Unlock your full potential by mastering the most common Color vision assessment interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Color vision assessment Interview
Q 1. Explain the difference between color deficiency and color blindness.
The terms “color deficiency” and “color blindness” are often used interchangeably, but there’s a subtle difference. Color deficiency is a more accurate and encompassing term. It refers to a reduced ability to distinguish between certain colors, ranging from mild difficulty to complete inability. Color blindness, while widely used, is a less precise term often implying a complete lack of color vision, which is rare. Think of it this way: color deficiency is the umbrella term, while color blindness represents a specific, extreme end of the spectrum.
Q 2. Describe the Ishihara test and its limitations.
The Ishihara test is a widely used, quick screening tool for color vision deficiencies. It consists of a series of colored plates, each containing a number or pattern embedded within a background of differently colored dots. Individuals with normal color vision can easily identify the numbers or patterns, while those with deficiencies may see different numbers or have difficulty discerning them.
However, the Ishihara test has limitations. It primarily detects red-green color deficiencies and is less effective at identifying blue-yellow deficiencies or milder forms of color vision impairment. It’s also susceptible to errors due to lighting conditions and test administration inconsistencies. It serves as a good initial screening, but further testing is often needed for a definitive diagnosis and detailed characterization of the deficiency.
Q 3. What are the various types of color vision deficiencies?
Color vision deficiencies are categorized primarily by the types of cones affected (cones are photoreceptor cells in the retina responsible for color vision). The main types are:
- Red-Green color deficiency (most common): This encompasses protanopia (lack of functioning red cones), deuteranopia (lack of functioning green cones), and protanomaly and deuteranomaly (reduced function of red and green cones, respectively). Individuals with these deficiencies struggle to distinguish shades of red and green.
- Blue-Yellow color deficiency (less common): This includes tritanopia (lack of functioning blue cones) and tritanomaly (reduced function of blue cones). Individuals with these deficiencies have difficulty distinguishing blues and yellows.
- Monochromacy (rare): This is a complete lack of color vision, resulting in a grayscale perception of the world. There are two types: rod monochromacy (complete lack of cone function) and cone monochromacy (only one type of cone is functional).
It’s important to note that the severity of a color deficiency can vary greatly within each type.
Q 4. Explain the Farnsworth-Munsell 100-Hue test.
The Farnsworth-Munsell 100-Hue test is a more comprehensive and precise method for assessing color vision than the Ishihara test. It involves arranging 100 colored caps in a circle, ordering them from hue variations along a color spectrum. The test is scored based on the number and magnitude of errors made in arranging the caps. This provides a quantitative measure of the degree and type of color vision deficiency, offering a more nuanced assessment than the Ishihara test. It’s especially useful for identifying subtle color vision defects and distinguishing between different types of color deficiencies, including blue-yellow deficiencies, which the Ishihara test struggles to detect accurately.
Q 5. How do you interpret the results of a color vision test?
Interpreting color vision test results requires careful consideration of the specific test used and the individual’s performance. For example, the Ishihara test results are typically categorized as normal or showing a specific type of color deficiency (e.g., red-green). The Farnsworth-Munsell 100-Hue test provides a numerical score indicating the magnitude and type of color vision defect.
The results aren’t simply a pass/fail; they provide information about the type and severity of the color vision deficiency, guiding appropriate accommodations or further investigation. For instance, a high error score on the 100-Hue test suggests a more significant color vision problem than a few errors on the Ishihara test. Clinicians combine test results with a patient’s medical history and symptoms for a comprehensive diagnosis and management plan.
Q 6. Discuss the genetic basis of color vision deficiencies.
Color vision deficiencies are primarily inherited, with the genes responsible for the production of photopigments in the cone cells located on the X chromosome. This explains why they are far more common in males (who have only one X chromosome) than females (who have two X chromosomes; a normal gene on one X chromosome can compensate for a defective gene on the other). Most red-green deficiencies are linked to mutations in the genes for the opsin proteins in the red and green cone photopigments. Blue-yellow deficiencies are less common and involve different genetic mechanisms.
Q 7. What are the common causes of acquired color vision deficiencies?
Acquired color vision deficiencies, while less frequent than inherited ones, can result from various conditions affecting the visual pathway. These include:
- Eye diseases: Glaucoma, cataracts, macular degeneration, and optic neuritis can all impact color vision.
- Neurological disorders: Conditions such as multiple sclerosis or stroke can damage the neural pathways involved in color processing.
- Toxic exposure: Exposure to certain chemicals or medications (e.g., some antibiotics or anti-malarial drugs) can temporarily or permanently affect color vision.
- Head trauma: Injuries to the head can sometimes lead to acquired color vision deficiencies.
