Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Salmeterol Administration interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Salmeterol Administration Interview
Q 1. What are the indications for Salmeterol?
Salmeterol is a long-acting beta2-agonist (LABA) bronchodilator primarily indicated for the maintenance treatment of asthma and chronic obstructive pulmonary disease (COPD). It’s not for immediate relief of symptoms; instead, it works to prevent symptoms from occurring.
- Asthma: Salmeterol is used to prevent wheezing, shortness of breath, chest tightness, and coughing associated with asthma. It’s typically used in combination with inhaled corticosteroids for optimal asthma control.
- COPD: Salmeterol helps to improve lung function and reduce the frequency of exacerbations (worsening of symptoms) in patients with COPD. Again, it’s most effective when used as part of a comprehensive treatment plan.
Q 2. Describe the mechanism of action of Salmeterol.
Salmeterol works by binding to beta2-adrenergic receptors located in the smooth muscles of the airways. Activation of these receptors triggers a cascade of intracellular events that lead to relaxation of the airway smooth muscles, resulting in bronchodilation. Think of it like this: your airways are slightly narrowed; salmeterol acts like a key that unlocks the muscles, allowing them to relax and open the airways, making breathing easier. This effect is long-lasting, providing relief for up to 12 hours.
Importantly, Salmeterol’s long-acting nature means it’s not for immediate symptom relief. It’s for preventing symptoms from developing in the first place. A quick-relief inhaler (like albuterol) is needed for immediate symptom management.
Q 3. What are the common side effects of Salmeterol?
While generally well-tolerated, Salmeterol can cause some side effects, although they are usually mild and transient. The most common include:
- Tremor: A shaking sensation, often in the hands.
- Headache: Can range from mild to moderate.
- Muscle cramps or aches: Uncommon but possible.
- Increased heart rate (tachycardia): Less frequent but important to monitor, especially in patients with pre-existing heart conditions.
- Cough or throat irritation: Related to the inhalation process.
The severity of these side effects can vary from person to person. Always report any unusual or bothersome side effects to your healthcare provider.
Q 4. What is the correct dosage and frequency of Salmeterol?
Dosage and frequency of Salmeterol depend on the patient’s age, condition, and overall health. It’s crucial to follow the physician’s prescription exactly. Typical dosages involve inhaling two puffs twice a day, typically morning and evening, using a metered-dose inhaler (MDI) or a dry powder inhaler (DPI). However, there are variations, and some patients might require different doses or schedules.
Example: A common prescription might be 50 mcg twice daily. The specific dosage should always be determined and monitored by a healthcare professional.
Q 5. How is Salmeterol administered? Explain the steps.
Salmeterol is administered via inhalation using either a metered-dose inhaler (MDI) or a dry powder inhaler (DPI). The steps may vary slightly depending on the device, but the general principles remain the same:
- MDI: Check the inhaler for proper priming. Shake the inhaler well. Breathe out completely. Place the mouthpiece in your mouth and seal your lips around it. Press down on the canister while you slowly and deeply inhale. Hold your breath for 10 seconds and then slowly exhale. Wait about one minute before taking the second puff (if prescribed).
- DPI: Follow the manufacturer’s instructions, which may involve piercing a foil blister or loading a capsule. Inhale deeply and forcefully through the inhaler mouthpiece.
Proper technique is vital for effective delivery of the medication to the lungs. A healthcare professional should demonstrate the correct technique, and it’s advisable to practice until comfortable.
Q 6. What are the contraindications for Salmeterol?
Salmeterol is contraindicated in patients with known hypersensitivity or allergy to Salmeterol or any of its components. It is generally advised to avoid using Salmeterol in patients with certain conditions, which must be individually evaluated by a physician.
Q 7. What are the drug interactions of Salmeterol?
