Unlock your full potential by mastering the most common Cough Assist interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Cough Assist Interview
Q 1. Describe the mechanism of action of Cough Assist.
Cough Assist is a device that helps patients with weak or ineffective coughs clear secretions from their airways. Its mechanism of action revolves around delivering positive and negative pressures to the lungs in a controlled manner, mimicking a natural cough.
During the inspiratory phase, the device delivers a positive pressure, inflating the lungs with air. This is followed by a brief pause, allowing for adequate air filling.
Then, in the expiratory phase, the device generates a negative pressure, assisting in the forceful expulsion of air and secretions from the lungs. This negative pressure helps to overcome airway resistance and facilitate a more effective cough.
Think of it like this: the positive pressure is like a deep breath, and the negative pressure is like the forceful push of a cough. The machine simply enhances and supports this natural process for patients who struggle to do so independently.
Q 2. Explain the contraindications for Cough Assist therapy.
Contraindications for Cough Assist therapy are situations where using the device could be harmful. These include:
- Recent facial, oral, or nasal surgery: The pressure changes could disrupt healing or cause bleeding.
- Uncontrolled hemoptysis (coughing up blood): Cough Assist could worsen the bleeding.
- Pneumothorax (collapsed lung): The pressure changes could further damage the lung.
- Active pulmonary hemorrhage: Similar to hemoptysis, this represents a risk of increased bleeding.
- Certain unstable cardiovascular conditions: The pressure changes may put an extra strain on the heart.
- Severe head trauma or increased intracranial pressure: Pressure fluctuations could be harmful to the brain.
- Uncontrolled vomiting or nausea: The procedure could induce more vomiting.
- Recent esophageal surgery: Pressure changes may disrupt the healing process.
Always consult with a physician to determine suitability for Cough Assist, considering the patient’s specific medical history and condition.
Q 3. What are the different modes of Cough Assist and when would you use each?
Cough Assist devices typically offer several modes of operation:
- Assisted Cough: This is the most common mode. It uses both positive and negative pressures to assist the patient’s cough. It’s ideal for patients who can initiate their own cough but need assistance to make it more effective.
- Forced Cough: This mode delivers both positive and negative pressures without the patient initiating a cough. It’s used for patients who are completely unable to cough effectively on their own.
- Inspiratory Support: This mode only provides positive pressure, helping patients with weak inspiratory muscles to take a deeper breath. This can be helpful before attempting an assisted cough.
- Expiratory Support: This mode primarily provides negative pressure to aid in clearing secretions. Useful for patients with weak expiratory muscles.
The choice of mode depends entirely on the patient’s individual respiratory capabilities and needs. A thorough assessment is crucial for selecting the most appropriate mode and adjusting the settings accordingly.
Q 4. How do you assess a patient’s suitability for Cough Assist?
Assessing a patient’s suitability for Cough Assist involves a multi-faceted approach:
- Respiratory Assessment: Evaluate the patient’s cough effectiveness, respiratory rate, oxygen saturation, lung sounds, and the presence of secretions.
- Medical History: Review the patient’s medical history for contraindications, such as those listed previously.
- Physical Assessment: Assess the patient’s level of consciousness, muscle strength, and overall ability to cooperate with the therapy.
- Trial Run: Often, a short trial run of the Cough Assist is performed under close supervision to assess the patient’s response and tolerance.
A comprehensive evaluation helps to determine whether the patient will benefit from Cough Assist and what settings should be used.
Q 5. What are the potential complications associated with Cough Assist therapy?
While generally safe, Cough Assist therapy carries some potential complications:
- Hypoxemia (low blood oxygen): This can occur if the device settings are not appropriately adjusted.
- Hypotension (low blood pressure): This may result from the negative pressure phase.
- Injury to the airway or lungs: This risk is minimized by proper technique and device settings.
- Pain or discomfort: Some patients may experience discomfort during therapy.
- Nausea or vomiting: This can be a response to the pressure changes.
- Infection: Proper hygiene practices during therapy are crucial to minimize infection risk.
Careful monitoring and appropriate adjustments of settings by trained personnel are essential in mitigating these risks.
Q 6. How do you monitor a patient’s response to Cough Assist therapy?
Monitoring a patient’s response to Cough Assist is crucial for optimizing therapy and ensuring safety. This includes:
- Monitoring vital signs: Closely monitor heart rate, blood pressure, oxygen saturation, and respiratory rate before, during, and after each treatment session.