Understanding the cause of an acquired color vision deficiency is crucial for appropriate treatment and management. Addressing the underlying condition may improve or stabilize color vision, though full recovery isn’t always possible.
Q 8. Explain the difference between congenital and acquired color vision deficiencies.
The key difference between congenital and acquired color vision deficiencies lies in their onset. Congenital color vision deficiencies, also known as color blindness, are present from birth. They’re typically inherited, resulting from genetic mutations affecting the cone cells in the retina responsible for color perception. Think of it like being born with a slightly ‘miswired’ color processing system. These deficiencies are usually stable throughout life.
In contrast, acquired color vision deficiencies develop later in life due to various factors such as eye diseases (e.g., cataracts, glaucoma, macular degeneration), neurological conditions, or exposure to toxins. Imagine your perfectly functioning color system being damaged by an external factor. These deficiencies can vary in severity and may even be reversible depending on the underlying cause and its treatment. For instance, cataract surgery can sometimes improve color vision if cataracts were the contributing factor.
Q 9. How do you differentiate between protanopia, deuteranopia, and tritanopia?
Protanopia, deuteranopia, and tritanopia are the three main types of inherited color vision deficiencies, each affecting a different type of cone cell:
- Protanopia: Affects the long-wavelength (red) cone cells. Individuals with protanopia have difficulty distinguishing reds and greens, often perceiving them as shades of yellow or gray. Imagine a world where ripe tomatoes and green leaves look strikingly similar.
- Deuteranopia: Affects the medium-wavelength (green) cone cells. Similar to protanopia, individuals struggle to differentiate reds and greens. The impact on color perception might be slightly different from protanopia, but the overall difficulty in red-green discrimination remains.
- Tritanopia: Affects the short-wavelength (blue) cone cells. This is the rarest type and involves difficulty distinguishing blues and yellows. The world might appear more muted in terms of blue and yellow hues. Imagine a clear sky appearing more gray-white.
These distinctions are made through careful testing using various color vision tests, observing the specific types of color confusion experienced by the individual. The Ishihara plates, for example, are designed to pinpoint these specific cone deficiencies.
Q 10. Describe the clinical significance of color vision deficiencies in various professions.
Color vision deficiencies can significantly impact professional performance in various fields. For example, in professions requiring precise color discrimination, such as:
- Piloting/Aviation: Misinterpreting signal lights could have catastrophic consequences.
- Medicine: Diagnosing conditions often relies on recognizing subtle color variations in tissues or blood tests.
- Art and Design: Accurate color perception is fundamental for creating and reproducing art.
- Textiles and Fashion: Matching colors accurately is crucial in manufacturing and design.
The clinical significance lies in identifying these deficiencies early, especially in high-risk professions. Appropriate accommodations, such as using color-coded software with alternative cues, modified testing procedures, or assistive technologies, can help mitigate potential risks and ensure safe and effective professional practice.
Q 11. What are the challenges in assessing color vision in children?
Assessing color vision in children presents unique challenges. Young children may lack the verbal skills to accurately describe what they see, making traditional tests, like the Ishihara plates, less reliable. Their attention spans might be shorter, and they may not fully understand the instructions. Moreover, the development of their color vision continues throughout early childhood, making it crucial to consider developmental norms when interpreting results.
Strategies for overcoming these challenges include using age-appropriate tests, incorporating play-based methods, and employing alternative assessment tools that rely less on verbal responses and more on behavioral observations. Building rapport and trust with the child is essential for obtaining reliable data. In some cases, parents or caregivers can provide valuable information on the child’s color perception.
Q 12. How would you adapt your assessment approach for individuals with low vision?
Adapting the assessment approach for individuals with low vision requires sensitivity and creativity. Standard color vision tests often rely on sharp visual acuity; individuals with low vision might struggle with the visual details. Modifying the test parameters is often necessary. For instance:
- Enlarging the test plates: This makes the colored patterns easier to distinguish.
- Increasing the contrast: This makes the color differences more apparent.
- Using alternative methods: This might include evaluating color discrimination using verbally described color samples rather than visually presented ones.
- Adjusting the lighting conditions: This can enhance visibility and reduce glare.
The overall goal is to modify the testing environment and techniques to match the individual’s visual capabilities, while still obtaining a reliable assessment of their color perception abilities. Using a combination of methods to gather data often provides the most complete picture.
Q 13. What are some alternative methods for color vision assessment beyond the traditional tests?
Beyond traditional tests like the Ishihara plates and Farnsworth-Munsell 100-hue test, alternative methods exist for assessing color vision. These include:
- Computerized color vision tests: These offer advantages in terms of standardization, automated scoring, and adaptive testing protocols, tailoring the difficulty of the test to the individual’s performance.
