Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Hammertoe Surgery interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Hammertoe Surgery Interview
Q 1. Describe the different surgical techniques used in hammertoe correction.
Hammertoe correction surgery aims to restore the natural alignment of the affected toe. Several surgical techniques exist, chosen based on the severity of the deformity and the patient’s individual needs. These techniques generally involve either soft tissue procedures or osteotomies (bone cuts).
- Soft Tissue Procedures: These focus on releasing tight tendons and ligaments that contribute to the bending of the toe. Examples include tendon lengthening (e.g., extensor tendon lengthening), flexor tenotomy (cutting the flexor tendon), and capsulotomy (releasing the joint capsule).
- Osteotomies: For more severe hammertoes, osteotomies are often necessary to correct the bone deformity itself. Different types of osteotomies exist, including wedge osteotomies (removing a wedge of bone to shorten the toe), arthrodesis (joint fusion), and proximal phalangeal osteotomies (cutting the bone of the middle section of the toe). The choice of osteotomy depends on the location and severity of the bone deformity.
- Arthroplasty (Joint Resurfacing): In some cases, particularly in younger, more active patients with less severe deformities, arthroplasty might be considered. This involves resurfacing the joint to improve motion and reduce pain.
The surgeon will carefully select the most appropriate technique based on a thorough assessment of the patient’s foot and the specific characteristics of their hammertoe.
Q 2. What are the indications and contraindications for hammertoe surgery?
Indications for hammertoe surgery are primarily driven by the patient’s symptoms and the severity of the deformity. Surgery is usually considered when conservative treatments like orthotics and padding have failed to provide adequate relief.
- Indications: Persistent pain, significant deformity causing difficulty with shoe wear, callus formation leading to ulceration, and functional limitations (e.g., difficulty walking or performing daily activities).
Contraindications, or reasons to avoid surgery, include:
- Poorly controlled systemic diseases: Conditions like diabetes or peripheral vascular disease (PVD) can significantly increase the risk of complications such as wound healing problems and infection.
- Significant peripheral neuropathy: Lack of sensation in the toe increases the risk of complications and makes post-operative care challenging.
- Patient’s unrealistic expectations: Surgery isn’t always a perfect solution and realistic expectations should be discussed pre-operatively.
- Severe vascular disease: Poor blood flow to the affected toe might compromise healing and lead to complications.
A thorough assessment is crucial to determine if surgery is the appropriate treatment option and minimize potential risks.
Q 3. Explain the preoperative assessment and planning for a hammertoe procedure.
Preoperative assessment for hammertoe surgery is crucial for planning a successful procedure. This includes a comprehensive medical history, a physical examination of the foot and ankle, and imaging studies.
- Detailed Medical History: This includes assessing the patient’s overall health, any existing medical conditions (especially those affecting blood circulation and wound healing), current medications, allergies, and smoking status.
- Physical Examination: A thorough examination of the foot and ankle will assess the extent of the hammertoe deformity, the range of motion of the affected joint, and the presence of any other foot problems like bunions or arthritis.
- Imaging Studies: X-rays are essential to evaluate the exact bone alignment and assess the severity of the deformity. Other imaging modalities like MRI or CT scans may be considered in specific cases to rule out other pathologies.
- Preoperative Planning: Based on the assessment, a surgical plan is developed that includes the specific surgical technique, type of incision, and the use of any implants. Detailed preoperative photographs and measurements help guide the surgical procedure. Realistic expectations regarding the surgical outcome are also discussed with the patient.
This comprehensive approach ensures that the surgery is tailored to the individual patient’s needs and reduces the risk of complications.
Q 4. Discuss the different types of implants used in hammertoe surgery and their advantages/disadvantages.
Implants are sometimes used in hammertoe surgery, particularly in osteotomies, to help maintain the corrected position of the bone fragments during healing. The choice of implant depends on the surgical technique and the surgeon’s preference.
- K-wires (Kirschner wires): These are thin, smooth metal wires that are inserted into the bone to stabilize it. They are relatively inexpensive, easy to use, and effective for simple osteotomies. However, they require a second procedure for removal, usually several weeks after the initial surgery.
- Small screws: These offer excellent stability and don’t require removal, simplifying the postoperative process. However, they can be more expensive and require a higher level of surgical precision.
