Unlock your full potential by mastering the most common Orthotics and Footwear Modification interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Orthotics and Footwear Modification Interview
Q 1. Explain the difference between custom and prefabricated orthotics.
The primary difference between custom and prefabricated orthotics lies in their manufacturing process and level of personalization. Custom orthotics are individually crafted for a specific patient, using a plaster or foam cast of their foot to create a precise, mirror image. This ensures a perfect fit and addresses the patient’s unique biomechanical needs. Prefabricated orthotics, on the other hand, are mass-produced in standard sizes. While they can offer some support, they lack the tailored precision of custom orthotics and may not effectively address complex foot problems. Think of it like this: custom orthotics are like bespoke tailoring, perfectly fitted to your individual measurements, while prefabricated orthotics are like off-the-rack clothing – they might fit adequately, but not perfectly.
Q 2. Describe the process of casting a patient’s foot for a custom orthotic.
Casting a patient’s foot for a custom orthotic is a meticulous process requiring precision and attention to detail. First, the patient’s lower limb is carefully positioned to achieve optimal weight-bearing. Then, a thin layer of foam padding is applied to protect the skin and ensure comfort. Next, a plaster bandage or foam material is applied, building up layers to create a rigid mold of the foot and ankle in a weight-bearing position. The material is allowed to set completely, and then the mold is carefully removed. It’s crucial to ensure the cast accurately represents the patient’s foot shape and any existing deformities. Any imperfections in the cast will directly impact the functionality and fit of the finished orthotic. Finally, the mold is prepared for the orthotic fabrication process, which might involve creating a positive model from the negative cast.
Q 3. What materials are commonly used in orthotic fabrication, and what are their respective advantages and disadvantages?
Numerous materials are used in orthotic fabrication, each with its own advantages and disadvantages. Common materials include:
- EVA (Ethylene-vinyl acetate): A lightweight, flexible material often used in accommodative orthotics. Advantages: Comfortable, shock-absorbing. Disadvantages: Not suitable for high-impact activities or significant structural support needs.
- Polypropylene: A semi-rigid material that offers good support and durability. Advantages: Provides moderate support, relatively inexpensive. Disadvantages: Less adaptable to complex foot shapes than other materials.
- Carbon fiber: A strong, lightweight material offering high levels of support. Advantages: Excellent for high-impact activities and significant structural corrections. Disadvantages: Can be expensive and less comfortable than other materials.
- Leather: A traditional material known for its breathability and conformability. Advantages: Comfortable, breathable. Disadvantages: Requires more maintenance, can be less durable than synthetic materials.
The choice of material depends on the patient’s specific needs and the type of orthotic being fabricated. For example, a patient with plantar fasciitis might benefit from a soft EVA orthotic, while an athlete with severe foot pronation might require a more rigid carbon fiber orthotic.
Q 4. How do you assess a patient’s gait and biomechanics to determine the appropriate orthotic prescription?
A thorough gait and biomechanical assessment is crucial for determining the appropriate orthotic prescription. This involves a combination of observation, palpation, and measurement. We observe the patient’s gait during walking, running, and other activities, looking for abnormalities such as excessive pronation, supination, or limited ankle dorsiflexion. Palpation helps assess the condition of the soft tissues and identify areas of tenderness or muscle imbalance. Range of motion measurements are taken to assess the flexibility of the joints. We also use tools such as pressure plates or gait analysis systems to obtain quantitative data on foot pressure distribution and movement patterns. This comprehensive assessment provides a detailed understanding of the patient’s biomechanics, informing the design and prescription of the most effective orthotic.
Q 5. Describe different types of orthotic designs and their indications (e.g., UCBL, semi-rigid, accommodative).
Orthotic designs vary based on the level of support and correction needed:
- Accommodative Orthotics: These are typically soft, flexible devices used to relieve pressure and provide cushioning. They’re indicated for patients with conditions like plantar fasciitis or diabetic neuropathy.
- Semi-rigid Orthotics: These offer a balance of support and flexibility, addressing mild to moderate biomechanical issues. They are suitable for patients with metatarsalgia, mild pronation, or mild to moderate plantar fasciitis.
- Rigid Orthotics (e.g., UCBL): These are firm devices often used for significant structural corrections. UCBL (University of California Biomechanics Laboratory) orthotics are a well-known example, providing substantial control over foot motion and are used for conditions like pes cavus (high arch) or severe pronation.
The selection of the appropriate design depends heavily on the patient’s diagnosis, their activity level, and the severity of their biomechanical issues.
Q 6. Explain the role of different components within an orthotic device (e.g., heel cup, medial post, metatarsal pad).
Each component of an orthotic plays a specific role in supporting the foot and correcting biomechanical abnormalities:
- Heel Cup: Provides stability and support for the heel, influencing the overall alignment of the foot and ankle.
- Medial Post: A wedge-shaped component placed on the inside of the heel to control excessive pronation (inward rolling of the foot). It helps to support the arch and stabilize the foot.
- Metatarsal Pad: Provides cushioning and support to the ball of the foot, relieving pressure and alleviating metatarsalgia.
- Longitudinal Arch Support: Supports the arch of the foot, improving alignment and reducing strain on the plantar fascia.
