The right preparation can turn an interview into an opportunity to showcase your expertise. This guide to Achilles Tendon Rupture Repair interview questions is your ultimate resource, providing key insights and tips to help you ace your responses and stand out as a top candidate.
Questions Asked in Achilles Tendon Rupture Repair Interview
Q 1. Describe the different surgical techniques used for Achilles tendon rupture repair.
Several surgical techniques exist for Achilles tendon rupture repair, all aiming to restore the tendon’s integrity and biomechanical function. The choice depends on factors like the rupture’s location, size, and the patient’s overall health and activity level. The most common include:
- End-to-End Repair: This involves directly suturing the torn ends of the tendon back together. It’s suitable for fresh, clean ruptures without significant tendon retraction.
- Augmentation Repair: This technique uses additional material, such as a tendon allograft (donor tendon) or synthetic material, to reinforce the repair. It’s often preferred for larger gaps, older ruptures, or cases where tendon quality is compromised.
- Bunnell Stitch: This is a specific type of suture technique within the end-to-end repair category, utilizing a series of interlocking sutures to create a strong, reliable repair. It is known for its relatively low risk of tendon shortening.
- Modified Kessler Stitch: Another variant of the end-to-end repair, using different suture placement to optimize tendon apposition and reduce the risk of suture pull-through.
Minimally invasive techniques, using smaller incisions and specialized instruments, are also becoming increasingly popular, offering potential benefits like reduced scarring and faster recovery.
Q 2. What are the advantages and disadvantages of each technique?
Each technique has its own set of advantages and disadvantages:
- End-to-End Repair: Advantages include simplicity, relatively shorter surgical time, and less foreign material introduced. Disadvantages include potential for rerupture, especially in larger defects, and difficulty achieving perfect alignment in severely retracted ruptures.
- Augmentation Repair: Advantages include enhanced strength and reduced risk of rerupture, particularly in challenging cases. Disadvantages are slightly increased surgical complexity, the potential for increased inflammation from foreign material (though minimized with modern allografts), and higher cost.
- Bunnell and Kessler Stitches: These benefit from improved suture placement leading to a stronger, more secure repair and reduced risk of early failure. However, these require a surgeon skilled in their application.
The ideal technique is chosen based on individual patient circumstances and surgeon experience, always weighing the potential benefits and risks for a given situation.
Q 3. Explain the principles of proper post-operative management and rehabilitation.
Post-operative management is crucial for successful healing. It involves:
- Immobilization: Initially, the foot is typically immobilized in a cast or splint to protect the repair and prevent movement. The duration varies depending on the technique and the patient’s progress.
- Pain Management: Pain control is essential for patient comfort and compliance with the rehabilitation protocol. This might involve medication, ice therapy, or other modalities.
- Early Range of Motion (ROM): As healing progresses, guided ROM exercises are initiated to prevent stiffness and maintain joint mobility. This should be done under the supervision of a physical therapist. Early controlled ROM is often crucial to reduce the risk of adhesions and stiffness.
- Progressive Weight-bearing: Gradual weight-bearing is initiated according to the surgeon’s and physical therapist’s recommendations, starting with non-weight-bearing, transitioning to partial, and finally to full weight-bearing. This progression prevents overloading the healing tendon.
- Rehabilitation: A comprehensive rehabilitation program is critical for restoring full strength, flexibility, and functional mobility. This typically involves a combination of exercises focused on strengthening the calf muscles, increasing range of motion, and improving proprioception (body awareness).
Close monitoring and compliance with the rehabilitation program are paramount to prevent complications and ensure a successful outcome.
Q 4. How do you assess the healing process of an Achilles tendon repair?
Assessment of the healing process is multi-faceted and includes:
- Clinical Examination: This involves regular physical examinations to assess the patient’s pain, range of motion, strength, and gait. Palpation of the repair site helps to detect tenderness or abnormalities.
- Imaging Studies: Ultrasound or MRI scans can be used to assess tendon healing, identify potential complications, and monitor the repair’s integrity. Ultrasound is generally preferred due to its accessibility and lack of ionizing radiation.
- Functional Tests: These help evaluate the patient’s functional ability, such as hop tests and single-leg stance tests. These objectively measure the patient’s progress towards a full recovery.
A combination of these methods provides a comprehensive picture of the healing process.
Q 5. What are the common complications associated with Achilles tendon rupture repair?
