Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Ability to collaborate effectively with other professionals (e.g., physicians, teachers, social workers) interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Ability to collaborate effectively with other professionals (e.g., physicians, teachers, social workers) Interview
Q 1. Describe a situation where you had to negotiate a compromise with a colleague from a different professional background.
Negotiating compromises is crucial for effective interprofessional collaboration. It involves finding mutually acceptable solutions when differing professional perspectives arise. In one instance, I was working with a physician and a social worker on a case involving a patient with complex medical and social needs. The physician prioritized immediate medical intervention, focusing on aggressive treatment, while the social worker emphasized the patient’s emotional wellbeing and long-term support system. The disagreement stemmed from resource allocation – the aggressive treatment plan was expensive and might compromise the funds available for crucial social support services. To find a compromise, I facilitated a discussion using a collaborative problem-solving approach. We clarified each other’s goals, explored the potential consequences of each plan, and brainstormed alternatives. We ultimately agreed on a modified treatment plan that incorporated the physician’s medical expertise and the social worker’s knowledge of the patient’s social context, ensuring both the immediate medical needs and long-term support were addressed while considering budget constraints.
Q 2. How do you handle disagreements with colleagues in a professional setting?
Disagreements are inevitable in any collaborative setting. My approach prioritizes respectful communication and a focus on shared goals. I begin by actively listening to understand the colleague’s perspective, ensuring that I fully grasp their reasoning. Then, I clearly and respectfully articulate my own position, emphasizing the evidence supporting my viewpoint. If a direct resolution isn’t immediately apparent, I suggest structured methods like brainstorming alternative solutions or seeking input from another team member as a neutral mediator. The focus remains on finding common ground and a solution that benefits the patient or the overall team objective, not on winning an argument.
Q 3. Explain your approach to conflict resolution in an interprofessional team.
My approach to conflict resolution within an interprofessional team follows a structured process. First, I identify the source of the conflict, ensuring everyone understands the issue from multiple perspectives. Then, I facilitate open and respectful dialogue, encouraging each member to express their concerns without interruption. I actively listen, summarizing each point to ensure mutual understanding. If the team cannot reach a resolution, I advocate for involving a neutral third party mediator—someone with experience in conflict resolution within interprofessional teams. This approach ensures that all voices are heard, that the process is fair, and that a solution is reached that prioritizes the best interests of the patient or the overall objective.
Q 4. How do you ensure effective communication with professionals from diverse backgrounds?
Effective communication with diverse professionals requires adaptability and cultural sensitivity. I begin by clarifying my own communication style and recognizing its strengths and weaknesses. Then I make a conscious effort to adapt my approach to the communication style of my colleagues. For instance, some colleagues prefer direct communication while others prefer more nuanced or indirect approaches. I actively listen to understand how each professional prefers to receive and provide information and adapt accordingly. I also prioritize the use of clear and concise language, avoiding jargon and technical terms that may not be universally understood. Finally, I am mindful of cultural differences in communication styles, recognizing that these differences can impact the way information is shared and interpreted.
Q 5. Describe your experience working within an interdisciplinary team to achieve a shared goal.
In a recent interdisciplinary project focused on improving patient discharge planning, our team – comprising nurses, physicians, social workers, and physical therapists – collaborated effectively to achieve a shared goal. We established clear roles and responsibilities at the outset. Each member’s specific expertise was acknowledged and valued. We regularly held meetings using a structured agenda to ensure efficiency and to track progress against pre-determined milestones. We utilized a shared electronic platform to facilitate communication and document sharing, minimizing misunderstandings. Regular progress checks allowed us to identify and address challenges early on, thereby avoiding significant delays or setbacks. The result was a more streamlined and effective patient discharge process, improving patient outcomes and satisfaction.
Q 6. How would you handle a situation where a colleague’s actions are detrimental to patient care?