While numerous medications can be used concomitantly with Salmeterol, there are specific interactions that warrant caution. For example, beta-blockers can antagonize the effects of Salmeterol. Therefore, the use of beta-blockers (except for ophthalmic or cardioselective beta-blockers under specific circumstances) should be carefully evaluated by the physician when considering using Salmeterol. The use of other medications, especially those that can influence the cardiovascular system, should also be thoroughly reviewed with a healthcare professional before initiation of Salmeterol therapy.
Important Note: This information is not exhaustive. Always consult a healthcare professional or pharmacist for a comprehensive list of drug interactions and any potential implications for your individual health situation.
Q 8. How do you monitor a patient receiving Salmeterol?
Monitoring a patient on Salmeterol involves a multifaceted approach focusing on both efficacy and safety. We primarily assess the control of their underlying respiratory condition, usually asthma or COPD. This involves regularly checking their peak expiratory flow (PEF) readings, which measure the patient’s ability to forcefully exhale air. A consistent improvement or maintenance of their PEF within their personal best range indicates effective treatment. We also monitor for any worsening of symptoms, such as increased shortness of breath, wheezing, or coughing, which could signal a need for adjustment to their treatment plan. Regular assessment of lung function through spirometry (a more objective measure of lung capacity) is also valuable, especially during periods of exacerbation or if the PEF monitoring suggests a lack of control. Finally, we need to actively monitor for potential side effects, such as tremor, palpitations, or paradoxical bronchospasm (worsening of breathing difficulties). Any adverse reactions necessitate immediate evaluation and may require dose adjustment or switching to an alternative medication.
Q 9. What patient education is crucial for Salmeterol use?
Patient education is paramount for successful Salmeterol therapy. Patients need to understand that Salmeterol is a long-acting beta-agonist (LABA), meaning it provides long-term bronchodilation but is not a rescue medication for acute symptoms. We emphasize that it should be taken regularly as prescribed, even when feeling well, to prevent exacerbations. We explain the importance of using a spacer device with the MDI (Metered Dose Inhaler) to improve drug delivery to the lungs. Furthermore, they should be aware of the proper inhaler technique (which will be detailed separately). It’s crucial to educate them about recognizing and reporting any side effects such as tremors, nervousness, or increased heart rate. Importantly, we must inform them that Salmeterol is not a substitute for quick-relief medications like albuterol (short-acting beta-agonist, or SABA), which are essential for immediate relief of sudden breathing difficulties. We also explain the importance of adherence to their overall asthma or COPD management plan, including using other prescribed medications like inhaled corticosteroids or other therapies.
Q 10. How do you differentiate between Salmeterol and other bronchodilators?
Salmeterol distinguishes itself from other bronchodilators primarily through its long duration of action. Unlike short-acting beta-agonists (SABAs) like albuterol, which provide rapid but short-lived relief (typically 4-6 hours), Salmeterol’s effects can last for up to 12 hours. This makes it suitable for prophylaxis (prevention) of bronchospasm rather than the acute treatment of an attack. Other classes of bronchodilators, such as anticholinergics (e.g., ipratropium), also have different mechanisms of action and durations of effect. Anticholinergics block a different receptor in the airways than beta-agonists, and their duration varies depending on the specific drug. The choice of bronchodilator depends on the patient’s specific needs and the severity of their respiratory condition. For instance, patients with severe asthma or COPD might benefit from a combination of a LABA like Salmeterol and an inhaled corticosteroid (ICS) to reduce inflammation and prevent exacerbations.
Q 11. Explain the difference between Salmeterol and Serevent.
There is no difference between Salmeterol and Serevent. Serevent is simply the brand name for Salmeterol. Both names refer to the same active pharmaceutical ingredient: salmeterol xinafoate. The only difference would be the pharmaceutical company that produces it and any inactive ingredients which may be used in formulating the medication.
Q 12. What are the potential long-term effects of Salmeterol use?