Complications can occur, although with meticulous surgical technique and appropriate post-operative management, they can be minimized. Common complications include:
- Rerupture: This can happen during the early healing phase or later, especially with inadequate rehabilitation or premature return to high-impact activities.
- Wound Infection: This is a serious complication that can delay healing and compromise the repair. Prophylactic antibiotics are often used.
- Surrounding Tissue Adhesions: These can lead to restricted range of motion and pain.
- Delayed or Non-Union: The tendon may fail to heal properly or completely. Surgical revision may be necessary.
- Gastrocnemius Equinus (Heel Cord Tightness): Tightness in the calf muscles can restrict ankle mobility and require specific stretching exercises.
- Complex Regional Pain Syndrome (CRPS): This is a less common but serious complication characterized by chronic pain, swelling, and changes in skin color and temperature.
Proper surgical technique, meticulous patient selection, and careful adherence to the post-operative rehabilitation protocol significantly reduce the risk of these complications.
Q 6. How do you manage complications such as wound infection or rerupture?
Management of complications requires a tailored approach:
- Wound Infection: This necessitates aggressive treatment with antibiotics, wound debridement (removal of infected tissue), and possibly surgical drainage. In severe cases, a secondary operation might be required.
- Rerupture: This typically requires a second surgical repair, often using augmentation techniques to enhance the strength of the repair.
- Adhesions: These can be addressed with physical therapy, including techniques such as manual mobilization and stretching. In recalcitrant cases, surgical intervention may be necessary to release the adhesions.
- Delayed or Non-Union: Often requires revision surgery, which might involve tendon grafting or other advanced techniques.
Early detection and prompt management of complications are crucial to minimize their impact and prevent long-term sequelae.
Q 7. Describe your experience with different types of suture materials and fixation devices.
My experience encompasses a wide range of suture materials and fixation devices. The choice depends on factors like the size of the rupture, the patient’s individual characteristics, and personal preferences. Examples include:
- Suture Materials: I frequently utilize high-strength, biocompatible materials like #2 non-absorbable braided sutures (e.g., Ethibond, Prolene) for the primary repair. Absorbable sutures (e.g., Vicryl) may be used for subcutaneous layers.
- Fixation Devices: I have experience using various techniques such as simple sutures, modified Kessler sutures, Krackow stitches, and occasionally percutaneous transosseous fixation with small screws, particularly in challenging cases. The use of devices is carefully considered based on the anatomy and the size of the defect.
The selection of the material and device is always driven by a desire to optimize the chances of a robust and successful repair, while also considering the balance between strength and the risk of adverse reactions.
Q 8. How do you determine the appropriate timing for return to sports activities?
Determining the appropriate time for a patient to return to sports after Achilles tendon rupture repair is crucial and depends on several factors. It’s not a one-size-fits-all answer; we individualize it based on the patient’s healing progress, strength, and functional capacity.
We typically follow a phased approach. Initially, the focus is on pain management and achieving full range of motion. Then we progress to strengthening exercises, focusing on the gastrocnemius and soleus muscles – the muscles that work the Achilles tendon. The patient will gradually increase the intensity and duration of exercise, progressing from simple calf raises to more dynamic activities like hopping and jumping. We use objective measures, such as isokinetic dynamometry (measuring muscle strength) and functional tests like single-leg hops, to track their progress.
A patient might be cleared for low-impact activities, such as swimming or cycling, much earlier than high-impact activities. Full return to sports, especially high-impact sports like basketball or tennis, usually takes 6-9 months, or even longer, ensuring that tendon strength is sufficient to prevent re-rupture. Throughout this process, we carefully monitor the patient for any signs of pain or weakness, adjusting the rehabilitation program accordingly.
Imagine a marathon runner; their return to running will be a much slower, more gradual process than someone who plays recreational tennis. Every patient has a unique timeline.
Q 9. What are the indications for surgical versus non-surgical management?
The decision between surgical and non-surgical management for an Achilles tendon rupture depends primarily on the extent of the rupture, the patient’s activity level, and their personal preferences.
- Non-surgical management (also known as conservative management) is often considered for patients with smaller partial tears or for individuals with low activity levels who are comfortable with a longer recovery period. This typically involves immobilization in a cast or boot followed by a rigorous physiotherapy program.
- Surgical repair is usually the preferred option for complete ruptures, particularly in active individuals who need to return to high-impact activities quickly. Surgery involves reattaching the torn tendon ends using sutures. This method offers the potential for faster healing and a lower risk of re-rupture in high-demand individuals.