- Assessing secretion clearance: Observe the amount and characteristics of secretions removed. Improvement in cough effectiveness should also be noted.
- Assessing patient tolerance: Monitor the patient for signs of discomfort, pain, or distress during and after the treatment.
- Regular assessment of lung sounds: Listening to lung sounds can help to assess the effectiveness of the therapy and detect any adverse effects.
- Documenting all observations: Maintain detailed records of the treatment sessions, including settings used, patient response, and any complications observed.
Based on these observations, adjustments to the device settings may be necessary to improve efficacy and patient comfort.
Q 7. What are the common settings adjustments for different patient populations (e.g., pediatrics, geriatrics)?
Settings adjustments for different patient populations often involve modifications to pressure levels, inspiratory/expiratory ratios, and treatment durations:
- Pediatrics: Lower pressure settings and shorter treatment times are generally used in children due to their smaller lung volumes and increased airway sensitivity. Careful attention should be paid to their tolerance and response.
- Geriatrics: Older adults might require more gradual pressure increases and longer expiratory times, considering age-related changes in lung compliance and muscle strength. A gentler approach is often warranted.
It’s crucial to remember that these are general guidelines. Individualized adjustments are necessary based on each patient’s unique needs and tolerance. Experienced clinicians make these decisions based on ongoing monitoring and careful observation of the patient’s responses.
Q 8. Describe the process of setting up and operating a Cough Assist device.
Setting up and operating a Cough Assist device involves several steps to ensure patient safety and effective treatment. First, you’ll need to assemble the device according to the manufacturer’s instructions, typically involving connecting the tubing and ensuring all parts are securely fastened. Next, you’ll select the appropriate settings based on the patient’s individual needs and respiratory status. This often involves adjusting pressure levels (typically measured in cm H2O), inspiratory and expiratory times, and the number of cycles. The pressure setting is crucial; it needs to be high enough to assist the patient in generating a cough, but not so high as to cause discomfort or injury. It’s vital to start with a low pressure and gradually increase it as tolerated.
Once the settings are determined, you’ll help the patient assume a comfortable seated or semi-recumbent position. The mask or mouthpiece is then properly secured, creating an airtight seal. The Cough Assist device is then activated, and the programmed cycle begins. During the inspiratory phase, the device delivers positive pressure, expanding the lungs and promoting deeper breaths. This is followed by an expiratory phase, typically with a lower pressure setting, assisting the patient to exhale more forcefully. Finally, a brief period of apnea (no breathing) may follow before the cycle repeats. Continuous monitoring of the patient’s respiratory status and comfort is critical during the treatment.
Think of it like this: the Cough Assist is like a helping hand for your lungs. It assists with the deep breath (inspiration) necessary for an effective cough and then helps forcefully expel air (expiration) to clear secretions. Patient education is crucial for comfort and successful usage.
Q 9. How do you troubleshoot common problems encountered with Cough Assist devices?
Troubleshooting Cough Assist devices requires a systematic approach. Common problems include insufficient cough, discomfort, or device malfunctions. If the patient isn’t generating an effective cough, check the pressure settings – they might be too low. If the patient reports discomfort, the pressure might be too high or the mask seal inadequate. Adjust settings accordingly, ensuring the patient’s comfort is prioritized. Always re-assess the patient’s needs and adjust the settings based on their tolerance.
If the device malfunctions, check the power supply, tubing connections, and the overall integrity of the equipment. Refer to the manufacturer’s troubleshooting guide for specific error codes and solutions. If the problem persists, contact technical support or replace the device as needed. It’s critical to document all troubleshooting steps taken and the final resolution, as well as any adverse events.
For example, if a patient is experiencing discomfort during the expiratory phase, we would reduce the expiratory pressure or duration, ensuring patient comfort always comes first. If the device displays an ‘air leak’ message, we would systematically check all the connections and the seal of the mask to resolve the issue. A systematic approach ensures rapid identification and resolution of any issues.
Q 10. How do you educate patients and families about Cough Assist therapy?
Educating patients and families about Cough Assist therapy is paramount for successful treatment. Start by explaining the purpose of the therapy – to help clear secretions from the lungs and improve breathing. Use clear, simple language, avoiding technical jargon. Show them how the device works, demonstrating the process step-by-step.
