail, possibly with a less invasive approach like a nail splint or cauterization, rather than surgery.
Q 22. How do you educate patients about preventative measures for ingrown toenails?
Preventing ingrown toenails starts with proper nail hygiene and footwear choices. I educate my patients on the importance of trimming their toenails straight across, avoiding curved cuts that can lead to the nail digging into the skin. We discuss the significance of wearing shoes that fit properly, avoiding shoes that are too tight or too narrow. This prevents pressure on the nail and allows for proper blood circulation.
- Proper Trimming: I demonstrate the correct technique using a sharp nail clipper, emphasizing cutting straight across and avoiding rounding the corners. I explain that this prevents the nail from growing into the surrounding skin.
- Appropriate Footwear: We discuss the importance of wearing shoes that are the correct size and width, with enough room for the toes to move freely. Athletic shoes, or shoes with a wide toe box are ideal. I advise against consistently wearing tight, pointed-toe shoes.
- Hygiene: Maintaining clean, dry feet is crucial. I recommend daily washing with soap and water, ensuring the area between the toes is thoroughly cleaned and dried. This prevents fungal infections which can exacerbate ingrown nails.
- Diabetic Foot Care: For patients with diabetes, I emphasize the added importance of meticulous foot care, as they are at higher risk for complications. Regular checks for any signs of infection or damage are highly recommended.
By emphasizing these preventative measures, I empower my patients to take control of their nail health and reduce the risk of developing ingrown toenails.
Q 23. Describe your experience with using different types of surgical instruments used during ingrown toenail surgery.
My experience encompasses a wide range of surgical instruments used in ingrown toenail surgery. The choice of instrument depends on the severity of the ingrown toenail and the individual patient’s needs. Commonly used instruments include:
- Scalpels: Used for precise incision and removal of the affected portion of the nail. Different blade sizes allow for adaptability to different nail thicknesses and ingrown depths.
- Nail Avulsion Forceps: These specialized forceps are used to gently remove the ingrown portion of the nail, minimizing trauma to the surrounding tissue.
- Curettes: Small, spoon-shaped instruments used to clean out any granulation tissue or debris from under the nail.
- Electrocautery: This is sometimes used for hemostasis (to stop bleeding) and to help cauterize small blood vessels to prevent post-operative bleeding.
- Nail Matrixectomy Instruments: In cases of recurrent ingrown toenails, phenol or chemical matrixectomy may be employed. Specialized instruments are used to accurately apply the chemical to the nail matrix, which produces long-term results by reducing or halting nail regrowth in a portion of the nail bed.
I’m experienced in using these instruments with precision and care, prioritizing minimal discomfort and optimal cosmetic outcomes for my patients. Choosing the right instrument is crucial for ensuring a clean and successful surgical procedure and requires a deep understanding of anatomy and surgical technique.
Q 24. What is the post-operative care following ingrown toenail surgery?
Post-operative care for ingrown toenail surgery is critical for a successful outcome and preventing complications. My instructions always include:
- Wound Cleaning: Daily cleaning of the surgical site with soap and water is essential to prevent infection. I often recommend using an antiseptic solution as well.
- Dressing Changes: Depending on the extent of the surgery, I may instruct the patient on how to change the dressing, or they may be seen for dressing changes in the office. Proper wound dressing ensures a clean environment to support healing.
- Pain Management: Over-the-counter pain relievers such as ibuprofen or acetaminophen are usually sufficient to manage any post-operative pain. If the patient requires stronger medication, a prescription will be given.
- Elevation: Elevating the foot helps reduce swelling and discomfort. I explain the importance of keeping the foot elevated as much as possible during the initial recovery period.
- Follow-up Appointments: Regular follow-up appointments are scheduled to monitor healing progress and address any concerns.
- Avoidance of Tight Shoes: Patients are advised to avoid wearing tight shoes or socks that might put pressure on the surgical site.
- Signs of Infection: I clearly outline signs of infection (increased pain, swelling, redness, or pus) and instruct the patient to seek immediate medical attention if any of these occur.
Providing clear and detailed instructions ensures that the patients understand how to manage their post-operative care effectively and contribute to optimal healing.
Q 25. What are some long term solutions to prevent future ingrown toenails?
Long-term solutions for preventing future ingrown toenails focus on addressing the underlying causes. These strategies aim to prevent recurrence and improve overall nail health.
- Consistent Nail Trimming: This remains the cornerstone of prevention. Patients should be educated on the importance of regularly trimming their toenails straight across and using appropriate nail clippers.
