Are you ready to stand out in your next interview? Understanding and preparing for Aerosol Therapy Management interview questions is a game-changer. In this blog, we’ve compiled key questions and expert advice to help you showcase your skills with confidence and precision. Let’s get started on your journey to acing the interview.
Questions Asked in Aerosol Therapy Management Interview
Q 1. Explain the different types of aerosol delivery devices and their mechanisms.
Aerosol delivery devices aim to get medication deep into the lungs. Several types exist, each with a unique mechanism:
- Metered-Dose Inhalers (MDIs): These use a propellant to deliver a measured dose of medication as a fine mist. The patient coordinates actuation with inhalation. They often require a spacer to improve drug deposition in the lungs.
- Dry Powder Inhalers (DPIs): These contain a dry powder medication. Inhalation by the patient creates an airflow that disperses the powder into the lungs. They don’t require coordination with actuation but rely on sufficient inspiratory flow.
- Nebulizers: These devices use compressed air or ultrasonic vibrations to turn liquid medication into a fine mist that the patient inhales. Nebulizers are suitable for patients with difficulty coordinating inhalation with actuation, such as young children or those with severe respiratory compromise.
- Soft Mist Inhalers (SMIs): These are relatively new devices that deliver medication as a soft mist without the use of propellants. This design may be easier to use than MDIs and allows for better coordination of actuation and inhalation.
Each device’s mechanism ensures that the medication reaches the target area of the respiratory tract, optimizing therapeutic effect.
Q 2. Describe the advantages and disadvantages of using different aerosol delivery systems (e.g., MDI, DPI, nebulizers).
The choice of aerosol delivery system depends on individual patient needs. Let’s compare:
- MDIs:
- Advantages: Portable, relatively inexpensive, various medications available.
- Disadvantages: Requires good hand-breath coordination, propellant may irritate the lungs, potential for medication wastage.
- DPIs:
- Advantages: No propellant, generally easier to use than MDIs, less reliance on hand-breath coordination.
- Disadvantages: Can be more expensive, requires a sufficient inspiratory flow (can be challenging for some patients), may not be suitable for all medications.
- Nebulizers:
- Advantages: Suitable for patients with poor coordination, delivers medication quickly, suitable for a wide range of medications.
- Disadvantages: Less portable, time-consuming treatment, potential for contamination, some medications may not be suitable for nebulization.
For example, a young child with asthma might benefit from a nebulizer due to the ease of use. An older adult with good coordination might prefer an MDI with a spacer. A patient with COPD might use a DPI for its convenience.
Q 3. How do you assess a patient’s suitability for different aerosol therapy devices?
Assessing patient suitability involves considering several factors:
- Respiratory Function: Peak expiratory flow (PEF) measurements, spirometry, and oxygen saturation help determine the severity of respiratory impairment, guiding device choice.
- Coordination Ability: Observing the patient’s ability to use an inhaler, including hand-breath coordination for MDIs, is crucial. Patients with poor coordination may require nebulizers or DPIs.
- Cognitive Ability: Understanding and following instructions are key to effective inhaler use. Patients with cognitive impairment may require assistance or simpler devices.
- Medication Properties: Some medications are available in different inhaler types. Factors such as particle size and drug stability dictate which device is appropriate.
- Patient Preferences: Patient preferences and willingness to learn the appropriate technique are essential for adherence.
For instance, a patient with severe COPD and limited inspiratory effort may require a nebulizer, while a patient with mild asthma and good coordination may benefit from an MDI with a spacer.
Q 4. What are the common complications associated with aerosol therapy, and how are they managed?
Complications from aerosol therapy are rare but can occur:
- Oral Thrush (candidiasis): This fungal infection can develop in the mouth and throat, especially with inhaled corticosteroids. Good oral hygiene and rinsing the mouth after use can help prevent it. Treatment involves antifungal medications.
- Dysphonia (hoarseness): Corticosteroids can cause irritation of the vocal cords. Using a spacer and rinsing the mouth can help mitigate this.
- Bronchospasm (Paradoxically): In some cases, inhaled bronchodilators can trigger bronchospasm. This is often related to the medication itself, not the delivery method. This should be managed by promptly initiating appropriate treatment.
