Preparation is the key to success in any interview. In this post, we’ll explore crucial Ability to provide culturally sensitive and trauma-informed care interview questions and equip you with strategies to craft impactful answers. Whether you’re a beginner or a pro, these tips will elevate your preparation.
Questions Asked in Ability to provide culturally sensitive and trauma-informed care Interview
Q 1. Define culturally sensitive care and provide a specific example.
Culturally sensitive care involves providing healthcare services that are respectful of and responsive to a patient’s cultural beliefs, values, practices, and preferences. It recognizes that culture significantly influences health behaviors, communication styles, and health-seeking behaviors. Ignoring cultural factors can lead to misunderstandings, mistrust, and ultimately, ineffective care.
Example: Imagine a patient from a culture where direct eye contact is considered disrespectful. A healthcare provider who maintains consistent eye contact throughout the conversation might be unintentionally perceived as aggressive or challenging by the patient, hindering open communication. Culturally sensitive care would involve adjusting the communication style to be more comfortable for the patient, perhaps minimizing direct eye contact while still maintaining attentiveness.
Q 2. Explain the principles of trauma-informed care.
Trauma-informed care is a strengths-based framework that recognizes the widespread impact of trauma and understands potential paths for recovery. It shifts from a ‘what’s wrong with you?’ approach to a ‘what happened to you?’ approach. The core principles are:
- Safety: Creating a physically and emotionally safe environment for patients.
- Trustworthiness and Transparency: Building rapport and fostering open communication.
- Peer Support: Utilizing peer-to-peer support and connection opportunities when appropriate.
- Collaboration and Empowerment: Involving patients in decision-making about their care.
- Choice, Control, and Autonomy: Offering patients choices and respecting their autonomy.
These principles guide healthcare professionals to avoid re-traumatizing patients and instead promote healing and recovery.
Q 3. How would you identify a patient’s cultural background and its relevance to their care?
Identifying a patient’s cultural background is crucial for providing effective care. This involves using open-ended questions, active listening, and observing non-verbal cues. It’s important to be sensitive and avoid making assumptions. For example, instead of asking, “What’s your ethnicity?”, a more respectful approach might be, “Could you tell me a little about your background and where you’re from?” This allows the patient to share what they feel comfortable sharing.
The relevance of cultural background to care is multifaceted. It influences communication styles, health beliefs (e.g., views on medication, alternative therapies), family involvement in decision-making, and preferred ways of expressing pain or discomfort. Understanding these nuances is critical to providing culturally competent and effective care.
Q 4. Describe a situation where you had to adapt your approach due to cultural differences.
I once cared for a patient from a collectivist culture where family decisions were paramount. Initially, I focused my communication solely on the patient regarding treatment options. However, I noticed the patient seemed hesitant and deferential to her family members, who were present throughout the consultations. After recognizing this cultural nuance, I adapted my approach to include the family in the decision-making process. This led to greater patient comfort, trust, and improved adherence to the treatment plan.
Q 5. What are some common trauma responses you might observe in patients?
Common trauma responses can vary widely but may include:
- Emotional: Anxiety, depression, fear, anger, shame, numbness, difficulty regulating emotions.
- Behavioral: Hypervigilance, avoidance, social isolation, substance use, self-harm, aggression.
- Physical: Chronic pain, sleep disturbances, gastrointestinal issues, fatigue.
- Cognitive: Difficulty concentrating, memory problems, intrusive thoughts, flashbacks, nightmares.
It’s vital to remember that these responses are not signs of weakness but are normal reactions to abnormal experiences. Understanding these responses allows for a more empathetic and effective therapeutic approach.
Q 6. How would you assess a patient for trauma history?
Assessing a patient for trauma history requires a sensitive and gradual approach. It’s crucial to establish trust and rapport before directly inquiring about trauma. I would begin by creating a safe and comfortable environment and using open-ended questions to explore their experiences and coping mechanisms. For example, I might ask, “Many people have experienced difficult times in their lives. Have there been any experiences that have significantly impacted your well-being?” If a patient discloses trauma, it’s crucial to listen without judgment, validate their experience, and offer support and resources. The level of detail shared should be determined entirely by the patient.