- Proper Footwear: Choosing shoes with ample toe space is essential. Tight-fitting shoes can compress the toes and exacerbate ingrown nails. I encourage patients to examine their footwear habits.
- Regular Foot Care: Maintaining good foot hygiene, including regular washing and drying, prevents infections that could worsen ingrown nails.
- Orthonyxic Procedure: For recurring ingrown toenails, an orthonyxic procedure is a potential solution. This involves placing a small splint or bracket under the corner of the nail to lift it away from the skin. It’s a less invasive procedure than matrixectomy, but may not be as effective.
- Partial Nail Avulsion/Matrixectomy: For severe or recurrent cases, surgical intervention might be necessary. This could involve partial or complete removal of the nail (avulsion), or more frequently a partial removal of the nail matrix (matrixectomy) to reduce or stop nail regrowth in a portion of the nail bed.
Combining these preventative measures provides a comprehensive approach to prevent future ingrown toenail issues. Patient education is critical to the success of these long-term solutions.
Q 26. How do you document and chart ingrown toenail treatment?
Documentation of ingrown toenail treatment is meticulous and detailed. My charting follows a structured format and includes:
- Patient Demographics: Name, date of birth, medical record number, etc.
- Presenting Complaint: Detailed description of the patient’s symptoms, including the duration and severity of the ingrown toenail.
- Physical Examination Findings: Documentation of the physical exam, including the location, severity, and any signs of infection.
- Diagnosis: ICD-10 code for ingrown toenail (e.g., L60.1).
- Treatment Plan: Details of the chosen treatment, whether conservative or surgical. For surgical procedures, the specific instruments used are documented. Post-op instructions provided are also documented.
- Post-Operative Care Instructions: Detailed description of the post-operative instructions given to the patient including wound care, pain management, and follow-up appointments.
- Progress Notes: Subsequent visits are documented, noting healing progress, any complications, and modifications to the treatment plan.
- Imaging: If relevant, any imaging results (X-rays, etc.) are included in the chart.
Thorough documentation is vital for continuity of care, communication with other healthcare providers, and legal protection. A clear and concise record ensures that the patient’s treatment is well-documented and easily accessible.
Q 27. Describe your experience with managing patient expectations for ingrown toenail treatment.
Managing patient expectations is crucial for a positive experience. I begin by providing a thorough explanation of the condition, the various treatment options, and the potential outcomes for each. I always involve the patient in shared decision-making, helping them to choose the treatment path best suited to their needs and preferences. I clearly outline the possible risks and benefits of each procedure.
For example, I explain that while surgical treatment usually resolves the ingrown toenail, it might involve some discomfort and a period of healing. I also mention the possibility of recurrence, especially if the patient doesn’t follow post-operative instructions carefully. For conservative management options, I set realistic expectations about the healing time and possibility of needing surgical intervention if the condition doesn’t improve.
By communicating honestly and openly, building rapport with patients, and setting realistic expectations, I aim to minimize misunderstandings and foster trust.
Q 28. What are the common billing codes for ingrown toenail procedures?
Billing codes for ingrown toenail procedures vary depending on the specific services provided and the level of complexity. Common CPT (Current Procedural Terminology) codes used include:
- 11750: Removal of ingrown toenail, partial or complete, simple.
- 11751: Removal of ingrown toenail, partial or complete, complex.
- 11760: Partial avulsion of nail.
- 11761: Total avulsion of nail.
- 11762: Nail bed cautery.
- 11763: Surgical removal of nail matrix.
The correct code is selected based on the exact procedure performed. It’s crucial to accurately reflect the work done for appropriate reimbursement. Modifiers may also be added depending on circumstances. It is advisable to check the most up-to-date CPT codes with your billing service to ensure accuracy.
Key Topics to Learn for Ingrown Toenails Treatment Interview
- Anatomy and Physiology of the Toe Nail: Understanding the structure and function of the nail unit is crucial for diagnosing and treating ingrown toenails. This includes knowledge of the nail matrix, nail bed, and surrounding tissues.
- Diagnosis of Ingrown Toenails: Learn to differentiate between various stages of ingrown toenails, identifying associated complications like infection or inflammation. Practice accurate assessment techniques.
- Conservative Treatment Methods: Master the techniques of proper nail trimming, soaking, and the use of topical treatments to manage mild ingrown toenails. Understand when these methods are appropriate and their limitations.
- Surgical Techniques (Partial or Complete Nail Avulsion): If conservative methods fail, familiarity with different surgical approaches, including chemical matricectomy and partial or complete nail avulsion, is essential. Understand the indications, contraindications, and post-operative care for each.