The combination and size of these components are customized to meet the individual needs of the patient, as identified through the biomechanical assessment.
Q 7. How do you address common orthotic-related patient issues, such as skin irritation or discomfort?
Addressing common orthotic-related issues requires careful consideration and a patient-centered approach. Skin irritation is often caused by friction or pressure. We can manage this by suggesting the use of appropriate socks, ensuring proper fit and adjusting the orthotic as needed. For example, adding additional padding or modifying the edges of the orthotic can alleviate pressure points. Discomfort can stem from improper fit, incorrect material selection, or an abrupt transition to orthotic use. We address discomfort through a combination of adjusting the orthotic, recommending a gradual wear schedule, and recommending over-the-counter pain relievers. Open communication with the patient is key to identifying the source of their discomfort and tailoring solutions to meet their specific needs. We might also reassess the patient’s gait to ensure the orthotic continues to be appropriate for their needs.
Q 8. How do you modify footwear to accommodate orthotic devices?
Modifying footwear to accommodate orthotic devices often involves creating space and ensuring proper support. This isn’t simply about shoving an orthotic into any shoe; it’s a precise process. We assess the orthotic’s shape and thickness, then consider the shoe’s design and material.
Common modifications include:
- Depth Modification: If the orthotic is thick, we might remove the insole or part of it to create enough depth. Sometimes, we need to stretch the shoe’s upper material to accommodate the increased volume.
- Length and Width Adjustment: Depending on the patient’s foot shape and the orthotic design, we may need to stretch the shoe’s length or width to provide a comfortable fit. We use specialized stretching tools and techniques to avoid damaging the shoe’s structure.
- Heel Counter Modification: The heel counter (the back part of the shoe) might need modification to ensure proper heel support and alignment with the orthotic.
- Padding: Strategic padding can help address pressure points created by the orthotic or the shoe’s structure. We use various padding materials, selecting those appropriate for the patient’s needs and the shoe’s material.
- Custom Inserts: In some cases, we create custom inserts to improve the fit and comfort, working in conjunction with the orthotic.
For example, a patient with a high arch might need a shoe with a deeper heel cup to accommodate both the orthotic and the arch itself. We might also use padding to alleviate pressure points near the metatarsal heads.
Q 9. What are the common causes of foot deformities, and how can orthotics help to manage them?
Foot deformities can stem from various causes, including genetics, trauma, neurological conditions, and diseases like diabetes. Common deformities include bunions (hallux valgus), hammertoes, flat feet, and plantar fasciitis.
- Bunions (Hallux Valgus): Develop due to a combination of genetic predisposition, ill-fitting shoes, and biomechanical factors. Orthotics can help alleviate pain by supporting the metatarsophalangeal joint and reducing pressure on the bunion.
- Hammertoes: Characterized by a bent toe joint. Orthotics offer cushioning and support to prevent further deformity and reduce pain.
- Flat Feet (Pes Planus): Occur when the arch collapses. Orthotics provide arch support, helping redistribute weight and reduce strain on muscles and ligaments.
- Plantar Fasciitis: Inflammation of the plantar fascia, a band of tissue on the bottom of the foot. Orthotics can help alleviate pain by providing arch support and cushioning.
Orthotics work by providing structural support, cushioning, and correcting biomechanical imbalances. They don’t ‘cure’ the deformity but significantly improve pain management and help prevent further progression in many cases. It’s important to remember that treatment often requires a holistic approach that combines orthotics with other therapies like physiotherapy or medication.
Q 10. Describe your experience with different types of footwear modifications (e.g., stretching, adding padding, altering shoe structure).
My experience encompasses a wide range of footwear modifications. I’ve worked with various materials and techniques, adapting my approach depending on the patient’s needs and the shoe’s properties.
- Stretching: I use both heat-based and mechanical stretching techniques to increase the length and width of shoes. Heat-based methods involve applying heat to specific areas of the shoe to soften the material, making it more pliable. Mechanical stretching employs tools to gently expand the shoe’s structure. This is carefully done to avoid structural damage.
- Padding: I use various padding materials, such as foams, gels, and felt, to create cushioning and reduce pressure points. The selection of padding is crucial, considering factors like breathability and durability. For instance, a diabetic patient might require extra cushioning and non-irritating materials to prevent ulcer formation.
- Altering Shoe Structure: In some cases, I may need to make more significant alterations, such as removing parts of the insole, adjusting the heel height, or even modifying the shoe’s upper to accommodate orthotics and the patient’s foot shape. This usually involves meticulous craftsmanship and specialized tools.
Each modification requires a detailed assessment of the patient’s needs and the shoe’s material. For example, a delicate leather shoe will require different techniques compared to a more robust athletic shoe. Proper training and experience are essential to ensure the effectiveness and safety of the modifications.
Q 11. How do you select appropriate footwear for patients with specific foot conditions?
Selecting appropriate footwear involves a thorough assessment of the patient’s condition, foot type, and activity level. It’s a collaborative process involving patient input and professional judgment.
- Foot Condition Assessment: We start by evaluating the specific foot condition (e.g., plantar fasciitis, bunions, diabetes). The severity and location of symptoms will strongly influence our recommendations.