We carefully weigh the risks and benefits of both approaches with each patient, considering factors such as age, occupation, and overall health. Sometimes, the gap between the tendon ends influences the surgical decision; larger gaps might necessitate a surgical approach to achieve optimal healing.
Q 10. How do you counsel patients on realistic expectations regarding recovery time?
Counseling patients about realistic expectations is vital. I always emphasize that recovery from an Achilles tendon rupture is a gradual process, not a race. I explain that even with surgery, complete recovery can take several months, and full return to pre-injury activity levels often takes longer.
I use visual aids, such as timelines and progress charts, to help patients visualize the recovery journey. I share examples of other patients’ experiences, emphasizing both the challenges and successes. Open communication is key. I encourage patients to share their concerns and to ask questions throughout the recovery period. We set realistic, achievable short-term goals to maintain motivation. For instance, rather than focusing on ‘return to basketball,’ we focus first on achieving full range of motion, then regaining strength, and only then consider sports-specific activities.
Managing expectations means being transparent about potential complications such as re-rupture, stiffness, or persistent pain. This honesty fosters trust and enables the patient to actively participate in their healing process. It also avoids disappointment later on.
Q 11. Explain the role of physiotherapy in Achilles tendon rupture rehabilitation.
Physiotherapy plays a critical role in the rehabilitation of Achilles tendon ruptures, regardless of whether the injury is treated surgically or conservatively. The physiotherapist’s role is to guide the patient through a structured program designed to restore function and strength.
The program typically starts with range-of-motion exercises, focusing on ankle and foot mobility, followed by gradual strengthening exercises. This progression involves moving from isometric exercises (contracting the muscle without movement) to isotonic exercises (contracting the muscle through a range of motion). The therapist will often use modalities such as ultrasound or electrical stimulation to help manage pain and inflammation.
As the patient progresses, the physiotherapy program incorporates balance exercises and proprioceptive training (improving awareness of the body’s position in space). This is extremely important for preventing re-injury and improving stability. Finally, the program culminates in sports-specific training to help the patient safely return to their chosen activities. The role of the physiotherapist extends beyond just exercises; it involves educating the patient on proper footwear, biomechanics, and activity modification to support long-term healing and prevent re-injury.
Q 12. What are the key elements of a successful patient education program?
A successful patient education program for Achilles tendon rupture repair is multifaceted. It starts from the very first consultation.
- Clear and concise explanations: We explain the injury, treatment options, and the recovery process using simple language and visuals. Avoid medical jargon.
- Realistic expectations: As mentioned earlier, setting realistic expectations is crucial. Emphasize the length of the recovery process and the importance of adherence to the rehabilitation plan.
- Active involvement: Patients should feel empowered to ask questions and participate in their treatment decisions. We encourage them to track their progress and to communicate any concerns immediately.
- Practical advice: This includes advice on footwear, activity modifications, and preventative measures to reduce the risk of re-injury.
- Follow-up care: Regular follow-up appointments are essential to monitor progress, address any issues, and adjust the treatment plan as needed.
A well-designed brochure or online resources can further enhance the educational aspect of the program, providing consistent and accessible information for the patient throughout their journey.
Q 13. Discuss the role of imaging (e.g., ultrasound, MRI) in diagnosing and monitoring Achilles tendon ruptures.
Imaging plays a vital role in both diagnosing and monitoring Achilles tendon ruptures.
- Ultrasound is often the initial imaging modality used because it’s readily available, relatively inexpensive, and provides real-time images. Ultrasound can clearly show the tendon’s structure, helping to identify the presence, location, and extent of a tear.
- MRI (Magnetic Resonance Imaging) offers higher resolution and provides more detailed images of the soft tissues, including the tendon and surrounding structures. It’s particularly helpful for differentiating between partial and complete tears, assessing the extent of the injury, and identifying any associated complications.
During the healing process, follow-up imaging (usually ultrasound) helps us monitor the tendon’s repair and assess its structural integrity. It allows us to determine when the patient can progress to the next stage of rehabilitation, such as weight-bearing or sports-specific activities. Serial imaging, at regular intervals, provides visual evidence of how healing is progressing.
Q 14. How do you differentiate between a partial and complete Achilles tendon rupture?
Differentiating between a partial and complete Achilles tendon rupture is crucial for determining the appropriate management strategy.