- Systemic Effects: High doses or improper use can lead to systemic side effects, such as increased blood sugar or adrenal suppression. Careful medication titration is crucial.
Managing complications requires careful monitoring, prompt identification of symptoms, and appropriate treatment tailored to the specific issue. Patient education on proper inhaler technique and potential side effects is key to preventing complications.
Q 5. Describe the process of medication reconciliation in the context of aerosol therapy.
Medication reconciliation in aerosol therapy involves a systematic process to ensure the patient receives the correct medications via the appropriate delivery device.
- Collect Medication Information: Gather a complete list of all medications the patient is currently taking, including over-the-counter medications, supplements, and herbal remedies.
- Verify Prescriptions: Confirm that the prescribed aerosol medications and dosages are accurate and consistent with the patient’s needs.
- Assess Device Suitability: Ensure the prescribed delivery device is appropriate for the patient’s abilities and condition, and that the patient understands how to use it correctly.
- Check for Drug Interactions: Review for potential interactions between the aerosol medications and other medications the patient is taking.
- Document Findings: Maintain a comprehensive record of all medications, devices, and any identified issues or concerns.
This process minimizes medication errors and ensures the safe and effective use of aerosol therapy.
Q 6. How do you educate patients on proper inhaler technique?
Educating patients on inhaler technique is crucial for effective therapy. A step-by-step approach is essential:
- Demonstrate and Explain: Use a visual aid to show the correct technique, explaining each step clearly and simply.
- Practice: Have the patient practice using the inhaler with close supervision, correcting any errors.
- Feedback and Reinforcement: Provide positive reinforcement and constructive feedback, addressing any difficulties the patient is experiencing.
- Written Instructions: Provide written instructions that reinforce the verbal explanations and diagrams.
- Follow-Up: Schedule follow-up appointments to monitor the patient’s progress and address any remaining questions or concerns.
For example, when teaching MDI use, emphasize the importance of coordinating actuation with inhalation and the use of a spacer.
Q 7. Explain the role of peak flow monitoring in managing aerosol therapy.
Peak flow monitoring plays a vital role in managing aerosol therapy, particularly for patients with asthma or COPD.
- Assessing Lung Function: PEF measurements provide an objective assessment of lung function, allowing for early detection of worsening respiratory status.
- Guiding Treatment Decisions: Changes in PEF readings can indicate the need for adjustments in medication or treatment plans.
- Monitoring Response to Therapy: Regular PEF monitoring helps evaluate the effectiveness of aerosol therapy and ensures that the patient is responding appropriately.
- Patient Education and Empowerment: Teaching patients how to perform PEF monitoring empowers them to actively participate in their own care and identify potential problems early.
A significant drop in PEF readings might indicate an exacerbation of the condition and the need for immediate medical attention. Conversely, a consistent improvement in PEF readings suggests effective management.
Q 8. How do you monitor and evaluate the effectiveness of aerosol therapy?
Monitoring the effectiveness of aerosol therapy is crucial to ensure the treatment is achieving its intended goals. We assess effectiveness through a combination of methods focusing on both subjective and objective measures. Subjectively, we rely on the patient’s reported symptom improvement – for example, reduced cough frequency, improved breathing ease, or less shortness of breath. Objectively, we may use various tools like spirometry (measuring lung function) to quantify changes in lung capacity and flow rates. Peak expiratory flow (PEF) monitoring can be used to track changes in airflow, especially for patients with asthma. Pulse oximetry, measuring blood oxygen saturation, helps determine if the treatment is improving oxygen levels. Chest auscultation, listening to lung sounds with a stethoscope, can reveal improvements in wheezing or crackles. Finally, regular clinical examinations and reviewing imaging such as chest X-rays can aid in assessing overall respiratory health and response to treatment. The choice of monitoring method depends heavily on the patient’s specific condition and the goals of therapy. For instance, a child with cystic fibrosis may require more frequent spirometry assessments compared to an adult with a mild case of bronchitis.
Q 9. What are the key considerations for aerosol therapy in pediatric and geriatric populations?
