Cracking a skill-specific interview, like one for Ankle and Foot Sprains and Injuries Management, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Ankle and Foot Sprains and Injuries Management Interview
Q 1. Describe the Ottawa Ankle Rules and their application.
The Ottawa Ankle Rules are a clinical decision tool used to determine whether an ankle X-ray is necessary after an ankle injury. They’re crucial in minimizing unnecessary radiation exposure while ensuring that significant fractures aren’t missed. The rules are based on the presence or absence of specific symptoms and findings during a physical examination.
The rules state that an X-ray is indicated if any of the following are present:
- Bone tenderness at the posterior edge or tip of the medial or lateral malleolus (the bony prominences on the inner and outer ankle).
- Inability to bear weight immediately after the injury and during the examination (four steps).
- Tenderness at the base of the fifth metatarsal.
- Tenderness at the navicular bone.
Application: Imagine a patient comes in after twisting their ankle. A doctor would assess for bone tenderness along the malleoli, check if the patient can bear weight, and palpate the base of the fifth metatarsal and the navicular. If any of the criteria are met, an X-ray is ordered. If none are met, the injury is likely a sprain and further management can focus on conservative treatment. The Ottawa Ankle Rules significantly reduce unnecessary X-rays, leading to cost savings and reduced radiation exposure for patients while still ensuring timely diagnosis of fractures.
Q 2. Explain the difference between a Grade I, II, and III ankle sprain.
Ankle sprains are classified into three grades based on the severity of ligament damage:
- Grade I (Mild): This involves stretching of the ligament fibers with minimal tearing. There is mild pain, swelling, and instability. The ankle remains relatively stable. Think of it like slightly overstretching a rubber band – it’s still intact, but stretched.
- Grade II (Moderate): This involves a partial tear of the ligament(s). There is moderate pain, swelling, and instability. The ankle might feel somewhat ‘wobbly.’ This is like a rubber band with a small tear – it’s still holding, but it’s weaker.
- Grade III (Severe): This involves a complete rupture of the ligament(s). There is severe pain, swelling, and instability. The ankle may feel very unstable, and significant functional impairment is likely. Imagine the rubber band being completely snapped.
The grading is determined by clinical examination and assessment of the patient’s pain, swelling, range of motion, and functional ability. MRI scans can sometimes be used to confirm the diagnosis, especially in borderline cases.
Q 3. What imaging techniques are used to diagnose ankle and foot injuries?
Several imaging techniques are used to diagnose ankle and foot injuries, depending on the suspected diagnosis and clinical presentation:
- X-ray: This is the most common initial imaging modality used to rule out fractures. It provides clear images of bones and can detect bone fragments, dislocations, and fractures.
- Ultrasound: Ultrasound provides real-time images of soft tissues, making it helpful in evaluating ligament tears, tendon injuries, and other soft tissue damage. It’s less invasive than MRI and can be used at the bedside in some cases.
- MRI (Magnetic Resonance Imaging): MRI provides detailed images of bones and soft tissues, allowing for precise visualization of ligaments, tendons, cartilage, and other structures. It’s particularly helpful in diagnosing complex injuries and determining the extent of ligament damage. It’s more expensive and time-consuming than X-rays or ultrasound.
- CT (Computed Tomography) Scan: A CT scan provides detailed cross-sectional images, which are particularly useful for evaluating complex fractures, particularly those involving multiple bones or small bone fragments.
The choice of imaging technique will depend on the clinical suspicion and the specific information needed to guide treatment.
Q 4. Outline the initial management of an acute ankle sprain.
Initial management of an acute ankle sprain focuses on reducing pain, swelling, and inflammation, and preventing further injury. This is commonly known as the RICE protocol:
- Rest: Avoid weight-bearing and any activities that aggravate the injury. Crutches may be necessary.
- Ice: Apply ice packs for 15-20 minutes at a time, several times a day, to reduce swelling and pain. Never apply ice directly to the skin; wrap it in a thin cloth.
- Compression: Use an elastic bandage to provide compression, reducing swelling and providing support. Avoid excessive compression, as this can impair circulation.
