The thought of an interview can be nerve-wracking, but the right preparation can make all the difference. Explore this comprehensive guide to Tendonitis Management interview questions and gain the confidence you need to showcase your abilities and secure the role.
Questions Asked in Tendonitis Management Interview
Q 1. Describe the pathophysiology of tendonitis.
Tendonitis, or tendinopathy, encompasses a spectrum of tendon conditions characterized by pain and dysfunction. The pathophysiology isn’t fully understood but involves a complex interplay of factors. It typically begins with repetitive micro-tears in the tendon fibers, exceeding the body’s repair capacity. This leads to an inflammatory response, initially involving increased vascularity and cellular activity. However, in chronic cases, the inflammatory component may be less prominent, giving way to degenerative changes like collagen disorganization and decreased tendon strength. Essentially, the tendon becomes less resilient and more susceptible to further injury.
Imagine a frayed rope; each micro-tear is like a single strand breaking. Initially, the rope can still hold, but with enough damage, it weakens and is prone to snapping. The inflammatory response is like the body’s attempt to repair the rope, but if the damage is too much or too frequent, the repair process fails to keep up.
Q 2. Explain the difference between tendinitis, tendinosis, and tenosynovitis.
While these terms are often used interchangeably, there are subtle distinctions. Tendinitis traditionally implies an acute inflammatory process with significant swelling and pain. Tendinosis, on the other hand, represents a more chronic degenerative condition with less inflammation and more collagen disorganization and breakdown. The tendon is essentially damaged and weakened without a prominent inflammatory component. Finally, tenosynovitis involves inflammation of the tendon sheath (synovium) that surrounds and lubricates the tendon. This can occur alone or in conjunction with tendinitis or tendinosis, causing pain and potentially restricted movement.
Think of it this way: tendinitis is like a sprained ankle – acute inflammation and swelling. Tendinosis is like the long-term wear and tear on a joint, where cartilage gradually degrades. Tenosynovitis is like the inflammation of the joint’s lining, causing stiffness and pain.
Q 3. What are the common risk factors for developing tendonitis?
Numerous risk factors contribute to tendonitis development. These include:
- Overuse: Repetitive movements or excessive force placed on a tendon (e.g., repetitive typing, throwing a baseball).
- Improper Technique: Incorrect form during activities stresses tendons unevenly.
- Muscle Imbalances: Weakness or tightness in surrounding muscles can overload the tendon.
- Age: Older individuals often have decreased tendon elasticity and healing capacity.
- Underlying Medical Conditions: Conditions like diabetes, rheumatoid arthritis, and hyperthyroidism can impair tendon healing.
- Poor Footwear: Inadequate support can contribute to tendon stress.
- Previous Injury: A prior tendon injury can predispose to future problems.
For example, a tennis player using an improper backhand stroke might develop lateral epicondylitis (tennis elbow). Similarly, a construction worker repeatedly using a jackhammer could develop de Quervain’s tenosynovitis.
Q 4. How do you differentiate tendonitis from other musculoskeletal conditions?
Differentiating tendonitis from other musculoskeletal conditions requires a thorough history and physical examination. Key differences include:
- Location of pain: Tendon pain is typically localized over the affected tendon, whereas other conditions might have more diffuse pain.
- Palpation: Tenderness directly over the tendon is a hallmark of tendonitis.
- Range of motion: Tendonitis may cause restricted movement, but the pattern of limitation differs from conditions like arthritis or nerve impingement.
- Provocative tests: Specific maneuvers can reproduce tendon pain (e.g., resisted wrist extension for tennis elbow).
- Systemic symptoms: Conditions like rheumatoid arthritis or systemic lupus erythematosus may have associated fever, fatigue, and other systemic symptoms absent in tendonitis.
For instance, carpal tunnel syndrome involves nerve compression, causing numbness and tingling in the hand, distinct from the localized pain over the wrist tendons in de Quervain’s tenosynovitis.
Q 5. What are the key elements of a comprehensive history taking for a patient presenting with tendonitis?
A comprehensive history includes:
- Detailed description of pain: Location, onset, character, duration, intensity, and aggravating/relieving factors.
- Mechanism of injury: Acute trauma vs. gradual onset.
- Activity history: Occupational and recreational activities involving repetitive movements or heavy lifting.
- Past medical history: Relevant medical conditions and previous injuries.
- Medications: Any medications that might affect healing or inflammation.
- Social history: Smoking, alcohol use, and overall lifestyle factors.
For example, understanding a patient’s work as a painter helps establish the potential role of repetitive wrist movements in the development of their wrist pain.
Q 6. Describe your approach to the physical examination of a patient with suspected tendonitis.
The physical examination focuses on:
- Inspection: Assessing for swelling, redness, deformity, or skin changes over the affected area.
- Palpation: Carefully palpating the tendon for tenderness and assessing the surrounding tissues.
- Range of motion: Evaluating active and passive range of motion to identify limitations.
- Strength testing: Assessing muscle strength in movements related to the affected tendon.
- Special tests: Performing specific tests to provoke pain in the suspected tendon (e.g., Finkelstein’s test for De Quervain’s tenosynovitis).
For instance, palpating the lateral epicondyle and performing resisted wrist extension are crucial for evaluating suspected tennis elbow.
Q 7. What imaging modalities are useful in diagnosing tendonitis, and when would you use them?
Imaging studies aren’t always necessary for diagnosing tendonitis, but they can be helpful in certain situations.
- Ultrasound: This is often the first-line imaging modality. Ultrasound provides real-time images and can identify tendon thickening, tears, and surrounding inflammation.