- Foot Type Analysis: We determine the patient’s foot type (high arch, normal arch, flat foot) and consider any pre-existing deformities. This assessment guides the selection of shoes that provide appropriate support and cushioning.
- Activity Level Consideration: The patient’s daily activities (walking, running, standing) impact shoe selection. An individual who stands for long hours will require different footwear from a runner.
- Shoe Features Assessment: We evaluate key features such as arch support, heel counter support, outsole flexibility, and shoe width. We also look at material breathability, especially for patients with diabetes.
For example, a patient with plantar fasciitis would benefit from shoes with good arch support, deep heel cups, and shock-absorbing midsoles. A diabetic patient would need shoes that provide ample space to prevent pressure points and made from breathable materials to avoid moisture buildup.
Q 12. What are the ethical considerations in orthotic and footwear modification practice?
Ethical considerations in orthotic and footwear modification are paramount. We must prioritize patient safety and well-being above all else.
- Informed Consent: Patients must fully understand the proposed modifications, their potential benefits and risks, and any alternative treatment options. We need to obtain their informed consent before proceeding.
- Competence and Expertise: We must only undertake modifications within our scope of practice, referring patients to other specialists as needed. Ongoing professional development is crucial to maintain our competence.
- Honesty and Transparency: We must be honest about the limitations of our modifications and avoid making unrealistic promises. We must be transparent about costs and billing practices.
- Confidentiality: Patient information must be kept confidential and handled according to relevant data protection regulations.
- Evidence-Based Practice: We should base our recommendations on current research and evidence-based practice, avoiding treatments lacking scientific support.
For instance, we should avoid modifying shoes beyond our capabilities, potentially harming the patient or the shoe’s integrity. We should also clearly communicate any potential limitations of our interventions, ensuring that patients have realistic expectations.
Q 13. Explain the importance of proper patient education regarding orthotic use and care.
Proper patient education is critical for successful orthotic use and care. It ensures patients understand how to use their orthotics effectively and maintain them properly.
- Orthotic Use Instructions: We explain how to properly insert and remove the orthotics, ensuring a secure and comfortable fit. We address common issues like pressure points and discomfort.
- Orthotic Care Instructions: We teach patients how to clean and maintain their orthotics to prevent wear and tear and maintain hygiene. This involves using appropriate cleaning methods and materials.
- Foot Care Education: We emphasize proper foot care practices, especially crucial for patients with diabetes or other conditions that increase the risk of foot ulcers. This includes daily foot inspections, proper hygiene, and moisturizing.
- Follow-up Appointments: Regular follow-up appointments are crucial to monitor the patient’s progress, address any concerns, and make necessary adjustments to the orthotics or footwear.
For example, we explain that daily inspection of feet is essential for early detection of any problems, such as blisters or sores. We might also provide written instructions or visual aids to support learning.
Q 14. How do you manage patients with specific conditions like plantar fasciitis, hallux valgus, or diabetic foot ulcers?
Managing patients with specific conditions requires a tailored approach combining orthotics, footwear modification, and other therapeutic interventions.
- Plantar Fasciitis: Treatment focuses on reducing inflammation and supporting the plantar fascia. Orthotics with good arch support and cushioning are essential, along with stretching exercises and sometimes medication.
- Hallux Valgus (Bunions): We use orthotics to provide metatarsal support and reduce pressure on the bunion. Shoe modifications, such as increased width, may also be necessary. In severe cases, surgical intervention might be considered.
- Diabetic Foot Ulcers: Management is critical to prevent complications. We use custom-molded orthotics to redistribute pressure, preventing ulcer formation or recurrence. Footwear modifications are crucial to ensure ample space and protection. Close monitoring and wound care are essential.
Each patient requires an individualized treatment plan. For example, a diabetic patient with an ulcer may need specialized footwear and orthotics made from offloading materials to minimize pressure on the affected area. Regular monitoring and collaboration with other healthcare professionals, such as podiatrists or diabetologists, is paramount.
Q 15. Describe your experience with using different types of measuring tools and assessment technologies.
Accurate measurement is fundamental to successful orthotic and footwear modification. My experience encompasses a wide range of tools, from traditional methods to advanced technologies. This includes using:
- Foot length and width measurements: Using a Brannock device for standardized measurements, and manually measuring using a ruler for specific areas of concern.
- Plantar pressure measurement systems: Incorporating both static and dynamic plantar pressure systems (e.g., Pedar, Tekscan) to analyze weight distribution and identify areas of high pressure, which inform orthotic design.
- Goniometers and inclinometers: Used to quantify joint range of motion (ROM) in the ankles, knees, and hips, critical for determining the need for specific orthotic features like joint articulation.
- Three-dimensional (3D) scanning systems: Utilizing various 3D scanning technologies to capture detailed anatomical information of the foot and lower limb, providing highly accurate data for CAD/CAM orthotic fabrication.
Understanding the strengths and limitations of each tool is crucial. For example, while a Brannock device offers standardized measurements, manual measurements are necessary to detect subtle asymmetries or deformities. Similarly, 3D scanning provides unparalleled detail but requires careful post-processing and may not always be necessary for simpler cases.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you document patient assessments and treatment plans?