- Elevation: Keep the ankle elevated above the heart as much as possible to reduce swelling. Elevate the leg using pillows when resting or sleeping.
Over-the-counter pain relievers such as ibuprofen or naproxen can help manage pain and inflammation. Early mobilization is crucial, and often physical therapy is started fairly early in the healing process under appropriate guidance.
Q 5. Discuss the role of physiotherapy in ankle sprain rehabilitation.
Physiotherapy plays a vital role in ankle sprain rehabilitation. A well-designed physiotherapy program aims to restore ankle function, range of motion, strength, proprioception (awareness of the joint’s position in space), and reduce the risk of recurrent sprains.
Physiotherapy interventions typically include:
- Range of motion exercises: Gentle exercises to improve ankle flexibility and mobility.
- Strengthening exercises: Exercises to strengthen the muscles surrounding the ankle joint, improving stability and support.
- Proprioceptive exercises: Exercises designed to improve balance and coordination. Examples include balance boards, wobble boards, and exercises on uneven surfaces.
- Manual therapy: Techniques such as joint mobilization and soft tissue mobilization to address any joint restrictions or muscle tightness.
- Functional exercises: Exercises simulating activities of daily living to help the patient regain normal function and return to their activities. This might include activities like walking, jogging, stair climbing, or sport-specific activities.
- Taping and bracing: Providing additional support and stability during rehabilitation.
Physiotherapists also educate patients on injury prevention strategies and proper footwear to reduce the risk of future sprains.
Q 6. What are the common complications of untreated ankle sprains?
Untreated or improperly treated ankle sprains can lead to several complications:
- Chronic pain and instability: Persistent pain, swelling, and ankle instability, making it difficult to participate in normal activities.
- Osteoarthritis: Repeated sprains can damage the cartilage in the ankle joint, leading to osteoarthritis over time. This can cause significant pain and stiffness in later life.
- Ligament laxity: Repeated ankle sprains can lead to persistent ligament laxity, increasing the risk of future sprains.
- Chronic swelling: Persistent swelling in the ankle joint, leading to discomfort and functional limitations.
- Ankle impingement: Formation of bone spurs or other bony abnormalities that can cause pain and restrict movement.
- Functional limitations: Significant challenges in performing daily activities like walking, running, or participating in sports.
Proper management of ankle sprains is crucial to prevent these long-term complications. Early diagnosis, appropriate treatment, and diligent participation in rehabilitation greatly enhance the chances of a full recovery.
Q 7. Explain the difference between a Lisfranc and a Jones fracture.
Both Lisfranc and Jones fractures are common foot fractures, but they occur in different locations:
- Lisfranc fracture-dislocation: This injury involves the disruption of the Lisfranc joint, which connects the midfoot bones (metatarsals) to the tarsals (bones in the hindfoot). It is often caused by a high-energy trauma, such as a fall from a significant height or a crush injury. It usually involves multiple bones and ligaments and can be complex to treat.
- Jones fracture: This is a fracture of the base of the fifth metatarsal bone, commonly caused by a twisting injury. It’s located more laterally in the foot, near the pinky toe, compared to a Lisfranc injury, which is more central.
Key Differences:
- Location: Lisfranc involves the midfoot joints; Jones involves the base of the fifth metatarsal.
- Mechanism of injury: Lisfranc is often high-energy trauma; Jones is usually a twisting injury.
- Involvement of structures: Lisfranc usually involves multiple bones and ligaments; Jones typically involves only one bone.
- Treatment: Lisfranc injuries often require surgical intervention; Jones fractures can sometimes be managed non-operatively, but surgery might be needed depending on the fracture type and stability.
Accurate diagnosis is crucial because both injuries have different management strategies and potential complications. Imaging techniques like X-rays and CT scans are essential to distinguish between the two.
Q 8. Describe the treatment options for plantar fasciitis.
Plantar fasciitis, a common cause of heel pain, involves inflammation of the plantar fascia, a thick band of tissue on the bottom of your foot. Treatment focuses on reducing inflammation and pain, and improving flexibility and strength.