A partial rupture involves a tear in only part of the tendon, leaving some intact fibers. Patients with partial tears often experience pain and some functional impairment but still retain some ability to plantarflex (point their foot downward). The symptoms are generally milder compared to a complete rupture.
A complete rupture is a complete tear through the entire width of the tendon. This results in a noticeable gap or defect in the tendon, and patients usually experience significant pain, swelling, and an inability to plantarflex the foot. There may also be a palpable defect (a visible or felt gap) in the tendon. Clinical examination, along with imaging studies (ultrasound or MRI), are usually sufficient to confirm the diagnosis.
Imagine a rope; a partial tear is like fraying at one end, while a complete rupture is like the rope snapping entirely.
Q 15. What are the specific considerations for managing an Achilles tendon rupture in a high-level athlete?
Managing an Achilles tendon rupture in a high-level athlete requires a highly individualized approach prioritizing a rapid, safe return to sport. The primary goal is not just healing the tendon, but restoring pre-injury strength, power, and agility. This necessitates a multidisciplinary team involving surgeons, physiotherapists, and athletic trainers.
Early surgical intervention is often favored, minimizing prolonged immobilization and potentially improving functional outcomes. The surgical technique itself may be modified based on the athlete’s specific sport and demands – a basketball player will have different demands than a long-distance runner.
Post-operative rehabilitation is meticulously planned and aggressively pursued. It progresses through phases, starting with controlled range of motion and progressing to eccentric strengthening exercises crucial for functional recovery. Regular monitoring, often including advanced imaging like ultrasound, helps track healing progress and guide rehabilitation intensity. The return-to-sport protocol is carefully tailored to the athlete’s sport-specific demands and physiological readiness, which may involve biomechanical analysis and gradual reintegration into training. A premature return can lead to re-rupture, therefore a cautious and individualized approach is paramount.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you handle patients with comorbidities (e.g., diabetes, peripheral vascular disease)?
Patients with comorbidities like diabetes or peripheral vascular disease present unique challenges in Achilles tendon rupture management. These conditions can impair healing and increase the risk of complications. Careful preoperative assessment is crucial, evaluating blood sugar control in diabetics and vascular status in patients with PVD.
Diabetes can delay tendon healing due to impaired blood supply and increased risk of infection. Strict glycemic control before and after surgery is essential. We may opt for prophylactic antibiotics to minimize infection risk.
Peripheral vascular disease further compromises blood supply to the tendon, potentially hindering healing. Non-invasive vascular studies may be necessary to assess perfusion and identify areas of compromise. Surgical techniques minimizing tissue trauma are preferred. We may use growth factors or other adjunctive therapies to enhance healing in these patients. Post-operative monitoring is intensified, closely watching for signs of infection or impaired healing. Close collaboration with specialists like endocrinologists and vascular surgeons is crucial for optimal patient management.
Q 17. Describe your experience with minimally invasive surgical techniques for Achilles tendon repair.
I have extensive experience with minimally invasive surgical techniques for Achilles tendon repair, including percutaneous repair and mini-open techniques. These methods offer several advantages over traditional open surgery, including smaller incisions, less tissue trauma, reduced post-operative pain, and faster recovery times.
Percutaneous repair involves using specialized instruments to repair the tendon through small incisions. This technique is particularly suitable for patients with uncomplicated ruptures.
Mini-open techniques involve a slightly larger incision than percutaneous repairs but allow for better visualization and more precise repair, particularly beneficial for complex ruptures or those with significant retraction. My preference for a technique is determined by the individual patient’s anatomy and the specifics of their rupture. Careful surgical planning, precise instrument selection, and meticulous surgical execution are vital for success with both techniques.
Q 18. What are the latest advancements in Achilles tendon rupture repair?
Recent advancements in Achilles tendon rupture repair focus on improving healing and functional outcomes. This includes the development of novel biomaterials and regenerative medicine approaches.
Bioabsorbable implants offer the potential to reduce the need for secondary surgery for implant removal.
Growth factors and stem cell therapies are being explored to accelerate tendon healing and improve tissue quality. There’s ongoing research into optimizing surgical techniques, such as the use of advanced imaging to guide the procedure and ensure precise repair. The field is continuously evolving, and staying abreast of the latest research and clinical trials is crucial for providing the best possible patient care.
Q 19. What are your preferred methods for pain management post-operatively?
My approach to post-operative pain management is multimodal and patient-centered. It focuses on minimizing pain while promoting early mobilization and rehabilitation.