- MRI: MRI offers higher resolution images and can better visualize subtle tendon abnormalities, including tendinosis. It’s particularly useful when ultrasound findings are inconclusive or when there’s suspicion of other pathologies.
I generally use imaging when the diagnosis is uncertain based on history and physical exam, when there is suspicion of a significant tendon tear, or when the response to conservative management is poor. For example, if a patient presents with persistent lateral epicondylitis despite conservative treatment, an ultrasound might be ordered to rule out a complete tendon rupture.
Q 8. What are the conservative management strategies for tendonitis?
Conservative management of tendonitis focuses on reducing pain and inflammation while promoting healing. It’s the first line of defense and often yields excellent results. Key strategies include:
- Rest and Modification of Activity: Avoiding the activities that aggravate the tendon is crucial. This might involve modifying your work tasks, changing sports techniques, or temporarily ceasing the activity altogether. Think of it like giving your tendon a chance to recover.
- Ice and Compression: Applying ice packs for 15-20 minutes at a time, several times a day, helps reduce swelling and pain. Compression with a bandage can further minimize inflammation.
- Elevation: Elevating the affected limb above the heart helps reduce swelling by promoting fluid drainage. For example, if you have wrist tendonitis, keep your hand elevated while resting.
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Over-the-counter pain relievers like ibuprofen or naproxen can help manage pain and inflammation. Always follow the recommended dosage.
- Physical Therapy: A physical therapist can guide you through specific exercises, stretches, and modalities to improve range of motion, strength, and flexibility. This is a vital component for long-term recovery.
- Bracing and Splinting: In some cases, a brace or splint might be used to immobilize the tendon and promote healing, particularly in the acute phase.
The combination of these strategies, tailored to the individual’s condition and needs, forms the cornerstone of effective conservative management.
Q 9. Explain the principles of eccentric loading exercise in tendonitis rehabilitation.
Eccentric loading exercises are a cornerstone of tendonitis rehabilitation. They involve lengthening the muscle while it’s contracting, placing a controlled stress on the tendon. This type of loading stimulates tendon healing and improves its strength and resilience. Think of it as controlled ‘micro-tears’ that promote repair and adaptation.
The principles are:
- Controlled Movement: Exercises are performed slowly and deliberately, focusing on the eccentric (lengthening) phase of the movement. This allows for precise control and prevents over-stress.
- Gradual Progression: The intensity and volume of the exercises are gradually increased over time to avoid re-injury. This prevents overloading the healing tendon.
- Pain Management: Exercises should be stopped if they cause significant pain. A slight discomfort is acceptable, but sharp or intense pain signals that you’re pushing too hard.
- Specificity: Exercises should target the specific tendon affected and the muscle group responsible for its movement. A physical therapist can help develop a personalized program.
Example: For patellar tendonitis (jumper’s knee), an eccentric exercise would involve slowly lowering yourself from a jump or chair, placing controlled tension on the patellar tendon. This is contrasted with a concentric contraction, where you’d push yourself back up.
Q 10. What are the indications and contraindications for corticosteroid injections in tendonitis?
Corticosteroid injections provide rapid pain relief in tendonitis by reducing inflammation. However, their use is controversial due to potential long-term risks.
Indications: Corticosteroid injections are sometimes considered for:
- Severe pain that significantly impacts function and doesn’t respond to conservative measures.
- Acute, incapacitating flares of tendonitis.
Contraindications: These injections are generally avoided in:
- Patients with diabetes, as they may increase the risk of tendon rupture.
- Patients with infections near the injection site.
- Patients with significant tendon degeneration or thinning (as evidenced by imaging), as this increases the risk of rupture.
- Cases of chronic tendonitis, where the primary issue is often tendon degeneration rather than simple inflammation. In this case, they can hasten tendon rupture and provide only temporary relief.
It’s crucial to carefully weigh the benefits and risks with your doctor before considering corticosteroid injections. They are not a long-term solution and are typically reserved for specific situations.
Q 11. Discuss the role of platelet-rich plasma (PRP) therapy in tendonitis management.
Platelet-rich plasma (PRP) therapy is a relatively new treatment for tendonitis. It involves injecting a concentration of the patient’s own platelets into the affected tendon. Platelets are rich in growth factors that promote tissue healing and regeneration.
The role of PRP is to potentially:
- Stimulate Tendon Healing: The growth factors in PRP aim to accelerate the natural healing process of the tendon.
- Reduce Inflammation: PRP may also have anti-inflammatory effects, contributing to pain relief.
- Improve Tendon Quality: In some cases, PRP may help improve the structural integrity and strength of the tendon.
However, the evidence supporting PRP’s effectiveness is still emerging. Its use is considered an option in cases where conservative management has failed and surgery is not yet warranted, but it’s not a guaranteed solution for every case. Further research is needed to establish its long-term efficacy and ideal application.
Q 12. When is surgical intervention considered for tendonitis?
Surgical intervention for tendonitis is typically considered only after conservative management and other treatments like PRP have failed to provide adequate relief. This is usually the case when the patient experiences significant functional limitations and persistent pain despite extensive conservative efforts.
Specific scenarios that might lead to surgical consideration include:
- Tendon Rupture: A complete tear of the tendon requires surgical repair.
- Severe Tendon Degeneration: In cases where the tendon shows significant structural damage and there’s minimal potential for improvement with conservative therapies.
- Failed Conservative Management: After a prolonged period (often 6-12 months) of unsuccessful conservative treatment, surgery can be an option.
