Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Respiratory Care Planning interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Respiratory Care Planning Interview
Q 1. Explain the process of developing an individualized respiratory care plan.
Developing an individualized respiratory care plan is a collaborative process that begins with a thorough assessment of the patient’s respiratory status and overall health. It’s like building a custom house – you need a solid foundation (assessment) before you can start constructing the walls (treatment plan).
- Assessment: This involves reviewing the patient’s medical history, conducting a physical examination (including auscultation, palpation, and inspection), and reviewing relevant diagnostic tests (e.g., arterial blood gas, chest X-ray, pulmonary function tests).
- Diagnosis: Based on the assessment, the respiratory therapist identifies the primary respiratory problem(s) and any contributing factors.
- Goal Setting: The plan outlines specific, measurable, achievable, relevant, and time-bound (SMART) goals. For example, a goal might be to improve oxygen saturation to 95% or reduce shortness of breath during activities of daily living.
- Intervention Selection: Appropriate respiratory interventions are chosen, such as oxygen therapy, bronchodilators, airway clearance techniques, or mechanical ventilation. The choice depends on the patient’s condition and the identified goals.
- Implementation and Monitoring: The plan is put into action, and the patient’s response to the interventions is closely monitored. Adjustments are made as needed to optimize treatment efficacy.
- Evaluation and Documentation: Regular evaluations assess the effectiveness of the plan and identify areas for improvement. All interventions and patient responses are meticulously documented.
For example, a patient with COPD might have goals focusing on improving their exercise tolerance, reducing dyspnea, and preventing exacerbations. Their plan might include pulmonary rehabilitation, inhaled bronchodilators, and education on self-management techniques.
Q 2. Describe the key components of a comprehensive respiratory assessment.
A comprehensive respiratory assessment is crucial for effective respiratory care planning. It’s like a detective investigating a crime scene – you need to gather all the clues to understand the situation.
- History: This includes the patient’s medical history (e.g., smoking history, allergies, previous respiratory illnesses), current symptoms (e.g., cough, dyspnea, chest pain), and medications.
- Physical Examination: This involves observing the patient’s respiratory rate, rhythm, and effort; assessing their level of consciousness; listening to their breath sounds for wheezes, crackles, or rhonchi; and palpating the chest for tenderness or abnormal movement.
- Arterial Blood Gases (ABGs): ABGs provide valuable information about the patient’s blood oxygen and carbon dioxide levels, pH, and bicarbonate levels, reflecting the efficiency of gas exchange.
- Pulse Oximetry: This non-invasive method measures the oxygen saturation (SpO2) in the blood, providing a continuous assessment of oxygenation.
- Chest X-ray: This imaging technique helps visualize the lungs and identify abnormalities such as pneumonia, atelectasis, or pneumothorax.
- Pulmonary Function Tests (PFTs): These tests measure lung volumes and flows, providing objective data on the severity of lung disease.
Imagine a patient presenting with shortness of breath. A comprehensive assessment would involve considering their medical history (e.g., asthma), listening for wheezing, checking their oxygen saturation, and potentially ordering a chest X-ray to rule out pneumonia. The assessment findings then inform the appropriate respiratory care plan.
Q 3. How do you determine the appropriate mode of mechanical ventilation for a patient?
Selecting the appropriate mode of mechanical ventilation is a critical decision that requires careful consideration of the patient’s clinical status and underlying pathology. It’s like choosing the right tool for a specific job – a screwdriver won’t work for hammering a nail.
The choice depends on various factors, including:
- Respiratory Drive: Patients with intact respiratory drive may benefit from pressure support ventilation (PSV) or synchronized intermittent mandatory ventilation (SIMV). Conversely, patients with impaired respiratory drive may require controlled mandatory ventilation (CMV).
- Lung Mechanics: Patients with stiff lungs (e.g., ARDS) may require low tidal volume ventilation with high PEEP (positive end-expiratory pressure) to improve oxygenation and prevent lung injury. Patients with hyperinflation (e.g., COPD) may benefit from volume-limited ventilation to avoid overdistension.
- Patient-ventilator synchrony: The chosen mode should ensure optimal synchrony between the patient’s breathing efforts and the ventilator to promote comfort and reduce work of breathing.
- Gas exchange: The ventilator settings need to be adjusted to maintain adequate oxygenation and ventilation, as reflected by ABGs and clinical assessment.
For example, a patient with acute respiratory distress syndrome (ARDS) might require low tidal volume ventilation with high PEEP to protect their lungs, while a patient with COPD exacerbation might be managed with PSV to help reduce their work of breathing.
Q 4. What are the indications for non-invasive ventilation (NIV)?
Non-invasive ventilation (NIV) is a valuable tool for supporting ventilation without the need for endotracheal intubation. It’s like giving respiratory support through a gentler approach, avoiding the risks associated with invasive ventilation.
Indications for NIV include:
- Acute exacerbations of COPD: NIV can help reduce dyspnea and improve oxygenation in patients with acute COPD exacerbations, reducing the need for intubation.