Q 7. How would you modify your communication style to be more trauma-informed?
To modify my communication style for trauma-informed care, I would focus on:
- Using validating language: Acknowledging the patient’s experience and feelings.
- Avoiding judgmental or leading questions: Letting the patient lead the conversation.
- Giving choices: Empowering patients by offering options within the therapeutic process.
- Controlling the pace: Allowing for breaks and adjustments based on the patient’s comfort level.
- Setting clear boundaries: Ensuring a safe and predictable therapeutic environment.
- Focusing on strengths and resilience: Emphasizing the patient’s coping abilities and positive attributes.
This approach helps to create a sense of safety and control, which is crucial for patients who have experienced trauma.
Q 8. Describe your experience working with diverse populations.
My experience working with diverse populations is extensive. I’ve worked in settings with significant cultural and linguistic diversity, including [mention specific settings, e.g., urban community clinics, refugee resettlement programs, international NGOs]. This involved interacting with individuals from a wide range of ethnic, racial, religious, socioeconomic, and LGBTQ+ backgrounds. For example, I recall working with a family of recent immigrants from Somalia who were struggling to navigate the healthcare system. Their experience highlighted the importance of cultural humility, patience, and the use of culturally appropriate communication strategies. Another instance involved supporting a transgender patient who felt uncomfortable sharing their medical history due to past discriminatory experiences. This reinforced the need for creating a safe and affirming space for all individuals, irrespective of their identity.
Q 9. How do you ensure you are providing equitable care?
Equitable care ensures that every individual receives the services they need, regardless of their background. This requires a multifaceted approach. Firstly, it means actively identifying and addressing systemic barriers that limit access to healthcare for marginalized communities. For example, language barriers can prevent patients from fully understanding their treatment plan. To counteract this, I prioritize access to qualified interpreters and culturally appropriate educational materials. Secondly, I strive to personalize care, recognizing that individual needs vary even within the same cultural group. Instead of applying blanket assumptions, I actively listen to my patients’ preferences and tailor my approach accordingly. Finally, I am committed to ongoing self-reflection and professional development to continually improve my cultural competency.
Q 10. What are the ethical considerations when providing culturally sensitive care?
Ethical considerations in culturally sensitive care are paramount. Central to this is respecting patient autonomy and self-determination. This means making sure that individuals understand their treatment options and feel empowered to make informed decisions, even if those decisions differ from what we might recommend. Confidentiality is another critical ethical issue, particularly when dealing with sensitive cultural practices or beliefs. I always maintain strict confidentiality, unless legally obligated otherwise. Furthermore, I am mindful of potential power imbalances in the doctor-patient relationship. I work to establish trust and mutual respect, ensuring that the patient feels heard and valued, and that their cultural perspective is acknowledged and integrated into their care. Avoiding stereotypes and assumptions is another ethical imperative. Each individual is unique, even within their cultural group.
Q 11. Explain the concept of vicarious trauma and how you mitigate its effects.
Vicarious trauma is the emotional toll that healthcare professionals can experience as a result of exposure to the trauma of their patients. It can manifest in various ways, from emotional exhaustion and burnout to feelings of hopelessness and cynicism. To mitigate vicarious trauma, I prioritize self-care practices such as mindfulness, regular exercise, and spending time with loved ones. I also engage in regular supervision with a trusted colleague or therapist to process my experiences and receive support. Maintaining professional boundaries is crucial; I avoid becoming overly invested in my patients’ lives, recognizing that this can contribute to compassion fatigue. Finally, teamwork and mutual support are vital. Openly discussing challenging cases with colleagues can help prevent isolation and foster a sense of shared responsibility.
Q 12. How do you manage potential cultural misunderstandings with patients?
Cultural misunderstandings can arise easily in healthcare interactions. My approach involves active listening, demonstrating patience, and clarifying any ambiguities. For instance, if a patient’s response seems unexpected, I’d ask clarifying questions to ensure I understand their perspective. If I am unsure about something, I would directly and respectfully ask questions, such as, ‘Could you tell me more about that?’ or ‘Could you explain your understanding of this issue?’ I also utilize non-verbal cues to show attentiveness and respect, creating a safe space for open communication. If language barriers exist, I make sure to utilize certified interpreters to ensure accurate communication. I always strive to approach these situations with humility, recognizing that misunderstandings are often unavoidable and opportunities for learning.