Addressing a colleague’s actions detrimental to patient care requires a thoughtful and professional approach. I would first attempt a private conversation with the colleague, clearly and respectfully explaining my concerns and providing specific examples of the behavior. I would focus on the impact of their actions on patient safety and well-being, rather than on making a personal attack. If the behavior continues after this initial discussion, I would involve my supervisor or a designated ethics committee, documenting all occurrences with dates, times and witnesses. My primary concern remains patient safety, and I would act according to established protocols and professional guidelines to ensure patient wellbeing.
Q 7. Provide an example of how you adapted your communication style to effectively collaborate with someone with a different communication style.
I once collaborated with a physician who preferred concise, data-driven communication, while my communication style is more narrative and context-focused. Recognizing this difference, I adjusted my approach. When presenting information, I focused on providing concise data points and key clinical findings first. After presenting the core data, I would then provide additional context and background information only if needed. By structuring my communication to address his preference for succinctness while still providing all the necessary information, I ensured effective collaboration and avoided potential misunderstandings. This adaptation significantly improved our working relationship and enhanced our shared project’s success.
Q 8. Explain your understanding of the importance of respecting different professional roles and perspectives.
Respecting different professional roles and perspectives is paramount for effective interprofessional collaboration. It acknowledges that each profession brings unique expertise, values, and approaches to problem-solving. Failure to appreciate these differences can lead to misunderstandings, conflict, and ultimately, suboptimal patient or client outcomes.
For instance, a physician might prioritize immediate medical interventions, while a social worker focuses on the patient’s broader social and environmental context. A teacher might highlight the importance of a child’s learning environment, while a therapist addresses their emotional well-being. Recognizing these varied viewpoints allows for a more holistic and comprehensive understanding of the situation and a more effective collaborative solution.
Respect extends to actively listening to others, valuing their contributions, and acknowledging their expertise even if it differs from your own. It also involves being mindful of communication styles and adapting your approach as needed to foster understanding. This might involve using clear and concise language, avoiding jargon, and being open to feedback.
Q 9. How do you contribute to a positive and productive team environment?
Contributing to a positive and productive team environment involves several key strategies. I believe in fostering open communication, actively listening to colleagues, and providing constructive feedback. I strive to be a proactive team member, taking initiative and offering support where needed.
For example, during a recent project involving a complex case, I identified a potential communication breakdown between the nursing staff and the physiotherapy team. I facilitated a brief meeting where we could openly discuss the concerns and collaboratively establish a clear communication protocol. This prevented misunderstandings and helped streamline the patient’s care.
I also prioritize building rapport with colleagues through casual interactions, showing genuine interest in their work and perspectives, and celebrating team successes. A positive and respectful atmosphere encourages everyone to feel valued and contributes significantly to productivity.
Q 10. Describe a time you successfully facilitated a collaborative decision-making process.
In a previous role, we faced a challenging situation with a patient exhibiting complex behavioral issues. The interprofessional team (including physicians, nurses, therapists, and social workers) had differing opinions on the best course of action. I facilitated a collaborative decision-making process by using a structured approach.
First, I ensured all team members had a clear understanding of the patient’s situation and challenges. Then, I guided a brainstorming session, where each member shared their perspectives and proposed potential solutions. I documented all suggestions, ensuring everyone felt heard.
Next, we systematically evaluated each proposed solution against established evidence-based practices and the patient’s specific needs. This involved weighing the pros and cons of each approach, considering potential risks and benefits. Finally, we reached a consensus on the best course of action through respectful discussion and compromise. The success of this collaborative process resulted in a comprehensive and effective care plan that addressed the patient’s complex needs and significantly improved their outcomes.
Q 11. How do you handle differing opinions within an interprofessional team?
Differing opinions within an interprofessional team are inevitable and often beneficial, as they lead to a more comprehensive understanding of the issue at hand. My approach focuses on respectful dialogue and constructive conflict resolution. I encourage each member to clearly articulate their viewpoints, providing rationale and supporting evidence.
I actively listen to understand each perspective, asking clarifying questions to ensure I fully grasp their concerns and reasoning. If a compromise isn’t immediately apparent, I encourage the team to focus on common goals and shared values. We might use tools such as prioritizing objectives or creating a decision matrix to weigh options objectively.