- Cardiogenic pulmonary edema: NIV can help reduce pulmonary congestion and improve oxygenation in patients with heart failure-related pulmonary edema.
- Pneumonia: In selected cases, NIV can assist in managing severe pneumonia, especially in patients with respiratory muscle fatigue.
- Pre-operative support: NIV may be used before surgery in patients with high-risk respiratory conditions.
- Neuromuscular weakness: NIV can provide respiratory support for patients with conditions causing muscle weakness.
For instance, a patient with a severe COPD exacerbation exhibiting significant dyspnea and hypoxemia would be a prime candidate for NIV. It helps improve gas exchange and reduces the workload on the respiratory muscles, often preventing the need for intubation.
Q 5. Explain the weaning parameters you monitor when a patient is on mechanical ventilation.
Weaning from mechanical ventilation is a gradual process that requires careful monitoring of several parameters. It’s like slowly releasing a tight grip, ensuring stability before completely letting go.
Key weaning parameters include:
- Respiratory Rate: A stable and sustainable respiratory rate (typically below 30 breaths/minute) indicates readiness for weaning.
- Tidal Volume: Adequate tidal volume (typically > 5ml/kg ideal body weight) signifies sufficient lung capacity and ventilation.
- Minute Ventilation: This parameter, reflecting the total volume of air breathed per minute, should be within an acceptable range.
- Vital Capacity (VC) and Inspiratory Capacity (IC): These measures of lung volume provide insight into respiratory muscle strength and endurance.
- Rapid Shallow Breathing Index (RSBI): A low RSBI (typically <106 breaths/minute/L) suggests readiness for weaning, while higher values indicate respiratory muscle fatigue.
- Hemodynamics: Close monitoring of blood pressure and heart rate is vital as weaning may cause hemodynamic changes.
- Level of Consciousness and Mental Status: The patient should be alert and cooperative to facilitate participation in weaning.
For example, a patient with a stable respiratory rate, good tidal volume, and an RSBI below 106 would be considered a good candidate for a weaning trial. However, if their oxygen saturation drops or their respiratory rate significantly increases during the trial, weaning would be temporarily halted.
Q 6. How do you manage a patient experiencing respiratory distress?
Managing a patient experiencing respiratory distress requires immediate action and a systematic approach. It’s like responding to a fire – you need to act swiftly and methodically to contain the situation.
The immediate steps include:
- Assess the patient’s airway, breathing, and circulation (ABCs): This is the priority, ensuring a patent airway and adequate ventilation and circulation.
- Provide supplemental oxygen: High-flow oxygen via a non-rebreather mask or other appropriate devices is crucial to improve oxygenation.
- Position the patient: Positioning the patient to optimize ventilation, such as the upright position or high-fowler’s, can help reduce respiratory distress.
- Monitor vital signs: Continuously monitoring respiratory rate, heart rate, blood pressure, and oxygen saturation helps assess the patient’s response to interventions.
- Initiate advanced respiratory support: Depending on the severity of the distress, this might involve non-invasive ventilation (NIV), or invasive mechanical ventilation.
- Address the underlying cause: Treating the underlying condition causing respiratory distress is essential for long-term management.
For instance, a patient with acute asthma exacerbation exhibiting severe dyspnea and wheezing would require immediate oxygen therapy, bronchodilators (e.g., albuterol), and potentially NIV or intubation if there’s no improvement.
Q 7. Describe your experience with managing patients with COPD.
I have extensive experience managing patients with chronic obstructive pulmonary disease (COPD). It’s a complex condition requiring a multifaceted approach – it’s not a one-size-fits-all situation.
My experience encompasses:
- Assessment and Diagnosis: Performing comprehensive respiratory assessments, including spirometry and ABG analysis, to diagnose and stage COPD.
- Pharmacological Management: Prescribing and monitoring bronchodilators (e.g., albuterol, ipratropium), inhaled corticosteroids, and other medications to optimize lung function.
- Non-Pharmacological Management: Educating patients on effective pulmonary rehabilitation programs, including breathing exercises, and self-management techniques.
- Oxygen Therapy: Prescribing and monitoring long-term oxygen therapy (LTOT) for hypoxemic patients.
- Disease Management: Collaborating with the healthcare team to develop and implement comprehensive COPD management plans, focusing on preventing exacerbations and improving quality of life.
- Exacerbation Management: Managing acute COPD exacerbations, often involving supplemental oxygen, bronchodilators, and potentially NIV.
I recall one patient with severe COPD who was frequently hospitalized due to exacerbations. By implementing a comprehensive plan that included LTOT, pulmonary rehabilitation, regular medication reviews, and education on infection prevention, we were able to significantly reduce the frequency and severity of their exacerbations, improving their overall quality of life.
Q 8. How do you manage a patient with acute respiratory failure?
Managing acute respiratory failure requires a rapid and systematic approach focusing on immediate life support and identifying the underlying cause. Think of it like a fire: you need to extinguish the immediate flames (respiratory distress) while simultaneously investigating the source (underlying pathology).