Q 13. What resources would you utilize to better understand a patient’s cultural background?
Understanding a patient’s cultural background often requires a multi-pronged approach. I begin by directly engaging the patient in conversation, respectfully asking about their cultural background and practices, always being mindful of their comfort level. I consult cultural resources such as reputable websites, books, and academic articles focused on understanding the cultural nuances and healthcare beliefs of different communities. When possible, I seek input from community leaders or trusted members of the patient’s cultural group, ensuring ethical and appropriate use of such networks. Furthermore, I use electronic health record (EHR) systems to identify relevant information, such as language preferences and cultural affiliations. It’s crucial to utilize these resources ethically and respectfully, ensuring the information is relevant and avoiding harmful stereotypes.
Q 14. How would you address potential biases in your own practice?
Addressing potential biases in my practice is an ongoing process that requires constant self-reflection and a commitment to lifelong learning. I actively engage in self-reflection, considering my own cultural background and potential biases that might unconsciously influence my interactions with patients. I regularly attend continuing education programs and workshops focused on cultural competency and bias mitigation. I also engage in peer supervision and seek feedback from colleagues who might offer insights into my behavior and interactions. I actively listen to my patients’ lived experiences to identify instances where my own biases might be affecting my care, and I seek out opportunities to work with mentors and colleagues from diverse backgrounds who can provide critical feedback and guidance.
Q 15. What are the limitations of culturally sensitive care?
While culturally sensitive care aims to provide equitable healthcare, its limitations stem from several factors. One major limitation is the inherent complexity of culture itself. Culture isn’t a monolithic entity; it’s a dynamic intersection of ethnicity, religion, socioeconomic status, gender, and many other factors. Attempting to understand and accommodate every nuance is practically impossible.
Another limitation lies in the potential for stereotyping. Even with the best intentions, generalizations about cultural groups can lead to misinterpretations and inaccurate assumptions about individual patient needs. For example, assuming all patients from a particular culture prefer a specific communication style could overlook individual preferences and lead to misunderstandings.
Finally, resource limitations can hinder the provision of truly culturally sensitive care. Healthcare systems may lack the necessary interpreters, culturally competent staff, or educational materials to effectively meet the diverse needs of their patient population. This lack of resources can lead to disparities in care and create barriers for patients from marginalized communities.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe a time you had to advocate for a patient facing cultural barriers.
I once worked with a young woman from a Southeast Asian community who was hesitant to disclose a severe medical issue due to deeply ingrained cultural beliefs about shame and family honor. She feared the potential consequences of revealing her condition to her family. Initially, she presented with vague symptoms, hindering accurate diagnosis and treatment.
To advocate for her, I first actively listened to her concerns and validated her feelings, acknowledging the cultural context of her hesitations. I then collaborated with a community health worker fluent in her language and familiar with her cultural background. Together, we carefully explained the potential consequences of delaying treatment in a way that respected her cultural values. We emphasized the importance of her well-being and created a plan that allowed her to share information gradually with her family, maintaining a balance between her cultural beliefs and her medical needs. With consistent support and culturally-sensitive communication, she eventually received appropriate treatment and improved significantly. This experience highlighted the vital role of collaboration and cultural understanding in patient advocacy.
Q 17. How do you ensure patient confidentiality within a culturally sensitive context?
Ensuring patient confidentiality within a culturally sensitive context requires a multifaceted approach. Firstly, it’s crucial to understand that concepts of privacy and disclosure vary significantly across cultures. Some cultures prioritize collective well-being over individual privacy, while others emphasize individual autonomy. Therefore, explicitly explaining confidentiality protocols in a way that is understandable and respects the patient’s cultural perspective is paramount.
Secondly, I employ culturally sensitive communication strategies. This includes using interpreters when necessary, avoiding medical jargon, and ensuring that all discussions about sensitive information occur in private settings where the patient feels comfortable and safe. Furthermore, I always obtain informed consent before sharing any information with family members or other healthcare professionals, ensuring the patient has a clear understanding of who will have access to their information and why. This builds trust and respects their autonomy.