- Electrophysiological methods: Techniques like electroretinography (ERG) and multifocal ERG can measure the electrical responses of the retina to different wavelengths of light, providing objective information about cone function. These are more commonly used in research settings and when investigating underlying physiological mechanisms of color vision deficits.
- Behavioral assessments: Observing how an individual interacts with colors in real-life scenarios, such as sorting colored objects or identifying colors in everyday items, can provide valuable insights, particularly useful in younger children or individuals with limited verbal communication abilities.
Choosing the appropriate method depends on the clinical context, the individual’s abilities and cooperation, and the resources available. Often, a combination of methods provides the most complete and accurate assessment.
Q 14. Discuss the role of technology in color vision assessment.
Technology plays a crucial role in modern color vision assessment. Computerized tests are more efficient, offer objective scoring, and can adapt to the individual’s performance. Software analysis can detect subtle differences that might be missed by human observation. For instance, some programs can analyze an individual’s responses to color stimuli and generate a detailed report of their color vision performance.
Furthermore, technologies like virtual reality (VR) and augmented reality (AR) offer exciting possibilities for creating more immersive and engaging color vision tests, potentially leading to more accurate and reliable assessments, especially in pediatric populations. The ongoing development of sophisticated image processing techniques also enhances the accuracy and efficiency of color vision analysis.
Q 15. Explain the concept of color matching and its application in color vision assessment.
Color matching is a fundamental principle in color vision assessment. It’s based on the idea that individuals can match any color by mixing together specific proportions of three primary colors – typically red, green, and blue. This is done using a colorimeter or similar device. In a color vision assessment, we use this principle to understand how an individual perceives and mixes