The goal is not to eliminate differences but to find common ground and reach a solution that respects the various perspectives and prioritizes the best interests of the patient or client. If necessary, I might facilitate a structured process, such as a consensus-building meeting, to ensure everyone feels heard and valued throughout the discussion.
Q 12. Describe your experience using technology to facilitate collaboration with colleagues.
Technology plays a vital role in facilitating collaboration. We regularly use secure video conferencing platforms (e.g., Zoom, Teams) for meetings, allowing for real-time interaction and discussion, even when team members are geographically dispersed.
We utilize secure electronic health records (EHR) systems and project management software to share information, documents, and updates efficiently. Example: Using a shared Google Doc to collaboratively write a care plan. This ensures that everyone has access to the most up-to-date information. Secure messaging platforms enhance quick communication for urgent updates and reduce reliance on less secure channels like personal email.
The use of technology necessitates careful attention to data privacy and security. We adhere strictly to confidentiality protocols to protect sensitive patient information. Understanding and implementing the security features of our chosen platforms is crucial.
Q 13. How do you ensure confidentiality and ethical conduct when collaborating with other professionals?
Confidentiality and ethical conduct are paramount in any interprofessional collaboration. We adhere strictly to HIPAA regulations and other relevant privacy laws. All discussions and communications regarding patients or clients are conducted within secure channels and only with authorized personnel.
Before sharing any information, I ensure I have obtained appropriate consent and understand the limitations on disclosure. I am mindful of the potential risks associated with information sharing and take proactive measures to minimize those risks. If any ethical dilemmas arise, I actively seek guidance from relevant authorities or professional bodies.
Open communication about confidentiality protocols is key. I regularly remind team members about their responsibilities and the importance of protecting sensitive information. This includes the appropriate use of technology, including secure messaging and the proper disposal of physical documents containing confidential information.
Q 14. How do you contribute to team building and morale within an interprofessional team?
Team building and morale are essential for effective interprofessional collaboration. I actively participate in team-building activities, such as informal gatherings or professional development workshops. These events foster camaraderie and strengthen working relationships.
I actively celebrate team successes, acknowledging the contributions of individual members. Recognizing accomplishments, big or small, boosts morale and fosters a sense of shared purpose. I also advocate for a supportive and inclusive environment where all team members feel comfortable sharing their ideas and concerns.
Furthermore, I promote open communication and feedback, ensuring that everyone feels heard and valued. Providing constructive feedback and actively seeking feedback from others contributes to continuous improvement and strengthens team cohesion. I believe in a collaborative atmosphere where everyone feels empowered and respected – this is essential for high morale and sustained productivity.
Q 15. What methods do you use to gather and incorporate input from colleagues with different expertise?
Gathering input from colleagues with diverse expertise requires a multifaceted approach. It’s not just about hearing their opinions, but actively incorporating their unique perspectives into a cohesive strategy. I employ several methods to achieve this:
Structured Meetings: I facilitate meetings with clear agendas and defined roles, ensuring everyone has a chance to contribute. This often includes pre-reading materials to level the playing field and maximize efficiency.
Brainstorming Sessions: We use brainstorming to generate a wide range of ideas, fostering a safe space for all members to share freely, even seemingly unconventional thoughts. These sessions usually follow a structured process to ensure all voices are heard and ideas are categorized and prioritized.
Individual Consultations: I schedule one-on-one consultations with team members to delve deeper into their specialized areas. This ensures I understand their perspectives and concerns fully, creating a more personalized and comprehensive approach.
Collaborative Documents & Platforms: We utilize shared documents (e.g., Google Docs) and project management platforms (e.g., Asana or Trello) to collect and organize inputs, track progress, and maintain a centralized repository of information. This enhances transparency and allows for asynchronous collaboration.
For example, in a recent project involving a patient with complex medical and social needs, I used this combined approach. Structured meetings allowed us to define the patient’s needs, brainstorming sessions generated potential interventions, individual consultations with the social worker and physician clarified specific requirements, and a collaborative document ensured we kept accurate records and tracked progress.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you delegate tasks effectively in an interprofessional team?