Lastly, I adhere strictly to all HIPAA regulations and institutional policies regarding patient confidentiality. These guidelines provide a strong ethical and legal framework for protecting patient information, ensuring that confidentiality is upheld regardless of cultural background.
Q 18. How do you build rapport and trust with patients from diverse backgrounds?
Building rapport and trust with patients from diverse backgrounds is foundational to effective care. It starts with demonstrating genuine respect and empathy. This means actively listening to their stories, validating their experiences, and showing genuine interest in their cultural background. Avoid making assumptions, instead asking open-ended questions to encourage them to share their perspectives and concerns.
I utilize active listening techniques to show I am fully present and engaged. I pay attention not just to what is said but also to non-verbal cues, which can vary significantly across cultures. I use simple, clear language, avoiding medical jargon and using an interpreter when language barriers exist. Showing cultural sensitivity can be as simple as learning a few basic phrases in the patient’s language or acknowledging relevant cultural celebrations or traditions.
For example, I might ask about their family structure, their preferred ways of communicating, or their dietary needs and restrictions. This demonstrates respect for their cultural practices and helps create a sense of comfort and connection. Building trust takes time and consistent effort, but it’s essential for establishing a positive therapeutic relationship.
Q 19. What is your understanding of intersectionality in relation to providing care?
Intersectionality recognizes that individuals hold multiple intersecting identities—such as race, gender, class, sexual orientation, and disability—which create unique experiences of discrimination and privilege. In healthcare, this means understanding that a patient’s experience is shaped by the complex interplay of these identities, and not just one factor in isolation.
For example, a Black woman experiencing domestic violence will have different needs and challenges compared to a white woman facing the same situation. Her experience is influenced by both her gender and her race, leading to potential disparities in access to resources and the quality of care received. Ignoring the intersectionality of her identities would lead to incomplete and potentially harmful care.
To provide truly equitable care, I strive to understand the unique combination of factors influencing each patient’s health and well-being. This involves actively listening, asking thoughtful questions, and being mindful of how systemic biases and inequalities impact individuals from marginalized groups. Providing culturally sensitive and trauma-informed care necessitates acknowledging and addressing these intersecting identities.
Q 20. How would you navigate a situation where a patient’s cultural practices conflict with medical recommendations?
Navigating conflicts between a patient’s cultural practices and medical recommendations requires a delicate balance of respect, education, and negotiation. The key is to avoid imposing one viewpoint over the other. First, I strive to fully understand the patient’s cultural perspective and the reasoning behind their practices. I actively listen and seek clarification, ensuring I don’t misinterpret their beliefs or intentions.
Next, I use clear and respectful communication to explain the medical rationale for the recommendation, avoiding judgmental language and tailoring the information to their cultural context. I collaborate with the patient to find mutually acceptable solutions, exploring options that honor their cultural beliefs while also promoting their health. This might involve adapting treatment plans to accommodate specific practices or finding alternative approaches that address both medical needs and cultural sensitivities.
Involving cultural mediators or community health workers can be invaluable in such situations. They can provide additional support, ensure accurate communication, and help bridge cultural divides. The goal is always to empower the patient to make informed decisions that align with their values and their health goals. The process is about collaboration, not imposition.
Q 21. What strategies do you employ to reduce the stigma surrounding mental health issues?
Reducing stigma surrounding mental health requires a multi-pronged approach. It begins with education – both for patients and for the broader community. I actively engage in conversations that normalize mental health challenges, emphasizing that mental illness is a common experience, and help is available. I use clear, non-stigmatizing language and avoid labeling individuals.
Moreover, I encourage open conversations with patients about their mental health concerns, creating a safe and supportive environment where they feel comfortable sharing their experiences without judgment. Emphasizing hope and recovery is crucial, focusing on strengths and resilience rather than deficits. Collaborating with community organizations to offer resources and support groups can extend the reach of this message beyond the clinical setting.
Finally, I advocate for policies and initiatives that promote mental health awareness and reduce stigma within the healthcare system and the wider community. This includes challenging discriminatory practices and promoting culturally competent mental health services that are accessible to all.
Q 22. Explain how you incorporate the patient’s preferences and values into their treatment plan.