Aerosol therapy in pediatrics and geriatrics requires careful consideration due to age-related physiological differences. In pediatrics, smaller airways and a higher risk of bronchospasm necessitate the use of smaller doses and specialized delivery devices such as a soft mist nebulizer or spacer with a metered-dose inhaler (MDI). We must also prioritize age-appropriate communication strategies, perhaps involving playful approaches to make the treatment less intimidating. In geriatrics, age-related decline in lung function, decreased coordination, and potential cognitive impairments need careful consideration. We might utilize larger-volume nebulizers with slower delivery to make it easier for them to manage. Additionally, clear, simple instructions and potential assistance with medication administration are vital. Common issues like medication side effects (e.g., tremors from albuterol) must be closely monitored and managed. Moreover, the co-morbidities common in the elderly, like cardiac disease, need careful consideration when choosing the treatment regimen.
Q 10. Discuss the importance of hygiene and infection control in aerosol therapy administration.
Hygiene and infection control are paramount in aerosol therapy to prevent the spread of pathogens. Aerosol treatments create a humid environment that can harbor bacteria and fungi, potentially leading to nosocomial (hospital-acquired) infections. We must adhere to strict protocols including meticulous hand hygiene before and after administration. Using sterile equipment and solutions is mandatory; any reusable equipment must be thoroughly cleaned and disinfected according to manufacturer recommendations. Single-use components, whenever possible, should be employed to minimize contamination. The treatment area should also be cleaned and disinfected, especially after treating patients with known or suspected infections. Appropriate personal protective equipment (PPE), including gloves and masks, should always be used by healthcare professionals to protect both themselves and patients. Regular monitoring of the cleanliness of equipment and adherence to infection control guidelines are crucial for minimizing the risk of infection.
Q 11. How do you manage adverse effects related to aerosol therapy?
Adverse effects of aerosol therapy can range from mild to severe and often depend on the medication administered and the patient’s underlying condition. Common side effects include cough, throat irritation, and oral thrush (candidiasis) with some medications. More serious reactions like bronchospasm, paradoxical bronchoconstriction (worsening of airway narrowing), or hypersensitivity reactions (allergic responses) require immediate intervention. Management depends on the specific reaction. For mild side effects, simple measures like reducing the medication dose, using a spacer, or rinsing the mouth after treatment may suffice. More serious reactions require immediate discontinuation of the medication, administration of appropriate countermeasures (e.g., bronchodilators for bronchospasm), and, if necessary, transferring the patient to a higher level of care. Careful monitoring of the patient’s response to treatment and close communication with the physician are essential. For example, if a patient experiences significant tremors after albuterol administration, the dose may need to be adjusted or an alternative medication considered.
Q 12. What are the legal and ethical considerations related to aerosol therapy?
Legal and ethical considerations in aerosol therapy revolve around informed consent, patient privacy, and safe medication practices. Patients or their legal guardians must be fully informed about the treatment, including its benefits, risks, and alternatives. Written consent is usually required before administering any medication. Maintaining patient confidentiality is crucial, adhering strictly to HIPAA (Health Insurance Portability and Accountability Act) regulations in the US, and equivalent legislation elsewhere. Accurate record-keeping is not only an ethical responsibility but often a legal requirement. Moreover, healthcare providers must adhere to the legal requirements related to medication storage, handling, and disposal, as well as ensuring appropriate qualifications and certifications for administering treatments. Failing to adhere to these standards can lead to legal repercussions, including malpractice lawsuits and disciplinary actions.
Q 13. Explain the importance of documentation in aerosol therapy management.
Thorough documentation is critical in aerosol therapy for several reasons. It serves as a legal record of the treatment provided, protects the healthcare provider from liability, and ensures continuity of care. Documentation should include the patient’s identification details, the type of medication administered, the dose, the method of administration (e.g., nebulizer type), the duration of treatment, the patient’s response to the treatment, any adverse effects observed, and the date and time of administration. Accurate documentation allows for effective tracking of treatment efficacy and helps in identifying potential problems or trends. It also facilitates communication between healthcare professionals involved in the patient’s care. In the event of a legal dispute, comprehensive documentation plays a crucial role in protecting both the patient and healthcare provider. For example, documenting a patient’s worsening respiratory symptoms after an aerosol treatment allows for timely intervention and informs future treatment decisions.
Q 14. Describe different types of nebulizers and their applications.