Effective delegation in an interprofessional team hinges on understanding individual strengths, matching tasks to those strengths, and fostering a culture of trust and accountability. My approach involves:
Needs Assessment: I begin by clearly identifying the task and the specific skills required. Then, I assess each team member’s expertise, workload, and availability to ensure I delegate appropriately.
Clear Communication: When delegating, I provide clear and concise instructions, setting realistic deadlines and expected outcomes. This includes outlining any resources available and potential challenges the team member might encounter.
Authority & Responsibility: I clearly define the level of authority given to the team member and hold them accountable for their assigned task. I am available to offer guidance and support without micromanaging.
Feedback Mechanism: Regular check-ins are essential to monitor progress, address any roadblocks, and provide timely feedback. I encourage open communication and ensure that team members feel comfortable seeking help if needed.
For instance, in a recent case, I delegated the task of developing a patient education pamphlet to a nurse educator, given her expertise in health literacy. I provided her with the necessary information, established a clear deadline, and scheduled regular check-ins to ensure the process was moving smoothly and that her needs were met.
Q 17. How do you ensure all team members understand their roles and responsibilities?
Ensuring everyone understands their roles and responsibilities is crucial for seamless team collaboration. I achieve this through:
Team Charter: A team charter is created at the outset, outlining each member’s role, responsibilities, and reporting structure. This document serves as a reference point throughout the project.
Role-Specific Training: When necessary, I provide role-specific training or assign mentorship opportunities to enhance team members’ understanding of their tasks.
Regular Communication: Open communication is key. I hold regular team meetings to review progress, clarify expectations, and address any questions or concerns that arise.
Visual Aids: Workflow diagrams or organizational charts can visually clarify roles and responsibilities, making it easier for everyone to understand how their work integrates with the overall team objective.
Think of it like a well-oiled machine; each part has a specific function, and understanding those functions leads to efficient teamwork. In one project, a detailed workflow chart outlining the steps involved in patient discharge planning clarified everyone’s roles, leading to a smoother and more efficient process.
Q 18. How do you monitor the effectiveness of collaborative efforts and make necessary adjustments?
Monitoring the effectiveness of collaborative efforts is an ongoing process that requires both quantitative and qualitative assessment. I use a combination of methods:
Data Tracking: We track key metrics relevant to our goals. This might involve monitoring patient outcomes, project timelines, or team productivity. These data help identify areas for improvement.
Regular Evaluations: We conduct regular team evaluations, including self-assessments and peer feedback, to reflect on our performance and identify areas for improvement. This can take the form of structured feedback sessions or informal discussions.
Process Improvement: Based on the data and feedback, we collaboratively brainstorm solutions and implement process improvements to enhance our effectiveness. This might include revising workflows, improving communication strategies, or seeking additional training.
Outcome Measurement: Ultimately, we measure the success of our collaborative efforts by assessing whether we achieved our stated goals. This ensures that our actions align with our overall objectives.
For example, in a project aimed at reducing hospital readmissions, we tracked readmission rates, patient satisfaction scores, and team collaboration effectiveness. When we noticed a rise in readmissions, we analyzed the data, reviewed our processes, and implemented changes resulting in a marked improvement.
Q 19. Describe your experience mentoring or guiding other professionals in a collaborative setting.
I have extensive experience mentoring and guiding other professionals in collaborative settings. My approach focuses on fostering growth, developing skills, and promoting collaborative spirit.
Personalized Guidance: I tailor my mentorship style to the individual’s needs and learning style, providing customized guidance and support.
Skill Development: I help mentees develop essential skills for effective collaboration, such as communication, conflict resolution, and teamwork.
Observation and Feedback: I observe mentees in action, providing constructive feedback to help them improve their performance. This feedback is always framed constructively and focused on growth.
Resource Provision: I connect mentees with relevant resources, such as training materials, workshops, or networking opportunities, to further enhance their skills and professional development.