Incorporating a patient’s preferences and values is paramount to providing truly person-centered care. It’s about moving beyond a checklist approach and understanding the individual’s unique circumstances, beliefs, and goals. This involves active listening, asking open-ended questions, and demonstrating genuine empathy.
- Active Listening: I pay close attention to both verbal and nonverbal cues, ensuring I understand their perspective fully before offering suggestions. For example, if a patient expresses discomfort with a particular medication due to past experiences, I wouldn’t dismiss it; I’d explore those experiences to understand the underlying concerns.
- Shared Decision-Making: I view treatment planning as a collaborative process. I present treatment options clearly, discuss potential benefits and risks, and weigh them against the patient’s values and priorities. A patient may value a faster recovery even if it means more intense treatment, while another may prefer a gentler approach that fits better with their lifestyle.
- Cultural Considerations: I understand that values and preferences are deeply rooted in culture. For example, a patient’s religious beliefs might influence their treatment choices, such as their views on blood transfusions or specific dietary restrictions. I actively seek to understand and respect these.
Ultimately, the goal is to create a treatment plan that is not only medically sound but also aligns with the patient’s individual needs and desires, leading to better adherence and improved outcomes.
Q 23. How do you utilize self-reflection to improve your cultural competency?
Self-reflection is crucial for continuous improvement in cultural competency. It’s a process of critically examining my own biases, assumptions, and practices to identify areas where I can improve my understanding and responsiveness to diverse populations.
- Journaling: I regularly reflect on my interactions with patients, noting instances where I felt comfortable and instances where I felt less so. This helps me identify patterns and triggers.
- Seeking Feedback: I actively solicit feedback from colleagues, supervisors, and even patients (with appropriate consent and confidentiality measures in place) to gain diverse perspectives on my interactions and identify blind spots.
- Continuing Education: I regularly participate in workshops and training sessions focused on cultural competency, trauma-informed care, and implicit bias reduction. This helps me stay abreast of current best practices and learn new strategies for effective cross-cultural communication.
- Mentorship: I seek out mentors and role models from diverse backgrounds who can offer guidance and support in navigating complex cultural situations. This provides invaluable insight and helps broaden my understanding.
By consistently engaging in these self-reflective practices, I strive to continuously enhance my cultural competence and provide more equitable and effective care.
Q 24. How do you ensure safety in your practice while considering cultural factors?
Ensuring patient safety while considering cultural factors requires a multi-faceted approach that prioritizes trust, communication, and understanding.
- Building Rapport: Establishing a strong therapeutic relationship based on trust and respect is foundational. This involves taking the time to understand the patient’s background, experiences, and concerns, making them feel safe and comfortable sharing information.
- Culturally Sensitive Communication: I use clear, concise language, avoiding jargon and adapting my communication style to the patient’s preferred way of interacting. This might include adjusting my tone, pace, and nonverbal cues to align with cultural norms.
- Safety Planning: For patients who have experienced trauma or have safety concerns, I collaborate with them to develop a personalized safety plan. This could include strategies for managing triggers, connecting with support systems, or accessing emergency services.
- Collaboration with Community Resources: Recognizing the limitations of my own expertise, I work closely with community resources and organizations that specialize in culturally specific services, providing referrals when appropriate. This could include domestic violence shelters, immigrant support services, or culturally specific mental health organizations.
Addressing safety concerns requires careful consideration of cultural factors that might influence a patient’s ability or willingness to seek help. It’s not enough to just offer resources; I need to ensure that those resources are accessible and culturally appropriate for the patient.
Q 25. How would you adapt your care for a patient experiencing PTSD?
Adapting care for a patient with PTSD requires a trauma-informed approach that prioritizes safety, trust, and empowerment. It’s crucial to avoid retraumatization and to foster a sense of control and collaboration.
- Establishing Safety and Trust: I begin by creating a safe and non-judgmental therapeutic environment. This involves carefully considering the patient’s comfort level, respecting their boundaries, and proceeding at their pace.
- Trauma-Sensitive Language: I use language that avoids triggering the patient. I avoid terms like “victim” or “abuse” unless the patient uses them, opting for more neutral phrasing like “experience” or “situation.”