Long-term use of Salmeterol, while generally safe when used as prescribed, can carry some potential risks. One concern is the potential for increased risk of serious cardiovascular events, such as cardiac arrhythmias or heart attacks, particularly in susceptible individuals. Although these risks are relatively low, regular monitoring for cardiac symptoms is crucial. Another potential issue is the risk of paradoxical bronchospasm, where the medication inadvertently causes airway constriction. This is less common but important to watch out for. Finally, long-term use of LABAs without concurrent use of an ICS (inhaled corticosteroid) can increase the risk of severe exacerbations in some patients, especially those with a history of severe asthma. Therefore, the use of Salmeterol is usually best when combined with an appropriate anti-inflammatory medication like an ICS.
Q 13. Describe the appropriate technique for using a metered-dose inhaler (MDI) with Salmeterol.
The proper technique for using a Salmeterol MDI is crucial for maximizing its efficacy. First, check the inhaler and ensure you understand the number of puffs in one dose. Next, shake the inhaler well. Then, exhale completely. Hold the inhaler upright with the mouthpiece facing upwards. If using a spacer, attach it now. Place the mouthpiece between your lips, ensuring a tight seal. Begin inhaling slowly and deeply, then, press down on the canister to release a puff of medication while continuing to inhale deeply and slowly. Hold your breath for at least 10 seconds (counting slowly helps), then exhale slowly. If using more than one puff, wait approximately 30 seconds to a minute between puffs. Rinse your mouth thoroughly with water after each dose to reduce the risk of oral thrush (a fungal infection). If using a spacer, you can release the puff into it and then inhale normally and steadily from the spacer. It helps distribute the medicine to your lungs efficiently.
Q 14. What are the signs and symptoms of an adverse reaction to Salmeterol?
Adverse reactions to Salmeterol are relatively uncommon but can include several signs and symptoms. The most frequently reported side effects are related to the medication’s beta-agonist properties and might include: tremors (shaking), palpitations (rapid or irregular heartbeat), nervousness, headache, muscle cramps, and insomnia. More serious, though rare, adverse reactions can include paradoxical bronchospasm (worsening of wheezing and shortness of breath), which necessitates immediate discontinuation of the medication and alternative treatment. Any signs of allergic reaction, such as rash, hives, or swelling, should also be considered as potential adverse reactions. Patients should be instructed to report any such symptoms to their healthcare provider immediately. Careful monitoring of patients, particularly those with cardiovascular conditions, is crucial to detect and manage any potential adverse events.
Q 15. How would you handle a patient who experiences an adverse reaction to Salmeterol?
Managing an adverse reaction to Salmeterol requires immediate action. First, I’d assess the severity of the reaction. Symptoms can range from mild, like tremor or headache, to serious, such as paradoxical bronchospasm (worsening of breathing difficulties) or cardiac arrhythmias. For mild reactions, monitoring the patient’s vital signs and offering reassurance might suffice. However, for severe reactions, immediate medical attention is crucial. This involves administering appropriate countermeasures like oxygen therapy, bronchodilators (for paradoxical bronchospasm), and in severe cases, potentially epinephrine. The patient would need to be transferred to a hospital for further evaluation and management. Documentation of the event, including the symptoms, interventions, and the patient’s response, is essential. Furthermore, the reaction needs to be reported to the appropriate regulatory authorities, as per guidelines. For example, if a patient develops a paradoxical bronchospasm, my immediate response would involve discontinuing Salmeterol, administering a rapid-acting beta-agonist like albuterol via nebulizer or MDI, and providing supplemental oxygen. Continuous monitoring of vital signs and respiratory status would be critical until the symptoms subside.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you store Salmeterol?
Proper storage of Salmeterol is key to maintaining its efficacy and preventing degradation. Salmeterol inhalers, whether metered-dose inhalers (MDIs) or dry powder inhalers (DPIs), should be stored at room temperature, away from direct sunlight and excessive heat or moisture. This typically means keeping them in a cool, dry place, away from sources of heat or humidity. Avoid extreme temperatures – both hot and cold can affect the medication’s potency. The specific storage instructions are usually printed on the product label; always refer to these instructions. Expired inhalers should be disposed of appropriately according to local guidelines, usually in a designated sharps container.