Comprehensive documentation is essential for effective patient care and communication. My approach integrates both subjective and objective data. Patient assessments are meticulously documented using a standardized form that includes:
- Patient demographics and medical history: Including relevant diagnoses, medications, and previous treatments.
- Subjective findings: Detailed notes from the patient’s description of their symptoms, pain location, and functional limitations.
- Objective findings: Quantitative measurements (e.g., foot length, width, ROM, plantar pressure data) and qualitative observations (e.g., gait analysis, presence of deformities).
- Diagnosis and treatment plan: A clear statement of the diagnosed condition(s) and the proposed treatment plan, including the type of orthotic, materials, and modification details.
- Progress notes: Regular updates documenting the patient’s response to treatment, adjustments made to the orthotic, and any modifications to the treatment plan.
All documentation is stored securely in the patient’s electronic medical record (EMR) and conforms to relevant privacy regulations (e.g., HIPAA).
Q 17. What is your experience with different types of casting materials and techniques?
My experience spans various casting materials and techniques, each chosen strategically based on the patient’s needs and the desired orthotic properties. These include:
- Plaster of Paris: A traditional material offering good detail and support, but can be messy and time-consuming.
- Positive-mold casting: Direct casting of the foot, providing a precise representation of the foot’s contours. I use this for patients requiring custom orthotics.
- Foam box casting: A faster method for obtaining a positive cast, useful when a quicker turnaround is required.
- Thermoplastic materials: Such as polypropylene or polyethylene, offering advantages like reusability, ease of modification, and durability. I often use these for vacuum-formed orthotics or orthoses.
- Digital scanning: Eliminates the need for traditional casting, generating a digital model for direct manufacturing. This is particularly useful for complex cases or when high precision is required.
The selection of casting materials and techniques always prioritizes patient comfort and accurate reproduction of the foot’s anatomy to ensure the effectiveness of the final orthotic.
Q 18. How do you ensure the proper fit and function of orthotic devices?
Ensuring proper fit and function is paramount. This involves a multi-step process starting with accurate assessment and culminating in ongoing monitoring. This includes:
- Initial fitting and adjustments: The orthotic is initially fitted to the patient, and adjustments are made to ensure optimal comfort and alignment. This often involves trimming, padding, or modifying the shape of the device.
- Gait analysis: Observing the patient’s gait with and without the orthotic to assess its impact on their movement patterns. This helps identify areas for further refinement.
- Patient feedback: Regularly soliciting feedback from the patient regarding comfort, function, and any issues they experience with the orthotic. This is crucial for identifying and addressing any problems.
- Follow-up appointments: Scheduling follow-up appointments to monitor the patient’s progress and make necessary adjustments to the orthotic. This iterative process is key to ensuring long-term success.
- Shoe modifications: If necessary, we modify shoes to accommodate the orthotics, creating a seamless and comfortable system for the patient.
Think of it like a finely tuned instrument: it needs adjustments and calibrations to perform optimally.
Q 19. Describe your experience with digital scanning and CAD/CAM technology in orthotics.
Digital scanning and CAD/CAM technology have revolutionized orthotics. My experience with these technologies includes:
- Foot scanning: Utilizing various 3D scanning systems to capture precise anatomical data of the patient’s feet and ankles.
- CAD software: Employing CAD software to design and model custom orthotics, incorporating specific features based on the patient’s needs and the assessment data. This allows for precise control over the shape, dimensions, and materials of the orthotic.
- CAM milling: Using CAM software to generate toolpaths for computer-aided milling machines that fabricate the orthotic from the digital model. This ensures high accuracy and repeatability.
- 3D printing: Utilizing 3D printing techniques for prototyping or manufacturing orthotics, offering flexibility in material selection and design complexity.
These technologies enable a higher level of precision, customization, and efficiency in orthotic fabrication compared to traditional methods. It also allows for more efficient and reproducible creation of consistent orthotics.
Q 20. How do you collaborate with other healthcare professionals (e.g., podiatrists, physicians) in the management of patient care?
Collaboration is vital for optimal patient care. I regularly interact with:
- Podiatrists: Collaborating on diagnosis, treatment planning, and monitoring for patients with foot and ankle conditions. This ensures a comprehensive approach to the patient’s overall health.
- Physicians (e.g., orthopedists, physiatrists): Consulting on patients with systemic conditions or complex musculoskeletal issues, integrating orthotic treatment into a holistic management plan.
- Physical therapists: Working together to develop integrated treatment plans that combine orthotic intervention with physical therapy exercises for improved functional outcomes. We coordinate to ensure the patient is progressing optimally.
Effective communication through shared EMR systems and regular meetings is paramount to ensuring smooth patient transitions and coordinated care.
Q 21. Describe a challenging case involving orthotic and footwear modification, and how you resolved it.
I once had a patient with Charcot-Marie-Tooth disease (CMT), a progressive neuromuscular disorder. The patient presented with significant foot deformities, including high arches, claw toes, and limited ankle mobility. Traditional casting was impractical due to the severity of the deformities and the patient’s pain.
The challenge was designing and fabricating an orthotic that would provide adequate support, accommodate the deformities, and be comfortable enough for daily use. I also needed to accommodate significant foot asymmetry.