Explain the importance of proper positioning and mask fitting for optimal effectiveness. Clearly detail the expected sensations, such as pressure changes during inspiration and expiration, to minimize anxiety. Teach them how to recognize potential problems, such as insufficient coughing or discomfort, and what steps to take (adjusting pressure, checking connections). Provide them with written instructions, and encourage them to ask questions. Emphasize the importance of regular follow-up appointments and open communication with the healthcare team.
Consider using visual aids like diagrams or videos to illustrate the therapy. Involve family members in the education process to ensure they can assist the patient at home. Regular reinforcement of the instructions through repeated sessions is beneficial to improve compliance and better manage the condition.
Q 11. Explain the importance of airway clearance techniques in conjunction with Cough Assist.
Airway clearance techniques, such as postural drainage, percussion, and vibration, are often used in conjunction with Cough Assist to maximize its effectiveness. These techniques help loosen and mobilize secretions in the lungs, making them easier to expel during the Cough Assist cycle. They are complementary, not mutually exclusive. Think of it this way: airway clearance techniques help prepare the lungs for the Cough Assist, while the Cough Assist provides the mechanical force needed to remove the mobilized secretions.
For example, postural drainage positions the patient to allow gravity to help drain secretions from specific lung segments. Then, percussion and vibration techniques, applied by a trained professional, help loosen these secretions, making them more easily removed by the subsequent use of the Cough Assist. The combination of these methods is far more effective than using any one technique alone. The strategy is tailored to the individual needs and condition of each patient.
Q 12. How do you manage secretions effectively during and after Cough Assist treatment?
Effective secretion management during and after Cough Assist involves several strategies. During treatment, observe the patient for signs of effective secretion clearance, such as productive coughs and changes in breath sounds. After the treatment, encourage the patient to cough productively to remove any remaining secretions. Suctioning may be necessary if the patient is unable to clear secretions effectively on their own. Proper hygiene is paramount to prevent further respiratory complications.
Ensure that suction equipment is readily available and properly functioning. Techniques should be carefully explained and demonstrated. The use of humidification can help to thin the secretions, making them easier to remove. Regular monitoring of vital signs and respiratory status is crucial to detect any signs of respiratory distress or infection.
For instance, if a patient struggles to clear their secretions after Cough Assist, we might employ manual assisted coughing techniques or use a suction catheter to clear any remaining secretions safely and effectively. Documentation of the volume and nature of the secretions is essential for monitoring the effectiveness of the treatment.
Q 13. What are the appropriate hygiene protocols for Cough Assist devices?
Maintaining proper hygiene for Cough Assist devices is essential to prevent cross-contamination and infection. After each use, the device should be cleaned and disinfected according to the manufacturer’s instructions. This typically involves cleaning the tubing and mask with a suitable disinfectant, ensuring proper drying afterwards. Reusable components should be appropriately sterilized.
The device should be stored in a clean, dry place when not in use. Regular inspection for any damage or wear and tear is critical, and components should be replaced as needed. Regular maintenance and cleaning logs should be kept for traceability and quality control purposes.
For instance, we might use a specific hospital-grade disinfectant solution to clean the tubing and mask after each use, following manufacturer guidelines meticulously. We would also ensure that the device is stored in a designated, clean area to maintain its sterility and avoid accidental contamination.
Q 14. Describe the differences between positive expiratory pressure (PEP) therapy and Cough Assist.
While both positive expiratory pressure (PEP) therapy and Cough Assist aim to improve airway clearance, they differ significantly in their mechanism of action. PEP therapy involves the patient exhaling against a set resistance, creating positive pressure in the airways that helps mobilize secretions. The patient actively participates in the process. It is typically used for milder conditions.
Cough Assist, on the other hand, uses a mechanical device to deliver positive pressure during inspiration and controlled negative pressure during expiration, actively assisting the patient to cough. It is often used for patients with more severe respiratory conditions or impaired coughing ability. Think of PEP as a gentle encouragement to clear your lungs, while Cough Assist provides a more powerful, assisted cough.
In essence, PEP therapy relies on the patient’s own respiratory effort, while Cough Assist provides external assistance to generate a more effective cough. The choice of therapy depends on the patient’s individual needs and respiratory status. The decision should be based on a thorough respiratory assessment and patient’s ability to engage with each form of therapy.
Q 15. How do you document the Cough Assist therapy session?
Documenting a Cough Assist therapy session is crucial for tracking patient progress and ensuring effective treatment. A comprehensive record should include the date, time, and duration of the session. We meticulously document the patient’s baseline status, including their respiratory rate, oxygen saturation (SpO2), heart rate, and any observable signs of respiratory distress before, during, and after the therapy.