- Plates and screws: These are often used for more complex osteotomies where a high degree of stability is needed. While providing excellent stability, they involve more extensive surgery and can be associated with a slightly higher risk of complications like infection.
The advantages and disadvantages of each implant type need to be carefully weighed against the specific surgical situation and patient factors.
Q 5. How do you manage postoperative pain and complications in hammertoe surgery?
Postoperative pain management is crucial for patient comfort and recovery. A multi-modal approach is usually employed, combining different methods to achieve optimal pain control.
- Medication: Pain medication, including non-steroidal anti-inflammatory drugs (NSAIDs) and/or opioids, are prescribed to manage pain. The type and dosage are adjusted based on the patient’s individual needs and response.
- Ice: Applying ice packs to the affected area can help reduce swelling and pain.
- Elevation: Elevating the foot above the heart can reduce swelling.
- Physical Therapy: Once the initial healing phase is over, physical therapy is essential to restore range of motion, strengthen muscles, and improve function.
- Nerve Blocks: In some cases, nerve blocks may be used to provide more effective pain relief, especially in the immediate postoperative period.
Careful monitoring for complications such as infection, excessive swelling, or nerve injury is vital. Prompt attention to any concerning symptoms is essential for optimal outcomes.
Q 6. What are the common complications associated with hammertoe surgery, and how do you prevent them?
While hammertoe surgery is generally successful, potential complications can arise. Careful surgical technique, patient selection, and diligent postoperative care can significantly reduce these risks.
- Infection: Infection is a potential complication of any surgery. Prophylactic antibiotics are generally given before surgery and meticulous sterile techniques are followed in the operating room.
- Malunion or Nonunion: This refers to improper healing of the bone fragments after an osteotomy. Careful surgical technique, appropriate implant selection, and postoperative immobilization help minimize this risk.
- Recurrence: The hammertoe deformity may recur if the underlying cause isn’t adequately addressed. This is more likely if the surgical technique wasn’t optimized for the specific anatomy of the toe.
- Nerve Damage: Injury to nerves in the area can cause numbness, tingling, or pain. Careful surgical dissection and meticulous attention to anatomical landmarks help minimize this risk.
- Stiffness: Loss of joint mobility is a potential complication, and postoperative physical therapy is crucial to prevent or minimize this.
Prophylactic measures, such as appropriate patient selection, careful surgical technique, and diligent postoperative care, significantly reduce the likelihood of these complications. Regular follow-up appointments allow for prompt detection and management of any issues.
Q 7. Describe your experience with minimally invasive hammertoe surgery techniques.
Minimally invasive techniques for hammertoe correction, such as percutaneous procedures, have gained popularity due to their potential advantages over open surgery. These approaches typically involve smaller incisions, less tissue disruption, reduced postoperative pain, and faster recovery times.
My experience with minimally invasive techniques has shown that they are effective for select patients with less severe hammertoe deformities. While they offer potential benefits, careful patient selection is crucial. These techniques may not be suitable for all patients, especially those with severe deformities or complex anatomical issues. I carefully assess each patient to determine the most appropriate surgical approach. The advantages and disadvantages are carefully discussed with the patient to ensure shared decision making.
The success rate of minimally invasive surgery is highly dependent on the surgeon’s experience and expertise in these techniques. Proper training and ongoing refinement of these procedures is essential for achieving optimal results and minimizing complications. I continue to update my techniques based on evidence-based research and new developments in foot and ankle surgery.
Q 8. How do you determine the appropriate surgical approach for different types of hammertoes?
Choosing the right surgical approach for hammertoe depends heavily on the severity and type of deformity, the patient’s age, activity level, and overall health. We categorize hammertoes based on the joint involved (interphalangeal or metatarsophalangeal) and the degree of deformity.
- Mild hammertoes, primarily affecting the interphalangeal joint, might benefit from a simple
tendon lengtheningprocedure orarthrodesis(joint fusion), which stabilizes the joint. - More severe hammertoes, or those involving the metatarsophalangeal joint, often require a more extensive procedure such as an
osteotomy(bone resection and realignment) orarthrodesis. Sometimes, a combination of techniques is necessary. - For flexible hammertoes, where the toe can be passively straightened, conservative treatments like padding or splints are initially tried. Surgery is only considered if these methods fail to provide sufficient relief.
- Rigid hammertoes, where the toe is fixed in a bent position, invariably require surgery.