Pharmacological pain management often includes a combination of non-steroidal anti-inflammatory drugs (NSAIDs) and opioids, tailored to the individual patient’s needs and pain tolerance. The use of opioids is carefully monitored due to the risks of addiction and side effects.
Non-pharmacological strategies such as ice, elevation, and physical therapy are crucial in managing pain and reducing inflammation. Nerve blocks or other regional anesthetic techniques may be utilized for optimal pain control during the initial post-operative period. The goal is to provide effective pain relief while minimizing reliance on strong opioids and allowing for prompt initiation of rehabilitation.
Q 20. How do you assess patient satisfaction with their outcome after surgery?
Assessing patient satisfaction is an integral part of my practice. I use a combination of methods to evaluate outcomes and capture the patient’s perspective.
Functional outcome scores such as the American Orthopaedic Foot and Ankle Society (AOFAS) score provide objective measures of ankle function.
Patient-reported outcome measures (PROMs) such as questionnaires assessing pain, function, and quality of life give valuable insights into the patient’s experience.
Direct patient interviews are crucial for understanding individual challenges and concerns. These assessments are made at multiple points during the post-operative period – at regular intervals following surgery and at long-term follow up. This comprehensive approach helps identify areas for improvement and ensures patients are receiving the best possible care.
Q 21. What are your criteria for considering a surgical revision?
Criteria for considering a surgical revision after Achilles tendon rupture repair include persistent pain, significant functional limitations, and evidence of re-rupture or failed healing.
Persistent pain despite appropriate conservative management warrants further investigation.
Significant functional limitations that hinder activities of daily living or prevent return to desired functional levels may indicate the need for revision surgery.
Imaging findings such as ultrasound or MRI showing re-rupture or evidence of failed healing are strong indicators for revision surgery. The decision for revision surgery is made on a case-by-case basis, carefully weighing the potential benefits against the risks of further surgery. A thorough evaluation considering both objective and subjective findings is paramount.
Q 22. How do you manage a patient with delayed wound healing?
Delayed wound healing after Achilles tendon repair is a significant concern, potentially leading to infection, tendon re-rupture, or prolonged recovery. Management requires a multi-pronged approach focusing on identifying and addressing underlying causes.
- Thorough Examination: We start with a detailed assessment, looking for signs of infection (redness, swelling, pus), insufficient blood supply, or foreign body reaction. Imaging studies like ultrasound may be necessary to rule out hematoma or seroma formation.
- Optimize Systemic Factors: Underlying conditions like diabetes, smoking, or malnutrition significantly impair healing. We work with the patient and other specialists to optimize these factors. This might involve blood glucose control, smoking cessation support, and nutritional counseling.
- Wound Care: Meticulous wound care is crucial. This includes regular cleaning with appropriate antiseptic solutions, appropriate dressing changes to promote a moist wound environment and debridement of necrotic tissue if present. We may utilize negative pressure wound therapy in severe cases.
- Surgical Intervention: If there’s significant infection or non-healing, surgical debridement might be necessary to remove infected tissue. In rare cases, skin grafting may be required to close the wound effectively.
- Growth Factors and Medications: Topical growth factors or oral medications to promote healing may be considered. This is often used in conjunction with other measures, not as a standalone solution.
For example, I recently managed a patient with delayed healing due to poorly controlled diabetes. By optimizing his blood sugar levels and implementing intensive wound care, we were able to successfully promote healing and avoid surgical intervention.
Q 23. What is your experience with using platelet-rich plasma (PRP) or other regenerative medicine techniques?
Platelet-rich plasma (PRP) and other regenerative medicine techniques are increasingly used in Achilles tendon repair, though their effectiveness remains a topic of ongoing research and debate. My experience involves using PRP in carefully selected patients, mainly those with partial-thickness tears or those showing signs of delayed healing.
The procedure involves drawing the patient’s blood, centrifuging it to concentrate platelets, and then injecting the PRP directly into the injured tendon. I’ve found it to be most beneficial when used in conjunction with other standard surgical techniques, such as tendon repair or debridement. It’s important to manage patient expectations, as PRP is not a magical cure-all. There’s no guarantee of improved outcomes, and rigorous studies on long-term efficacy are still lacking.
Other regenerative techniques, such as stem cell therapy, are also being investigated. However, currently, the evidence base supporting their routine use in Achilles tendon repair is limited. The focus remains on established surgical techniques and optimizing post-operative care.