We then record the specific Cough Assist device settings used, such as the inspiratory pressure, expiratory pressure, cycle time, and the number of cycles delivered. Any adverse events, such as coughing fits, discomfort, or changes in vital signs, are carefully noted. Finally, we assess the effectiveness of the session by documenting the amount of secretions cleared and the patient’s subjective response to the therapy, noting any improvements in their breathing or comfort level. This information is often recorded on a standardized form, which helps to maintain consistency across treatments and allows for efficient data analysis.
For example, a typical entry might read: ’10/26/2024, 10:00 AM – Cough Assist session; Inspiratory pressure: 25 cm H2O, Expiratory pressure: 15 cm H2O, Cycle time: 2 seconds, Cycles: 10; Secretions cleared: significant; Patient reported improved breathing and less shortness of breath. Vital signs stable throughout.’ This detailed approach helps healthcare providers monitor patient response and make adjustments to the therapy plan as needed.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you adapt Cough Assist therapy for patients with specific conditions (e.g., tracheostomy, neuromuscular disease)?
Adapting Cough Assist therapy for patients with specific conditions requires a nuanced understanding of their physiology and potential limitations. For patients with a tracheostomy, the connection between the Cough Assist device and the airway is different. We use a tracheostomy cuff to ensure a proper seal, often adjusting pressure parameters to account for the altered airway dynamics and prevent accidental dislodgement of the tracheostomy tube. Regular monitoring is essential to prevent any complications.
Patients with neuromuscular diseases, like muscular dystrophy, often have weakened respiratory muscles. In these cases, we typically start with lower pressure and cycle settings to avoid over-exertion or discomfort. We gradually increase the settings as tolerated, closely observing the patient’s response and carefully monitoring their respiratory effort. We might also incorporate other interventions, such as assisted coughing techniques or postural drainage, to enhance the effectiveness of the therapy.
Think of it like adjusting the intensity of a workout – you wouldn’t start a marathon runner with the same intensity as a beginner. Similarly, the Cough Assist settings need careful titration based on the patient’s individual condition and capabilities.
Q 17. What are the safety precautions to be taken while using a Cough Assist device?
Safety is paramount when using a Cough Assist device. Before each session, we meticulously inspect the device for any damage or malfunction, paying close attention to the tubing, connections, and pressure gauges. We carefully check the patient’s airway for proper positioning and secure connections. A crucial step is explaining the procedure to the patient, addressing any anxieties or questions, and ensuring their cooperation throughout the session.
Monitoring the patient’s vital signs – heart rate, respiratory rate, and oxygen saturation – before, during, and after each session is critical. We remain vigilant for any signs of discomfort, respiratory distress, or adverse events, such as cyanosis (bluish discoloration of the skin) or decreased oxygen saturation. Emergency equipment, including oxygen and suction, should always be readily available. Training for all personnel involved in administering Cough Assist is vital for safe and effective application. Regular maintenance of the device is also non-negotiable to prevent malfunctions.
Q 18. How do you select appropriate pressure and cycle settings for different patients?
Selecting the appropriate pressure and cycle settings for Cough Assist is a personalized process, guided by the patient’s specific needs and respiratory status. We start with lower settings, gradually increasing them based on the patient’s tolerance and response. Factors considered include the patient’s age, underlying condition, respiratory muscle strength, and the viscosity of their secretions. Higher inspiratory pressures assist in creating a larger inspiratory volume, while higher expiratory pressures help to forcefully expel secretions. The cycle time determines the duration of inspiration and expiration.
For example, a patient with weak respiratory muscles might start with an inspiratory pressure of 15 cm H2O and an expiratory pressure of 10 cm H2O, with a cycle time of 2 seconds. A patient with thicker secretions might need higher pressures and a longer cycle time. Constant monitoring and adjustments are key to optimizing the therapy. This is done through a trial-and-error approach, coupled with careful observation of the patient’s response. We document these adjustments in the patient’s record to ensure consistency and facilitate ongoing monitoring.
Q 19. How do you address patient discomfort or anxiety during Cough Assist therapy?
Addressing patient discomfort or anxiety during Cough Assist therapy is crucial for a positive experience and effective treatment. We begin by thoroughly explaining the procedure, emphasizing the benefits and minimizing the perceived invasiveness. We use clear and simple language, reassuring the patient that they will be closely monitored and that the therapy is designed to improve their breathing and comfort. We encourage open communication, allowing the patient to express any concerns or discomfort they may be experiencing.