Q 17. What is the role of Salmeterol in asthma management?
Salmeterol plays a crucial role in asthma management as a long-acting beta2-agonist (LABA). Unlike short-acting beta-agonists (SABAs) used for quick relief of symptoms, Salmeterol provides long-term bronchodilation, preventing bronchoconstriction (narrowing of airways). It’s typically used in combination with an inhaled corticosteroid (ICS) as part of a maintenance strategy. This combination approach effectively controls inflammation (ICS) and prevents airflow obstruction (LABA), minimizing asthma exacerbations. Think of it as a preventative measure; Salmeterol helps keep the airways open and prevents attacks, rather than stopping one that’s already happening. It’s important to emphasize that Salmeterol is not a rescue medication and should not be used for immediate relief of asthma symptoms; that’s the role of a SABA like albuterol.
Q 18. What is the role of Salmeterol in COPD management?
In COPD management, Salmeterol serves a similar role to its use in asthma; it’s a LABA that provides long-term bronchodilation. It helps to improve airflow and reduce symptoms like breathlessness and wheezing. However, the use of Salmeterol in COPD is often approached differently. In COPD, the main goal is to improve lung function and quality of life. Salmeterol is often used in combination with other treatments, such as long-acting muscarinic antagonists (LAMAs), and sometimes inhaled corticosteroids, depending on the severity of the disease and the patient’s response to therapy. While Salmeterol can help alleviate symptoms, it’s crucial to remember it addresses only one aspect of COPD – the bronchoconstriction, not the underlying inflammatory process.
Q 19. Describe the differences in administration between Salmeterol and Formoterol.
Both Salmeterol and Formoterol are LABAs, but they differ slightly in their onset and duration of action. Salmeterol’s onset of action is slower, typically taking 15-30 minutes to reach its peak effect, and its bronchodilation lasts for approximately 12 hours. Formoterol, on the other hand, has a faster onset of action (within 1-5 minutes) and a slightly shorter duration (8-12 hours). Administratively, both are available as MDIs and DPIs. The administration technique is largely the same: proper inhalation technique is critical to ensure the medication reaches the lungs effectively. Patients need to be carefully educated on the correct use of their inhalers, regardless of whether they use Salmeterol or Formoterol.
Q 20. What are the specific considerations for administering Salmeterol to pediatric patients?
Administering Salmeterol to pediatric patients requires special considerations, primarily focusing on proper dosage and inhaler technique. The dose is carefully adjusted based on the child’s age and weight. It’s crucial to use age-appropriate inhaler devices like spacers or holding chambers with MDIs to improve drug delivery and reduce the risk of adverse effects. Parents or caregivers must be educated on the correct usage of the device and proper administration techniques. Close monitoring of the child’s response to the medication is vital, with regular assessments of lung function and symptom control. Always follow the pediatric prescribing guidelines and recommendations, ensuring the dose is appropriate for the individual child’s needs.
Q 21. What are the specific considerations for administering Salmeterol to geriatric patients?
Geriatric patients often experience age-related physiological changes that can affect Salmeterol’s efficacy and safety profile. They might have increased sensitivity to its side effects, such as tremors or palpitations. A thorough assessment of the patient’s overall health status, including other medications they’re taking, is essential before prescribing Salmeterol. Careful monitoring for adverse reactions, especially cardiac effects, is necessary. Dosage adjustments might be required based on the patient’s renal and hepatic function, as these organs play a role in drug metabolism and excretion. Additionally, consider the patient’s dexterity and cognitive abilities when choosing an inhaler device. If they struggle with inhaler technique, a spacer or alternative delivery system may be more appropriate. Clear and simple instructions, ideally in written and verbal formats, are crucial for medication adherence.