colors. For example, someone with normal color vision will mix the primaries in a specific ratio to match a target color, while someone with a color vision deficiency might require different proportions, revealing their altered perception of color.
Its application is crucial because it allows us to quantify the nature and severity of color vision deficiencies. The discrepancies between a patient’s color matches and the matches made by someone with normal vision provide a precise measurement of their color vision defect. This quantitative data is essential for diagnosis, treatment planning (e.g., specialized lenses or software), and even occupational guidance. For instance, a pilot with a significant color vision deficiency might be restricted from certain roles based on the findings from a color matching test.
Career Expert Tips:
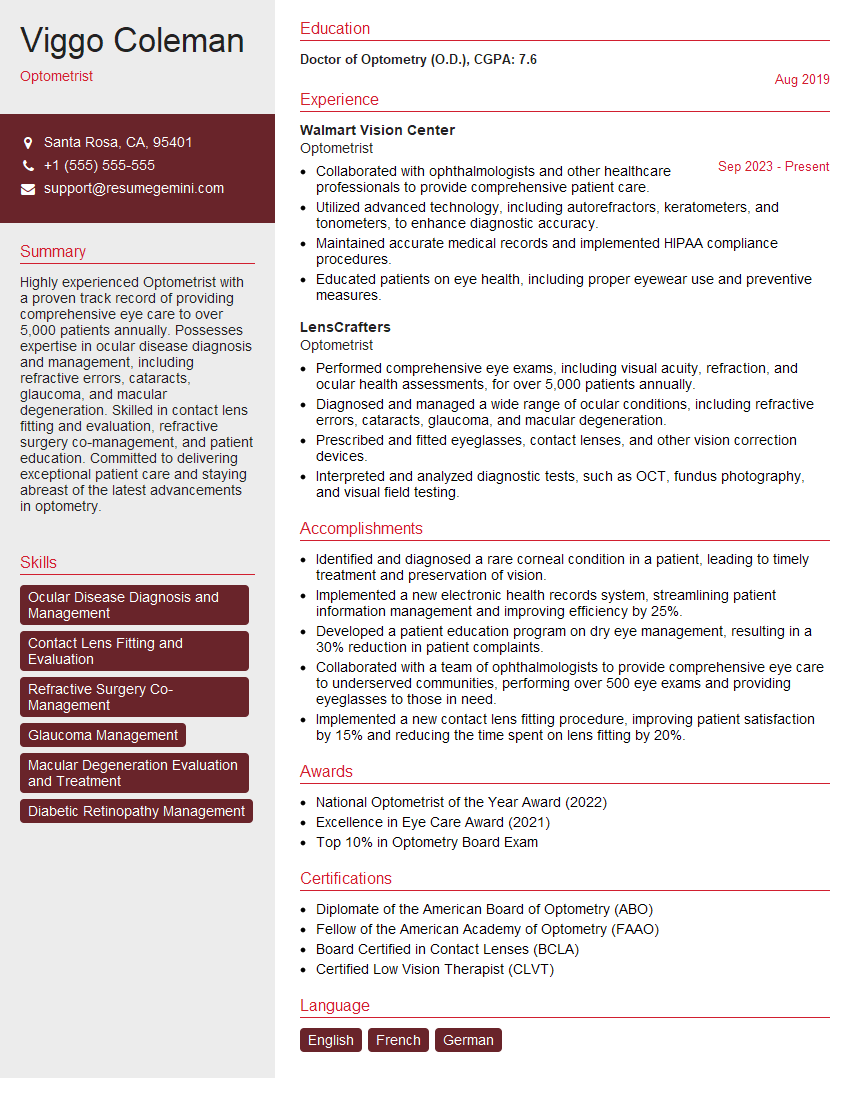
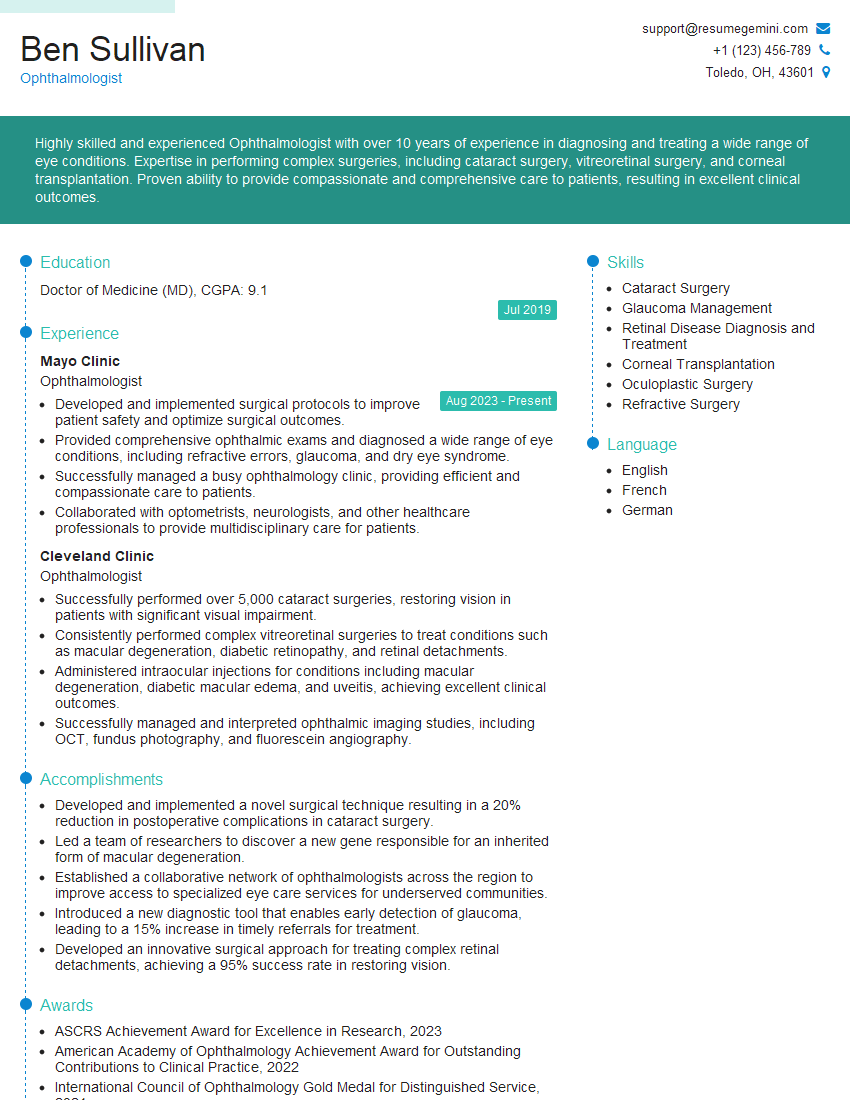
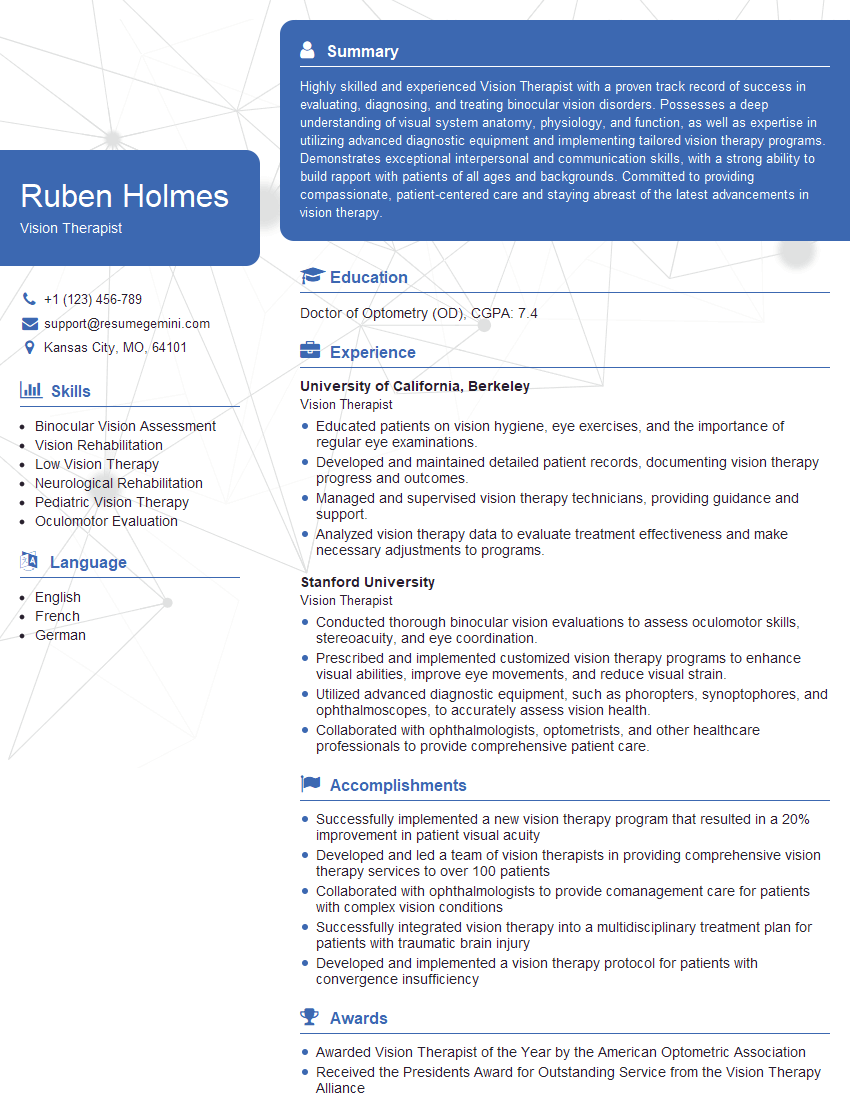
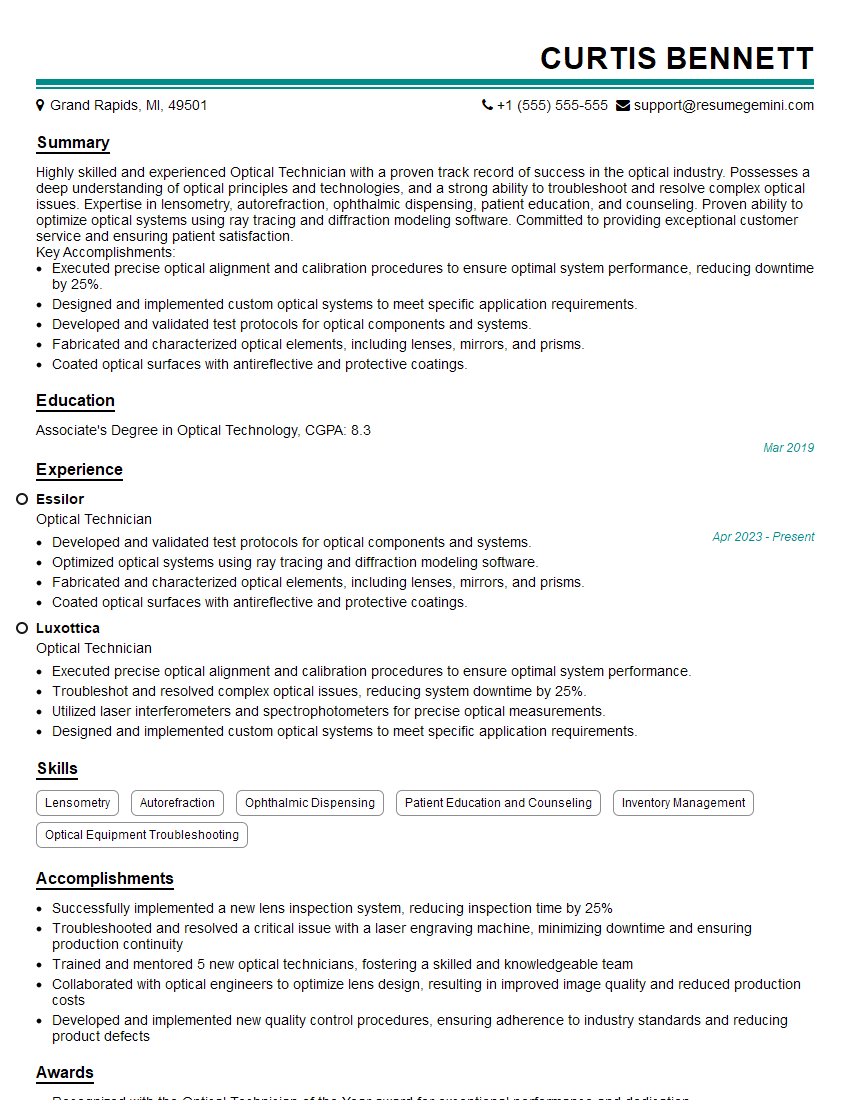
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the ethical considerations in conducting color vision assessments?