Some patients may experience discomfort from the pressure changes during the therapy. In these instances, we may adjust the settings to find a balance between effective secretion clearance and patient comfort. We can also use pain management strategies, such as relaxation techniques or analgesics, as clinically indicated. A supportive and empathetic approach, providing encouragement and positive reinforcement, significantly reduces patient anxiety and helps create a positive therapeutic experience. Creating a sense of control, such as letting them know they can stop the treatment at any time if needed, is key.
Q 20. What are the key performance indicators (KPIs) for successful Cough Assist therapy?
Key Performance Indicators (KPIs) for successful Cough Assist therapy focus on both objective and subjective measures. Objective KPIs include improvements in vital signs (e.g., increased SpO2, decreased respiratory rate), the volume and viscosity of secretions cleared, and a reduction in the frequency of respiratory infections. We closely monitor these parameters throughout the treatment course. For instance, if a patient consistently shows improved oxygen saturation levels after each session, it indicates effective clearance of airway secretions and improved gas exchange.
Subjective KPIs involve assessing the patient’s reported symptoms, such as improved breathing, reduced coughing, and decreased shortness of breath. We also evaluate the patient’s overall comfort level and ability to participate in daily activities. For example, an anecdotal improvement in a patient’s ability to eat without frequent coughing episodes demonstrates therapy success. Regular assessment of these KPIs allows us to track treatment efficacy, optimize the therapy plan, and identify any adjustments that need to be made to maximize therapeutic benefit and patient comfort. We often chart these KPIs visually to easily track trends and highlight areas of concern or improvement.
Q 21. Compare and contrast different brands of Cough Assist devices.
Several brands offer Cough Assist devices, each with unique features and capabilities. While the core function remains the same—assisting with airway clearance—differences exist in design, user interface, pressure settings, and overall ease of use. Some devices offer more advanced features like adjustable cycle times, variable pressure profiles, and data logging capabilities. Others prioritize simplicity and ease of use, particularly suited for home settings.
For example, one brand might excel in its intuitive interface and user-friendly controls, while another may provide more precise pressure control and a wider range of settings for patients with complex needs. Considerations like device size, portability, and maintenance requirements also vary significantly across brands. Choosing the right device for a particular patient depends on their individual needs, their clinical status, and the resources available. A thorough assessment of the patient’s needs and a review of the available devices are crucial steps in selecting the optimal device for therapy.
Q 22. Discuss the role of Cough Assist in managing different respiratory diseases.
Cough Assist, a form of airway clearance therapy, plays a vital role in managing various respiratory diseases by assisting patients in clearing secretions from their airways. It’s particularly beneficial for individuals who lack the ability to produce an effective cough due to weakness, paralysis, or other medical conditions.
- Cystic Fibrosis (CF): Cough Assist helps patients with CF, who often have thick, sticky mucus, to remove this mucus, preventing lung infections and improving lung function. Imagine it as a powerful, controlled ‘virtual cough’ that can clear airways more effectively than a weak natural cough.
- Post-operative patients: Following surgeries, particularly those involving the chest or abdomen, patients may experience reduced cough effectiveness. Cough Assist can help prevent atelectasis (lung collapse) and pneumonia by ensuring adequate airway clearance.
- Neuromuscular diseases: Patients with conditions like muscular dystrophy or amyotrophic lateral sclerosis (ALS) often have weak respiratory muscles. Cough Assist provides the necessary force to clear secretions, preventing respiratory complications.
- Traumatic brain injury (TBI): Individuals with TBI may experience impaired cough reflexes. Cough Assist can help restore airway clearance and reduce the risk of aspiration pneumonia.
The specific settings and frequency of Cough Assist therapy are tailored to the individual patient’s needs and the severity of their respiratory condition, always under the supervision of a respiratory therapist or physician.
Q 23. Explain the importance of regular maintenance and calibration of Cough Assist devices.
Regular maintenance and calibration of Cough Assist devices are crucial for ensuring safe and effective therapy. Neglecting these steps can lead to inaccurate pressure settings, malfunctioning equipment, and potentially harm the patient.
- Regular cleaning: Following manufacturer’s instructions for cleaning and disinfecting the device is essential to prevent bacterial growth and cross-contamination. Think of it like regularly cleaning a toothbrush – hygiene is paramount.