Q 24. Describe your approach to managing a patient who presents with a recurrent rupture.
A recurrent rupture after Achilles tendon repair is a challenging situation, often requiring a more aggressive surgical approach. My approach emphasizes a thorough evaluation to understand the cause of the re-rupture.
- Detailed History and Physical Exam: We meticulously review the patient’s history, focusing on the initial injury, the surgical technique used, and any post-operative complications. A comprehensive physical exam helps assess the extent of the re-rupture and any associated pathology.
- Imaging Studies: MRI is crucial to accurately assess the extent of the re-rupture, identify any scar tissue or other abnormalities that may have contributed to the failure, and guide surgical planning.
- Surgical Options: The surgical approach depends on the findings. Options include revision repair, using stronger sutures and possibly augmentation techniques such as allograft augmentation, or even tendon transfer procedures in cases of extensive tissue loss.
- Rehabilitation: A strict and modified post-operative rehabilitation program is critical to prevent further ruptures. This often involves a longer period of immobilization and a more gradual return to activity.
For instance, a patient with a re-rupture due to inadequate initial repair might require a stronger reconstruction using a different surgical technique, potentially with allograft augmentation to reinforce the tendon.
Q 25. Explain the biomechanics of the Achilles tendon and how this relates to rupture.
The Achilles tendon is a powerful structure responsible for plantarflexion of the ankle. Its biomechanics are crucial to understanding ruptures. The tendon is subjected to high tensile loads, especially during activities like jumping and sprinting. Factors such as the angle of insertion, tendon thickness, and muscle-tendon unit stiffness all play a role.
Ruptures typically occur in the watershed area, a region with reduced vascularity, making it more susceptible to injury. A combination of intrinsic factors (age-related degeneration, collagen abnormalities) and extrinsic factors (sudden forceful contraction, pre-existing tendinopathy) contributes to the rupture. The sudden, forceful contraction frequently exceeds the tendon’s tensile strength, causing a rupture, often at the myotendinous junction or within the paratenon. Understanding these biomechanical principles guides surgical planning and rehabilitation strategies.
Q 26. How do you assess the functional outcome of Achilles tendon repair?
Assessing the functional outcome of Achilles tendon repair involves a multi-faceted approach, combining clinical evaluation with standardized outcome measures.
- Clinical Assessment: This includes assessing range of motion, strength, gait analysis, and the presence of any pain or residual symptoms.
- Functional Scores: Standardized questionnaires such as the American Orthopaedic Foot and Ankle Society (AOFAS) Ankle-Hindfoot scale and the visual analog scale (VAS) for pain are used to quantify functional status and pain levels. These provide objective data to track recovery progress.
- Objective Measures: Isometric strength testing, and measurements of plantarflexion strength and speed can help objectively assess the recovery of muscle strength and function.
- Imaging: Ultrasound and MRI scans can be used to assess tendon healing and integrity, although these are often less frequently used in assessing functional outcomes.
A comprehensive approach combining clinical assessment and standardized outcome measures provides a more accurate and complete picture of the patient’s functional recovery following Achilles tendon repair.
Q 27. What are the potential long-term complications of Achilles tendon rupture?
Long-term complications after Achilles tendon rupture repair can impact a patient’s quality of life and functional ability. These include:
- Re-rupture: This is a significant concern and can occur even with successful initial repair. Factors like inadequate healing, insufficient rehabilitation, and underlying tendon pathology contribute to this risk.
- Stiffness and Limited Range of Motion: Scar tissue formation can limit ankle flexibility and mobility, affecting activities of daily living.
- Persistent Pain: Some patients experience persistent pain, even after the tendon has healed. This can be caused by nerve entrapment, tendinopathy, or other factors.
- Rupture of the opposite tendon: This is a risk, especially during early return to high-impact sports and activities, if rehabilitation was inadequate.
- Plantar fasciitis and other related issues: Because of biomechanical changes and compensatory mechanisms, other foot issues may arise as a complication.
- Arthritis: In some instances, long term changes in the joint can occur leading to arthritis.
It’s vital to emphasize the importance of thorough rehabilitation and adherence to post-operative instructions to minimize these risks. Regular follow-up appointments are also crucial for early detection and management of potential complications.
Q 28. How do you stay up-to-date with the latest research and advancements in Achilles tendon repair?
Staying current with the latest research and advancements in Achilles tendon repair involves continuous learning and engagement with the field.