Several types of nebulizers exist, each with its own advantages and disadvantages. Jet nebulizers use compressed air or oxygen to create a mist, offering consistent aerosol output but being relatively large and noisy. They are suitable for various medications and are often used in hospital settings. Ultrasonic nebulizers use high-frequency vibrations to produce a mist, being quieter than jet nebulizers but potentially degrading some medications. They are often used for home treatment. Mesh nebulizers employ a mesh membrane to atomize the medication, producing a fine mist with efficient drug delivery. They are portable and quieter than other options, offering convenience, particularly for home use. Each type has specific application depending on factors like medication compatibility, the patient’s age and mobility, and the setting of administration. For example, a jet nebulizer might be preferred for a hospitalized patient needing a continuous treatment, while a mesh nebulizer might be more convenient for a patient needing treatment at home. The selection is determined by multiple factors to ensure optimal medication delivery and patient comfort.
Q 15. Discuss the principles of administering dry powder inhalers.
Dry powder inhalers (DPIs) deliver medication as a fine powder directly into the lungs. The principle lies in the patient’s inspiratory effort, which draws the medication from the inhaler. Unlike metered-dose inhalers (MDIs), DPIs don’t require coordination with an actuation button.
- Inhalation Technique: The patient takes a deep breath, creating a flow of air that activates the DPI and disperses the powder. Proper technique is crucial for effective drug delivery. Poor inhalation can leave much of the medicine unused in the inhaler.
- Device Design: DPIs use various mechanisms to release the powder, such as blister packs, multi-dose reservoirs, or single-dose units. Each inhaler has its unique instructions. It’s critical for healthcare professionals to show the patient exactly how to use their particular inhaler.
- Particle Size: The size of the medication particles is engineered to reach the deeper airways effectively. Larger particles tend to deposit in the upper respiratory tract, reducing therapeutic efficacy.
Example: Imagine blowing through a straw to clear a blockage. The force of your breath is analogous to the patient’s inhalation, delivering the medication deep into the lungs. In this example, the blockage is the airway constriction that the medication addresses.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you troubleshoot common problems encountered with MDIs and spacers?
Troubleshooting MDIs and spacers involves systematic investigation. Problems often relate to technique, device malfunction, or medication issues.
- MDI Issues:
- No spray: Check if the canister is empty. If not, try a new canister. Inspect the mouthpiece for blockage.
- Weak spray: The canister might be low on medication. Check for proper actuation technique. Consider using a spacer.
- Clogged mouthpiece: Clean the mouthpiece with warm water. Ensure you properly clean and dry the MDI after each use.
- Spacer Issues:
- Lack of medication delivery: Check the spacer for any blockages. Make sure it’s correctly attached to the MDI.
- Inconsistent performance: Clean the spacer regularly as per the manufacturer’s instructions to ensure optimal performance.
Problem-solving steps: Always start by verifying correct patient technique. Then, examine the device for mechanical defects. If the problem persists, a new MDI or spacer may be required.
Example: A patient reports a weak spray. I first confirm their inhaler technique is correct. Next, I check if the canister is empty. If not, I might suggest using a spacer to improve drug delivery. If the issue persists with a new canister, I would consider a different inhaler type or refer the patient for further assessment.
Q 17. Describe the role of medication titration in aerosol therapy.
Medication titration in aerosol therapy is the gradual adjustment of medication dosage to achieve optimal therapeutic benefit while minimizing side effects. It’s a crucial aspect of personalized medicine, tailored to the patient’s response and clinical status.
- Initial Dose: Treatment starts with a low dose and is carefully increased based on the patient’s response. This stepwise approach helps assess the efficacy and tolerability of the medication.
- Monitoring: Regular monitoring of clinical parameters such as lung function (FEV1, PEFR), symptoms (cough, wheezing, dyspnea), and adverse effects is crucial. This data guides the titration process.
- Stepwise Adjustments: Dosage changes are made incrementally, observing the patient’s response at each stage. This allows for flexibility in managing the patient’s condition and minimizing the risk of adverse effects.
Example: A patient with asthma may start with a low dose of inhaled corticosteroid. Over several weeks, if symptoms don’t improve or worsen, the dosage might be increased gradually. If side effects like oral thrush develop, the dosage could be reduced or the administration technique altered.