I recently mentored a new social worker in our team, providing her with guidance on navigating the complexities of interprofessional collaboration, including effective communication strategies and conflict resolution techniques. Her professional development is now significantly improved, allowing her to contribute more effectively to the team.
Q 20. How do you balance the needs of individual patients or clients with the overall goals of the team?
Balancing individual patient needs with overall team goals requires a delicate balance of empathy and strategic planning. I utilize the following approaches:
Individualized Care Plans: We develop individualized care plans that address the unique needs of each patient while aligning with the team’s overall objectives. This requires open communication and shared decision-making.
Prioritization and Triage: In situations with competing needs, we prioritize interventions based on urgency and clinical significance, ensuring that the most critical needs are addressed first. This involves open discussion within the team to reach a consensus.
Ethical Considerations: We carefully consider ethical implications when prioritizing care, ensuring that all decisions are made in the best interests of the patient, while also adhering to resource limitations and team goals.
Advocacy: I advocate for patients’ needs within the team, ensuring their voices are heard and that their preferences are considered in the decision-making process. This includes actively participating in team discussions and presenting diverse viewpoints.
For example, in a case involving an elderly patient with multiple comorbidities, we carefully prioritized interventions based on the urgency of their needs while balancing resource allocation across the team. This approach ensured the patient received the most effective and timely care, in line with our team’s overall goals.
Q 21. How do you manage time constraints and competing priorities when working within a team?
Managing time constraints and competing priorities requires proactive planning and efficient teamwork. I employ several strategies:
Project Planning & Prioritization: We use project management tools to define tasks, establish timelines, and assign responsibilities. We prioritize tasks based on urgency and importance.
Time Blocking: I allocate specific time blocks for different tasks, ensuring sufficient time for each activity. This helps maintain focus and prevents multitasking which can reduce efficiency.
Regular Check-ins: Frequent team meetings and check-ins allow us to monitor progress, address potential delays, and make necessary adjustments. This allows for early identification and resolution of potential conflicts.
Delegation & Collaboration: Effective delegation and collaboration distribute the workload, maximizing efficiency and mitigating the impact of time constraints. This ensures that work is distributed fairly and effectively.
In a recent fast-paced project involving multiple patients, we utilized a Kanban board to visualize our workflow and prioritize tasks based on urgency. This allowed us to manage our time effectively, meet all deadlines, and maintain a high level of quality in our work.
Q 22. Describe a time you had to adapt your approach to collaboration due to unforeseen circumstances.
Adapting my collaborative approach often involves recognizing the unexpected and adjusting strategies accordingly. Think of it like navigating a river – you have a planned route, but unexpected rapids (unforeseen circumstances) require course correction.
For instance, during a community health initiative, our team (comprising physicians, nurses, and social workers) planned a series of workshops. A sudden surge in flu cases forced us to pivot. We quickly adapted by transitioning some workshops to a virtual format, utilizing teleconferencing and online platforms. We also collaborated with the local health department to prioritize flu prevention messaging in our remaining in-person sessions. This required open communication, flexibility, and a willingness to abandon the original plan to meet the community’s immediate needs.
This experience highlighted the importance of contingency planning and clear communication channels within a team. Having a flexible plan B—and the ability to communicate that plan effectively—is crucial for navigating unforeseen circumstances.
Q 23. How do you use constructive feedback to improve collaboration within your team?
Constructive feedback is the lifeblood of effective collaboration. It’s not about criticism, but about shared growth. I approach it using the ‘feedback sandwich’ method: starting with a positive comment, highlighting an area for improvement, and ending with another positive note. This helps mitigate defensiveness and focuses on solutions.
For example, if a colleague consistently misses deadlines in our shared project, I wouldn’t just say, ‘You’re always late’. Instead, I might say, ‘I appreciate your dedication to the project’s overall success. However, consistently missing deadlines impacts our timeline. Perhaps we could discuss time management strategies to ensure timely completion.’ Then I’d finish with, ‘Your insights are invaluable to the team, and I’m confident we can work together to improve this.’ This allows for a more receptive and productive conversation.
This approach is particularly beneficial when working with diverse personalities and experience levels, fostering a culture of continuous improvement and mutual respect.