My solution involved utilizing 3D scanning to obtain a highly accurate model of the patient’s feet. I then used CAD software to design a custom orthotic with multiple accommodative features, including deep heel cups, metatarsal pads, and toe separators to address the specific deformities. The design incorporated flexible materials to accommodate joint limitations. Finally, I used a CAD/CAM system to mill the orthotic from a lightweight yet supportive material.
The result was an orthotic that provided improved support, reduced pain, and enhanced mobility for the patient. Regular follow-up appointments allowed me to make minor adjustments as needed to optimize its fit and function over time. This case highlighted the value of advanced technologies in managing complex conditions.
Q 22. How do you stay current with the latest advancements and research in the field of orthotics and footwear modification?
Staying current in orthotics and footwear modification requires a multi-pronged approach. It’s not enough to rely solely on initial training; continuous learning is essential.
- Professional Organizations: Active membership in organizations like the American Academy of Orthopaedic Surgeons (AAOS), the American Orthotic & Prosthetic Association (AOPA), and similar international bodies provides access to journals, conferences, and continuing education courses. These events often feature cutting-edge research and practical workshops.
- Peer-Reviewed Journals: Regularly reading peer-reviewed journals like the Journal of Orthotics, Prosthetics & Rehabilitation Technology and other relevant publications keeps me updated on the latest research findings, new materials, and treatment techniques. I critically evaluate the methodology and conclusions to ensure the information is reliable and applicable to my practice.
- Conferences and Workshops: Attending national and international conferences allows for direct interaction with leading experts, the opportunity to network, and exposure to the newest technologies and approaches. Hands-on workshops are especially valuable for honing practical skills.
- Online Resources and Continuing Education: I utilize reputable online resources and participate in online continuing education courses to stay informed about regulatory changes and best practices. This ensures compliance and access to the most effective treatment modalities.
For example, recently I attended a workshop on the use of 3D printing in custom orthotic fabrication. This technology is revolutionizing the field, allowing for more precise and patient-specific devices. By actively participating in these activities, I ensure my practice remains at the forefront of this dynamic field.
Q 23. What are the legal and regulatory considerations in your practice?
Legal and regulatory considerations are paramount in my practice. Compliance is crucial to protect both the patient and myself.
- Licensing and Certification: Maintaining the appropriate licensing and certification in my state is essential. This ensures I meet the minimum qualifications and adhere to the established professional standards.
- HIPAA Compliance: Protecting patient privacy is paramount. I strictly adhere to HIPAA regulations regarding the storage, access, and disclosure of patient information, employing secure electronic health records and physical file storage.
- Medical Device Regulations: I am familiar with and compliant with FDA regulations concerning the materials and devices I use in orthotic fabrication and modification. This includes proper labeling, sterilization procedures, and documentation.
- Malpractice Insurance: Carrying adequate malpractice insurance is crucial to safeguard against potential liability related to errors or negligence in my practice. Regularly reviewing and updating this insurance coverage is necessary.
- Informed Consent: Before initiating any treatment, I ensure patients provide informed consent. This involves thoroughly explaining the procedure, potential risks and benefits, and alternative treatment options. I document this consent process meticulously.
For instance, incorrect documentation could lead to significant legal challenges. Maintaining accurate and complete records of patient interactions, treatments, and outcomes is non-negotiable. This includes consent forms, treatment plans, progress notes, and billing records.
Q 24. How do you maintain and sterilize orthotic devices?
Maintaining and sterilizing orthotic devices is crucial for hygiene and preventing infection. The method depends on the material the orthotic is made from.
- Cleaning: Before sterilization, orthotics should be thoroughly cleaned. This typically involves wiping them down with a disinfectant solution, such as a diluted bleach solution (following manufacturer instructions carefully). For washable orthotics, hand washing with soap and water is recommended. Always allow the orthotic to completely air dry.
- Sterilization: Sterilization methods vary depending on the material and the level of contamination. For many materials, autoclaving (steam sterilization) is appropriate. However, some materials may require alternative methods like gas sterilization (ethylene oxide) or chemical disinfection. It’s crucial to always consult the manufacturer’s instructions for cleaning and sterilization.
- Storage: After sterilization, orthotics should be stored in a clean, dry environment to prevent recontamination. Use appropriate storage containers to protect them from dust and debris.
For example, a thermoplastic orthotic can generally be autoclaved, while a leather orthotic would require a different, less aggressive disinfection method. Incorrect sterilization can lead to patient infections, so adhering to manufacturer guidelines and best practices is critical.
Q 25. What are the key aspects of a proper patient intake process in orthotics?
A proper patient intake process is the foundation of effective orthotic care. It ensures accurate diagnosis and appropriate treatment planning.
- Detailed Medical History: A thorough medical history is crucial. This includes the patient’s chief complaint, past medical conditions (relevant to musculoskeletal health), medications, allergies, and any previous treatments received for similar issues.
- Physical Examination: A comprehensive physical examination focuses on the affected area. This includes assessing posture, gait, range of motion, muscle strength, and any visible deformities or abnormalities. Observations of how the patient moves and their functional limitations are crucial.
- Foot and Ankle Assessment: This involves a specific evaluation of the foot and ankle, including assessment of arch height, alignment, and any signs of pathology. Measurements are taken to determine appropriate orthotic dimensions.