- Presence of other complicating factors: Conditions like significant bone spurs or other structural abnormalities that exacerbate the tendonitis and negatively impact conservative treatment efficacy.
The decision to proceed with surgery is made collaboratively between the surgeon and the patient, carefully weighing the potential benefits against risks and complications.
Q 13. Describe different surgical techniques used to treat tendonitis.
Surgical techniques for tendonitis vary depending on the specific tendon involved and the nature of the problem. Some common procedures include:
- Tendon Repair: For complete tendon ruptures, the torn ends are surgically reattached. This often involves sutures and possibly anchors to reinforce the repair.
- Debridement: Removing damaged or degenerated tissue from the tendon. This aims to improve the environment for healing and reduce inflammation.
- Tendon Graft: In cases of severe tendon damage where repair is not possible, a tendon graft from another part of the body may be used to replace the damaged section.
- Tenosynovectomy: Removing the inflamed tissue surrounding the tendon (the tenosynovium). This is often done in cases of tenosynovitis, which is inflammation of the tendon sheath.
- Open vs. Arthroscopic Surgery: Some tendon surgeries can be performed arthroscopically (minimally invasive, with smaller incisions), while others require open surgery (larger incisions). The approach depends on the specific situation and surgeon preference.
The choice of surgical technique is highly individualized and depends on the severity of the tendonitis, the specific tendon affected, and the surgeon’s expertise.
Q 14. What are the common complications associated with tendonitis and its treatment?
Complications associated with tendonitis and its treatment are possible, though not always common. These can include:
- Persistent Pain: Despite treatment, some individuals may experience ongoing pain. This can be due to incomplete healing, underlying conditions, or other factors.
- Tendon Rupture: This is a risk with certain treatments, particularly corticosteroid injections, especially in cases of pre-existing tendon degeneration.
- Infection: Infection at the injection site (corticosteroids or PRP) or surgical incision is a potential complication requiring treatment with antibiotics.
- Stiffness and Loss of Range of Motion: Immobilization, either from injury or treatment, can lead to stiffness. Physical therapy helps to mitigate this.
- Nerve Damage: Rare but possible, especially during surgical procedures.
- Delayed Healing: Sometimes, the healing process may be slower than anticipated.
- Scar Tissue Formation: Scar tissue can form after surgery or injury, potentially leading to reduced flexibility or strength.
It’s important to work closely with your healthcare provider to minimize these risks through proper diagnosis, appropriate treatment selection, and diligent post-treatment rehabilitation.
Q 15. How do you assess the effectiveness of treatment for tendonitis?
Assessing the effectiveness of tendonitis treatment relies on a multifaceted approach, combining subjective patient feedback with objective clinical findings. We look for improvements in pain levels, both at rest and during activity. This is often measured using standardized pain scales like the Visual Analog Scale (VAS) or Numerical Rating Scale (NRS). Secondly, we assess functional improvements – can the patient perform activities of daily living (ADLs) or return to their previous activity levels without pain? We use functional outcome measures specific to the affected tendon, like the QuickDASH for upper extremity tendonitis or the Foot and Ankle Outcome Score (FAOS) for Achilles tendonitis. Finally, physical examination assesses range of motion, strength, and tenderness around the affected tendon. Imaging, such as ultrasound or MRI, may be utilized to monitor tendon healing, though these are typically not used for routine follow up and are more useful for diagnosis.
For example, a patient with lateral epicondylitis (tennis elbow) might initially report a VAS pain score of 8/10. After several weeks of physiotherapy and activity modification, a reduction to 2/10, along with an increase in grip strength and improved ability to perform activities like shaking hands or gripping a tennis racquet, would indicate effective treatment. Lack of progress, or worsening symptoms, prompts a reassessment of the treatment plan.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What patient education is crucial for successful tendonitis management?
Patient education is paramount for successful tendonitis management. It empowers patients to actively participate in their recovery and significantly improves outcomes. Key aspects include understanding the cause of their tendonitis (often overuse, repetitive movements, or improper technique), recognizing early warning signs of a flare-up (increased pain, swelling, stiffness), and learning appropriate self-management strategies. This includes:
- Activity modification: Identifying and avoiding aggravating activities. This might involve modifying sports technique, reducing work-related repetitive movements, or taking rest breaks during strenuous tasks.
- Pain management: Utilizing appropriate pain relief methods such as ice, compression, elevation (RICE protocol), over-the-counter pain relievers (NSAIDs), or in some cases, prescription medications.
- Self-mobilization exercises: Learning and performing exercises to maintain range of motion and prevent stiffness.
- Gradual return to activity: Following a structured rehabilitation program that progressively increases the intensity and duration of activity to avoid re-injury.
Analogies are useful. For example, I often compare the tendon to a rubber band that has been overstretched. Rest allows it to heal, while gradual loading (exercise) helps to strengthen it gradually.
Q 17. How do you manage a patient who is not responding to conservative treatment for tendonitis?
If a patient doesn’t respond to conservative treatment (rest, ice, medication, physiotherapy), several avenues are explored. First, we ensure the diagnosis is accurate and rule out other conditions mimicking tendonitis. A referral to a specialist, such as an orthopedic surgeon, may be necessary to evaluate for possible underlying issues, such as a partial tear or other structural abnormalities. Further investigations such as ultrasound or MRI scans may be undertaken. If no other pathology is found, alternative treatment options can be considered including:
- Corticosteroid injections: These provide temporary pain relief but have limitations (risk of tendon rupture with repeated injections) and shouldn’t be the first-line treatment.
- Platelet-rich plasma (PRP) therapy: A relatively new treatment that involves injecting concentrated platelets from the patient’s own blood into the affected tendon to promote healing.