For example, a young, active patient with a mild hammertoe might be a good candidate for a tendon lengthening procedure, focusing on minimizing invasiveness and maximizing recovery. An older patient with significant arthritis in the affected joint might be better suited for arthrodesis to achieve stable joint fusion and pain relief, even if it means some loss of toe mobility.
Q 9. What are the key factors to consider when choosing between arthroplasty and osteotomy for hammertoe correction?
The decision between arthroplasty (joint replacement) and osteotomy for hammertoe correction involves careful consideration of several factors:
- Severity of the deformity: Osteotomy is generally preferred for more severe deformities where significant bone realignment is needed. Arthroplasty is better suited for milder deformities with minimal bone changes.
- Joint arthritis: The presence of significant arthritis makes arthroplasty a more appropriate option, as it replaces the damaged joint surface. Osteotomy may not be as effective in the presence of severe arthritis.
- Patient age and activity level: Younger, more active patients often tolerate osteotomy better, as it leads to a more stable joint over the long term. Older patients or those with lower activity levels might prefer the less invasive arthroplasty procedure, although recovery can be longer.
- Bone quality: Osteotomy requires sufficient bone quality to allow for bone healing. Patients with poor bone quality, such as those with osteoporosis, might be better suited for arthroplasty.
Think of it like this: osteotomy is like fixing a crooked fence post by cutting and realigning it, while arthroplasty is replacing the damaged post entirely with a new one. The best choice depends on the condition of the ‘post’ and your overall goals.
Q 10. Describe your experience with managing patients with diabetes who require hammertoe surgery.
Managing diabetic patients undergoing hammertoe surgery requires a multidisciplinary approach and meticulous attention to detail due to their increased risk of complications. These patients often have impaired circulation and neuropathy, which can significantly delay wound healing and increase the risk of infection.
- Preoperative assessment: We thoroughly evaluate the patient’s blood glucose control, vascular status (checking for peripheral arterial disease), and neurological function before surgery. We may require optimization of diabetes management prior to surgery to reduce risks.
- Surgical technique: We might opt for minimally invasive techniques to minimize trauma and reduce the risk of complications. Meticulous hemostasis (control of bleeding) is crucial to prevent hematoma formation.
- Postoperative care: Close monitoring of blood glucose levels and wound healing is paramount. We utilize appropriate antibiotic prophylaxis to prevent infection. Regular wound care and diligent follow-up are essential. Patient education on foot care is critical.
For example, a patient with poorly controlled diabetes might require a longer hospital stay for more intensive monitoring and wound care. We might also use specialized dressings to support wound healing and reduce infection risk.
Q 11. Explain your approach to postoperative care and rehabilitation after hammertoe surgery.
Postoperative care after hammertoe surgery is crucial for optimal healing and functional recovery. It’s a collaborative effort between the surgical team, physical therapists, and the patient.
- Immediate postoperative period: Pain management is vital, often using a combination of analgesics and ice. Elevation of the foot helps reduce swelling. The surgical site is carefully monitored for signs of infection.
- Early mobilization: Patients are encouraged to start gentle range-of-motion exercises as soon as tolerated to prevent stiffness. Weight-bearing is gradually increased based on the surgical procedure and the patient’s progress.
- Physical therapy: A tailored rehabilitation program, including strengthening and range-of-motion exercises, is typically initiated within a few weeks of surgery. This helps restore joint mobility and muscle strength.
- Follow-up appointments: Regular follow-up visits allow for monitoring of healing, addressing any complications, and adjusting the rehabilitation plan as needed.
The recovery process is highly individualized, but generally, patients can expect to return to normal activities within several weeks, though the full recovery may take a few months.
Q 12. How do you assess the long-term outcomes of hammertoe surgery?
Assessing long-term outcomes of hammertoe surgery involves a combination of clinical examination, patient-reported outcome measures (PROMs), and radiographic evaluation.
- Clinical examination: We assess the alignment of the corrected toe, range of motion, presence of any residual deformity, and the overall appearance of the foot.
- PROMs: Standardized questionnaires such as the American Orthopaedic Foot and Ankle Society (AOFAS) score are used to measure patient satisfaction, pain levels, and functional improvement.
- Radiographic evaluation: X-rays help assess the position of the bones and the integrity of the corrected joint. They can reveal any evidence of arthritis or other complications over time.