- Gait Analysis: Observing the patient’s gait (walking pattern) provides insights into their movement patterns and identifies any abnormalities or compensatory mechanisms. This can be performed visually or with advanced gait analysis technologies.
- Imaging Review (if applicable): If indicated, reviewing relevant medical imaging (X-rays, MRIs) further clarifies the diagnosis and helps in treatment planning.
- Patient Goals and Expectations: Understanding the patient’s goals and expectations is critical. This establishes realistic treatment outcomes and ensures patient satisfaction.
For instance, a patient with plantar fasciitis will require a different assessment and treatment plan than a patient with a diabetic foot ulcer. A thorough intake ensures the appropriate orthotic prescription is developed.
Q 26. Describe the process of making adjustments to pre-fabricated orthotics.
Adjusting pre-fabricated orthotics requires precision and an understanding of biomechanics. The goal is to customize the device to fit the individual patient’s needs.
- Assessment: First, assess the fit of the pre-fabricated orthotic on the patient’s foot. Identify areas of pressure, discomfort, and any gaps.
- Material Considerations: Understand the material the orthotic is made from. Some materials are more readily modifiable than others (e.g., ethylene vinyl acetate (EVA) is easier to modify than a rigid carbon fiber composite).
- Tools: Appropriate tools are necessary for modification. These may include rotary tools (grinders, drills), files, heat guns (for thermoplastic materials), and various cutting instruments. Safety precautions are paramount when using these tools.
- Modification Techniques: Techniques include grinding down high-pressure areas, adding material to fill gaps, and adjusting the shape of the shell to improve alignment and support. This often involves using heat to reshape thermoplastic materials or carefully removing material to alleviate pressure points.
- Re-evaluation: After each modification step, re-evaluate the fit and comfort on the patient’s foot. This iterative process ensures the final orthotic is well-fitting and addresses the patient’s specific needs.
For example, if an off-the-shelf orthotic is pressing on the patient’s metatarsal heads, I would carefully grind down the material in those areas until the pressure is relieved, ensuring the modification doesn’t compromise the structural integrity of the device.
Q 27. How do you communicate effectively with patients regarding their treatment plan?
Effective communication is vital for successful patient care. It involves both verbal and non-verbal communication.
- Clear and Simple Language: Avoid using technical jargon; explain things in terms the patient can easily understand. Use visual aids (diagrams, models) to illustrate complex concepts.
- Active Listening: Actively listen to the patient’s concerns and questions. Show empathy and validate their experiences.
- Patient Education: Educate the patient about their condition, the purpose of the orthotic, how to properly care for it, and what to expect during the treatment process.
- Written Instructions: Provide written instructions that reinforce the verbal explanation. Include details on wearing schedules, maintenance, and follow-up appointments.
- Follow-up and Feedback: Schedule regular follow-up appointments to monitor progress, address concerns, and make any necessary adjustments to the orthotic. Solicit feedback from the patient to gauge their satisfaction and identify areas for improvement.
For example, when explaining the use of a custom foot orthotic to a patient, I would demonstrate how it supports the arch and reduces pressure on the heel and metatarsal heads. I would then provide them with written instructions on wearing the orthotics and the importance of cleaning and storing them properly.
Q 28. What are your strengths and weaknesses as an orthotist/pedorthist?
Self-assessment is crucial for professional growth. Here’s an honest appraisal of my strengths and weaknesses.
- Strengths: I possess strong biomechanical analysis skills and a keen eye for detail, allowing me to create highly effective custom orthotics. My patient communication skills are a strength, enabling me to build trust and rapport, leading to better adherence to treatment plans. I am adept at problem-solving and finding creative solutions to complex biomechanical challenges. I stay current with advances in the field through continuous learning and actively participate in professional organizations.
- Weaknesses: While I am proficient in various orthotic fabrication techniques, I could improve my proficiency in specific niche areas, such as pediatric orthotics or advanced gait analysis technology. Time management can sometimes be challenging, especially with a busy patient load. Therefore, I actively work on improving my organizational skills and efficiency to better manage my time.
Recognizing my weaknesses is a vital part of my professional development. I actively seek opportunities to enhance these areas through continuing education, mentorship, and improved practice management techniques. This commitment to self-improvement ensures that I consistently provide the highest quality care to my patients.
Key Topics to Learn for Orthotics and Footwear Modification Interview
- Biomechanics of the Foot and Ankle: Understanding gait analysis, pressure distribution, and common foot deformities (e.g., pes planus, cavus foot).
- Orthotic Design Principles: Practical application of biomechanical principles to design and fabricate custom orthotics, including material selection and fabrication techniques.
- Footwear Modification Techniques: Methods for modifying footwear to accommodate orthotic devices and address specific patient needs (e.g., stretching, adding padding, modifying shoe structures).
- Patient Assessment and Communication: Conducting thorough patient evaluations, interpreting medical documentation, and effectively communicating treatment plans.
- Casting and Molding Techniques: Proper procedures for creating accurate plaster or foam casts for orthotic fabrication.
- Material Properties and Selection: Understanding the characteristics of various orthotic materials (e.g., plastics, foams, carbon fiber) and selecting appropriate materials for specific patient needs.