- Pressure checks: Regularly verifying the accuracy of the pressure gauge is crucial. Inaccurate pressure can compromise therapy effectiveness or cause patient discomfort or injury. Imagine trying to inflate a tire with an inaccurate pressure gauge – you might under-inflate or over-inflate, causing problems.
- Leak checks: Testing for leaks in the tubing and connections is vital to ensure that the delivered pressure is consistent and effective. Leaks can drastically reduce the effectiveness of the therapy.
- Calibration: Scheduled calibration by a qualified technician ensures the device is operating within its specified parameters. This is analogous to having your car’s engine regularly tuned for optimal performance.
Documentation of maintenance and calibration is also essential for maintaining a comprehensive patient record and adhering to best practices.
Q 24. How do you handle emergencies related to Cough Assist therapy (e.g., equipment malfunction, adverse patient reaction)?
Emergencies involving Cough Assist therapy require immediate action and a systematic approach.
- Equipment Malfunction: If the device malfunctions (e.g., power failure, pressure gauge error), immediately disconnect the patient from the device and assess their respiratory status. Have a backup device or alternative airway clearance method ready. Notify the physician and respiratory therapist immediately.
- Adverse Patient Reaction: If a patient experiences an adverse reaction (e.g., hypoxia, discomfort, bleeding), immediately stop the therapy. Assess vital signs, provide appropriate supportive care, and notify the medical team. Document the event thoroughly.
A well-rehearsed emergency plan is crucial. This plan should include clear steps for troubleshooting equipment issues, managing adverse events, and contacting relevant medical personnel. Regular drills and training help to ensure that staff are prepared to respond effectively to any situation.
Q 25. Describe your experience with different types of airway clearance techniques.
My experience encompasses various airway clearance techniques, including manual techniques and mechanical devices.
- Manual techniques: These include chest physiotherapy (CPT), which involves techniques like percussion, vibration, and postural drainage to loosen and mobilize secretions. I have extensive experience in instructing patients and caregivers in proper CPT techniques.
- Mechanical devices: Besides Cough Assist, I’m proficient with high-frequency chest wall oscillation (HFCWO) devices and positive expiratory pressure (PEP) masks. Each technique offers unique advantages depending on the patient’s specific needs and condition. I consider the patient’s tolerance, disease characteristics and individual needs to choose the best airway clearance technique.
Selecting the appropriate technique involves careful consideration of the patient’s clinical presentation, tolerance, and overall respiratory status. It’s often a collaborative decision involving the patient, physician, and respiratory therapist.
Q 26. What are the ethical considerations related to Cough Assist therapy?
Ethical considerations in Cough Assist therapy primarily revolve around patient autonomy, beneficence, and non-maleficence.
- Informed Consent: Patients must fully understand the benefits and risks of Cough Assist therapy before initiating treatment. This includes understanding the procedure, potential side effects, and alternative treatment options. The process must be clear and free from coercion.
- Resource Allocation: In settings with limited resources, ethical considerations arise in determining which patients receive priority access to Cough Assist therapy. Decisions should be based on clinical need and a fair allocation process.
- Patient Dignity and Privacy: Maintaining patient dignity and privacy during therapy is essential. The procedure should be performed in a respectful manner, with consideration for the patient’s comfort and modesty.
These ethical considerations are paramount and require ongoing reflection and adherence to professional guidelines to ensure the ethical provision of Cough Assist therapy.
Q 27. How do you determine the effectiveness of Cough Assist therapy?
Determining the effectiveness of Cough Assist therapy involves a multi-faceted approach that goes beyond simply observing whether the patient coughs.
- Clinical Assessment: Assessing the patient’s respiratory status before and after therapy is crucial. This includes monitoring vital signs, auscultating lung sounds to check for decreased wheezing or crackles, and observing for improved oxygen saturation levels.
- Secretion Production: Quantifying the amount and characteristics of expectorated secretions provides evidence of effective airway clearance. This can be done via sputum collection and analysis.
- Patient Reported Outcomes: Gathering information from the patient about their perceived improvement in breathing, cough effectiveness, and overall comfort is equally important. This involves using validated patient-reported outcome measures.
- Pulmonary Function Tests: In some cases, pulmonary function tests (PFTs) may be used to objectively measure changes in lung function before and after therapy.
A combination of these assessments paints a comprehensive picture of the effectiveness of the therapy and helps to guide adjustments in the treatment plan as needed.
Q 28. Explain the process of integrating Cough Assist into a comprehensive respiratory care plan.
Integrating Cough Assist into a comprehensive respiratory care plan requires a systematic approach that considers the patient’s overall condition and goals.