Conservative Management: This is the first line of treatment and often involves rest, ice, and over-the-counter pain relievers like ibuprofen or naproxen. Stretching exercises, particularly those targeting the plantar fascia and calf muscles, are crucial. Night splints help maintain dorsiflexion (bending the foot upwards) overnight, preventing the plantar fascia from tightening.
Physical Therapy: A physical therapist can guide you through a tailored exercise program, including strengthening exercises for the intrinsic foot muscles and potentially techniques like ultrasound or iontophoresis to reduce inflammation.
Orthotics: Custom or over-the-counter arch supports can help redistribute pressure on the plantar fascia, reducing strain. These provide cushioning and support to the arch of the foot.
Injections: Corticosteroid injections can provide temporary pain relief, but they shouldn’t be relied upon long-term due to potential side effects and risk of plantar fascia rupture.
Surgery: Surgery is rarely needed and is usually considered only if conservative measures have failed after a prolonged period (typically 6-12 months). It may involve a plantar fasciotomy (release of the plantar fascia) or other surgical procedures.
Imagine plantar fasciitis as a tight rubber band constantly pulling on your heel. The treatments aim to loosen that band, allowing for better function and reducing pain.
Q 9. How do you assess the stability of an ankle joint?
Assessing ankle stability involves a comprehensive examination focusing on both the subjective and objective findings. We look at the mechanism of injury, patient’s history, and the physical examination.
History: Understanding how the injury occurred (e.g., inversion sprain, eversion sprain) provides valuable information. We ask about the severity of the initial pain, any associated sounds (pop or crack), and the patient’s ability to bear weight immediately after the injury.
Physical Examination: This includes:
Inspection: Assessing for swelling, bruising, deformity, and skin discoloration.
Palpation: Feeling for tenderness around the ligaments, bones, and tendons.
Range of Motion (ROM): Evaluating the ankle’s ability to move in all directions (dorsiflexion, plantarflexion, inversion, eversion). Limited ROM is indicative of injury.
Ligamentous Stability Tests: Performing specific tests, such as the anterior drawer test and talar tilt test, to assess the integrity of the anterior talofibular ligament (ATFL) and calcaneofibular ligament (CFL). These tests evaluate the stability of the joint and detect any laxity.
Neurovascular Assessment: Checking for any loss of sensation or weakness in the foot and toes to ensure proper blood supply and nerve function.
Imaging: X-rays are often used to rule out fractures, while MRI scans may be necessary for detailed assessment of ligament injuries or other soft tissue damage if there is ongoing concern.
Think of it like checking the structural integrity of a building. We assess the overall structure (bones), the supporting elements (ligaments), and the movement (ROM) to determine the overall stability of the ankle.
Q 10. What are the signs and symptoms of a stress fracture in the foot?
Stress fractures, tiny cracks in a bone, often occur in weight-bearing areas like the foot, particularly in athletes. They often develop gradually, rather than from a single traumatic event.
Gradual onset of pain: Pain typically starts subtly, worsening with activity and gradually improving with rest. The pain may be localized to a specific point on the foot.
Point tenderness: Palpating the affected area will usually reveal a very specific point of intense pain.
Swelling: While usually less pronounced than with other injuries, there might be some swelling or mild bruising around the fracture site.
Pain with weight-bearing: Pain increases when putting weight on the affected foot.
Possible audible crackle: In some cases, a subtle crackling sound might be felt or heard when the fractured bone fragments rub against each other.
Imagine a hairline crack in a ceramic plate; it might not be immediately obvious, but it will weaken the plate and cause pain when pressure is applied. Stress fractures are similar – subtle, yet increasingly painful with weight-bearing activity.
Q 11. Describe the various types of ankle braces and their indications.
Ankle braces provide support and stability to the ankle joint, helping to prevent re-injury and promote healing. Various types exist, each with specific indications:
Lace-up braces: These offer customizable compression and support, useful for mild to moderate ankle instability. They are adjustable and allow for a personalized fit.