- Common Orthotic Designs and Indications: Familiarity with different orthotic designs (e.g., accommodative, functional, corrective) and their appropriate applications.
- Problem-Solving and Troubleshooting: Identifying and addressing challenges during orthotic fabrication and fitting, such as pressure points or inadequate support.
- Legal and Ethical Considerations: Understanding relevant regulations and ethical practices in the field of orthotics and footwear modification.
- Technological Advancements: Familiarity with CAD/CAM technology and other digital tools used in orthotic design and fabrication.
Next Steps
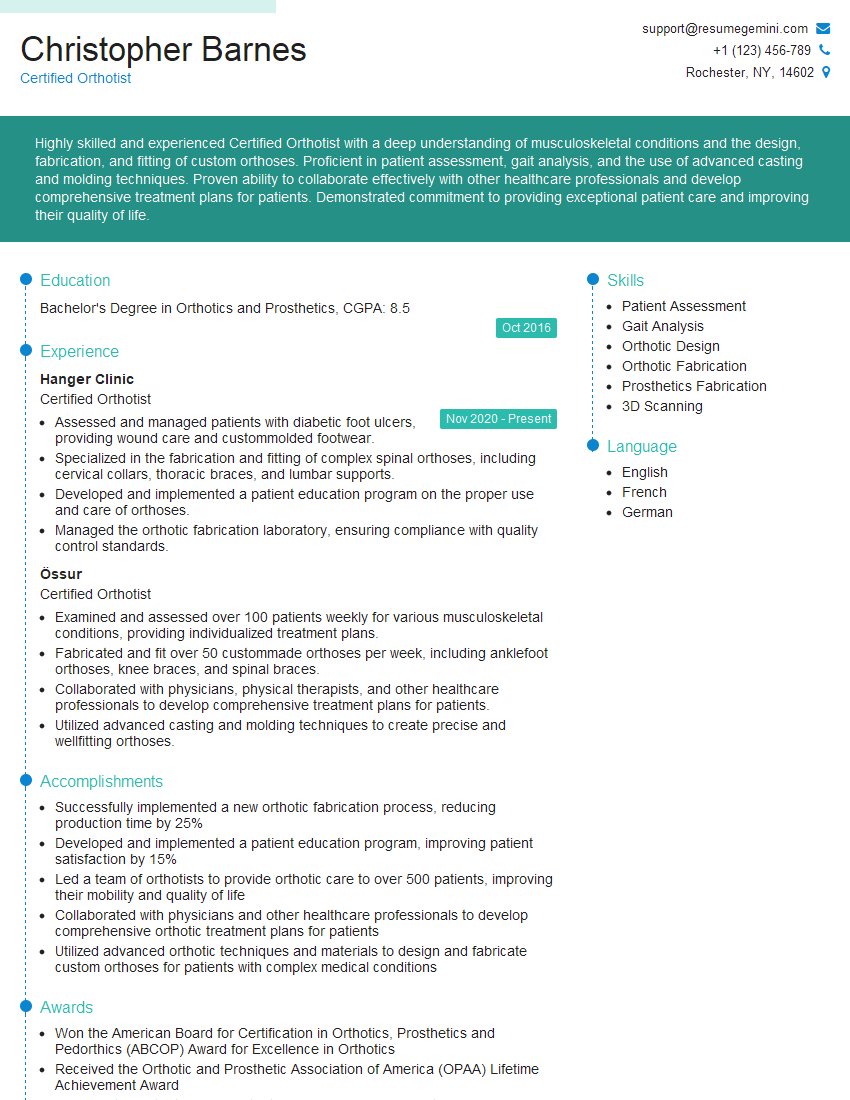
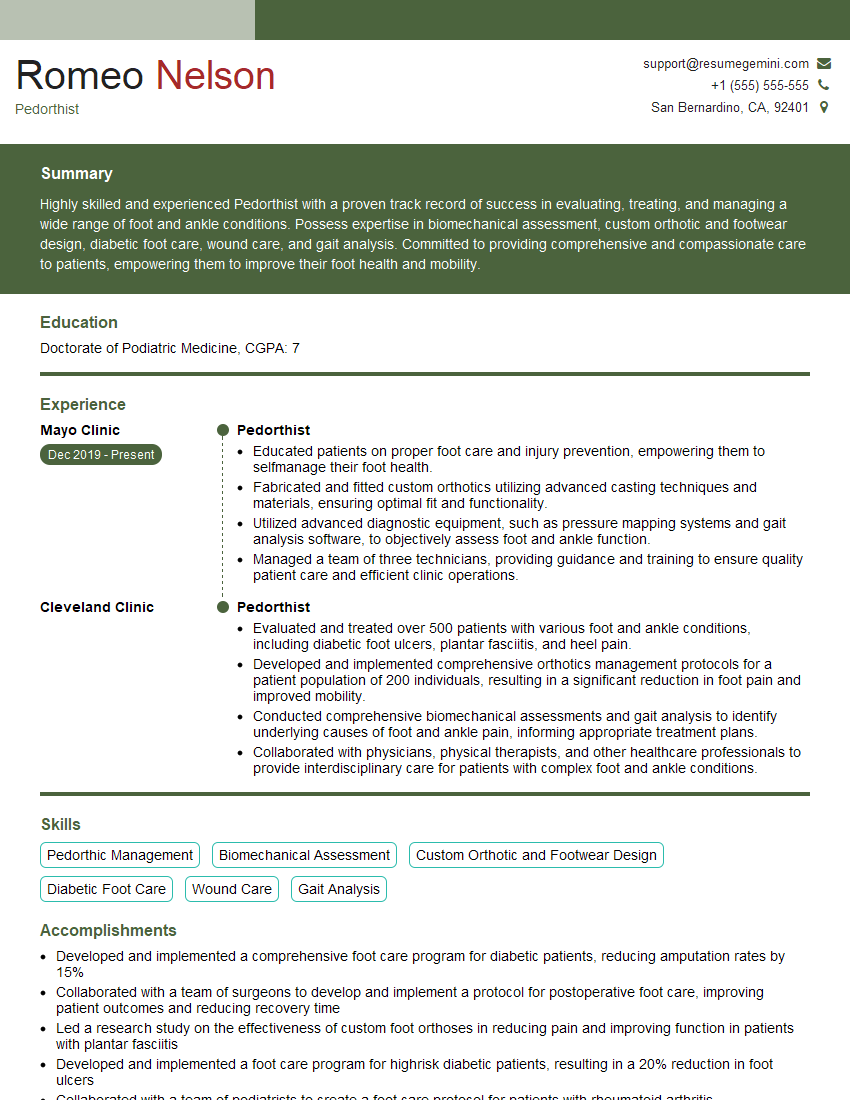