Q 18. How do you assess patient understanding and adherence to aerosol therapy regimens?
Assessing patient understanding and adherence is vital for successful aerosol therapy. This involves a multifaceted approach encompassing education, demonstration, and follow-up.
- Education: Provide clear, concise instructions about the medication, inhaler technique, and dosage regimen. Use visual aids or demonstrations. Explain the importance of adherence to the prescribed treatment plan.
- Demonstration: Show the patient how to use the inhaler correctly. Observe their technique and provide feedback. Encourage them to practice.
- Follow-up: Schedule regular follow-up appointments to monitor their progress, address any concerns, and assess their adherence. Use techniques such as pill counts, medication event monitoring system (MEMS) or patient self-reporting. The patient’s understanding of their condition and treatment is key.
- Questioning: Engage in open-ended discussions with patients, allowing them to describe their understanding of their treatment. The ‘teach-back’ method (asking the patient to explain it back to you) is highly effective.
Example: After demonstrating DPI use, I would ask the patient to show me how they would use it and explain the reasoning. If any steps are unclear, I provide further explanation and allow them to practice again. Regular follow up visits assess their adherence and adjust treatment as needed.
Q 19. Explain the use of spacers and holding chambers.
Spacers and holding chambers are devices used with MDIs to improve medication delivery to the lungs. They act as reservoirs, allowing the patient to inhale the medication more effectively, even if their coordination is poor.
- Mechanism: The MDI delivers the medication into the spacer. The patient then inhales from the spacer, which allows a longer time to inhale the medication, improving drug deposition in the lungs. This is especially helpful for children and elderly individuals with poor coordination.
- Benefits: Spacers minimize the loss of medication in the mouth and throat and reduce the risk of side effects like oral thrush. They also improve the overall efficacy of the inhaled medication.
- Types: Various types of spacers exist, ranging from simple tubes to more complex valved holding chambers (VHCs). VHCs prevent exhaled air from mixing with the medication, maximizing drug delivery.
Example: A child with asthma may struggle to coordinate pressing the MDI and inhaling simultaneously. A spacer helps overcome this coordination challenge, ensuring a larger portion of the medication reaches their lungs.
Q 20. What are the guidelines for the safe handling and disposal of aerosol medications and equipment?
Safe handling and disposal of aerosol medications and equipment are crucial for patient safety and environmental protection. This involves several key steps:
- Medication Handling: Always read the medication label carefully. Follow the instructions for use, storage, and handling. Store medications in a cool, dry place, away from direct sunlight or extreme temperatures. Never mix different medications in the same device.
- Equipment Cleaning: Clean the inhaler and spacer regularly as per the manufacturer’s instructions. Usually, this involves wiping the device with a clean, damp cloth. Some devices are designed for washing with warm water and mild soap. Always allow components to dry completely before reuse.
- Disposal: Dispose of used inhalers and spacers according to local regulations. This may involve returning them to a pharmacy for proper disposal or following specific household waste guidelines.
- Environmental Considerations: Avoid releasing aerosols into the environment. This can contribute to air pollution. The propellant in MDIs contributes to greenhouse effect so disposal is important.
Example: After using an MDI, I would instruct the patient to rinse the mouthpiece with warm water. Dispose of the empty canister in a sharps container, if available, or as per local guidelines.
Q 21. Discuss the use of bronchodilators and corticosteroids in aerosol therapy.
Bronchodilators and corticosteroids are two major classes of drugs used in aerosol therapy for respiratory conditions. They address different aspects of the disease process.
- Bronchodilators: These medications relax the muscles around the airways, widening them and improving airflow. They provide quick relief of symptoms like wheezing and shortness of breath. Common examples include albuterol (salbutamol) and ipratropium bromide, often used as rescue medication. They work rapidly but the effect is short-lived.
- Corticosteroids: These are anti-inflammatory medications that reduce swelling and inflammation in the airways. They are typically used for long-term control of symptoms and prevention of exacerbations. Examples include fluticasone and budesonide. They are effective in preventing inflammation and reducing the severity of exacerbations but do not provide immediate relief.