Rigid braces: These are more supportive and provide greater stability, ideal for severe ankle sprains or post-surgical rehabilitation. They often include a rigid shell for immobilization.
Air braces: These inflatable braces offer adjustable compression and support, allowing for a personalized fit while being lightweight and comfortable. Useful for those with mild to moderate instability and needing good comfort.
Hinged braces: These braces feature hinges to provide controlled range of motion, assisting with the rehabilitation process after a significant ankle injury. They help prevent unwanted inversion or eversion movements.
Stirrup braces: These wrap around the ankle and provide support across the malleoli. These are great options for mild instability and provide easy slip-on functionality.
The choice of brace depends on the severity of the injury, the patient’s activity level, and the stage of recovery. A physician or physical therapist will determine the best type of brace for your specific needs.
Q 12. How do you differentiate between an Achilles tendon rupture and a strain?
Differentiating between an Achilles tendon rupture and strain is crucial for appropriate management. Ruptures are complete tears of the tendon, while strains are partial tears or injuries.
Achilles Tendon Rupture: Often presents with a sudden, sharp pain, often described as a ‘pop’ or ‘snap’ in the back of the heel. There may be immediate swelling, bruising, and a palpable gap in the tendon. The patient will have significant difficulty in plantarflexion (pointing the toes down).
Achilles Tendon Strain: Typically involves a gradual onset of pain in the back of the heel, often associated with overuse. Swelling and bruising are usually less pronounced than in a rupture. The patient will likely experience pain with plantarflexion but will still be able to perform the movement to some degree.
Imagine snapping a rubber band (rupture) versus stretching it too far (strain). The rupture is a complete break, while the strain is a partial injury. A physical examination and often imaging (ultrasound or MRI) are necessary to confirm the diagnosis.
Q 13. What are the risk factors for developing ankle sprains?
Ankle sprains are common injuries, often caused by twisting or rolling the ankle. Several risk factors increase the likelihood of developing an ankle sprain:
Previous ankle sprain: A prior ankle sprain significantly increases the risk of future sprains. This is because previous injuries often leave the ankle ligaments weaker and more susceptible to re-injury.
Poor proprioception: Proprioception is your body’s awareness of its position in space. Poor proprioception makes it harder to maintain balance and stability, increasing the risk of an ankle sprain.
Inadequate footwear: Wearing inappropriate footwear, such as high heels or worn-out shoes, reduces ankle support and increases the risk of injury.
Muscle weakness: Weakness in the muscles surrounding the ankle, particularly the calf muscles, compromises stability and support.
Activity level: Individuals involved in high-impact sports or activities that place stress on the ankles (e.g., running, basketball, soccer) are at greater risk.
Underlying conditions: Conditions such as osteoarthritis, diabetes, or certain neurological disorders can also increase the risk of ankle sprains.
Think of the ankle as a finely tuned mechanism; any weakening of its components (ligaments, muscles, proprioception) increases its vulnerability to injury.
Q 14. What are the common causes of foot and ankle pain in athletes?
Athletes often experience foot and ankle pain due to the repetitive stress and impact forces associated with their activities. Common causes include:
Ankle sprains: These are highly prevalent, often caused by sudden inversion or eversion movements.
Plantar fasciitis: Repetitive stress on the plantar fascia leads to inflammation and pain.
Achilles tendinopathy: Overuse and repetitive stress on the Achilles tendon causes inflammation, pain, and potentially rupture in severe cases.
Stress fractures: Repetitive impact forces can cause tiny cracks in the bones of the foot and ankle.
Tarsal tunnel syndrome: Compression of the tibial nerve in the tarsal tunnel can cause pain, numbness, and tingling in the foot.
Bunions and hammertoes: These deformities can be exacerbated by athletic activities, leading to pain and discomfort.
Metatarsalgia: Pain in the ball of the foot often caused by repetitive impact or improper footwear.
The repetitive nature of athletic training puts significant stress on the foot and ankle structures. Proper training, appropriate footwear, and injury prevention strategies are critical for reducing the risk of these injuries.
Q 15. Explain the role of bracing and taping in ankle injury prevention.