- Professional Societies and Conferences: Active membership in professional organizations like the American Academy of Orthopaedic Surgeons (AAOS) provides access to journals, conferences, and continuing medical education (CME) opportunities. Attending national and international conferences allows for direct engagement with experts and the latest research.
- Peer-Reviewed Journals: Regularly reviewing leading orthopedic journals, such as the Journal of Bone and Joint Surgery, allows for staying updated on the latest findings in surgical techniques, rehabilitation protocols, and the management of complications.
- Online Resources: Reputable online resources and databases (PubMed, Google Scholar) enable me to access research articles, review studies, and access online courses related to current best practice.
- Collaboration and Mentorship: Discussing complex cases with colleagues and mentors, whether through journal clubs, conferences, or in-house discussions, provides valuable insights.
This multi-faceted approach ensures that my practice remains aligned with the latest evidence-based guidelines and best practices in Achilles tendon repair.
Key Topics to Learn for Achilles Tendon Rupture Repair Interview
- Anatomy and Physiology: Deep understanding of the Achilles tendon, its surrounding structures, and biomechanics.
- Diagnosis: Mastering physical examination techniques, interpreting imaging (ultrasound, MRI), and recognizing clinical presentations.
- Surgical Techniques: Familiarity with various surgical approaches (e.g., open repair, minimally invasive techniques), including advantages and disadvantages of each.