- Assessment: Begin with a thorough assessment of the patient’s respiratory status, including history, physical examination, and relevant diagnostic tests. This helps identify the need for airway clearance therapy and determines the optimal technique.
- Treatment Plan Development: Based on the assessment, develop a tailored treatment plan that specifies the frequency, duration, and settings of Cough Assist therapy. This plan should also include other respiratory interventions, such as medication, oxygen therapy, and mobility exercises.
- Patient and Family Education: Educate the patient and their family about the purpose, procedure, and potential benefits and risks of Cough Assist therapy. This empowers them to actively participate in their care.
- Monitoring and Evaluation: Closely monitor the patient’s response to the therapy and regularly evaluate the effectiveness of the treatment plan. Adjustments may be necessary based on the patient’s progress and any adverse effects.
Regular communication between the respiratory therapist, physician, and other members of the healthcare team is essential to ensure the effective implementation and ongoing optimization of the respiratory care plan.
Key Topics to Learn for Cough Assist Interview
- Mechanism of Action: Understand the principles behind how a Cough Assist device works, including the generation of positive and negative pressures and their effect on airway clearance.
- Patient Selection and Indications: Learn the criteria for selecting appropriate patients for Cough Assist therapy and the various medical conditions where it’s beneficial (e.g., neuromuscular diseases, post-surgical patients).