- Collaboration in Treatment Planning: I work collaboratively with the patient to develop a treatment plan that aligns with their needs and goals, acknowledging their expertise in their own experiences. I might incorporate techniques such as EMDR, CBT, or mindfulness practices, tailoring them to the individual’s preferences and responses.
- Phased Approach: I often use a phased approach, starting with stabilization and safety planning before moving to deeper processing of traumatic memories. This gradual approach prevents overwhelming the patient.
- Focus on Empowerment: Throughout the treatment process, I focus on building the patient’s resilience and self-efficacy, empowering them to regain control over their lives.
It’s important to remember that PTSD presents differently across individuals, and cultural factors significantly influence the expression and experience of trauma. My approach always considers these nuances.
Q 26. Describe your experience working with interpreters or translators.
My experience with interpreters and translators has been extensive and crucial in providing culturally competent care. Effective communication is the cornerstone of any therapeutic relationship, and when language barriers exist, skilled interpretation becomes indispensable.
- Choosing Qualified Interpreters: I prioritize using qualified, professional interpreters who are fluent in both languages and understand the nuances of medical terminology and cultural sensitivity. I avoid using family members or untrained individuals as interpreters, as this can compromise confidentiality and accuracy.
- Direct Communication with the Patient: Even with an interpreter present, I always address my communication directly to the patient, maintaining eye contact and engaging in non-verbal communication as appropriate. This shows respect and ensures the patient feels seen and heard.
- Cultural Considerations in Interpretation: I am aware that even professional interpreters might have their own cultural biases, which could affect the interpretation. Therefore, I try to be mindful of this potential and adapt my communication to be as clear and simple as possible.
- Post-Session Debriefing (Optional): In complex or sensitive situations, I might have a brief debriefing with the interpreter after the session to ensure accurate understanding and address any concerns.
My work with interpreters highlights the importance of recognizing that access to healthcare isn’t just about medical expertise; it’s also about ensuring clear, culturally sensitive communication.
Q 27. How would you explain the benefits of trauma-informed care to a patient?
Explaining the benefits of trauma-informed care to a patient involves demonstrating understanding and empathy. I’d start by acknowledging the impact of past experiences and emphasizing the importance of safety and collaboration.
I would say something like:
“Trauma-informed care recognizes that your past experiences might have affected how you feel and interact with the world. This approach isn’t about focusing solely on the trauma itself, but rather creating a safe and supportive environment where you feel empowered to heal at your own pace. We’ll work together to create a treatment plan that is tailored to your needs and respects your preferences. This means we’ll avoid anything that might trigger you, and we’ll focus on building your strengths and resilience.”
I would also highlight the specific ways trauma-informed care would differ from other approaches, emphasizing:
- Safety and Trust: We prioritize creating a secure and respectful environment.
- Choice and Control: You’re involved in making decisions about your treatment.
- Collaboration: We work together as partners.
- Empowerment: We focus on your strengths and abilities.
By explaining these benefits in simple, clear terms and demonstrating genuine concern, I aim to build trust and encourage active participation in the healing process.
Q 28. How would you handle a situation where you feel your own cultural biases are affecting your judgment?
Recognizing my own cultural biases is a crucial step towards providing culturally competent care. It’s important to acknowledge that biases are inherent and often unconscious, and their influence can be subtle.
If I detect my own biases affecting my judgment, I would take the following steps:
- Pause and Reflect: I would immediately pause the interaction and take some time to reflect on what triggered my biased response. What assumptions am I making? Where did these assumptions originate?
- Seek Supervision or Consultation: I would consult with a supervisor or colleague who has more experience in addressing cultural complexities. This could involve discussing the situation and exploring potential alternative approaches.
- Engage in Self-Education: I would engage in self-education through research, reading, or attending relevant workshops to further my understanding of the cultural context relevant to the situation.
- Apologize and Rectify (If Necessary): If my biases have negatively impacted the interaction, I would apologize to the patient and make efforts to rectify the situation, demonstrating a commitment to continuous improvement.
- Document the Incident: I would document the incident, including my reflection on the situation and the steps taken to address it. This contributes to self-awareness and learning from mistakes.
Addressing my biases is not a one-time event but an ongoing process. It requires continuous self-reflection, education, and a commitment to providing equitable and respectful care.