Ethical considerations in color vision assessments are paramount. We must ensure informed consent – the patient understands the purpose, procedures, and potential implications of the test before participating. Confidentiality is vital; test results are sensitive personal information and must be handled with utmost care and privacy. Accuracy and reliability of testing are also ethical imperatives. Using outdated or poorly calibrated instruments or employing improper testing procedures can lead to inaccurate results, potentially impacting a patient’s life choices. We must always strive for objectivity, avoiding bias in interpretation of results. For instance, if we suspect a patient might have a color vision deficiency due to family history, we mustn’t let this preconception influence our assessment. The results must be based purely on the objective data obtained from the test.
Additionally, it’s crucial to consider the impact of the assessment on the patient’s self-esteem and psychological well-being. Color vision deficiencies can cause emotional distress, especially if they impact employment or daily life. Providing sensitive, empathetic counseling alongside the results is a key ethical consideration. It is our responsibility to help individuals understand their condition, manage its limitations, and use their strengths effectively.
Q 17. How do you ensure the accuracy and reliability of color vision test results?
Ensuring accuracy and reliability starts with using validated and well-maintained instruments. Regular calibration of colorimeters and other assessment tools is crucial to minimize measurement errors. We also need to adhere to standardized testing procedures; each test should be conducted under consistent lighting conditions, using standardized stimuli and following established protocols. This guarantees that the results are comparable across different assessments and across different practitioners.
In addition to the technical aspects, careful attention to the testing environment is important. Minimizing distractions and ensuring the patient is comfortable and relaxed contribute to accurate results. For repeatability, we often conduct multiple trials of the same test and compare the results. Discrepancies can highlight potential sources of error, whether human or technical. We often use statistical analysis to evaluate the consistency of the results and identify any outliers that might indicate issues with the assessment process. It’s critical to document every step of the process meticulously, maintaining a complete and traceable record of the assessment.
Q 18. How do you communicate complex color vision test results to patients?
Communicating complex results requires clear, patient-centered language. Avoiding technical jargon is essential; instead of saying ‘anomalous trichromacy’, I might explain, ‘Your color vision is slightly different from normal; your eyes mix colors in a way that’s a little unusual’. I use visual aids, such as color plates showing the types of color confusion they may experience, to help them understand their specific condition. I then explain the implications of their condition in simple terms, relating it to potential challenges in their daily life or occupation.
I also emphasize that a color vision deficiency is not a disability; many people live full and productive lives with these conditions. I explore coping strategies and available assistive technologies like specialized software or eyewear. The conversation is focused on empowerment and providing resources to help them navigate their individual circumstances. For example, if the patient is a driver, I would explain the potential implications and inform them about driving regulations related to color vision. Open dialogue and active listening ensure that the patient feels understood and supported.
Q 19. Describe your experience with different types of color vision assessment instruments.
My experience encompasses a range of color vision assessment instruments, from traditional pseudoisochromatic plates (like Ishihara and Farnsworth-Munsell 100-hue) to computerized tests like the Anomaloscope and digital color vision analyzers. Pseudoisochromatic plates are relatively simple and cost-effective but are somewhat subjective and rely on the patient’s response to hidden numbers or patterns within colored fields. Anomaloscopes, on the other hand, allow for precise quantitative measurement of color matching ability using adjustable light sources and offer more detailed diagnostic information. Computerized tests often incorporate a wider variety of color stimuli and may incorporate dynamic test paradigms which provides a more comprehensive assessment.
I’ve worked extensively with the Farnsworth-Munsell 100-hue test which is particularly good at differentiating various types of color vision deficiencies. The choice of instrument depends on the specific clinical need and the resources available. For routine screening, pseudoisochromatic plates might suffice, while a more detailed assessment might necessitate the use of an anomaloscope or a computerized system. My experience covers a range of technologies ensuring I can select the most appropriate methodology for each individual’s needs.
Q 20. What are the limitations of current color vision assessment techniques?