We typically follow patients for at least one year, and sometimes longer, to assess the durability of the surgical correction. A successful outcome is characterized by a significant reduction in pain, improved function, and patient satisfaction.
Q 13. Discuss your experience with revision hammertoe surgery.
Revision hammertoe surgery is unfortunately sometimes necessary when the initial procedure fails to achieve the desired outcome or complications arise. This requires meticulous planning and a thorough understanding of the previous surgical approach and the current anatomy.
- Causes of revision surgery: Recurrence of the deformity, persistent pain, infection, malunion (improper bone healing), or nonunion (failure of bone to heal) are common reasons for revision surgery.
- Surgical approach: The approach is tailored to the specific reason for revision. It often involves more complex procedures and a higher degree of surgical skill. The use of bone grafts or alternative fixation techniques might be required.
- Challenges: Revision surgery can be more challenging than the initial procedure because of scar tissue and the potential for altered anatomy. The success rate is often lower, and the risk of complications is higher.
It’s important to emphasize that careful patient selection, proper surgical technique, and meticulous postoperative care are crucial in minimizing the need for revision surgery.
Q 14. What are the current trends and advances in hammertoe surgery?
Hammertoe surgery is constantly evolving, with several current trends and advances aiming to improve outcomes and minimize invasiveness:
- Minimally invasive techniques: Smaller incisions and the use of specialized instruments are reducing surgical trauma and improving recovery times.
- Improved implants and fixation techniques: Advanced biocompatible materials and minimally invasive fixation techniques provide better stability and promote faster healing.
- Computer-assisted surgery: This technology is enhancing surgical precision and reproducibility, potentially leading to better long-term results.
- Focus on personalized medicine: Tailoring surgical approaches and postoperative care based on individual patient factors like age, activity level, and comorbidities is becoming increasingly common.
- Research into regenerative medicine: Exploring techniques like stem cell therapy or growth factor application to improve bone healing and reduce the risk of complications is an active area of research.
These advancements are leading to better patient outcomes, shorter recovery times, and improved long-term satisfaction.
Q 15. Explain your understanding of the biomechanics of the foot and its relevance to hammertoe surgery.
Understanding the biomechanics of the foot is crucial for successful hammertoe surgery. The foot is a complex structure with multiple bones, joints, ligaments, and muscles working together to provide support, balance, and locomotion. Hammertoes, characterized by a flexion deformity of the proximal interphalangeal (PIP) joint of the toe, disrupt this intricate balance.
Specifically, muscle imbalances, particularly in the flexor and extensor tendons, are key factors in the development of hammertoes. Tight flexor tendons pull the toe down while weakened extensor tendons fail to counterbalance this effect. Additionally, changes in the metatarsophalangeal (MTP) joint, the joint connecting the toe to the foot, such as metatarsus primus varus (a bunion deformity) or plantar plate injury, can contribute significantly to the biomechanics leading to hammertoe formation. During surgery, we consider these factors carefully. For instance, if a significant MTP joint abnormality is present, we may address it alongside the hammertoe correction to avoid recurrence. A thorough understanding of the foot’s mechanics informs our surgical approach, ensuring we target the root cause of the deformity, rather than just the symptom.
For example, a patient may present with a hammertoe and a significant bunion. Simply correcting the hammertoe without addressing the underlying bunion would likely lead to recurrence of the hammertoe over time. A comprehensive biomechanical analysis is, therefore, an essential part of my surgical planning.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you counsel patients about the risks and benefits of hammertoe surgery?
Counseling patients about hammertoe surgery involves a balanced presentation of risks and benefits. I begin by explaining the condition itself, using clear and simple language, avoiding medical jargon. I often use models or diagrams to visually explain the deformity and the proposed surgical correction.
Regarding benefits, I emphasize the potential for improved comfort, improved cosmetic appearance, reduced pain and pressure, and restoration of normal foot function, allowing them to wear more comfortable shoes. I carefully detail the specific surgical technique planned and its advantages, and discuss realistic expectations about the outcomes.
I also transparently discuss potential risks. These include infection, nerve damage, poor wound healing, stiffness, recurrence of the deformity, and persistent pain. I explain that the success rate is excellent in most cases, but there is always a small chance of complications. I emphasize the importance of post-operative compliance with instructions for optimal healing and minimizing potential complications. I answer all their questions patiently and honestly, ensuring they feel comfortable and informed before proceeding.