Initial Steps: This involves securing the airway (intubation if necessary), providing supplemental oxygen, and initiating mechanical ventilation if the patient is unable to maintain adequate oxygenation and ventilation. We’ll monitor vital signs closely, paying special attention to oxygen saturation (SpO2), heart rate, blood pressure, and respiratory rate.
Diagnosis and Treatment: Once stabilized, we need to determine the root cause – is it pneumonia, pulmonary edema, COPD exacerbation, or something else? Blood gas analysis is crucial here. Based on the diagnosis, treatment will vary: antibiotics for infection, diuretics for fluid overload, bronchodilators for airway constriction, etc.
Example: I once managed a patient who presented with severe respiratory distress due to pneumonia. After securing the airway and initiating mechanical ventilation, we administered broad-spectrum antibiotics. Continuous monitoring and supportive care allowed for a gradual improvement and eventual extubation.
Ongoing Management: Continuous monitoring is paramount, including frequent arterial blood gas analysis and assessment of respiratory parameters. We adjust ventilator settings as needed based on the patient’s response, and we work closely with other specialists like pulmonologists and intensivists to optimize care.
Q 9. What are the signs and symptoms of a pneumothorax?
A pneumothorax, or collapsed lung, occurs when air leaks into the space between your lung and chest wall. Imagine a balloon (your lung) inside a box (your chest cavity). If air gets into the box, it compresses the balloon, preventing it from expanding fully.
Signs and Symptoms: These can range from mild to severe. Patients may experience sudden, sharp chest pain, especially on the affected side, often worsened by deep breaths or coughing. Shortness of breath (dyspnea) is a common symptom, and they may also have rapid heart rate (tachycardia), decreased breath sounds on the affected side, and cyanosis (bluish discoloration of skin).
Severe Cases: In more severe cases, a tension pneumothorax can occur, where air continues to build up in the pleural space, compressing the lung and great vessels. This is a life-threatening emergency, requiring immediate intervention. Symptoms are often more dramatic, with worsening shortness of breath, significant chest pain, and potential shock.
Q 10. How would you manage a patient with a suspected pulmonary embolism?
Suspected pulmonary embolism (PE) – a blood clot in the lung – is a serious condition requiring immediate attention. It’s like a traffic jam in the lung’s blood vessels, blocking blood flow and potentially causing serious complications.
Management: The primary goal is to rule out the possibility of a PE and initiate treatment if confirmed. This begins with a thorough assessment, including patient history, physical examination, and initial diagnostic tests like ECG and chest X-ray. A CT pulmonary angiogram (CTPA) is usually the gold standard diagnostic test for PE.
Treatment: If a PE is confirmed, the cornerstone of treatment is anticoagulation therapy (blood thinners) to prevent further clot formation and allow the existing clot to dissolve. This may involve heparin (immediate effect) followed by warfarin (longer-term). Oxygen therapy is crucial to address any hypoxia (low blood oxygen levels). Supportive care includes monitoring vital signs, managing pain, and addressing any other complications.
Example: I managed a patient with suspected PE presenting with sudden onset dyspnea and pleuritic chest pain. A CTPA confirmed the diagnosis, and we immediately started them on intravenous heparin and oxygen therapy. The patient responded well to treatment, and anticoagulation therapy was continued for several months.
Q 11. Explain the process of suctioning an endotracheal tube.
Suctioning an endotracheal tube is a crucial procedure to remove secretions from the airway and maintain a clear airway for the patient. Think of it as cleaning a drain to ensure proper flow.
Procedure:
- Prepare: Gather sterile supplies, including suction catheters (appropriate size), sterile gloves, and a suction device. Verify the suction pressure (typically 80-120 mmHg).
- Preoxygenate: Hyperoxygenate the patient with 100% oxygen for several minutes to prevent hypoxia during the procedure.
- Insertion: Gently insert the catheter into the endotracheal tube, avoiding excessive force. Use intermittent suction while withdrawing the catheter, rotating it gently to remove secretions.
- Monitor: Monitor the patient’s heart rate, oxygen saturation, and respiratory rate throughout the procedure.
- Post-Suctioning: Hyperoxygenate the patient again, assess breath sounds, and document the amount and character of secretions removed.
Important Considerations: Limit suction time to 10-15 seconds to prevent hypoxia and trauma to the airway. Proper technique and sterile procedure are essential to minimize the risk of infection.
Q 12. What are the potential complications of mechanical ventilation?
Mechanical ventilation, while life-saving, carries potential complications. It’s a powerful tool but needs careful handling.
Pulmonary Complications:
- Barotrauma: Damage to the lungs from high pressures during ventilation, leading to pneumothorax or pneumomediastinum.
- Volutrauma: Lung injury from excessive tidal volumes.
- Atelectasis: Collapse of alveoli due to inadequate ventilation.
- Infection: Ventilator-associated pneumonia (VAP) is a significant risk.