Current color vision assessment techniques have some limitations. Pseudoisochromatic plates can be influenced by factors such as lighting conditions and the patient’s attention and cooperation level. They may also not accurately capture the full spectrum of color vision deficiencies, particularly in milder cases. The interpretation of some tests can be subjective, leading to variability between assessors. Furthermore, current methods may not fully assess the dynamic aspects of color perception or the impact of different lighting conditions on color discrimination. Most assessments focus on static color perception, without necessarily assessing the effects of speed or temporal aspects of color.
Another significant limitation is the lack of standardized procedures across different settings and instruments. This inconsistency can make it challenging to compare results obtained from different tests or in different locations. The development of more sophisticated, standardized, and objective assessment techniques that are less susceptible to these limitations is an ongoing area of research and development. This includes exploring advanced technologies like spectral imaging and developing better algorithms for analyzing and interpreting color vision data.
Q 21. Explain the use of color vision assessments in the diagnosis of neurological conditions.
Color vision assessments play a crucial role in the diagnosis of several neurological conditions. Disorders affecting the visual pathways, such as optic neuritis, multiple sclerosis, and certain types of brain tumors can lead to acquired color vision defects. Changes in color perception can be an early sign of these neurological problems and thus, assessment of color vision can be a helpful diagnostic tool in detecting and monitoring disease progression. A thorough color vision assessment, particularly one that examines the spatial distribution and characteristics of color vision defects, might provide clues about the precise location of the neurological lesion.
For example, a specific type of color vision loss might be indicative of damage to a particular part of the optic nerve or visual cortex. The results from the color vision test should not be interpreted in isolation but rather considered in the context of other neurological examinations, brain imaging studies (MRI, CT scans), and clinical history to make a comprehensive diagnosis. In many situations, it can serve as a useful screening tool or aid in tracking changes in neurological status over time. It’s important to remember that color vision abnormalities can arise from multiple causes, and comprehensive assessment involving other techniques is always necessary for an accurate diagnosis.
Q 22. How do you manage a situation where a patient disputes their color vision test results?
Patient disputes about color vision test results are handled with empathy and a thorough review process. First, I’d calmly acknowledge their concerns and reiterate the test’s purpose and limitations. It’s crucial to understand the basis of their skepticism; perhaps they feel the test didn’t accurately reflect their daily experiences. Next, I’d carefully review the test procedure – ensuring it was administered correctly, the patient understood the instructions, and environmental factors didn’t interfere (lighting, for example). If any inconsistencies are found, a retest using a different method (e.g., switching from Ishihara plates to a Farnsworth-Munsell 100 Hue test) is warranted. In some cases, a consultation with an ophthalmologist is recommended to rule out other ophthalmological issues influencing color perception. Open communication, transparency in explaining the test results, and reiterating the implications of the findings are key to achieving mutual understanding and acceptance.
For example, a patient might dispute a diagnosis of mild red-green deficiency because they haven’t experienced problems in their daily life. I might explain that mild deficiencies often only manifest in specific situations, like distinguishing traffic lights under low light, or identifying specific shades in their profession. Showing them examples on a color vision simulator might help them understand their limitations better.
Q 23. What are the latest advancements in color vision assessment technology?
The field of color vision assessment is constantly evolving. Recent advancements include the development of more sophisticated automated tests using digital platforms and software. These offer advantages over traditional methods such as the Ishihara plates, providing objective, quantifiable results and minimizing subjectivity. Some systems utilize advanced algorithms to analyze color discrimination and identify specific types and severities of color vision deficiencies with greater accuracy. An example is the use of computer-based tests that can assess color discrimination under varying luminance conditions, mimicking real-world scenarios. Additionally, research is exploring genetic testing for color vision deficiencies, offering early detection and more precise diagnosis.
Another significant advance is the integration of virtual reality (VR) technology in testing and rehabilitation. VR environments allow for more immersive and realistic scenarios for assessing and training color perception, particularly beneficial for patients with significant deficiencies or for occupational training.
Q 24. Describe your experience with managing patients with different types of color vision deficiencies.
My experience encompasses a broad range of color vision deficiencies, including protanopia (lack of red cones), deuteranopia (lack of green cones), tritanopia (lack of blue cones), and various forms of anomalous trichromacy (reduced sensitivity to one or more cone types). Each deficiency requires a tailored approach. For instance, patients with protanopia might struggle with red-green discrimination, impacting their ability to differentiate traffic signals or interpret certain medical charts. I would explain the nature of their deficiency, its implications, and advise on strategies to compensate in everyday life, such as using assistive software or apps designed to enhance color contrast. Patients with deuteranopia would receive similar guidance, while those with tritanopia, which is far rarer, would need assistance tailored to their specific color perception challenges, such as difficulties distinguishing blues and yellows.