- Infection Management and Prevention: Learn to recognize signs of infection and implement appropriate treatment strategies, including antibiotic therapy and wound care. Understand the importance of preventative measures.
- Patient Education and Communication: Effective communication with patients is paramount. This includes explaining treatment options, managing expectations, and providing clear post-operative instructions for optimal healing.
- Post-Operative Care and Wound Healing: Understand the principles of wound healing and how to manage potential complications like bleeding, infection, and pain after surgical intervention.
- Common Complications and their Management: Be prepared to discuss potential complications such as recurrent ingrown toenails, granulomas, and chronic pain, and how to address them.
- Ethical Considerations and Professional Standards: Understand the ethical considerations related to patient care, informed consent, and maintaining professional standards in the treatment of ingrown toenails.
Next Steps
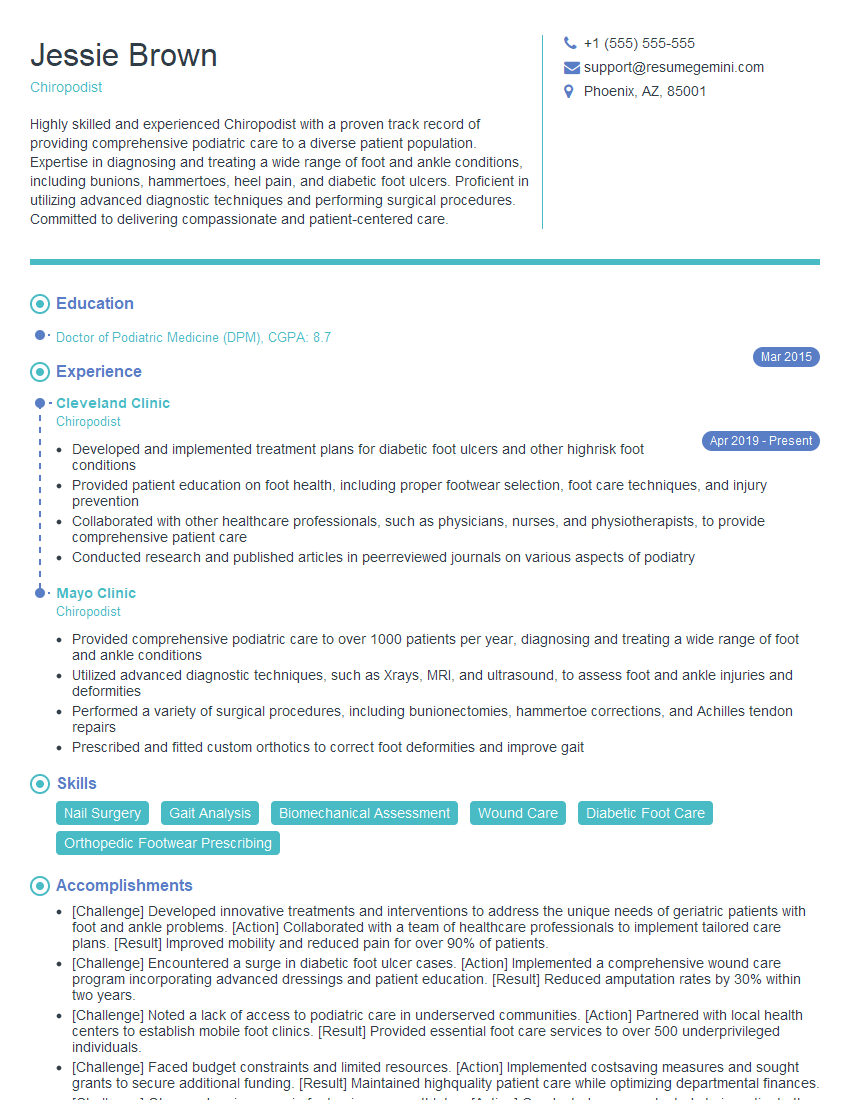
Mastering ingrown toenail treatment demonstrates a valuable skillset highly sought after in podiatry and related medical fields. This expertise significantly enhances your career prospects, opening doors to diverse and rewarding opportunities. To maximize your chances of landing your dream job, crafting an ATS-friendly resume is crucial. ResumeGemini is a trusted resource that can help you build a professional, impactful resume that highlights your skills and experience effectively. ResumeGemini provides examples of resumes tailored to Ingrown Toenails Treatment to further assist you in your job search.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.