Other Complications:
- Cardiovascular: Decreased cardiac output, arrhythmias.
- Gastrointestinal: Stress ulcers, gastroparesis.
- Renal: Acute kidney injury.
- Neurological: Anxiety, delirium.
Prevention: Careful monitoring, appropriate ventilator settings, meticulous infection control, and supportive care are key to minimizing these risks.
Q 13. How do you assess the effectiveness of respiratory treatments?
Assessing the effectiveness of respiratory treatments involves a multi-faceted approach, combining objective data with subjective observations. It’s about seeing the bigger picture and not just focusing on isolated parameters.
Objective Measurements:
- Arterial blood gas analysis: Measures oxygen and carbon dioxide levels in the blood.
- Pulse oximetry: Monitors oxygen saturation (SpO2).
- Lung function tests: Assess lung volumes and airflow.
- Chest X-ray: Provides an image of the lungs.
Subjective Assessments:
- Respiratory rate and effort: Observe the patient’s breathing pattern.
- Breath sounds: Listen for wheezes, crackles, or diminished breath sounds.
- Patient’s symptoms: Assess the patient’s subjective experience of shortness of breath, chest pain, and cough.
Example: In a patient with asthma, we’d monitor their peak expiratory flow (PEF) and assess their subjective experience of dyspnea before and after bronchodilator treatment. An improvement in PEF and reduction in dyspnea would indicate treatment efficacy.
Q 14. Describe your experience with oxygen therapy.
Oxygen therapy is a cornerstone of respiratory care, providing supplemental oxygen to patients with hypoxemia (low blood oxygen levels). It’s like giving a thirsty plant water.
Experience: I have extensive experience administering oxygen therapy using various delivery methods, including nasal cannulas, simple face masks, non-rebreather masks, and high-flow oxygen systems. I’m adept at selecting the appropriate method based on the patient’s needs and the severity of their hypoxemia. I regularly monitor oxygen saturation (SpO2) and arterial blood gas levels to ensure adequate oxygenation and to titrate oxygen flow as needed.
Example: I recently managed a patient with acute exacerbation of COPD requiring high-flow oxygen therapy to maintain adequate oxygenation. Continuous monitoring of SpO2 and arterial blood gases allowed for precise titration of oxygen flow, optimizing oxygen delivery while avoiding potential complications like oxygen toxicity.
Safety and Monitoring: I always emphasize safety and meticulous monitoring during oxygen therapy, paying attention to potential complications like oxygen toxicity and the impact of oxygen on the patient’s overall clinical picture. Proper oxygen delivery system selection and precise flow rate adjustment are critical components of my approach.
Q 15. How do you calculate the FiO2 for a patient receiving oxygen therapy?
Calculating the FiO2 (fraction of inspired oxygen) for a patient on oxygen therapy depends on the delivery method. FiO2 represents the percentage of oxygen in the inspired gas mixture. For example, room air has an FiO2 of approximately 21%.
Methods and Calculations:
- Low-Flow Oxygen Delivery Systems (Nasal Cannula, Simple Mask): These systems deliver oxygen at a specific liter flow, but the FiO2 is variable and depends on the patient’s breathing pattern and the ambient air mixed with the delivered oxygen. Precise FiO2 calculation is difficult, requiring pulse oximetry monitoring and clinical judgment. A rough estimate can be made using tables or nomograms, but these are imprecise.
- High-Flow Oxygen Delivery Systems (Venturi Mask, High-Flow Nasal Cannula): These systems deliver a precise FiO2 regardless of the patient’s breathing pattern, as they provide a consistent mixture of oxygen and air. The FiO2 is determined by the specific setting on the device. For example, a Venturi mask set at 40% will deliver an FiO2 of approximately 40%.
- Mechanical Ventilation: On a ventilator, the FiO2 is directly set by the respiratory therapist or clinician and is precisely controlled. It’s displayed on the ventilator’s monitor.
Example: A patient is receiving 4L/min oxygen via nasal cannula. While we can’t precisely calculate the FiO2 without knowing their breathing pattern, we know it’s significantly greater than 21% (room air) but likely less than 40%. Pulse oximetry is crucial in this situation to guide adjustments.
In summary: Calculating FiO2 requires understanding the oxygen delivery method and utilizing tools like pulse oximetry for low-flow systems. High-flow and mechanical ventilation systems provide direct FiO2 readings.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the common types of airway clearance techniques?
Airway clearance techniques aim to remove mucus and secretions from the airways, improving lung function and reducing symptoms. They are essential in managing conditions like cystic fibrosis, chronic bronchitis, and post-operative respiratory complications.
Common Types:
- Huff Coughing: A controlled coughing technique involving short, forceful exhales to loosen secretions.
- Active Cycle of Breathing (ACB): A series of breathing exercises combining controlled breathing, thoracic expansion exercises, and huffs to mobilize secretions.
- Autogenic Drainage (AD): A technique that uses controlled breathing to move secretions from the peripheral airways to the central airways for expectoration.