Bracing and taping play crucial roles in ankle injury prevention, primarily by providing support and stability to the ankle joint. Think of them as external reinforcements, limiting excessive or unnatural movements that could lead to sprains or fractures.
Braces offer more substantial support than taping. They come in various designs, from simple sleeves to more rigid structures with adjustable straps. A well-fitted brace can help control the range of motion, protecting against inversion (rolling inwards) and eversion (rolling outwards) sprains – the most common types of ankle injuries. For example, a patient recovering from a severe ankle sprain might use a brace for several weeks to prevent re-injury during weight-bearing activities.
Taping, often using athletic tape, provides a more customizable and lighter support. It’s frequently used by athletes to provide prophylactic protection before activities, helping to prevent injury in high-risk situations. Different taping techniques can target specific areas of the ankle, offering support to ligaments and reducing the likelihood of instability. For instance, the “figure-eight” taping method is common for supporting the lateral ligaments vulnerable during inversion sprains.
The choice between bracing and taping depends on the individual’s needs, the level of activity, and the severity of the risk. A healthcare professional can help determine the most appropriate method for prevention.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe the surgical management of a severe ankle fracture.
Surgical management of severe ankle fractures is necessary when the fracture is unstable, significantly displaced, or involves damage to the articular cartilage (the smooth surface of the joint). The goal of surgery is to restore the anatomical alignment of the bones and allow for proper healing.
The surgical procedure typically involves open reduction and internal fixation (ORIF). This means the surgeon makes an incision to expose the fractured bones, manipulates them back into their correct position (reduction), and then uses implants like screws, plates, or wires to hold the bones in place (fixation). The specific type of implant used depends on the nature and location of the fracture.
Post-operatively, the patient will require a period of immobilization, often using a cast or brace. Physical therapy plays a crucial role in regaining range of motion, strength, and stability after surgery. The recovery period can vary significantly based on the severity of the fracture and the individual’s response to treatment. For example, a complex fracture involving multiple bones may require a longer healing time compared to a simpler fracture.
Q 17. How do you manage a patient with a chronic ankle instability?
Chronic ankle instability (CAI) refers to persistent ankle instability and recurrent giving way of the ankle even after the initial injury has healed. Management of CAI requires a multi-faceted approach.
Conservative Management: This is often the first line of treatment and includes:
- Physical therapy: Strengthening exercises, proprioceptive training (improving balance and coordination), and neuromuscular re-education are crucial to improve joint stability and prevent further injury.
- Bracing or taping: Provides additional support during activities.
- Orthotics: Custom-made insoles can help correct foot biomechanics and reduce abnormal stress on the ankle.
Surgical Management: If conservative measures fail, surgery might be considered. This can involve procedures to reconstruct damaged ligaments, repair cartilage damage, or address other underlying issues contributing to instability. The specific surgical technique depends on the extent of the damage.
Patient Education: It’s vital to educate patients on proper footwear, activity modification, and recognizing early signs of ankle instability to prevent further injuries. Early intervention is crucial for successful management of CAI.
Q 18. What are the different types of ankle arthroscopy procedures?
Ankle arthroscopy is a minimally invasive surgical procedure that uses small incisions and a specialized instrument with a camera (arthroscope) to visualize the interior of the ankle joint. Several types of procedures can be performed arthroscopically.
- Debridement: Removing damaged cartilage, bone fragments, or inflamed tissue.
- Repair of cartilage lesions: Addressing cartilage defects using techniques like microfracture or chondrocyte implantation.
- Ligament repair: Repairing torn ligaments, often in conjunction with other procedures.
- Synovectomy: Removal of the inflamed synovial lining of the joint.
- Removal of loose bodies: Removing free-floating fragments of bone or cartilage within the joint.
Arthroscopy allows for a less invasive approach compared to open surgery, resulting in smaller scars, reduced pain, and faster recovery. The choice of procedure depends on the specific diagnosis and the surgeon’s judgment.
Q 19. Describe the use of ultrasound in evaluating ankle and foot injuries.