Managing patients also involves understanding the emotional and psychological impact of color vision deficiencies. Many individuals feel frustrated or embarrassed by their limitations, especially if their profession or daily life relies on accurate color perception. Providing reassurance, explaining adaptive strategies, and promoting self-advocacy skills are integral parts of the care process.
Q 25. How do you determine the severity of a color vision deficiency?
Determining the severity of a color vision deficiency involves using standardized tests that quantify the level of color discrimination impairment. The Farnsworth-Munsell 100 Hue test, for example, provides a numerical score representing the degree of error in arranging colored caps in order of hue. Lower scores indicate better color discrimination, while higher scores reflect greater impairment. Similarly, the Lanthony D-15 desaturated color test assesses color discrimination in a more clinically controlled setting. The Ishihara plates, while less quantitative, allow for the classification of color vision deficiency type and a rough estimate of severity based on the number of plates correctly identified. Further analysis often incorporates the patient’s self-reported difficulties and the impact of the deficiency on their daily life. This holistic approach helps paint a complete picture of the severity and implications of the deficiency.
Q 26. What are the different types of corrective lenses or aids available for individuals with color vision deficiencies?
Currently, there aren’t any corrective lenses or aids that can fully correct color vision deficiencies. However, several assistive technologies can improve color discrimination and reduce the impact of the deficiency. Specialized color-correcting filters or lenses (often tinted glasses) can modify the wavelengths of light reaching the eye, making it easier to distinguish certain colors. These filters are generally tailored to the specific type of color blindness. Software and apps are also available that enhance color contrast and help differentiate colors digitally; these are beneficial for tasks involving computer screens, charts, or images. Certain apps can change the hue and saturation of images and videos based on the user’s requirements. Although not a ‘cure,’ these aids can provide significant assistance and improve independence for individuals with color vision deficiencies.
Q 27. Discuss the role of color vision assessment in occupational health and safety.
Color vision assessment plays a crucial role in occupational health and safety, especially in industries where accurate color perception is vital for safety and efficiency. Pilots, train operators, electricians, and medical professionals, for example, need accurate color vision to interpret signals, distinguish wires, or analyze medical images correctly. Pre-employment screening for color vision deficiencies is standard practice in these professions to identify individuals who might pose a safety risk to themselves or others. Furthermore, routine color vision tests can be incorporated into periodic health assessments for those already employed in color-critical roles to ensure ongoing fitness for duty. Early detection of any deterioration in color vision can prevent accidents and ensure continued safe performance.
Q 28. How would you approach the assessment of color vision in a multicultural setting?
Assessing color vision in a multicultural setting requires cultural sensitivity and awareness of potential confounding factors. Firstly, it’s essential to consider that color perception and naming can vary across cultures. What one culture considers ‘green’ might be slightly different in another. The tests should be standardized to minimize bias and ensure fairness across different cultural groups. Using tests with universal color stimuli, avoiding culturally specific color terms or images, and providing clear, translated instructions are crucial steps. Additionally, I would be mindful of potential differences in visual acuity or exposure to light, which might influence test results. Interpreting results should also be done cautiously, keeping in mind cultural differences in color perception. If possible, using a test administrator from the same cultural background as the patient can improve communication and understanding and enhance test validity.
Key Topics to Learn for Color Vision Assessment Interview
- Types of Color Vision Deficiency: Understand the different types of color blindness (e.g., protanopia, deuteranopia, tritanopia) and their impact on visual perception.
- Color Vision Testing Methods: Familiarize yourself with various tests used to assess color vision, including Ishihara plates, Farnsworth-Munsell 100-hue test, and digital color vision tests. Be prepared to discuss the strengths and limitations of each method.
- Clinical Significance: Discuss the importance of accurate color vision assessment in various fields, such as aviation, healthcare, and design. Understand how color vision deficiencies can impact job performance and safety.
- Interpreting Test Results: Learn how to interpret the results of different color vision tests and understand what the findings signify regarding the severity and type of color vision deficiency.
- Technological Applications: Explore the role of technology in assessing and compensating for color vision deficiencies, such as color correction software and specialized eyewear.
- Ethical Considerations: Understand the ethical implications of color vision assessment and the importance of ensuring fair and unbiased testing practices.
- Differential Diagnosis: Be prepared to discuss how to differentiate between true color vision deficiency and other conditions that might mimic color vision problems.
Next Steps
Mastering color vision assessment knowledge significantly enhances your career prospects in various fields requiring precise visual perception. A strong understanding of this area demonstrates crucial skills and attention to detail, making you a more competitive candidate. To maximize your job search success, create an ATS-friendly resume that highlights your expertise. ResumeGemini is a trusted resource to help you build a professional and impactful resume that gets noticed. We provide examples of resumes tailored to Color vision assessment roles to help guide you. Take the next step in your career journey – build your best resume today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.