Q 24. How do you handle situations where there are power imbalances within the team?
Power imbalances are a significant challenge in interprofessional teams. They can stifle creativity and hinder effective collaboration. The key is to create a culture of shared decision-making and mutual respect, where everyone’s voice is heard.
In one instance, I worked on a project where a senior physician consistently dominated discussions. Instead of confronting them directly, I focused on facilitating inclusive participation. I actively sought input from other team members, explicitly asking for their opinions and ensuring their perspectives were considered during discussions. I also utilized techniques like round-robin brainstorming to provide each team member with equal opportunity to share their ideas. This helped to gradually redistribute power and ensure that decisions were based on collective knowledge and perspectives, rather than the opinion of one dominant individual.
By consciously creating a level playing field, I encouraged collaborative decision-making, and ultimately, stronger team cohesion.
Q 25. How do you recognize and address biases that may affect collaborative work?
Recognizing and addressing bias is paramount to effective collaboration. Unconscious biases can subtly influence our interactions and judgments, affecting the overall teamwork. I actively work to foster self-awareness and create a culture of accountability.
We use structured checklists during team meetings to ensure all voices are heard and to address potential biases in decision-making. For instance, we might ask ourselves: ‘Have we considered all perspectives, especially from those who may be underrepresented?’ or ‘Are our decisions based on evidence, or on unconscious assumptions?’ This approach promotes reflection and helps us challenge our own biases as well as the biases of others.
Ongoing training on diversity and inclusion also plays a critical role in creating a safe and equitable environment for everyone on the team.
Q 26. Explain your experience with documenting and reporting on interprofessional collaborations.
Documentation is essential for transparency and accountability in interprofessional collaboration. We use a combination of methods to ensure thorough recording and reporting.
Our team utilizes shared electronic platforms for tracking progress, recording meeting minutes, and sharing documents. We also maintain a central repository for all project-related communications and data. This ensures that all team members have access to the same information, facilitating consistent understanding and efficient progress. This includes detailed reports that highlight contributions from different professionals, highlighting individual expertise and collaborative efforts. Furthermore, we adhere to strict confidentiality protocols to safeguard patient data and adhere to ethical guidelines.
These meticulous documentation practices are crucial for tracking outcomes, demonstrating accountability, and ensuring adherence to legal and ethical standards.
Q 27. How do you maintain professional boundaries while building strong working relationships with colleagues?
Maintaining professional boundaries while building strong working relationships requires a delicate balance. It’s about fostering trust and respect while maintaining appropriate professional conduct.
I achieve this through clear communication, establishing expectations from the outset, and respecting personal boundaries. This involves limiting social interactions outside of work-related contexts, avoiding potentially compromising personal disclosures, and maintaining professional decorum at all times. This doesn’t mean you can’t be friendly or supportive; it means being mindful of professional limits to ensure a healthy and respectful work environment for everyone.
A key aspect involves understanding the ethical implications of your interactions, particularly within the context of patient care or sensitive information.
Q 28. Describe a time you resolved a conflict that threatened the effectiveness of an interprofessional team.
Conflict is inevitable in any collaborative setting. The key is addressing it constructively and promptly before it escalates. I utilize a collaborative conflict resolution approach that prioritizes understanding and finding a mutually acceptable solution.
During one project, disagreements arose between a physician and a social worker regarding a patient’s treatment plan. I facilitated a structured meeting where each individual clearly articulated their concerns and perspectives. I actively listened to both sides, emphasized the shared goal of patient well-being, and encouraged them to explore alternative solutions collaboratively. We eventually found common ground by focusing on the patient’s overall needs and redefining the treatment plan to incorporate both perspectives.
This experience emphasized the importance of active listening, empathy, and a focus on shared goals in resolving interprofessional conflicts. Utilizing a structured approach helps to prevent escalation and ensure a positive resolution, leading to stronger team dynamics in the long run.