Combined Therapy: Often, bronchodilators and corticosteroids are used together to provide both quick relief and long-term control of respiratory symptoms. A combination inhaler containing both medication types simplifies the treatment regimen.
Example: A patient with asthma might use a short-acting beta-agonist (SABA) bronchodilator, such as albuterol, for quick relief of wheezing attacks and an inhaled corticosteroid, such as fluticasone, daily to prevent inflammation and maintain control of their condition. This is a combination of rescue and maintenance treatment.
Q 22. How do you select appropriate aerosol medications for different respiratory conditions?
Selecting the right aerosol medication hinges on accurately diagnosing the respiratory condition and understanding the medication’s properties. We consider factors like the disease’s severity, the patient’s age and overall health, and the drug’s mechanism of action. For example, a patient with acute asthma exacerbation might require a short-acting beta-agonist (like albuterol) via a metered-dose inhaler (MDI) for immediate relief, while a patient with chronic obstructive pulmonary disease (COPD) might benefit from a long-acting bronchodilator (like tiotropium) via a dry powder inhaler (DPI) for long-term control. The choice also depends on the specific delivery device, considering factors such as the patient’s coordination and ability to use the device correctly.
- Asthma: Short-acting beta-agonists (SABAs) for quick relief, inhaled corticosteroids (ICS) for inflammation control, and long-acting beta-agonists (LABAs) for long-term bronchodilation (often combined with ICS).
- COPD: Long-acting bronchodilators (LABAs or long-acting muscarinic antagonists – LAMAs), and sometimes ICS for exacerbations.
- Cystic Fibrosis: Combination therapies involving bronchodilators, mucolytics (e.g., dornase alfa), and antibiotics depending on the infection present.
Careful consideration of potential drug interactions and side effects is crucial. For instance, some patients may experience tremors or palpitations with beta-agonists, requiring alternative therapies or dose adjustments.
Q 23. Describe the importance of patient education and counseling in aerosol therapy.
Patient education is the cornerstone of successful aerosol therapy. Without proper understanding and technique, even the most effective medication will fail to deliver optimal results. Counseling involves demonstrating correct inhaler technique (e.g., spacer use with MDIs), explaining the medication’s purpose, dosage, frequency, and potential side effects, and empowering patients to actively participate in managing their condition. I always emphasize the importance of adherence to the prescribed regimen and encourage patients to report any difficulties or side effects immediately.
For instance, I’d demonstrate the proper use of a spacer and coordinating inhalation with actuation for an MDI, explaining that this ensures the medication reaches the lungs more effectively. I would also detail potential side effects, such as hoarseness with ICS, and provide coping strategies. Regularly scheduled follow-up appointments reinforce this education and ensure patients are comfortable and successful with their treatment.
Q 24. Explain your approach to managing a patient experiencing a severe adverse reaction to aerosol medication.
Managing a severe adverse reaction requires immediate action and a calm, organized approach. The first step is to immediately stop the medication administration. I would then assess the patient’s vital signs (heart rate, blood pressure, respiratory rate, oxygen saturation) and symptoms. Based on the severity and type of reaction (e.g., bronchospasm, angioedema, hypersensitivity), I would initiate appropriate interventions such as administering oxygen, bronchodilators, or antihistamines, as needed. Severe reactions may necessitate calling for emergency medical assistance. Documentation of the event, including the medication administered, the symptoms observed, and the interventions taken, is essential for future reference and to prevent similar incidents.
For example, if a patient experiences sudden bronchospasm after using albuterol, I’d immediately give them a rescue inhaler (likely a different bronchodilator if the reaction suggests hypersensitivity), and if the symptoms don’t resolve promptly, I’d contact emergency services. Subsequent management might involve referring the patient to an allergist for allergy testing.
Q 25. How do you maintain quality control and ensure the proper function of aerosol delivery devices?
Quality control in aerosol therapy focuses on both the devices and the medications. Regular cleaning and maintenance of inhalers, including checking for proper function, are crucial. We need to ensure that devices are delivering the correct dose and that the medications themselves are within their expiration dates and stored correctly. For MDIs, we check for proper spray release; for DPIs, we ensure there’s no clogging or leakage.