I encourage patients to share their concerns and expectations, fostering open communication to make an informed decision together. For example, I will discuss realistic expectations about postoperative swelling, pain management, and the timeline for return to normal activity. The goal is shared decision-making, where the patient understands the implications of the surgery and feels confident in the chosen course of action.
Q 17. What is your approach to managing patient expectations after hammertoe surgery?
Managing patient expectations after hammertoe surgery is critical to a positive outcome. I set realistic expectations from the initial consultation, emphasizing that recovery is a gradual process, not an immediate transformation. I explain that swelling and pain are normal post-operative occurrences and provide detailed instructions on managing these symptoms.
I use visual aids such as photographs of previous patients’ results at various stages of healing to demonstrate the typical recovery timeline. I explain that full recovery can take several months, and even after healing, some minor residual changes may be present. I stress the importance of adherence to post-operative instructions, including regular follow-up appointments, wearing appropriate footwear, and performing prescribed exercises. Open communication is key. Patients are encouraged to contact me with any concerns, no matter how small, to address them promptly. Proactive communication and management of expectations help to minimize post-operative anxiety and ensure patient satisfaction.
For example, I’ll explain that although their toe will likely look better, perfect symmetry may not be achieved and that some slight scarring is expected. This transparency prevents unrealistic expectations and avoids potential disappointment down the line.
Q 18. Describe your experience with different types of anesthesia used in hammertoe surgery.
Anesthesia selection for hammertoe surgery depends on various factors, including the patient’s overall health, the extent of the surgery, and personal preferences. I often utilize regional anesthesia, such as an ankle block or a digital nerve block, providing excellent pain relief with minimal systemic effects. This allows the patient to remain awake and participate in the procedure, enabling quicker recovery and reduced risk of post-operative nausea and vomiting.
In some cases, general anesthesia may be necessary, particularly for patients with comorbidities or for extensive procedures involving multiple toes or other foot deformities. The choice between regional and general anesthesia is always made in collaboration with the anesthesiologist after a thorough assessment of the patient’s individual needs and risks. The safety and comfort of the patient are paramount in these decisions.
For example, a patient with significant anxiety might prefer general anesthesia despite the benefits of regional anesthesia for a simpler procedure. In contrast, a patient who has difficulty with post-operative nausea and vomiting is a prime candidate for regional anesthesia if the procedure is suitable.
Q 19. How do you ensure proper wound healing and infection prevention after hammertoe surgery?
Proper wound healing and infection prevention are crucial after hammertoe surgery. I use meticulous surgical techniques to minimize tissue trauma during the procedure. Post-operatively, I prescribe antibiotics to reduce the risk of infection. The surgical site is dressed with sterile dressings, and the patient is instructed on proper wound care, including keeping the wound clean and dry, and changing dressings as instructed.
Patients are advised to wear appropriate, supportive footwear to protect the surgical site from pressure and trauma. Regular follow-up appointments are scheduled to monitor the healing process, assess for any signs of infection (such as redness, swelling, increased pain, or purulent discharge), and address any patient concerns. Patient education about recognizing and reporting signs of infection is emphasized. Early detection and treatment of infection are essential in minimizing complications. In cases where infection does occur, prompt and appropriate treatment with intravenous antibiotics and, if necessary, surgical debridement are implemented.
For example, I will provide patients with visual aids demonstrating proper wound care and will carefully review the signs of infection, providing them with contact information for immediate assistance if needed.
Q 20. Explain your experience with using imaging modalities (X-ray, CT scan) in hammertoe surgery.
Imaging modalities such as X-rays and CT scans play important roles in the diagnosis and treatment planning of hammertoes. X-rays provide valuable information about the bone structure, degree of joint deformity, and any associated bony abnormalities. They are routinely used to assess the severity of the hammertoe and to document the pre-operative and post-operative condition.
CT scans, while less frequently used, can provide a more detailed three-dimensional image of the bone, which can be helpful in complex cases with multiple deformities or when planning complex reconstructive procedures. For example, in cases involving significant arthritis or bone spurs, a CT scan may offer more detail than a standard X-ray.