- Positive Expiratory Pressure (PEP) Therapy: Uses a device to create back pressure during exhalation, helping to open airways and facilitate secretion clearance. This can involve PEP masks or flutter valves.
- Chest Physiotherapy (CPT): This includes manual techniques like percussion (clapping), vibration, and postural drainage to loosen and mobilize secretions. This is often performed by a respiratory therapist.
- High-Frequency Chest Wall Oscillation (HFCWO): Uses a vest that applies vibrations to the chest wall to loosen secretions. This method is often used for patients with significant mucus buildup.
The choice of technique depends on the patient’s individual needs, condition, and capabilities. A respiratory therapist will assess the patient and recommend the most appropriate method.
Q 17. Explain your experience with administering bronchodilators and other respiratory medications.
Administering respiratory medications requires precision and attention to detail to ensure patient safety and efficacy. My experience encompasses a wide range of bronchodilators and other respiratory medications, administered via various routes.
Bronchodilators: I’m proficient in administering beta-agonists (like albuterol) and anticholinergics (like ipratropium) via metered-dose inhalers (MDIs) with and without spacers, nebulizers, and small-volume nebulizers (SVN). I carefully monitor patients for adverse effects such as tachycardia or tremors, adjusting dosages as needed under physician orders. I educate patients on proper inhaler technique to maximize medication delivery and minimize side effects. I have experience with various delivery systems including pressurized metered dose inhalers (pMDIs), dry powder inhalers (DPIs), and nebulizers.
Other Respiratory Medications: I’m experienced in administering corticosteroids (like fluticasone), mucolytics (like N-acetylcysteine), and other medications via inhalation or intravenous routes. I meticulously document administration, patient response, and any observed side effects. I also educate patients about their medications, including proper storage and potential interactions with other medications.
Example: I recently managed a patient experiencing an acute asthma exacerbation. I administered albuterol via nebulizer, closely monitoring their respiratory rate, oxygen saturation, and lung sounds. Following stabilization, I initiated inhaled corticosteroids to reduce inflammation. Throughout, I documented the treatment and the patient’s response, ensuring seamless communication with the physician.
Q 18. Describe your understanding of pulmonary function testing.
Pulmonary function testing (PFT) is a group of tests that measure and evaluate lung function, providing valuable insights into respiratory health. It involves various non-invasive procedures that assess lung volumes, airflow, and gas exchange.
Common PFTs:
- Spirometry: Measures lung capacity and airflow, assessing how well the lungs can take in and expel air. Key parameters include forced vital capacity (FVC), forced expiratory volume in one second (FEV1), and FEV1/FVC ratio.
- Lung Volumes: Measures total lung capacity, vital capacity, residual volume, and other parameters to assess lung size and gas distribution.
- Diffusion Capacity (DLCO): Measures how well oxygen moves from the lungs into the bloodstream.
- Body Plethysmography: Provides more precise measurements of lung volumes, including residual volume, which is difficult to measure accurately with other methods.
Interpretation: PFT results are interpreted in the context of the patient’s age, gender, height, and medical history. They help diagnose and monitor respiratory conditions such as asthma, COPD, and cystic fibrosis. Abnormal results might indicate restrictive or obstructive lung diseases. For example, a low FEV1/FVC ratio might suggest obstructive lung disease.
Practical Application: I utilize PFT results to guide treatment decisions, monitor disease progression, and assess the effectiveness of interventions. For example, a patient with asthma may undergo PFT before and after receiving bronchodilator medication to evaluate its effect on their lung function.
Q 19. How do you interpret arterial blood gas results?
Interpreting arterial blood gas (ABG) results is critical for assessing a patient’s oxygenation, ventilation, and acid-base balance. ABG analysis provides crucial information about the effectiveness of respiratory support and helps guide treatment decisions.
Key Parameters:
- PaO2 (Partial Pressure of Oxygen): Reflects the amount of oxygen dissolved in arterial blood. Low values indicate hypoxemia (low blood oxygen).
- PaCO2 (Partial Pressure of Carbon Dioxide): Reflects the amount of carbon dioxide in arterial blood. High values indicate hypercapnia (high blood carbon dioxide), suggesting hypoventilation. Low values suggest hyperventilation.
- pH (Hydrogen Ion Concentration): Reflects the acidity or alkalinity of the blood. Normal pH is around 7.4. Acidosis (pH <7.35) indicates excess acid, while alkalosis (pH >7.45) indicates excess base.
- HCO3- (Bicarbonate): A major buffer in the blood. Changes in HCO3- often indicate metabolic compensation for respiratory disturbances.
- SaO2 (Oxygen Saturation): Represents the percentage of hemoglobin carrying oxygen. Usually measured by pulse oximetry.
Interpretation: I systematically analyze each parameter to determine the underlying cause of any abnormalities. For example, a low PaO2 with a normal PaCO2 suggests a problem with oxygenation, possibly due to pneumonia. A high PaCO2 with a low pH suggests respiratory acidosis, potentially due to hypoventilation. The interplay between these parameters helps distinguish between respiratory and metabolic disturbances.