- Surgical intervention: This is generally considered only as a last resort, typically if the tendon is severely damaged or other treatments have failed. Surgery could involve debridement of damaged tissue or tendon repair.
The decision on the most appropriate approach is highly individualised and depends on factors such as the patient’s age, activity levels, and the severity and location of the tendonitis.
Q 18. Describe the rehabilitation protocol you would use for rotator cuff tendonitis.
Rehabilitation for rotator cuff tendonitis focuses on pain management, regaining range of motion, strengthening the rotator cuff muscles, and improving scapular stability. The protocol is usually phased:
- Phase 1 (Acute): Emphasis on pain control (RICE, NSAIDs), gentle range of motion exercises to prevent stiffness, and avoidance of aggravating activities. This phase lasts until pain is significantly reduced.
- Phase 2 (Subacute): Progressive strengthening exercises are introduced, focusing on isometric exercises (muscle contractions without movement) initially, then progressing to isotonic exercises (movement through a range of motion) with light weights or resistance bands. Emphasis on proper technique to avoid re-injury.
- Phase 3 (Return to activity): Functional exercises simulating sport-specific movements are incorporated, gradually increasing intensity and duration. A gradual return to normal activity is crucial.
Specific exercises include pendulum swings, wall slides, external and internal rotation exercises with light weights or resistance bands, and scapular stabilization exercises. The program is tailored to the individual’s needs and progresses based on their response.
Q 19. Describe the rehabilitation protocol you would use for De Quervain’s tenosynovitis.
De Quervain’s tenosynovitis affects the tendons on the thumb side of the wrist. Rehabilitation involves reducing inflammation, improving tendon gliding, and strengthening the muscles around the wrist and thumb. The protocol typically consists of:
- Rest and splinting: Initially, a thumb spica splint is used to immobilize the thumb and wrist to reduce inflammation. This is usually worn for a few weeks.
- Ice and pain management: Applying ice and using over-the-counter NSAIDs to reduce pain and swelling.
- Tendon gliding exercises: Gentle exercises to improve the movement of the tendons within their sheaths. These may include thumb extension and flexion, and wrist flexion and extension.
- Strengthening exercises: Once pain is reduced, strengthening exercises are incorporated, focusing on the wrist and thumb extensors and flexors. These often involve gentle resistance using therapy putty or resistance bands.
It’s crucial to avoid forceful gripping or pinching until symptoms improve significantly. The splint is gradually weaned off as symptoms subside. The focus is on restoring function and preventing recurrence.
Q 20. Describe the rehabilitation protocol you would use for Achilles tendonitis.
Achilles tendonitis rehabilitation involves carefully managing inflammation, restoring flexibility, and gradually building strength and endurance. A phased approach is key:
- Phase 1 (Acute): RICE protocol, NSAIDs, avoidance of aggravating activities like high-impact sports. Heel lifts may be used to reduce stress on the tendon.
- Phase 2 (Subacute): Gentle stretching exercises to improve flexibility and range of motion in the ankle and calf muscles. Eccentric calf raises (lowering the heel slowly against gravity) are often incorporated, gradually increasing the number of repetitions and sets.
- Phase 3 (Return to activity): Plyometric exercises (jump training) are progressively added to improve power and agility. A gradual return to running or other activities is essential, monitoring for pain or discomfort.
It’s crucial to listen to the body and avoid pushing through pain. A slow and progressive approach minimizes risk of re-injury. The exact duration of each phase depends on the individual’s response.
Q 21. How would you modify a training program for an athlete with patellar tendonitis?
Modifying a training program for an athlete with patellar tendonitis requires careful consideration to avoid overloading the tendon. The focus is on reducing stress on the patellar tendon while maintaining overall fitness and performance. This involves:
- Reducing high-impact activities: Temporary avoidance of activities like running, jumping, and plyometrics. These can be replaced with low-impact alternatives like cycling or swimming.
- Modifying training volume and intensity: Gradually reducing the number of training sessions, the duration of each session, and the intensity of workouts. Focusing on proper form is crucial to minimize stress on the tendon.
- Incorporating strengthening exercises: Strengthening the quadriceps muscles, particularly the vastus medialis obliquus (VMO), helps to improve patellar tracking and reduce strain on the tendon. Exercises like isometric quadriceps sets and leg extensions (with light resistance) are beneficial.
- Flexibility and mobility exercises: Improving flexibility in the hip and ankle can reduce stress on the knee joint and patellar tendon.
- Proper footwear and orthotics: Ensuring appropriate footwear and considering the use of orthotics to improve foot and ankle support can reduce stress on the patellar tendon.
The athlete’s return to sport is gradual and guided by pain tolerance. The training program will be modified and advanced based on clinical progress. Regular monitoring of pain and functional capacity guides this process.
Q 22. What are the common causes of lateral epicondylitis (tennis elbow)?
Lateral epicondylitis, or tennis elbow, is an overuse injury affecting the tendons that attach to the outside of the elbow. It’s not just for tennis players; anyone performing repetitive wrist and forearm movements can develop it.
- Repetitive movements: Activities like painting, carpentry, using a computer mouse extensively, or even gardening can repeatedly stress the tendons.
- Improper technique: Using incorrect form during sports or other activities can put excessive strain on the elbow.
- Sudden forceful movements: A sudden, forceful contraction of the wrist extensor muscles can cause a tear in the tendons.
- Underlying medical conditions: Conditions like rheumatoid arthritis can increase the risk of developing tennis elbow.