I use X-rays to assess the extent of the deformity, plan the surgical approach, and monitor the post-operative alignment. The pre-operative X-rays serve as a baseline for comparison during follow-up visits. CT scans are reserved for specific cases requiring further clarification of the bony anatomy.
Q 21. How do you manage patients with concomitant foot deformities alongside hammertoes?
Patients often present with concomitant foot deformities alongside hammertoes, such as bunions, metatarsalgia, plantar fasciitis, or arthritis. A comprehensive assessment of all foot deformities is essential for effective treatment planning. The surgical approach needs to consider the interaction between these different deformities. Treating just one deformity without considering the others may lead to inadequate correction or even exacerbate other problems.
In cases of multiple deformities, I often advocate a staged approach, addressing the most significant deformity first and then subsequently addressing other issues. This staged approach minimizes surgical time, risk of complications, and allows for optimal healing between procedures. However, some cases may benefit from a simultaneous correction of multiple deformities. This requires careful surgical planning and may involve a longer operative time and potentially a higher risk of complications. The decision of whether to adopt a staged or simultaneous approach is tailored to the individual patient’s specific circumstances.
For example, a patient with a hammertoe and a significant bunion might benefit from a simultaneous correction of both deformities during a single surgical procedure if the bunion significantly contributes to the hammertoe deformity. However, a patient with multiple hammertoes and arthritis might benefit from a staged approach, addressing the most symptomatic hammertoe first and then dealing with others after healing.
Q 22. What are your preferred methods for addressing associated conditions like metatarsalgia?
Metatarsalgia, pain in the ball of the foot, often accompanies hammertoe deformities. My approach is multifaceted and tailored to the individual patient. It starts with a thorough assessment, considering the severity of both the hammertoe and the metatarsalgia.
Conservative management is usually the first step, involving orthotics (custom-made shoe inserts) to redistribute pressure away from the affected metatarsal heads. These are particularly useful for mild cases or to address metatarsalgia after hammertoe surgery. Physical therapy may also be recommended to strengthen the foot muscles and improve flexibility.
If conservative measures fail, surgical intervention may be necessary. During hammertoe surgery, I often address associated metatarsalgia simultaneously. Techniques include procedures such as metatarsal osteotomy (resection or realignment of the metatarsal bone) to reduce pressure on the metatarsal head. In some cases, a procedure involving removing a small wedge of bone from the metatarsal head (to change the shape and relieve pain) could be combined with hammertoe correction. The decision to combine procedures is always made on a case-by-case basis considering the patient’s specific condition and anatomy. Post-operative care includes careful weight bearing and physical therapy to ensure optimal healing and pain management.
Q 23. Describe your experience with different types of surgical instruments used in hammertoe surgery.
My experience spans a wide range of surgical instruments used in hammertoe correction. The selection depends largely on the specific surgical approach, the severity of the deformity, and the patient’s individual anatomy. For example, I frequently utilize osteotomes (used to cut bone) of varying sizes and shapes – from small, precise osteotomes for minor bone corrections to larger ones for more extensive osteotomies.
I also rely on specialized instruments like small power saws (e.g., reciprocating saws) for precise bone cuts, particularly in cases requiring more extensive bone resection or realignment. Various types of forceps and clamps are crucial for holding and manipulating tissues. Different types of drills and screws are used for fixation of bones during osteotomy procedures. For example, I utilize cannulated screws that can pass through the drill hole to guide and prevent any deviation from the desired path. Finally, meticulous surgical technique is just as important as the specialized surgical instruments in obtaining excellent surgical outcomes.
Q 24. How do you choose the correct size and type of implant for a given patient?
Implant selection is crucial for successful hammertoe surgery. The size and type of implant, whether it’s a screw, pin, or plate, are determined by several factors. First, a thorough pre-operative assessment, including imaging (X-rays), is paramount to accurately gauge the size and shape of the bones involved. This helps to tailor the implant selection to the specific anatomy of the patient.
The severity of the deformity influences the choice of implant size. A more severe hammertoe might necessitate a larger or longer screw for adequate fixation. The implant material is also carefully considered. I typically favor biocompatible materials such as titanium, which is strong, lightweight and less prone to causing allergic reactions. The type of osteotomy performed will also influence implant selection. Certain osteotomies require specific types of implants for optimal stability and healing. Ultimately, the goal is to provide stable fixation while minimizing invasiveness and trauma to surrounding soft tissue.