Beyond the devices themselves, proper medication storage and handling are paramount. Maintaining an accurate inventory, tracking expiration dates, and ensuring that the medication is stored at the appropriate temperature are all critical aspects. In a clinical setting, rigorous adherence to infection control protocols is essential when managing multiple patients’ devices.
Regular audits and device checks by trained personnel are crucial parts of the maintenance process. We might use standardized checklists to confirm every aspect of device operation is functioning as intended. This proactive approach minimizes the risk of malfunction and ensures consistent, effective therapy.
Q 26. What are the essential components of a comprehensive aerosol therapy plan?
A comprehensive aerosol therapy plan should be patient-centered and holistic. It starts with a thorough assessment of the respiratory condition, including a review of the patient’s medical history, current medications, and functional status. This allows the selection of the appropriate medication and device, taking into account the patient’s physical abilities and preferences. The plan then needs to include detailed instructions on medication administration, including dosage, frequency, and technique. Patient education is a crucial component, as is a clear strategy for monitoring the effectiveness of therapy, including regular follow-up appointments to assess symptoms, lung function, and medication adherence. A plan also needs to incorporate a mechanism for handling adverse events or exacerbations.
For example, a plan for a patient with severe asthma might involve daily ICS, PRN use of a SABA, peak flow monitoring at home, and a clear escalation plan in case of an exacerbation, including guidance on when to seek medical attention.
Q 27. Discuss the role of technology (e.g., smart inhalers, electronic monitoring) in improving aerosol therapy outcomes.
Technology is transforming aerosol therapy, improving both adherence and treatment outcomes. Smart inhalers, for instance, can track medication use, providing valuable data for assessing adherence and identifying potential issues. Electronic monitoring systems can remotely track a patient’s lung function, providing real-time data to clinicians. These technologies allow for proactive interventions and adjustments to the treatment plan, optimizing therapy and reducing hospitalizations. Furthermore, digital health platforms can support patient education and remote monitoring, extending access to care for patients in remote locations or with limited mobility.
For example, data from a smart inhaler might show that a patient is using their rescue inhaler more frequently, suggesting a need for an adjustment in their long-term medication regimen. Similarly, remote monitoring of lung function via a connected device can alert the healthcare team to a worsening condition, allowing for early intervention.
Q 28. Describe your experience with specific aerosol therapy modalities, such as high-frequency oscillatory ventilation or non-invasive ventilation.
My experience with high-frequency oscillatory ventilation (HFOV) and non-invasive ventilation (NIV) is primarily in the context of managing critically ill patients with acute respiratory distress syndrome (ARDS) or other severe respiratory failures. HFOV delivers small tidal volumes at high frequencies, improving gas exchange and reducing lung injury in patients with severely compromised lung mechanics. NIV, on the other hand, provides respiratory support through a mask without the need for endotracheal intubation, reducing the risk of ventilator-associated pneumonia and improving patient comfort. Both modalities require careful patient selection, close monitoring, and a comprehensive understanding of their physiological effects. The decision to use HFOV or NIV is always made based on a careful assessment of the patient’s condition and response to initial treatment.
For example, I have managed patients with ARDS who responded well to HFOV, showing improvements in oxygenation and respiratory mechanics. In other cases, I have utilized NIV successfully to support patients with COPD exacerbations, avoiding the need for mechanical ventilation.
Key Topics to Learn for Aerosol Therapy Management Interview
- Aerosol Delivery Systems: Understanding various inhaler devices (MDIs, DPIs, nebulizers), their mechanisms, and appropriate patient selection.
- Pharmacokinetics and Pharmacodynamics of Aerosol Medications: Knowing how inhaled medications are absorbed, distributed, metabolized, and excreted, and their effects on the body. This includes understanding the impact of particle size and deposition.
- Patient Assessment and Education: Mastering techniques for assessing respiratory status, identifying patient needs, and providing clear, concise, and culturally sensitive education on inhaler technique and medication management.
- Monitoring Treatment Effectiveness: Understanding how to monitor patient response to therapy, recognizing adverse effects, and adjusting treatment plans accordingly. This includes interpreting relevant lab results and clinical data.
- Troubleshooting Common Problems: Developing the ability to identify and resolve issues related to inhaler technique, medication delivery, and patient compliance.