- Overtraining: A sudden increase in the intensity or duration of activities involving the wrist and forearm can overwhelm the tendons.
Think of it like this: imagine a rope (the tendon) repeatedly rubbing against a rough surface (the bone). Over time, the friction causes inflammation and pain.
Q 23. What are the common causes of medial epicondylitis (golfer’s elbow)?
Medial epicondylitis, or golfer’s elbow, is a similar overuse injury affecting the tendons on the inside of the elbow. Again, it’s not exclusive to golfers.
- Repetitive gripping and flexing: Activities such as throwing, using hand tools, or playing certain racquet sports can cause this condition.
- Improper lifting techniques: Incorrect lifting mechanisms put significant stress on the forearm muscles and tendons.
- Repetitive forearm pronation and supination: Constantly rotating the forearm can strain the tendons responsible for these actions.
- Direct trauma: A direct blow to the inside of the elbow can also cause medial epicondylitis.
Analogy: It’s like repeatedly squeezing a sponge too hard—eventually, it becomes sore and inflamed.
Q 24. How do you differentiate between lateral and medial epicondylitis?
The key difference lies in the location of pain and the muscles involved. Lateral epicondylitis causes pain on the outside of the elbow, radiating down the forearm. This is because it affects the wrist extensor tendons (muscles that straighten the wrist and fingers). Medial epicondylitis causes pain on the inside of the elbow, also radiating down the forearm, and it affects the wrist flexor tendons (muscles that bend the wrist and fingers).
Physical examination is crucial for diagnosis, identifying tenderness to palpation directly over the affected epicondyle. Further, specific resisted tests where the doctor asks the patient to resist certain movements against pressure are extremely helpful in localizing the issue.
Q 25. What is the role of bracing and splinting in tendonitis management?
Bracing and splinting play a vital role in tendonitis management, particularly in the initial stages. They provide rest and support to the injured tendons, reducing stress and promoting healing.
- Reduced muscle strain: By limiting the range of motion of the elbow and wrist, bracing can prevent the affected muscles from contracting and stressing the injured tendons.
- Pain relief: The immobilization offered by a brace or splint reduces pain by decreasing inflammation and tension on the affected area.
- Improved healing environment: Resting the injured tendons allows the body to focus its resources on repair and regeneration.
Think of a brace or splint as a temporary cast for the elbow, giving the injured tendons the time they need to recover. The type of brace and duration of use are determined on a case-by-case basis, and generally part of a broader rehabilitation program.
Q 26. What are the long-term outcomes for patients with tendonitis?
Long-term outcomes for patients with tendonitis vary depending on several factors, including the severity of the condition, the individual’s response to treatment, and adherence to a rehabilitation program.
- Complete recovery: Many patients experience complete resolution of their symptoms with proper management, including conservative treatment and rehabilitation.
- Partial recovery: In some cases, there might be some residual symptoms, like occasional mild discomfort during strenuous activity. This is particularly true in patients who didn’t follow their exercise program correctly.
- Chronic condition: In rare instances, tendonitis can become a chronic condition, requiring ongoing management. This is more likely with delayed treatment or lack of adherence to treatment.
Early diagnosis and intervention significantly improve the long-term prognosis. It’s important to emphasize the significance of adhering to the treatment and rehabilitation plan recommended by the healthcare professional.
Q 27. Describe your experience with managing chronic tendonitis cases.
I have extensive experience managing chronic tendonitis cases, often involving a multi-faceted approach. These cases require a great deal of patience and collaboration with the patient. Often, simply addressing pain isn’t enough; we must address underlying biomechanical issues, and sometimes systemic concerns.
For instance, I had a patient with chronic lateral epicondylitis who’d tried various treatments without success. After a thorough assessment, we discovered that his workstation setup contributed to his condition. We adjusted his posture, keyboard positioning, and mouse use, alongside incorporating a focused physiotherapy program. By addressing both the immediate pain and the underlying cause, we achieved significant improvement.
A key aspect is tailoring the treatment plan to each individual’s needs. This includes not only specific exercises but also adjustments to daily activities and work habits to avoid triggering factors and promoting sustainable healing.
Q 28. How do you stay updated on the latest advancements in tendonitis management?
Staying current with advancements in tendonitis management requires a multi-pronged approach.
- Peer-reviewed journals: I regularly review publications in journals like the American Journal of Sports Medicine and the Journal of Hand Surgery to stay informed about the latest research findings on diagnosis, treatment, and rehabilitation techniques.
- Professional conferences and workshops: Attending conferences and workshops allows me to network with colleagues and learn about the newest treatment approaches directly from experts in the field.
- Continuing medical education (CME): I actively participate in CME courses and seminars to update my knowledge and skills in tendonitis management.
- Collaboration with colleagues: I maintain an active network of colleagues, including physical therapists, occupational therapists, and sports medicine specialists, with whom I regularly discuss challenging cases and share insights.
This ongoing process ensures that I can offer my patients the most effective and up-to-date care available.
Key Topics to Learn for Tendonitis Management Interview
- Anatomy and Physiology of Tendons: Understanding tendon structure, function, and the biomechanics involved in tendon injuries is crucial.
- Tendonitis Pathophysiology: Explore the inflammatory process, cellular mechanisms, and contributing factors to tendonitis development.
- Differential Diagnosis: Learn to distinguish tendonitis from other musculoskeletal conditions presenting with similar symptoms.
- Conservative Management Strategies: Master the principles of rest, ice, compression, elevation (RICE), physiotherapy, and medication in managing tendonitis.
- Therapeutic Exercises and Rehabilitation: Understand the role of targeted exercises, stretching, and strengthening programs in restoring tendon function.