- Treatment Parameters and Settings: Become familiar with adjusting pressure, cycle time, and other parameters to optimize therapy for individual patient needs and monitor for adverse effects.
- Practical Application: Explore real-world scenarios, such as troubleshooting common issues (e.g., leaks, insufficient airway clearance), and adapting the treatment plan based on patient response.
- Safety and Monitoring: Understand the importance of patient monitoring during and after Cough Assist therapy, including recognizing and managing potential complications.
- Maintenance and Cleaning: Familiarize yourself with proper cleaning and maintenance procedures to ensure device functionality and hygiene.
- Ethical Considerations: Understand the ethical implications of using Cough Assist, including patient autonomy and informed consent.
- Integration with other therapies: How Cough Assist can be used in conjunction with other respiratory therapies or treatments.
Next Steps
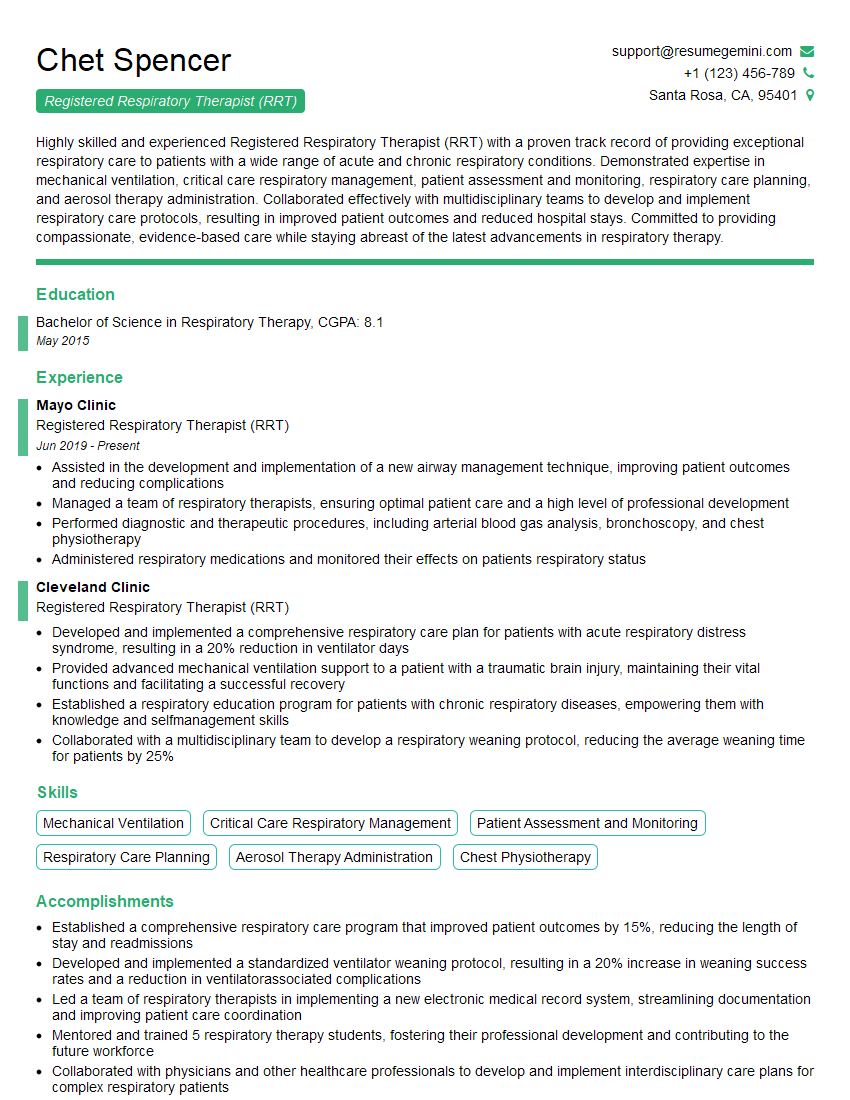
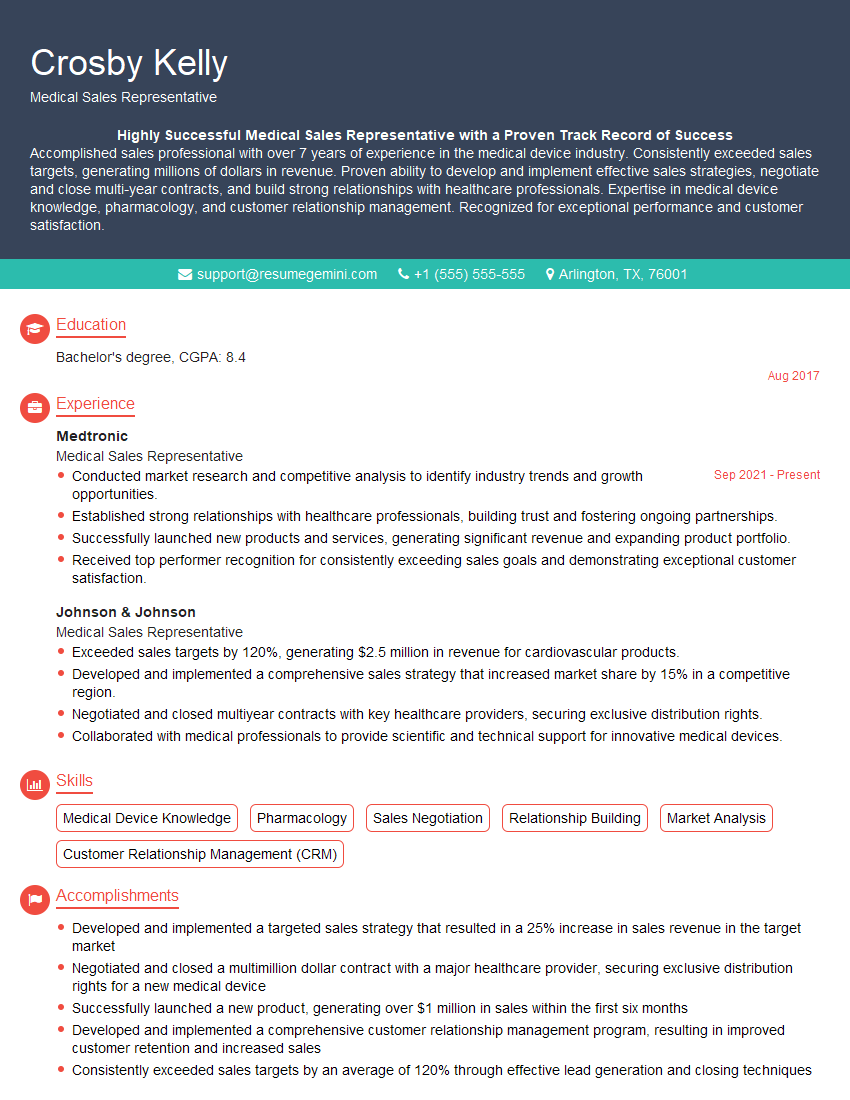
Mastering Cough Assist significantly enhances your value to healthcare teams, opening doors to specialized roles and career advancement in respiratory therapy and related fields. A well-crafted resume is crucial for showcasing your expertise and securing interviews. To increase your chances of getting noticed by Applicant Tracking Systems (ATS), focus on creating an ATS-friendly resume that highlights your relevant skills and experience. ResumeGemini is a trusted resource that can help you build a professional and impactful resume. Examples of resumes tailored to Cough Assist are available to guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.