Example: A patient presents with a PaO2 of 50 mmHg, PaCO2 of 60 mmHg, pH of 7.25, and HCO3- of 24 mEq/L. This indicates respiratory acidosis with hypoxemia, suggestive of severe respiratory failure requiring immediate intervention, like mechanical ventilation.
Q 20. What are the key considerations for managing a patient with cystic fibrosis?
Managing cystic fibrosis (CF) requires a multidisciplinary approach focusing on airway clearance, nutritional support, and infection control. It’s a challenging chronic condition impacting the lungs, pancreas, and other organs.
Key Considerations:
- Airway Clearance: Regular airway clearance techniques are essential to remove mucus buildup, which is a hallmark of CF. These can include CPT, PEP therapy, HFCWO, or other techniques, tailored to the patient’s individual needs.
- Medication Management: This involves administering bronchodilators, mucolytics, and antibiotics to manage infections and improve lung function. Many patients with CF benefit from CFTR modulator drugs.
- Nutritional Support: Malabsorption due to pancreatic insufficiency is common in CF. This often requires enzyme supplementation and a high-calorie, high-protein diet.
- Infection Control: Patients with CF are at high risk of recurrent respiratory infections, often caused by Pseudomonas aeruginosa and other bacteria. This necessitates aggressive management of infections, including antibiotics and infection control practices.
- Pulmonary Rehabilitation: This helps improve exercise tolerance, breathing techniques, and overall quality of life.
- Monitoring and Assessment: Regular monitoring of lung function, nutritional status, and infection markers is critical for early detection and management of complications.
Example: A CF patient may require daily airway clearance treatments, regular intravenous antibiotic therapy for chronic Pseudomonas aeruginosa infections, pancreatic enzyme supplements, and nutritional counseling to maintain adequate caloric intake. Close monitoring of their pulmonary function tests and other vital parameters is crucial for effective disease management.
Q 21. How do you manage a patient with sleep apnea?
Managing sleep apnea involves identifying the type of apnea (obstructive, central, or mixed), assessing its severity, and implementing appropriate treatment strategies. It’s a condition characterized by pauses in breathing during sleep.
Management Strategies:
- Lifestyle Modifications: For mild cases, lifestyle changes such as weight loss, avoiding alcohol and sedatives before bed, and sleeping on one’s side can be helpful.
- Positive Airway Pressure (PAP) Therapy: This is the gold standard treatment for moderate to severe obstructive sleep apnea. CPAP (continuous positive airway pressure) and BiPAP (bilevel positive airway pressure) machines provide consistent airflow to keep the airway open during sleep.
- Oral Appliances: Mouthguards or other oral appliances can reposition the jaw and tongue to prevent airway obstruction. They are often used for mild to moderate cases or as an alternative to CPAP in certain situations.
- Surgery: In some cases, surgery may be considered to correct structural abnormalities contributing to sleep apnea, such as tonsillectomy or uvulopalatopharyngoplasty (UPPP).
- Adaptive Servo-Ventilation (ASV): This advanced form of PAP therapy is used for patients with central sleep apnea or Cheyne-Stokes respiration.
Assessment: Diagnosis often involves a sleep study (polysomnography) to assess the severity and type of sleep apnea. This helps guide treatment decisions. Patients often report daytime sleepiness, snoring, and witnessed apnea events.
Example: A patient with moderate obstructive sleep apnea may be prescribed CPAP therapy. I would educate them on proper use, mask fitting, and troubleshooting common issues. Regular follow-up is important to ensure compliance and effectiveness of the treatment.
Q 22. Explain your experience with chest physiotherapy.
Chest physiotherapy (CPT) is a collection of techniques used to clear secretions from the lungs and improve lung function. My experience encompasses a wide range of CPT modalities, including postural drainage, percussion, vibration, and assisted coughing. I’ve worked with patients across the age spectrum, from infants with cystic fibrosis to elderly individuals with chronic obstructive pulmonary disease (COPD).
For instance, with a pediatric patient with cystic fibrosis, I would carefully select appropriate postural drainage positions to optimize gravity’s assistance in mobilizing mucus. This would be followed by gentle percussion and vibration to further loosen the secretions. With an elderly patient with COPD, the approach might necessitate more cautious techniques, possibly focusing on assisted coughing and breathing exercises to minimize strain and fatigue. I always assess the patient’s individual needs and tolerance levels to customize the treatment plan.
My experience also includes the use of airway clearance devices, such as the Flutter valve and the Acapella device. I’m proficient in educating patients and their families on proper self-administered CPT techniques to maintain lung health at home, empowering them to manage their condition effectively.
Q 23. How do you educate patients and their families about respiratory care?
Educating patients and their families about respiratory care is crucial for successful disease management and improved outcomes. My approach involves a multi-faceted strategy that emphasizes clear, concise communication tailored to the individual’s understanding. I avoid medical jargon and instead use simple, relatable analogies.