Ultrasound is a valuable imaging modality used to evaluate ankle and foot injuries. It uses high-frequency sound waves to produce real-time images of the soft tissues. This makes it particularly useful for assessing:
- Ligament injuries: Ultrasound can visualize ligament tears, though the accuracy is sometimes limited compared to MRI for subtle tears.
- Tendon injuries: It can effectively show tendon tears, inflammation (tendinitis), and other abnormalities.
- Muscle injuries: Ultrasound can identify muscle strains, tears, and hematomas (blood clots).
- Fluid collections: It can detect the presence of joint effusions (excess fluid in the joint) or other fluid accumulations.
- Bursitis: Inflammation of the bursae (fluid-filled sacs that cushion the joint) is easily visualized.
Ultrasound is cost-effective, readily available, and does not involve ionizing radiation. However, it has limitations in visualizing bony structures. It’s often used in conjunction with other imaging modalities such as X-rays or MRI for a comprehensive assessment.
Q 20. Explain the principles of gait analysis in assessing foot and ankle function.
Gait analysis is a systematic evaluation of how a person walks. It provides valuable information about the function of the foot and ankle during locomotion. This helps in diagnosing and managing various foot and ankle problems.
Principles of Gait Analysis:
- Observational Gait Analysis: A clinician observes the patient’s walking pattern, noting any abnormalities in stance phase (weight-bearing), swing phase (non-weight-bearing), or overall gait cycle.
- Kinematic Analysis: Uses cameras and motion capture technology to measure joint angles and movement patterns, providing objective data on joint ranges of motion, stride length, and gait speed.
- Kinetic Analysis: Measures the forces acting on the joints and limbs during walking, using force plates to quantify ground reaction forces.
- Electromyography (EMG): Assesses muscle activity during walking, helping identify muscles contributing to abnormal gait patterns.
By integrating these methods, gait analysis helps identify underlying causes of gait abnormalities, such as muscle weakness, joint stiffness, or foot deformities, aiding in the development of personalized treatment plans. For instance, identifying a gait pattern associated with plantar fasciitis allows targeting specific muscle groups and prescribing relevant orthotics to address the root cause.
Q 21. What are the different types of footwear that can help prevent foot and ankle injuries?
Appropriate footwear plays a vital role in preventing foot and ankle injuries. The best choice depends on the activity and individual needs, but key features include:
- Proper Fit: Shoes should fit comfortably and provide enough room for the toes. Shoes that are too tight or too loose can contribute to injuries.
- Good Arch Support: Arch support helps maintain proper foot biomechanics and reduces stress on the ankle.
- Stable Heel Counter: A firm heel counter provides stability and prevents excessive motion of the heel.
- Cushioning: Proper cushioning absorbs shock and reduces stress on the joints, especially important for high-impact activities.
- Appropriate Sole: The sole should provide adequate traction to prevent slips and falls.
Examples: Running shoes offer good cushioning and support for runners. Hiking boots provide ankle support and stability for uneven terrain. Supportive athletic shoes are beneficial for various sports and daily activities. People with pre-existing conditions might benefit from specialized orthotic shoes or custom-made inserts. Consulting a podiatrist can help determine the most appropriate footwear for individual needs.
Q 22. How do you counsel a patient on post-operative care for ankle surgery?
Post-operative care for ankle surgery is crucial for a successful outcome. It’s a highly individualized plan, tailored to the specific procedure and the patient’s overall health. Generally, it involves several key phases:
Immediate Post-Op (Hospital Stay): This focuses on pain management (often with medication and ice), monitoring for complications (infection, swelling, bleeding), and initiating early mobilization as directed by the surgeon. For example, this might involve gentle range-of-motion exercises within the limits of the pain and surgical restrictions.
Early Post-Op (Weeks 1-6): This phase emphasizes wound care, adherence to prescribed medication, and gradual weight-bearing as tolerated. Physical therapy is typically initiated during this period, focusing on range of motion, strengthening, and reducing swelling. The patient might use crutches or a walker initially, gradually progressing to less support. We often use the RICE protocol (Rest, Ice, Compression, Elevation) to manage swelling and pain. A specific example would be a patient transitioning from non-weight bearing on crutches to partial weight bearing with a walker within a couple of weeks.