Q 25. Explain your approach to selecting appropriate suture materials and techniques.
Suture material and technique are critical for optimal wound healing and minimizing complications in hammertoe surgery. My selection process considers factors such as tissue type, tension on the suture line, and the expected duration of healing. For example, I commonly use absorbable sutures such as polyglactin (Vicryl) for subcutaneous tissues, as they dissolve gradually without requiring removal.
For skin closure, non-absorbable sutures, such as nylon or polypropylene, are preferred. These offer sufficient strength and support to the wound until complete healing occurs and are then removed. My suture technique employs meticulous attention to detail, ensuring proper apposition of tissues while avoiding excessive tension, which could contribute to wound dehiscence (opening). We might even use layered closure for better cosmesis and to help support different tissue layers. Each suture is placed with precision to avoid injury to nerves or blood vessels. The goal is to achieve both a strong and aesthetically pleasing outcome.
Q 26. Describe your understanding of the anatomical structures relevant to hammertoe surgery.
A thorough understanding of the foot’s anatomy is essential for successful hammertoe surgery. The key structures include the metatarsophalangeal (MTP) joint, the proximal interphalangeal (PIP) joint, and the distal interphalangeal (DIP) joint. These are the joints involved in the hammertoe deformity itself.
Understanding the extensor tendons, flexor tendons, and collateral ligaments is also vital, as these structures are carefully manipulated during the surgical procedure. The digital nerves and neurovascular bundles, which lie close to these structures, require meticulous attention to avoid injury. The periosteum (the membrane covering the bone) is also crucial in healing and bone regeneration. The intricate anatomy of the foot necessitates precise surgical planning and skillful execution to achieve a favorable outcome without compromising the integrity of surrounding tissues. Accurate identification of the bone’s shape and the extent of deformity before incision is crucial. A thorough anatomical knowledge allows me to execute precise maneuvers, minimizing potential complications.
Q 27. How do you address potential nerve damage during hammertoe surgery?
Nerve damage is a potential complication of hammertoe surgery, given the proximity of nerves to the surgical site. My approach emphasizes meticulous dissection and careful retraction of tissues during the procedure. I utilize magnification (surgical loupes or microscope) whenever necessary to improve visualization of the delicate neurovascular structures. Employing fine instruments helps to minimize tissue trauma.
Careful preoperative planning, including reviewing the patient’s imaging, helps to anticipate and avoid potential nerve impingement. Identifying the exact location of the nerves during the procedure helps avoid accidental injury. Moreover, intraoperative nerve monitoring may be used in complex cases to ensure that nerve function is preserved. Postoperative care includes close monitoring for signs of nerve injury, such as numbness or paresthesia (abnormal sensations), and addressing any such issues promptly through physical therapy or, in rare cases, further surgical intervention. The delicate nature of the nerves necessitates an extremely high level of surgical precision.
Q 28. What is your experience with treating failed hammertoe surgeries?
Treatment of failed hammertoe surgeries requires a thorough evaluation of the initial procedure and its outcome. This begins with a careful review of the patient’s history, previous surgical notes, and radiographic images. The cause of the failure needs to be identified—it could be due to improper surgical technique, inadequate implant fixation, infection, or recurrent deformity.
The approach to revision surgery varies widely, depending on the cause of failure. This might involve removing the existing implants, addressing any infection, and revising the original osteotomy. In some cases, a different surgical technique may be adopted depending on the initial methodology used. For example, if the initial surgery involved a less invasive approach and that failed, revision surgery may require more extensive procedures. Other times, the failed surgery might have been adequately performed but the patient’s response was less than anticipated. In all cases, careful planning and a meticulous surgical approach are vital to increase the likelihood of successful revision surgery.
Key Topics to Learn for Hammertoe Surgery Interview
- Anatomy and Biomechanics of the Foot: Understanding the intricate structure of the foot, including bones, tendons, ligaments, and muscles, is crucial. Focus on the mechanics of hammertoe deformity development.
- Surgical Techniques for Hammertoe Correction: Familiarize yourself with various surgical approaches, including arthrodesis, tendon transfers, and osteotomy. Understand the indications and contraindications for each technique.
- Pre-operative Assessment and Planning: Master the process of evaluating patients, including physical examination, radiographic interpretation, and patient history. Learn how to develop a comprehensive surgical plan based on individual needs.