For example, when explaining asthma, I might compare the airways to a garden hose that’s narrowed by swelling, making it harder for air to flow. Similarly, I use visual aids like diagrams and videos to enhance comprehension. I encourage active participation through question-and-answer sessions and demonstrate techniques practically, such as using a spacer with an inhaler or performing proper breathing exercises.
Patient and family education extends beyond the initial sessions. I provide written materials, develop personalized care plans, and ensure easy access to follow-up consultations, addressing any emerging concerns or questions. I firmly believe that empowering patients with knowledge helps them become active participants in their healthcare, leading to better self-management and improved quality of life.
Q 24. Describe your experience with airway management techniques.
Airway management is a cornerstone of respiratory care, and my experience encompasses a range of techniques, from basic airway adjuncts to advanced procedures. I’m proficient in the use of oropharyngeal and nasopharyngeal airways, endotracheal intubation, and tracheostomy care. I’ve managed airways in various settings, including intensive care units (ICUs) and emergency departments.
For instance, I’ve assisted in managing patients experiencing respiratory distress, requiring rapid sequence intubation to secure the airway and provide mechanical ventilation. My experience includes troubleshooting airway complications, such as managing difficult airways and recognizing and addressing signs of airway obstruction. I am skilled in suctioning techniques and maintaining airway patency, ensuring optimal gas exchange and preventing potential life-threatening events. In tracheostomy care, I’m experienced in suctioning, cannula changes, and the management of potential complications, like bleeding and infection.
Safety is paramount in airway management. I meticulously follow established protocols and guidelines, ensuring the use of appropriate personal protective equipment (PPE). My training includes advanced cardiac life support (ACLS) and pediatric advanced life support (PALS), reflecting my commitment to providing safe and effective airway management in critical situations.
Q 25. What are the ethical considerations in respiratory care?
Ethical considerations in respiratory care are multifaceted and central to my practice. The core principles of beneficence (acting in the patient’s best interest), non-maleficence (avoiding harm), autonomy (respecting patient choices), and justice (fair and equitable treatment) guide my decision-making.
For example, respecting patient autonomy includes ensuring informed consent before initiating any procedures or treatments. This means providing clear and understandable explanations, addressing concerns, and ensuring the patient understands the risks and benefits before making a decision. Balancing beneficence and non-maleficence is crucial, for instance, when deciding the aggressiveness of treatment based on a patient’s prognosis and quality of life. It’s sometimes challenging to make these decisions, requiring careful consideration and collaboration with the healthcare team.
Maintaining confidentiality is also paramount. I meticulously protect patient information according to HIPAA regulations and hospital policies. Ensuring equitable access to respiratory care, regardless of a patient’s background or socioeconomic status, remains a critical ethical imperative.
Q 26. How do you handle challenging or stressful situations in respiratory care?
Respiratory care can present challenging and stressful situations, such as managing a patient experiencing acute respiratory failure or dealing with a family experiencing grief and loss. My approach involves remaining calm and organized, employing effective problem-solving strategies, and prioritizing teamwork.
In a critical situation, I follow established protocols, systematically assess the patient’s condition, and communicate clearly with the healthcare team. This includes promptly alerting the physician and implementing appropriate interventions based on the patient’s needs. I prioritize teamwork to ensure seamless and effective care delivery. Open and honest communication with the patient and family is crucial, offering empathy and support during difficult times.
To manage stress personally, I utilize stress-reduction techniques, including mindfulness and regular exercise. I recognize the importance of self-care to maintain my well-being and provide optimal patient care. Seeking support from colleagues and supervisors is also important in processing stressful experiences.
Q 27. Describe your experience with using respiratory monitoring equipment.
My experience with respiratory monitoring equipment is extensive, encompassing a wide range of devices used to assess and monitor patients’ respiratory status. This includes arterial blood gas analysis, pulse oximetry, capnography, spirometry, and mechanical ventilators. I am proficient in operating and interpreting data from these devices, using this information to guide treatment decisions and assess patient responses to therapy.
For example, I regularly interpret arterial blood gas results to assess a patient’s oxygenation, ventilation, and acid-base balance. This information is crucial in determining the need for supplemental oxygen, ventilator adjustments, or other respiratory support. I’m adept at troubleshooting equipment malfunctions, ensuring accurate data collection and timely intervention. I also understand the limitations of each device and utilize them judiciously, ensuring their appropriate application in various clinical contexts.
Continual professional development keeps me abreast of advancements in respiratory monitoring technology and ensures that my skills remain current and effective. Staying up-to-date on best practices and technological innovations is critical for providing optimal respiratory care.
Key Topics to Learn for Respiratory Care Planning Interview
- Assessment and Diagnosis: Understanding the process of evaluating patient respiratory status, interpreting arterial blood gases (ABGs), and identifying the underlying causes of respiratory distress. This includes mastering techniques for accurately assessing vital signs and recognizing subtle indicators of respiratory compromise.