Intermediate Post-Op (Weeks 6-12): Focus shifts to regaining strength and proprioception (body awareness and balance). More challenging exercises are introduced, and the patient may start to participate in low-impact activities. Regular follow-up appointments with both the surgeon and the physical therapist are critical to monitor progress and make adjustments to the plan as needed. An example at this stage would be the gradual introduction of exercises that mimic movements required for daily life, such as stair climbing and walking on uneven terrain.
Late Post-Op (Months 3-6 and beyond): This involves continued strengthening, improving functional mobility, and eventually return to previous activity levels, as approved by the surgeon. Return to sports or high-impact activities may require a graded exposure strategy to avoid re-injury.
Patient education is a cornerstone of post-operative care. We provide clear instructions regarding medication, wound care, physical therapy exercises, and potential complications to watch for. We also establish realistic expectations regarding recovery timelines and potential limitations. Open communication and regular follow-up visits ensure we can address any issues that arise promptly.
Q 23. Explain the process of using custom orthotics in managing foot and ankle conditions.
Custom orthotics are individually designed shoe inserts aimed at correcting biomechanical abnormalities in the foot and ankle. The process begins with a thorough clinical examination, including a detailed history and physical assessment. This helps identify the underlying foot and ankle problem. For instance, we might find that a patient with plantar fasciitis has excessive pronation (inward rolling of the foot).
Next, a comprehensive foot and ankle assessment is done, including gait analysis (observing how the patient walks) and possibly a static and dynamic foot pressure measurement. This detailed evaluation informs the design of the orthotics.
A plaster cast or 3D scan of the patient’s foot is then created. This data is used by a certified orthotist to fabricate the custom orthotic. The orthotics are usually made from materials like polypropylene, carbon fiber, or other materials depending on the individual’s needs. These materials offer support and cushioning, correcting any identified abnormalities.
Once the orthotics are ready, the patient is fitted, and instructions are given on how to wear and care for them. Follow-up appointments are scheduled to monitor the efficacy of the orthotics and to make any necessary adjustments. Custom orthotics are beneficial for many conditions, including plantar fasciitis, flat feet, high arches, and post-surgical rehabilitation. They help redistribute weight, reduce strain on specific structures, and promote proper foot function.
Q 24. What are the common causes of hallux valgus (bunion) formation?
Hallux valgus, or bunion, is a deformity characterized by the lateral deviation of the big toe. Several factors contribute to its formation:
Genetics: A family history of bunions significantly increases the risk. Inherited foot structure can predispose individuals to this condition.
Footwear: Tight-fitting, narrow-toed shoes are a major contributor. The constant pressure and friction on the big toe joint cause the bone to shift laterally.
Biomechanics: Abnormal foot mechanics, such as overpronation (excessive inward rolling of the foot), can strain the joint and lead to bunion development.
Rheumatoid Arthritis: This inflammatory condition can affect the joints of the foot, leading to deformities, including bunions.
Other Conditions: Certain neurological conditions can also play a role.
Often, it’s a combination of these factors that leads to bunion formation. It’s important to note that while shoes are a major factor, genetics predisposes people to bunions, thus, even if a person doesn’t wear high heels, they could still develop a bunion.
Q 25. Describe different surgical techniques for hallux valgus correction.
Surgical correction of hallux valgus is considered when conservative measures (orthotics, medications, and shoe modifications) fail to provide relief. Several surgical techniques are available, each with its own advantages and disadvantages:
Osteotomy: This involves reshaping the bone to realign the big toe. Various types of osteotomies exist, depending on the severity of the deformity.
Arthrodesis (Fusion): This procedure involves fusing the bones of the big toe joint to reduce pain and stabilize the joint. It’s often used in cases of severe arthritis or joint instability.
Soft Tissue Procedures: These techniques address soft tissue imbalances, such as ligament tightness, which might contribute to the bunion deformity.