Key Topics to Learn for Ability to Collaborate Effectively with Other Professionals (e.g., physicians, teachers, social workers) Interview
- Active Listening and Communication: Understanding diverse perspectives, clarifying expectations, and providing constructive feedback. This includes recognizing nonverbal cues and adapting communication styles to different professionals.
- Conflict Resolution and Negotiation: Strategies for addressing disagreements professionally, finding common ground, and achieving mutually beneficial outcomes. Consider role-playing scenarios involving differing opinions or priorities.
- Teamwork and Shared Goals: Defining roles and responsibilities, leveraging individual strengths, and working collaboratively towards shared objectives. Reflect on examples where you successfully contributed to a team project.
- Respectful Professional Boundaries: Understanding and maintaining appropriate professional relationships, respecting confidentiality, and navigating ethical considerations. This involves knowing when to escalate concerns to the appropriate channels.
- Interprofessional Collaboration Models: Familiarity with various models and frameworks for successful interprofessional collaboration (e.g., IPEC competencies). Consider researching and understanding best practices in your field.
- Technological Proficiency for Collaboration: Utilizing tools for effective communication and shared work, such as electronic health records, shared document platforms, and video conferencing. Think about how you’ve used technology to improve collaboration in the past.
- Understanding Different Professional Roles and Perspectives: Appreciating the unique contributions and challenges faced by physicians, teachers, social workers, and other professionals in your field. Reflect on how you’ve integrated information from different perspectives to reach a shared understanding.
Next Steps
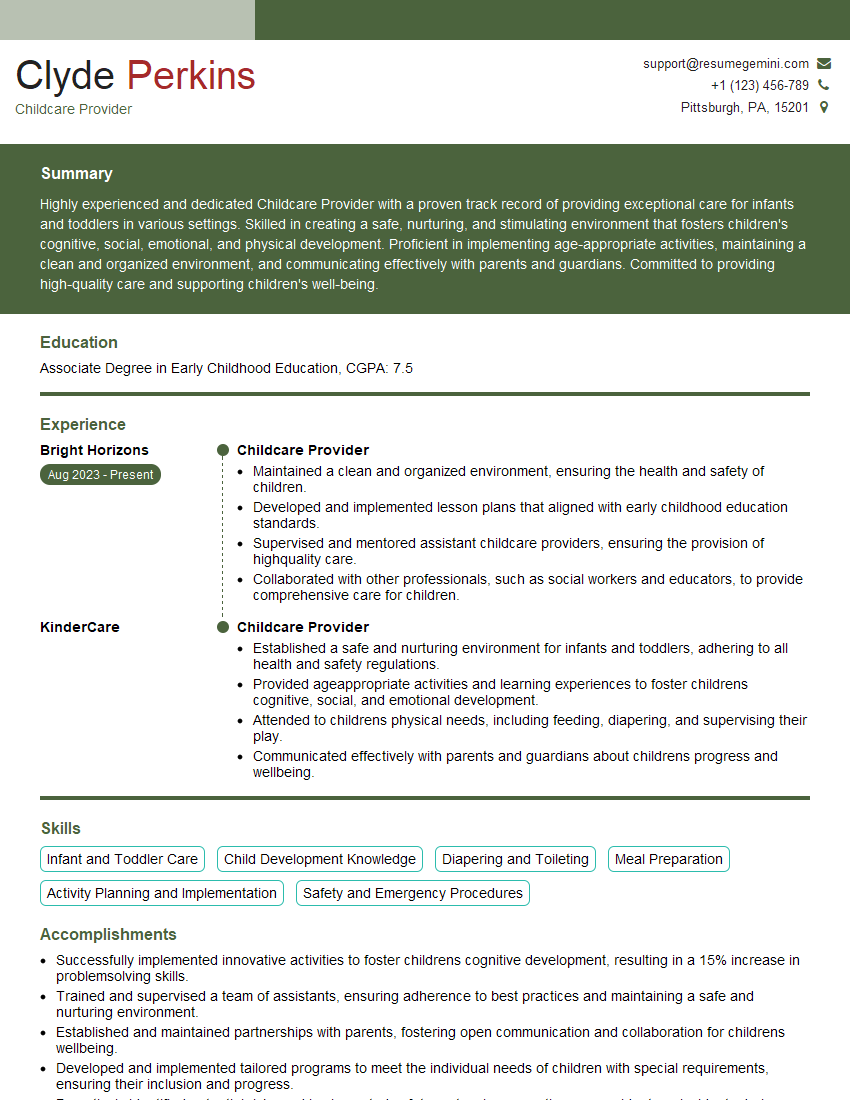
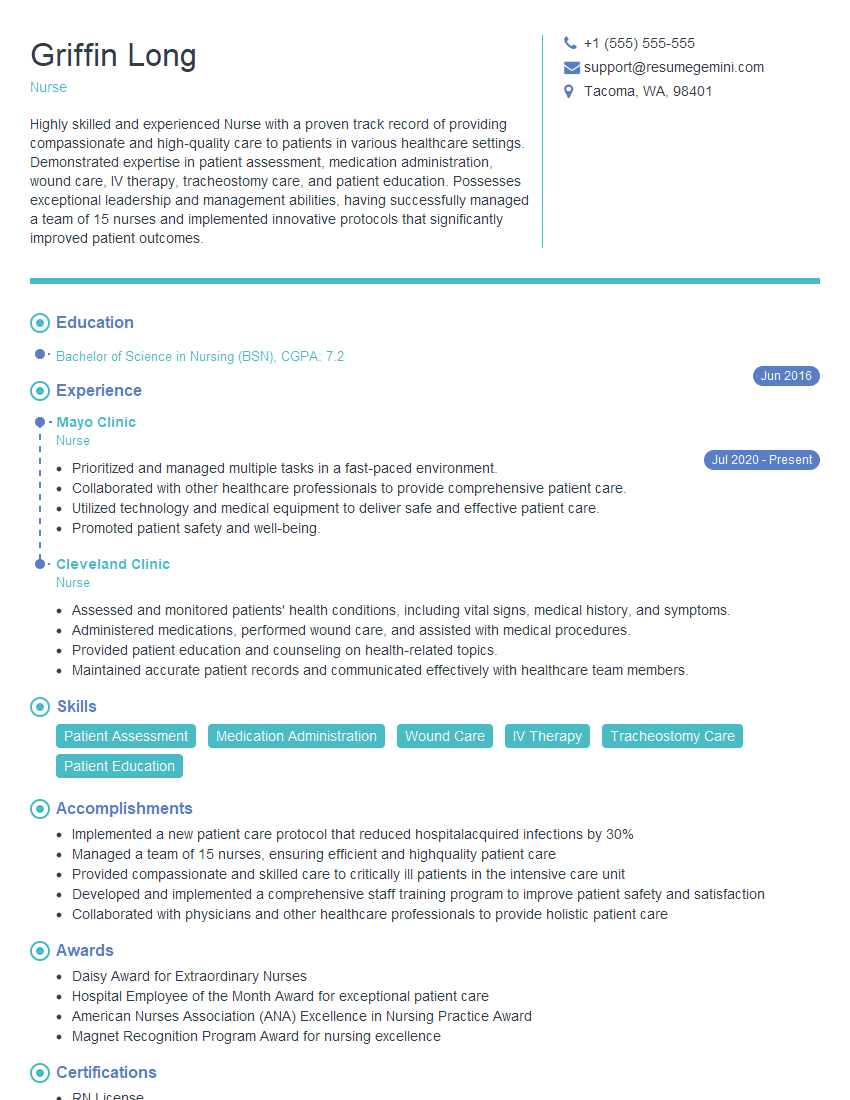
Mastering the ability to collaborate effectively is crucial for career advancement in almost any field. It demonstrates essential soft skills valued by employers and leads to more impactful and rewarding work experiences. Building an ATS-friendly resume that highlights your collaborative skills is essential for increasing your job prospects. ResumeGemini is a trusted resource that can help you craft a compelling resume showcasing your abilities. We offer examples of resumes tailored to highlight experience in collaborating effectively with other professionals like physicians, teachers, and social workers – review them to refine your own.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.