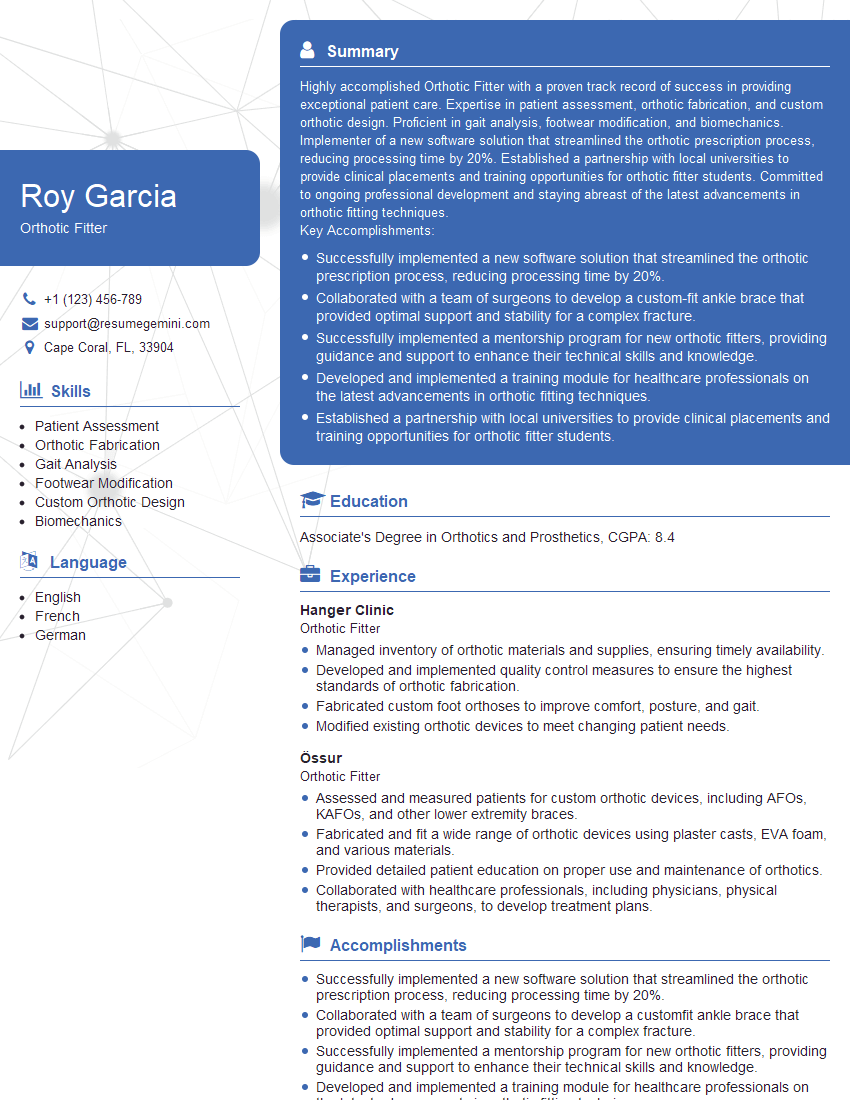
Mastering Orthotics and Footwear Modification opens doors to a rewarding career with opportunities for specialization and advancement. A strong resume is crucial for showcasing your skills and experience to potential employers. Creating an ATS-friendly resume significantly increases your chances of getting noticed by recruiters. To enhance your resume-building experience and maximize your job prospects, we recommend using ResumeGemini. ResumeGemini provides valuable tools and resources, including examples of resumes tailored to Orthotics and Footwear Modification, to help you present yourself effectively.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.