- Post-operative Management: Comprehensive knowledge of rehabilitation protocols, including weight-bearing restrictions, physiotherapy, and potential complications.
- Complications and Management: Understanding common complications (e.g., re-rupture, infection, sural nerve injury) and strategies for their prevention and management.
- Evidence-Based Practice: Ability to critically appraise relevant literature and apply research findings to clinical decision-making.
- Patient Communication and Counseling: Skills in effectively communicating with patients, addressing concerns, and managing expectations.
- Ethical Considerations: Understanding the ethical implications of treatment decisions and informed consent.
- Problem-Solving: Ability to analyze complex cases, identify potential challenges, and devise appropriate solutions.
- Current Trends and Research: Staying updated on the latest advancements in surgical techniques, rehabilitation strategies, and research findings.
Next Steps
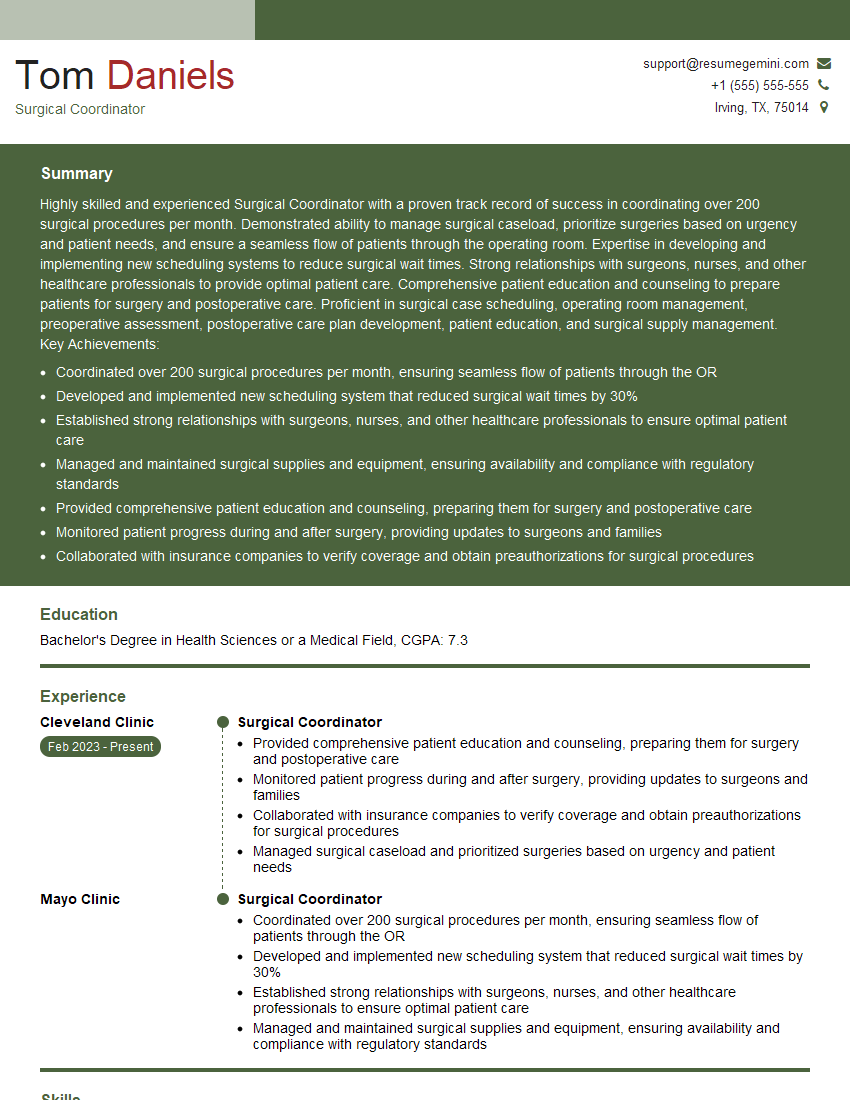
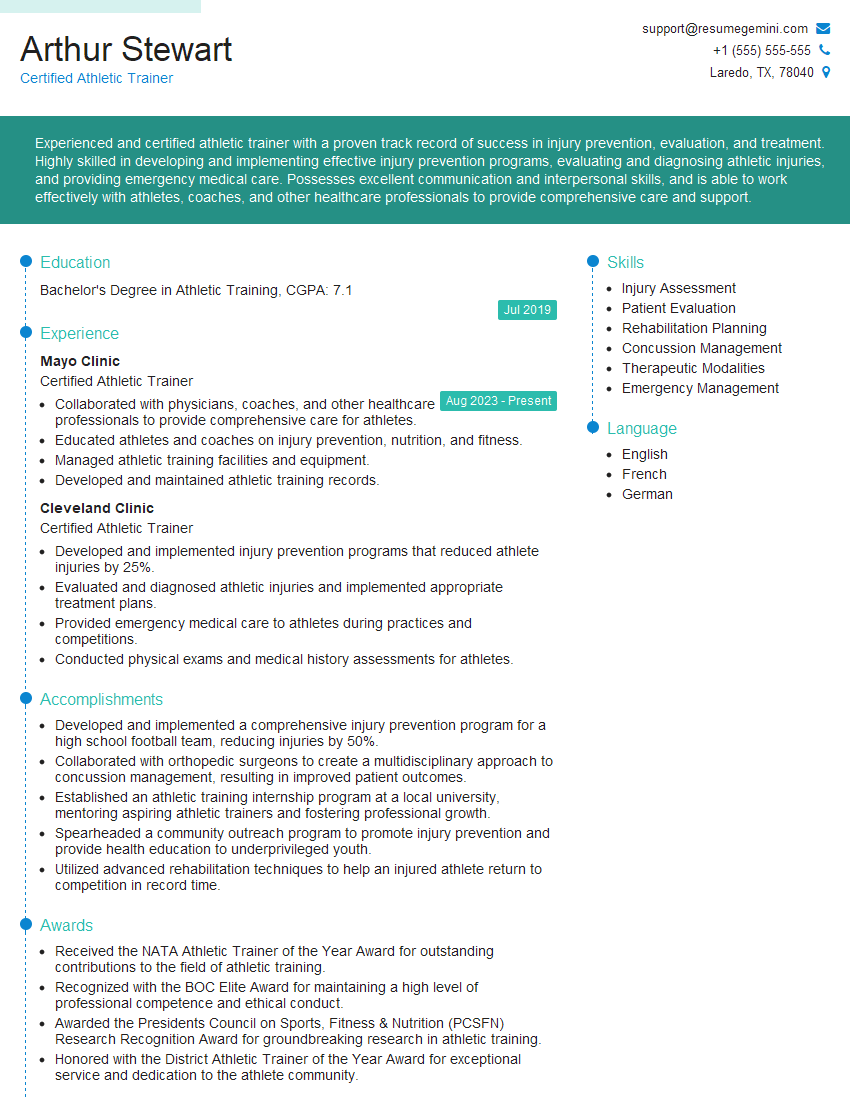
Mastering Achilles tendon rupture repair positions you for significant career advancement in orthopedics and sports medicine. A strong foundation in this area demonstrates expertise and commitment to patient care. To enhance your job prospects, it’s crucial to create an ATS-friendly resume that effectively highlights your skills and experience. ResumeGemini is a trusted resource to help you build a professional and impactful resume. Examples of resumes tailored to Achilles Tendon Rupture Repair are available to guide you, showcasing how to present your qualifications effectively. Invest in your career future – build a winning resume today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.