- Disease Management: A solid understanding of common respiratory conditions treated with aerosol therapy, such as asthma, COPD, cystic fibrosis, and bronchiectasis. Knowing the treatment goals and strategies for each condition is crucial.
- Safety and Quality Improvement: Familiarity with relevant safety protocols, infection control measures, and quality improvement initiatives within aerosol therapy.
- Legal and Ethical Considerations: Understanding the legal and ethical implications of aerosol therapy administration and patient care, including informed consent and medication safety.
Next Steps
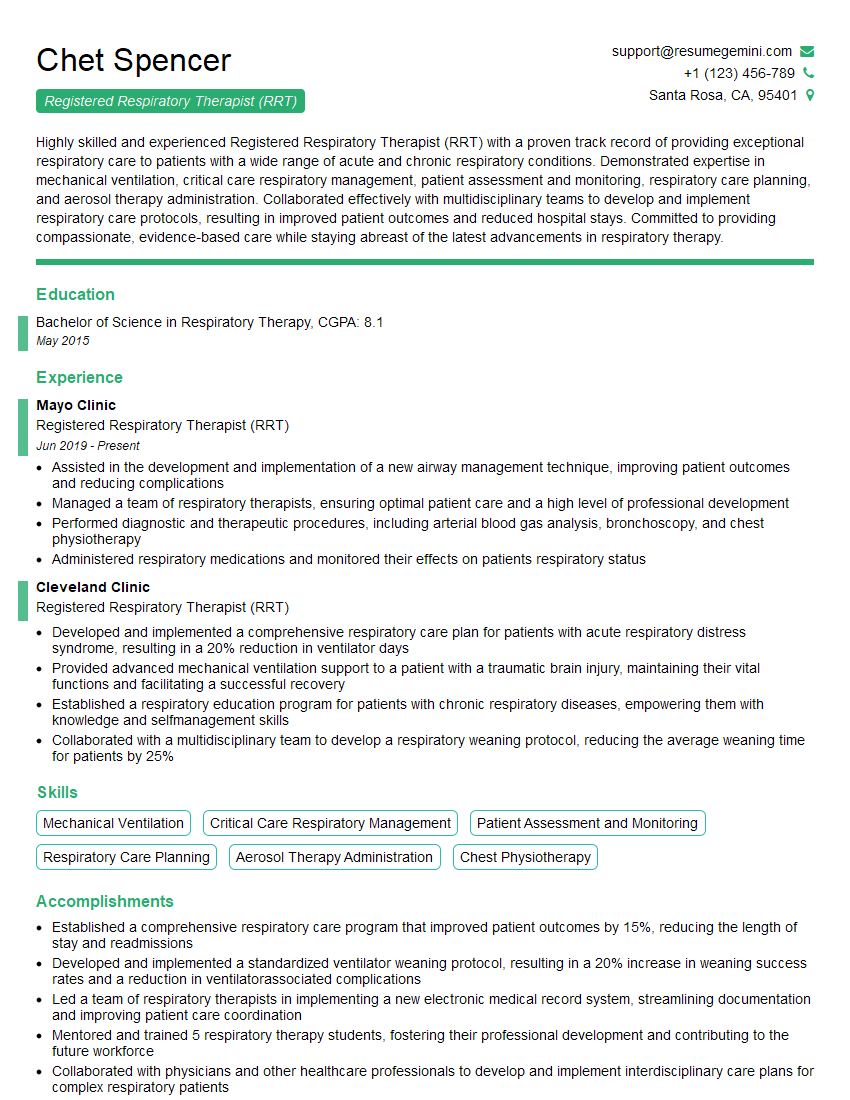
Mastering Aerosol Therapy Management opens doors to exciting career opportunities and positions you as a highly skilled and sought-after healthcare professional. To maximize your chances of landing your dream job, a strong, ATS-friendly resume is essential. This is where ResumeGemini can help. ResumeGemini provides a powerful platform to build a professional resume that highlights your skills and experience effectively. They even offer examples of resumes tailored specifically for Aerosol Therapy Management professionals, helping you create a compelling application that stands out from the competition. Invest time in crafting a winning resume – it’s a crucial step towards your successful career journey.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.