Q 22. How do you assess patient understanding of Salmeterol usage?
Assessing a patient’s understanding of Salmeterol involves a multi-faceted approach that goes beyond simply asking if they understand. It requires active listening and confirmation of their knowledge through demonstration and questioning.
- Teach-back method: After explaining how to use their inhaler, I’d ask the patient to explain back to me in their own words how and when to use it. This helps identify any gaps in their understanding. For example, I might ask, “Can you show me how you’d use this inhaler, and explain when you should take it each day?”
- Open-ended questions: Instead of yes/no questions, I use open-ended questions like, “What are your biggest concerns about using this medication?” or “What challenges do you anticipate facing while using Salmeterol?” This allows for a more in-depth understanding of their knowledge and potential barriers.
- Demonstration and observation: I always demonstrate the correct technique for using the inhaler, including proper inhalation and holding the breath. Then, I observe the patient attempting the technique to identify any errors and provide necessary corrections.
- Written instructions and resources: I provide patients with clear, written instructions tailored to their literacy level and additional resources such as videos or pamphlets for reinforcement. This helps ensure they retain the information.
By combining these methods, I can gain a comprehensive understanding of the patient’s knowledge and address any misconceptions or uncertainties they may have.
Q 23. What are the potential consequences of incorrect Salmeterol administration?
Incorrect Salmeterol administration can lead to several serious consequences, impacting both the effectiveness of treatment and the patient’s well-being. The most significant risks include:
- Ineffective treatment: Improper technique can significantly reduce the amount of medication reaching the lungs, leading to poor asthma control and increased risk of exacerbations.
- Increased side effects: Incorrect use, such as rapid inhalation or insufficient breath-holding, might increase the likelihood of experiencing side effects like tremor, palpitations, or headaches.
- Medication wastage: Incorrect use can lead to a loss of medication, making the treatment less cost-effective and potentially impacting the patient’s compliance.
- Severe respiratory events: In cases of severe asthma or COPD, improper use of Salmeterol can potentially worsen respiratory symptoms and lead to life-threatening complications requiring emergency medical attention.
It’s crucial to emphasize the importance of proper technique to patients to minimize these risks. Regular follow-up and assessment of patient technique are vital to ensure optimal treatment outcomes.
Q 24. How do you verify the correct patient identification before administering Salmeterol?
Verifying patient identity before administering Salmeterol is a critical step to prevent medication errors. I follow a strict protocol, usually involving three checks:
- Check 1: I check the patient’s identification band against the medication chart before retrieving the medication.
- Check 2: I verify the patient’s name and date of birth on the medication label against the patient’s identification band before preparing the medication.
- Check 3: Before administering the medication, I confirm the patient’s identity again by verbally asking them their name and date of birth, comparing it to the information on the medication label and their identification band.
In some settings, barcode scanning is also used to minimize human error and improve accuracy. This multi-step verification process is crucial for patient safety and reduces the likelihood of medication errors, particularly those with potentially severe consequences.
Q 25. Discuss the importance of proper documentation of Salmeterol administration.
Proper documentation of Salmeterol administration is essential for several reasons. It ensures accurate tracking of medication usage, aids in monitoring treatment effectiveness, supports continuity of care, and establishes a legal record.
- Accuracy of medication administration: Documentation provides a verifiable record of when, how, and by whom the medication was administered. It includes details such as the dose, route of administration (inhalation), and any observed patient reactions.
- Monitoring treatment effectiveness: The documentation helps monitor the effectiveness of Salmeterol in managing the patient’s condition and allows for timely adjustments to the treatment plan if needed.
- Continuity of care: Accurate documentation ensures seamless transitions in care between different healthcare professionals, improving the consistency and quality of patient care.
- Legal and regulatory compliance: Thorough documentation protects both the healthcare provider and the patient, adhering to legal and regulatory requirements concerning medication administration and patient safety.