- Surgical Interventions: Familiarize yourself with surgical techniques used in severe or unresponsive cases of tendonitis and their indications.
- Patient Education and Counseling: Learn effective communication strategies to educate patients about their condition and self-management techniques.
- Assessment and Evaluation Techniques: Gain proficiency in using physical examination, imaging techniques (e.g., ultrasound, MRI), and other diagnostic tools.
- Evidence-Based Practice: Understand how to critically evaluate research and apply the latest evidence to guide clinical decision-making in tendonitis management.
- Case Studies and Problem-Solving: Practice analyzing case studies to develop your problem-solving skills and decision-making process related to diagnosis and treatment planning.
Next Steps
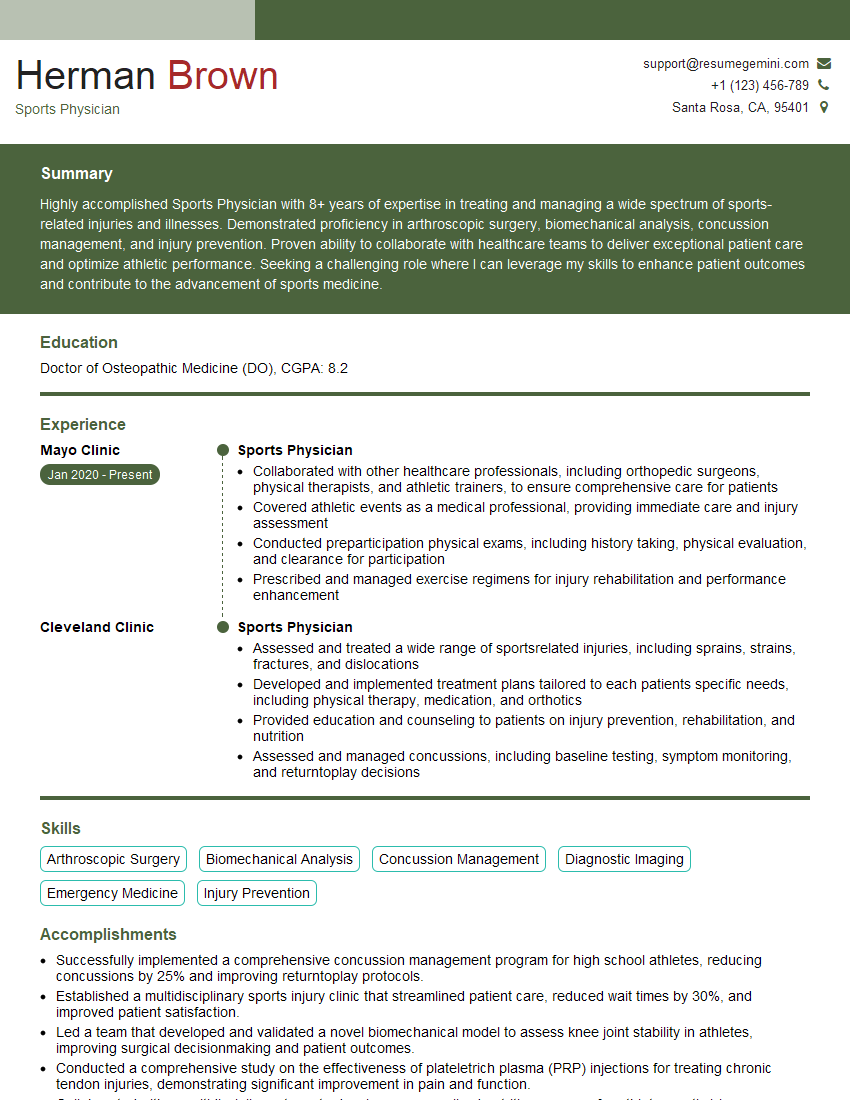
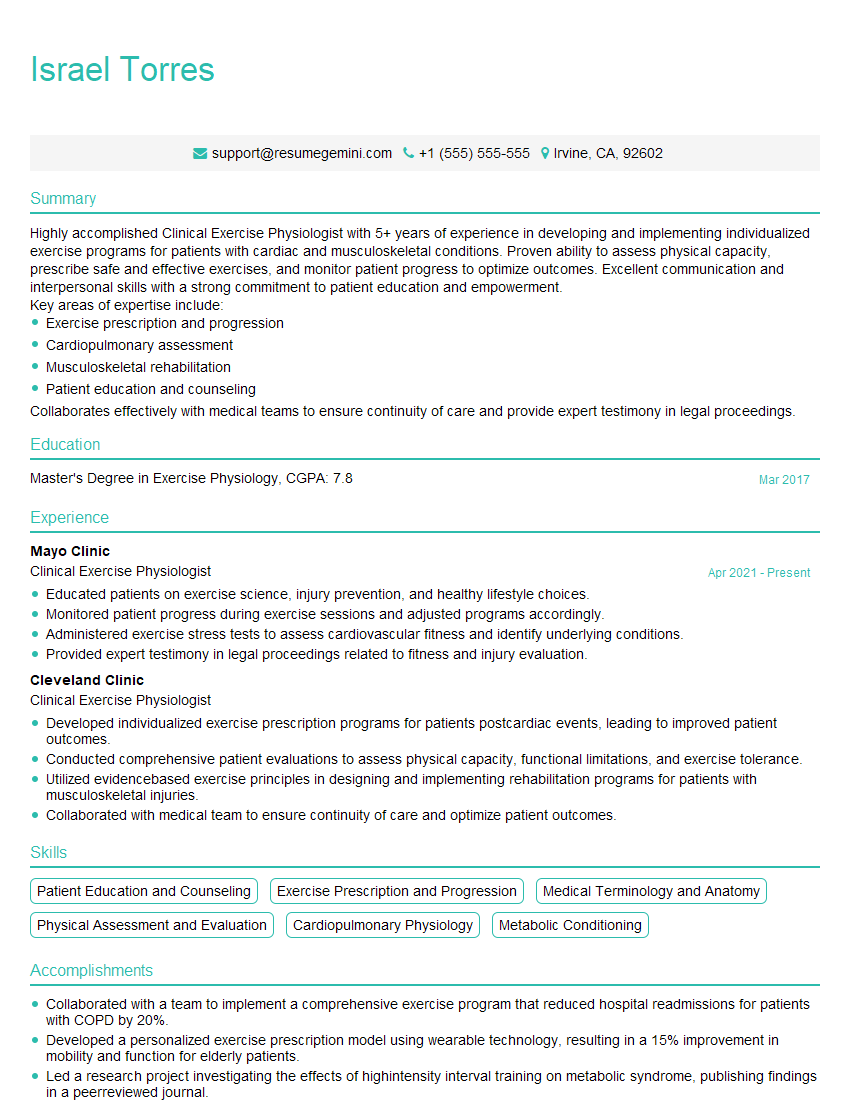
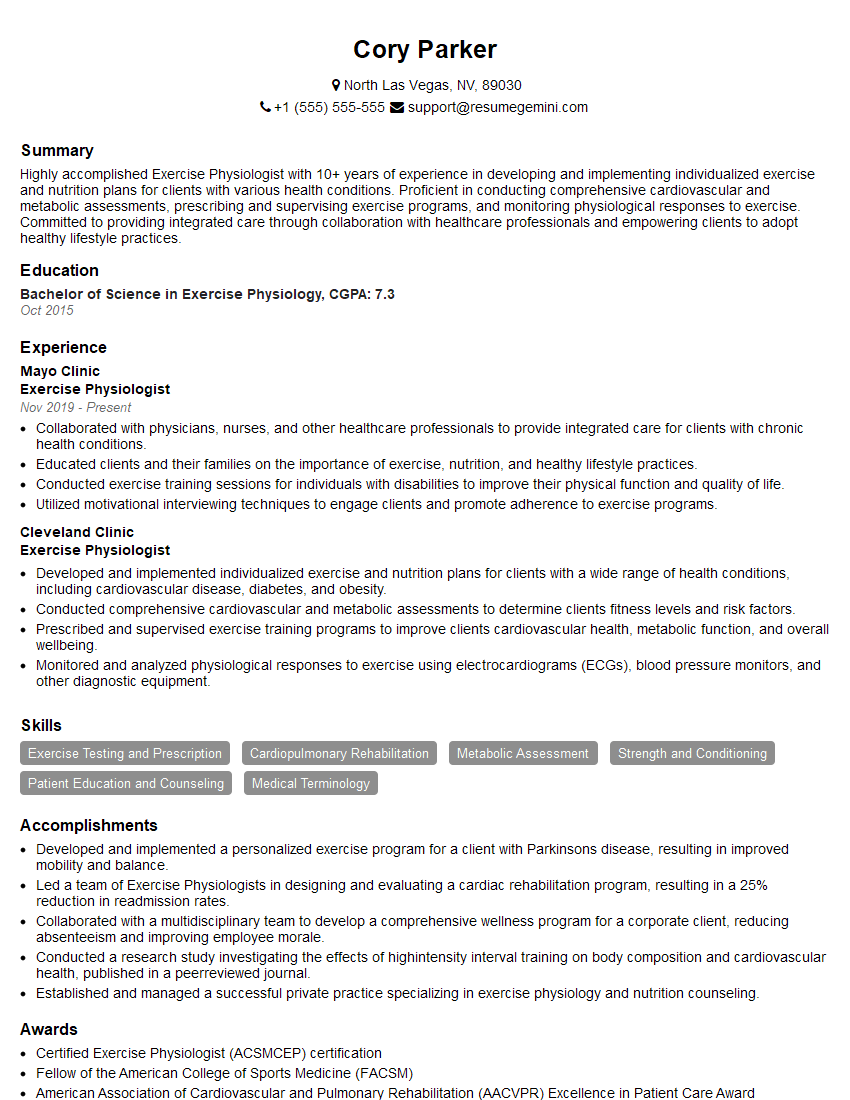
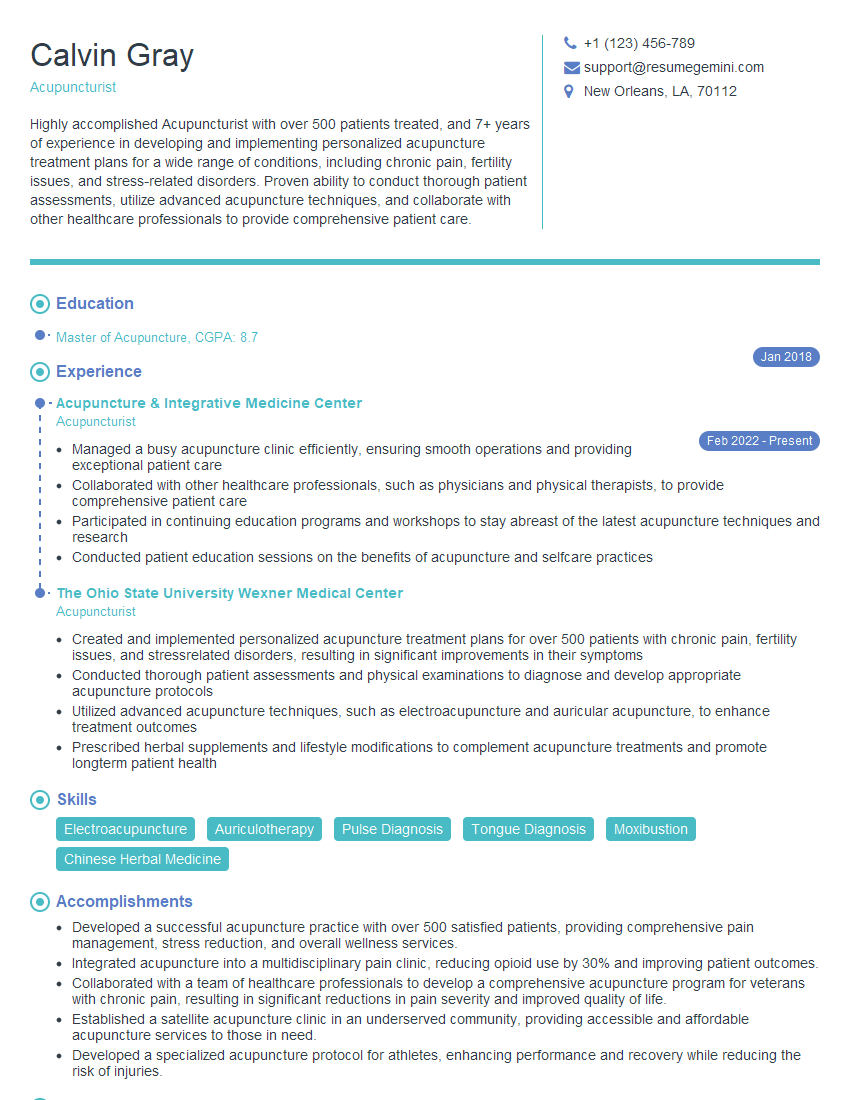
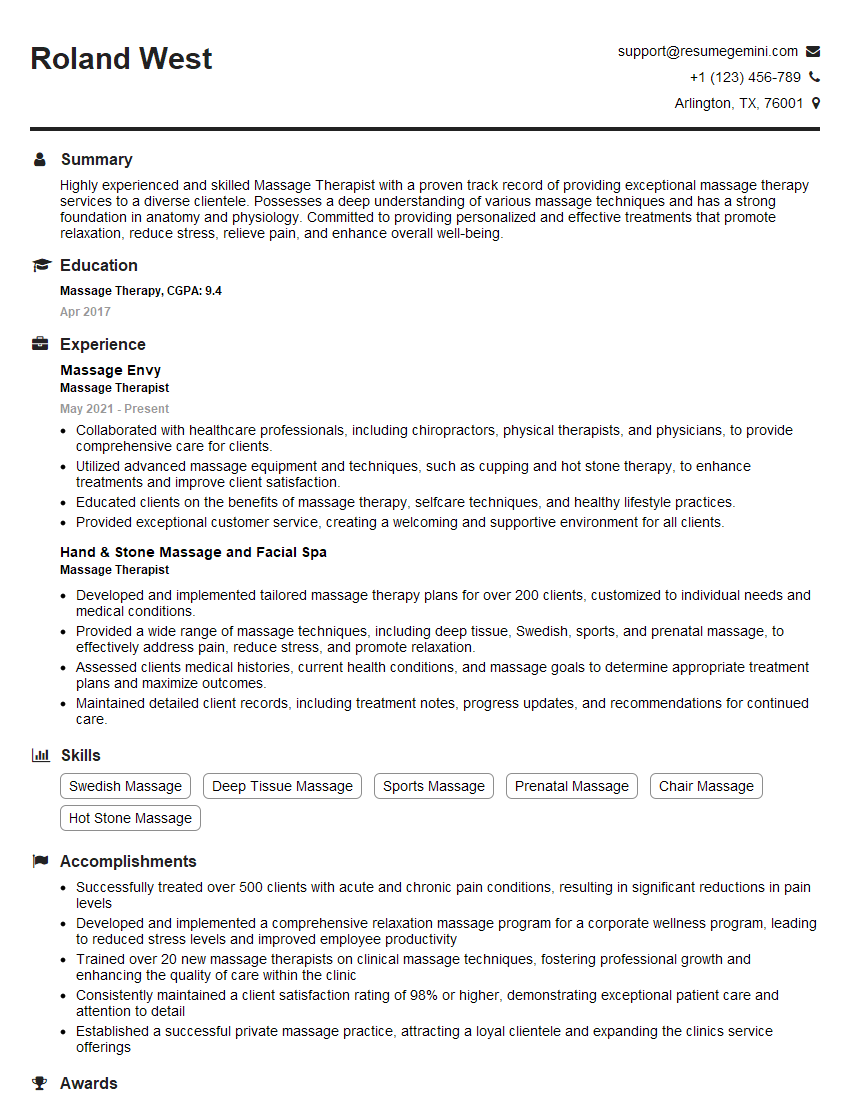
Mastering Tendonitis Management is essential for career advancement in healthcare. A strong understanding of this area demonstrates your clinical expertise and patient care capabilities, opening doors to specialized roles and leadership opportunities. To maximize your job prospects, create an ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource that can help you build a professional and impactful resume tailored to the healthcare industry. They offer examples of resumes specifically designed for professionals in Tendonitis Management to guide you in crafting a compelling application.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.