- Post-operative Care and Rehabilitation: Understand the importance of post-operative management, including pain control, wound care, and physical therapy protocols. Be prepared to discuss potential complications and their management.
- Complications and Their Management: Thoroughly review potential complications like infection, nerve damage, and non-union. Understand the diagnostic and treatment approaches for managing these issues.
- Patient Selection and Communication: Learn to effectively assess patient suitability for surgery and communicate the risks and benefits of the procedure clearly and empathetically.
- Current Trends and Research in Hammertoe Surgery: Stay updated on the latest advancements in surgical techniques, implants, and rehabilitation protocols. Demonstrate your commitment to continuous learning.
Next Steps
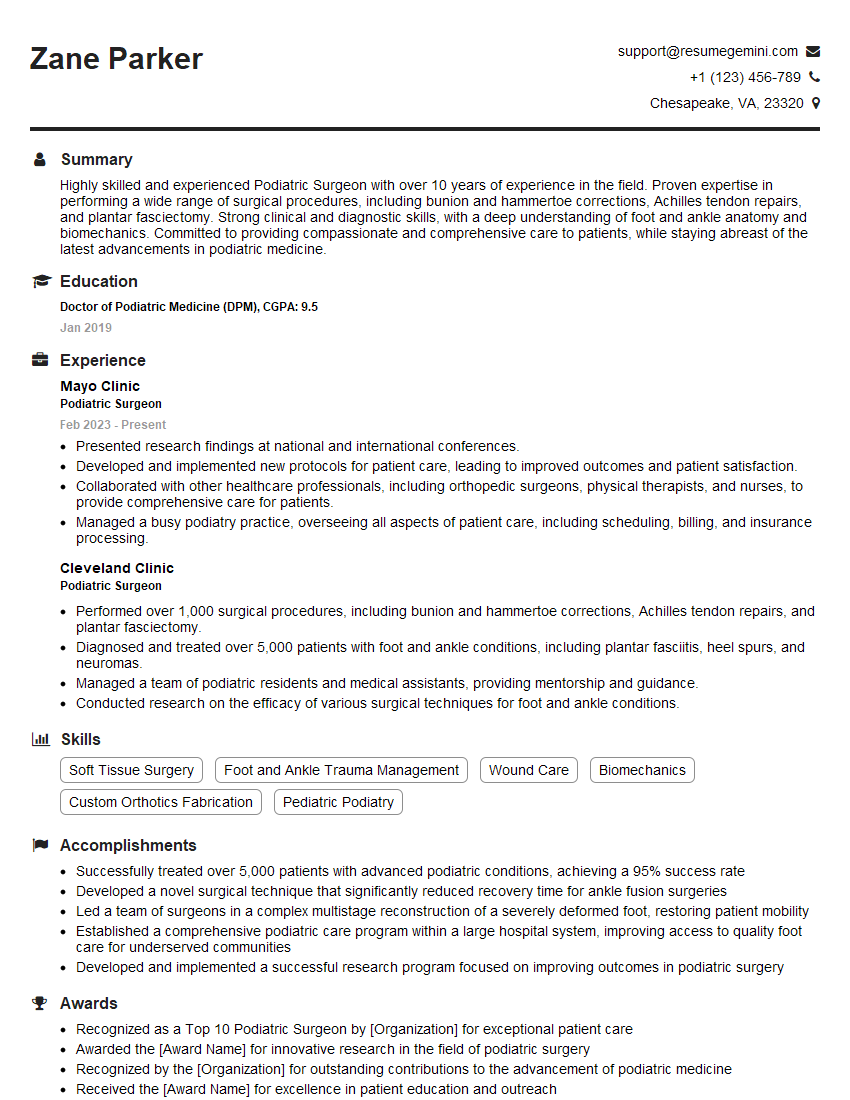
Mastering Hammertoe Surgery opens doors to exciting career opportunities and allows you to make a real difference in patients’ lives. To maximize your chances of landing your dream job, it’s essential to present your skills and experience effectively. Creating an ATS-friendly resume is crucial for getting your application noticed by recruiters. We highly recommend using ResumeGemini to build a professional and impactful resume tailored to the specific requirements of Hammertoe Surgery positions. Examples of resumes optimized for this field are available to guide you. Take the next step towards your career success today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.