Incomplete or inaccurate documentation can lead to miscommunication, errors in treatment, and legal implications. Therefore, meticulous record-keeping is paramount.
Q 26. How would you respond to a question about Salmeterol from a concerned patient?
Responding to a concerned patient about Salmeterol requires empathy, patience, and a clear, concise explanation. I would begin by acknowledging their concerns and validating their feelings. For instance, I might say, “I understand you have some concerns about Salmeterol. Let’s discuss them together.”
Then, I would explain the medication’s purpose, mechanism of action (long-acting bronchodilator), and expected benefits in a clear, simple manner avoiding medical jargon. I’d address their specific concerns with factual information and demonstrate the correct inhaler technique again if necessary. Finally, I’d reassure them that regular monitoring will be done to assess the medication’s effectiveness and address any side effects that may arise.
For instance, if a patient is concerned about tremors, I would explain that this is a relatively common, but usually mild, side effect that often resolves with continued use or a dosage adjustment. I would also encourage them to report any significant side effects immediately.
Q 27. What resources would you consult if you had questions about Salmeterol administration?
If I have questions about Salmeterol administration, I would consult several reputable resources:
- Pharmaceutical reference books: These provide detailed information about the drug, including its indications, contraindications, dosage, and potential side effects.
- Clinical practice guidelines: Guidelines from organizations such as the Global Initiative for Asthma (GINA) or the National Asthma Education and Prevention Program (NAEPP) offer evidence-based recommendations for the management of asthma and COPD, including the use of Salmeterol.
- Electronic drug databases: Databases like Micromedex or Lexi-Comp provide up-to-date information on medications, including potential drug interactions.
- Medical colleagues and specialists: I would consult with colleagues, especially pulmonologists, for clarification on specific cases or complex situations.
- Manufacturer’s prescribing information: The official prescribing information provided by the drug manufacturer contains detailed information about the medication and its usage.
By utilizing a combination of these resources, I can ensure I have the most current and accurate information available to provide optimal patient care.
Q 28. How would you address a patient’s concerns about the side effects of Salmeterol?
Addressing a patient’s concerns about Salmeterol’s side effects involves careful listening, accurate information, and a collaborative approach. I would start by acknowledging their concerns and asking specific questions about what side effects they’re experiencing or worried about.
I would then explain the common side effects (tremor, headache, palpitations) and their likelihood, emphasizing that many are mild and transient. I’d reassure the patient that these side effects are usually manageable and that we can work together to minimize any discomfort. If the side effects are severe or persistent, I would discuss strategies to manage them, such as dose adjustments, switching to an alternative medication, or contacting their physician.
For example, if a patient is experiencing tremors, we might try adjusting the dose or administering the medication at a different time of day. I’d also discuss the importance of reporting any concerning side effects immediately and reinforce the benefits of Salmeterol in controlling their respiratory condition, weighing the potential benefits against the risks.
Key Topics to Learn for Salmeterol Administration Interview
- Pharmacokinetics and Pharmacodynamics of Salmeterol: Understand the drug’s absorption, distribution, metabolism, and excretion. Explore its mechanism of action as a long-acting beta2-agonist.
- Indications and Contraindications: Master the appropriate uses of Salmeterol, specifically in chronic obstructive pulmonary disease (COPD) and asthma. Know the situations where it should be avoided.
- Dosage and Administration Techniques: Be proficient in different administration methods (e.g., inhaler use, proper technique to maximize efficacy and minimize side effects). Understand how dosage adjustments are made based on patient factors.
- Adverse Effects and Monitoring: Familiarize yourself with common and serious side effects. Know how to monitor patients for adverse reactions and manage them appropriately.
- Drug Interactions: Understand potential interactions with other medications frequently prescribed alongside Salmeterol. This includes both synergistic and antagonistic effects.