- Treatment Planning: Developing individualized treatment plans based on patient assessment findings. This involves selecting appropriate modalities such as oxygen therapy, mechanical ventilation, bronchodilators, and airway clearance techniques, considering patient-specific factors and potential complications.
- Medication Management: Knowing the indications, contraindications, side effects, and interactions of common respiratory medications. This includes understanding how to titrate medications based on patient response and monitoring for adverse effects.
- Mechanical Ventilation: A comprehensive understanding of ventilator settings, modes, and alarms. This involves troubleshooting ventilator malfunctions, understanding weaning parameters, and recognizing the signs of ventilator-associated complications.
- Airway Management: Proficiency in airway techniques, including endotracheal intubation, tracheostomy care, and suctioning. This includes understanding the proper procedures, potential risks, and complications associated with each.
- Ethical and Legal Considerations: Familiarity with ethical decision-making in respiratory care and adherence to legal standards of practice. This includes understanding patient rights, informed consent, and documentation requirements.
- Patient and Family Education: Developing effective communication strategies to educate patients and families about their respiratory condition and treatment plan. This includes adapting communication styles to meet diverse learning needs.
- Collaboration and Teamwork: Understanding the importance of interprofessional collaboration with physicians, nurses, and other healthcare professionals to ensure optimal patient care. This includes effective communication and coordination within the healthcare team.
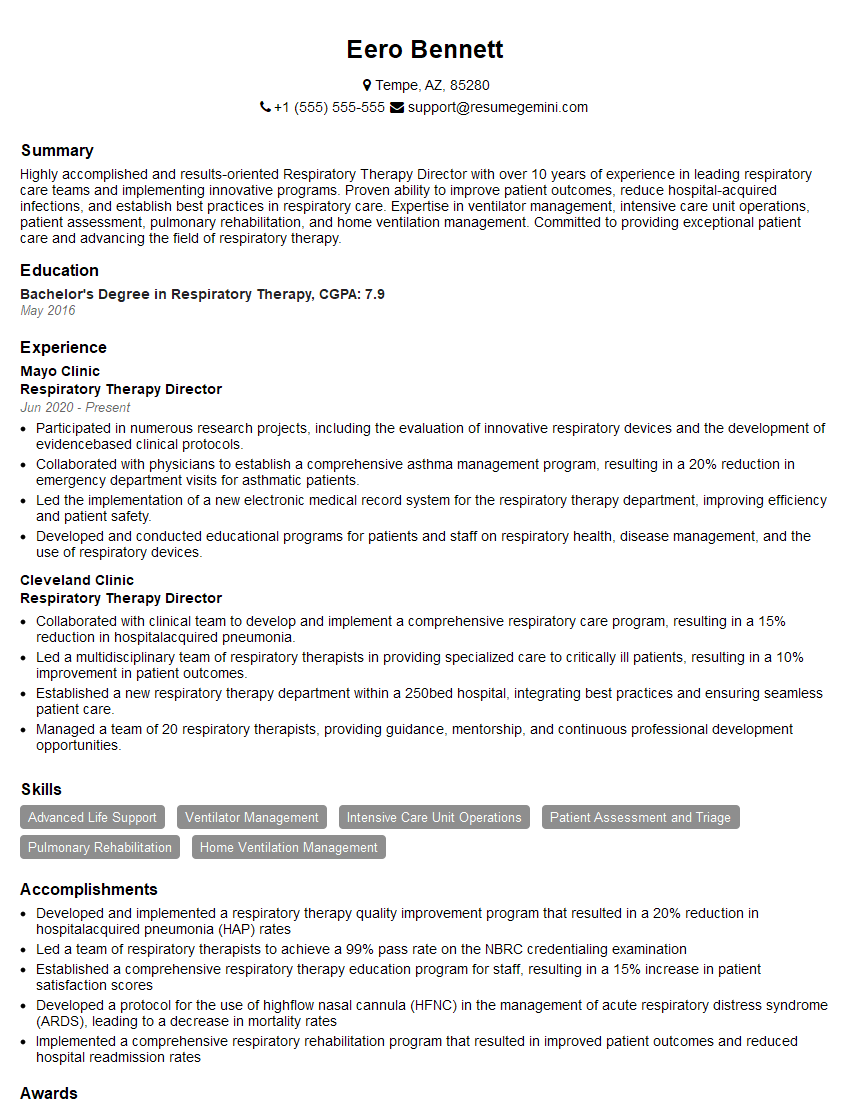
Next Steps
Mastering Respiratory Care Planning is crucial for advancing your career, opening doors to specialized roles and leadership opportunities. A well-crafted resume is your first impression; make it count! Building an ATS-friendly resume significantly increases your chances of getting noticed by recruiters and landing interviews. ResumeGemini is a trusted resource that can help you create a professional and impactful resume, tailored to highlight your unique skills and experience in Respiratory Care Planning. Examples of resumes specifically designed for Respiratory Care Planning professionals are available to help guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.