Key Topics to Learn for Ability to provide culturally sensitive and trauma-informed care Interview
- Cultural Humility: Understanding the limitations of your own cultural knowledge and the importance of continuous learning and self-reflection in providing culturally appropriate care. Practical application: Reflecting on personal biases and how they might impact patient interactions.
- Trauma-Informed Approach: Recognizing the pervasive impact of trauma on individuals and families and adapting care to minimize re-traumatization. Practical application: Employing trauma-sensitive language, creating a safe and supportive environment, and prioritizing patient autonomy.
- Understanding Cultural Differences in Health Beliefs and Practices: Exploring how diverse cultural backgrounds influence health perceptions, communication styles, and treatment preferences. Practical application: Developing strategies for effective cross-cultural communication and negotiation of care plans.
- Ethical Considerations: Addressing ethical dilemmas related to cultural sensitivity and trauma-informed care, including issues of consent, confidentiality, and power dynamics. Practical application: Analyzing case studies to develop solutions and decision-making strategies.
- Practical Application of Models & Frameworks: Familiarizing yourself with established models and frameworks for culturally sensitive and trauma-informed care. Practical application: Describing how specific frameworks guide your approach in different clinical settings.
- Self-Care and Compassion Fatigue: Recognizing the emotional toll of working with traumatized individuals and developing strategies for self-care and preventing burnout. Practical application: Discussing strategies for maintaining professional boundaries and promoting your own well-being.
Next Steps
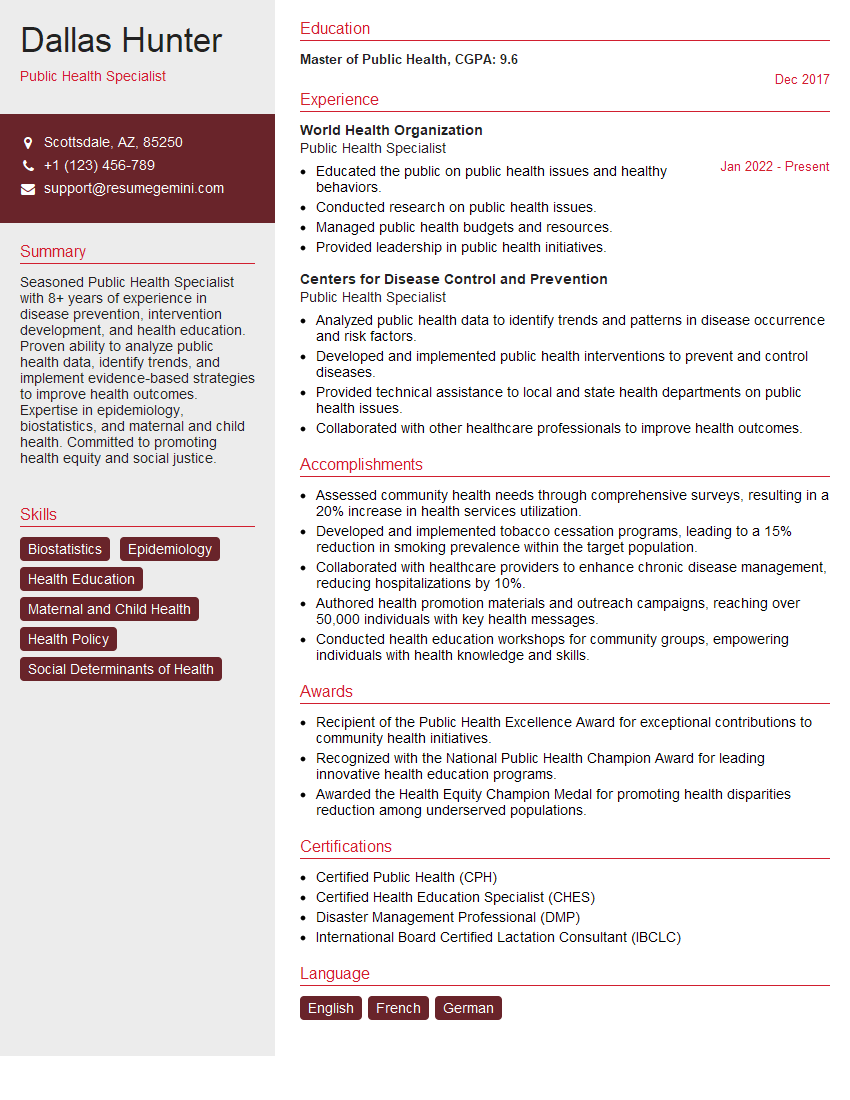
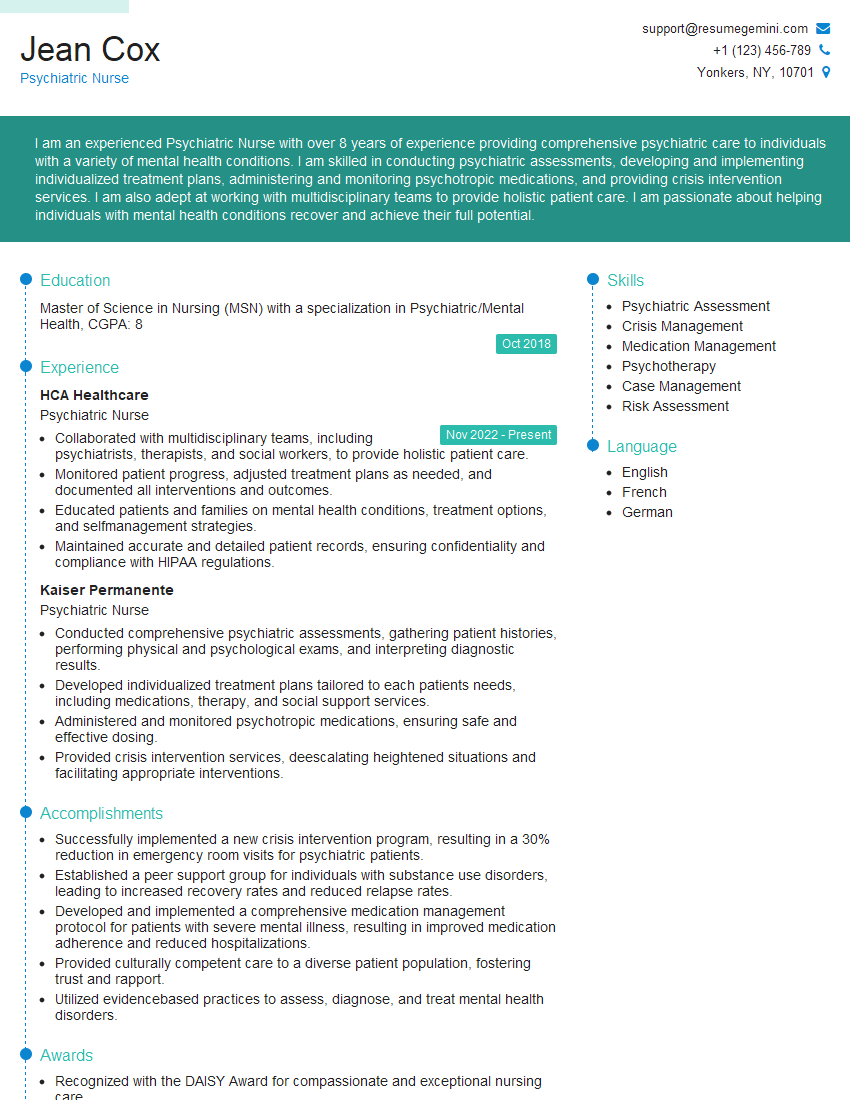
Mastering the ability to provide culturally sensitive and trauma-informed care is crucial for career advancement in today’s diverse healthcare landscape. It demonstrates empathy, competence, and a commitment to ethical practice, significantly enhancing your value as a professional. To maximize your job prospects, focus on building an ATS-friendly resume that showcases these essential skills. ResumeGemini is a trusted resource to help you create a compelling and effective resume that highlights your abilities. Examples of resumes tailored to showcasing expertise in culturally sensitive and trauma-informed care are available on ResumeGemini to guide your efforts. Invest the time to craft a strong resume—it’s a crucial step in securing your ideal role.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.