- Patient Education and Compliance: Be prepared to discuss the importance of patient education in successful Salmeterol therapy. Understand techniques to promote adherence to medication regimens.
- Troubleshooting Common Issues: Be ready to discuss problem-solving approaches to common challenges, such as inhaler technique difficulties, adverse effect management, and non-compliance.
Next Steps
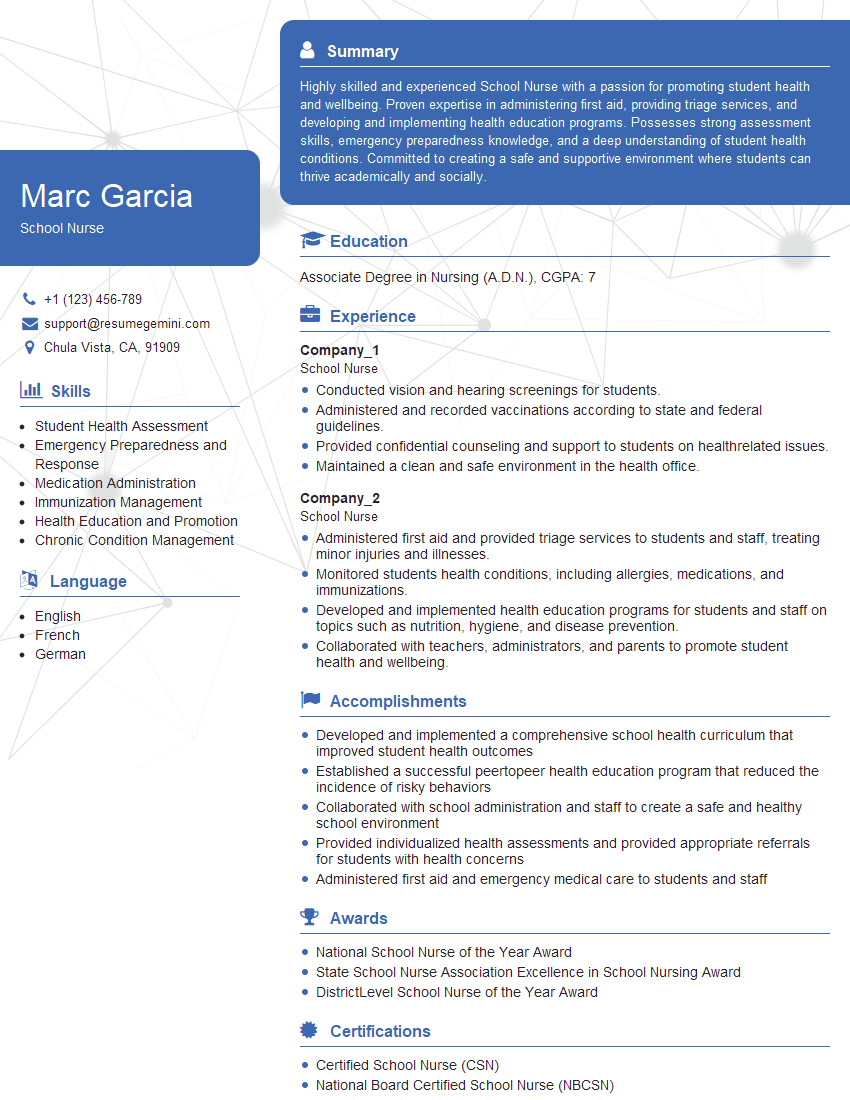
Mastering Salmeterol administration is crucial for career advancement in respiratory care and related fields. It demonstrates a strong foundation in pharmacology and patient care. To maximize your job prospects, focus on creating an ATS-friendly resume that highlights your skills and experience. ResumeGemini is a trusted resource for building professional resumes that stand out. We provide examples of resumes tailored to Salmeterol Administration to help you create a compelling application. Let ResumeGemini help you present yourself as the ideal candidate.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.