The choice of surgical technique is determined based on individual factors, such as the severity of the deformity, the presence of arthritis, patient age, and activity level. A thorough preoperative evaluation is crucial to determine the most suitable approach for each patient. Post-operative care is essential for a successful outcome, encompassing pain management, immobilization, and rehabilitation.
Q 26. How do you manage a patient with diabetic foot ulcers?
Managing diabetic foot ulcers requires a multidisciplinary approach due to the high risk of infection and complications. The core principles are prevention, prompt treatment, and meticulous wound care.
Initial Assessment: A thorough examination includes assessing the depth and size of the ulcer, the presence of infection (signs of redness, warmth, swelling, pus, and foul odor), and the patient’s overall vascular health (checking pulses and circulation). Neurological examination is equally crucial to assess for neuropathy (nerve damage) which might contribute to the ulcer’s formation.
Wound Care: This involves regular debridement (removal of dead tissue) to promote healing. The wound is typically cleaned and dressed appropriately, using specialized dressings that promote a moist healing environment. Infection control is paramount, often using antibiotics (systemic or topical) as needed. Offloading is critical to reduce pressure on the ulcer, using techniques like specialized footwear, crutches, or even total contact casts.
Vascular Assessment: Patients with diabetic foot ulcers often have underlying vascular disease (peripheral arterial disease). Vascular assessment might involve tests such as ankle-brachial index (ABI) to check blood flow to the feet. Intervention might involve angioplasty or bypass surgery to improve circulation.
Team Approach: Management is best done collaboratively, involving podiatrists, vascular surgeons, endocrinologists, infectious disease specialists, and other healthcare professionals. Regular follow-up visits are vital to monitor healing progress and manage any complications that arise.
Q 27. Explain the significance of nerve conduction studies in foot and ankle pathology.
Nerve conduction studies (NCS) are crucial diagnostic tools in evaluating foot and ankle pathology, particularly conditions affecting the nerves. NCS measures the speed and amplitude of nerve signals, helping to identify nerve damage or dysfunction. In foot and ankle problems, NCS can help diagnose:
Peripheral Neuropathy: NCS can reveal the presence and severity of nerve damage often associated with diabetes, alcohol abuse, or other causes. This manifests as decreased sensation, pain, or numbness in the feet.
Tarsal Tunnel Syndrome: This involves compression of the tibial nerve in the tarsal tunnel (behind the medial malleolus). NCS can pinpoint the location and extent of nerve compression.
Morton’s Neuroma: This is a thickening of the nerve tissue between the metatarsal heads (bones of the foot). NCS can help confirm the diagnosis.
Other Nerve Entrapments: NCS can help diagnose other nerve compressions or injuries affecting the foot and ankle.
The procedure involves placing small surface electrodes on the skin over the nerves. Mild electrical stimuli are delivered, and the response is measured. The results help differentiate between different types of nerve damage, guide treatment, and monitor the effectiveness of interventions.
Q 28. What are the different types of injections used in managing foot and ankle pain?
Various injections are used to manage foot and ankle pain, each targeting specific conditions:
Corticosteroid Injections: These are commonly used to reduce inflammation in conditions such as plantar fasciitis, tendinitis, and bursitis. The corticosteroid reduces pain and swelling, providing temporary relief.
Hyaluronic Acid Injections: These injections are used to lubricate joints affected by osteoarthritis, improving joint function and reducing pain. They are used for osteoarthritis affecting the ankle or smaller joints of the foot.
Platelet-Rich Plasma (PRP) Injections: PRP therapy involves injecting concentrated platelets derived from the patient’s own blood into the injured area. Platelets help heal damaged tissue, promoting regeneration.
Anesthetic Injections: Local anesthetics, such as lidocaine, can provide temporary pain relief for diagnostic purposes or before other interventions. Sometimes, a combination of anesthetic and corticosteroid is used for greater pain reduction and inflammation control.
Sclerotherapy: This involves injecting a solution into the blood vessel to reduce blood flow. This is used for vascular malformations and venous insufficiency in the leg and foot.
It is important to note that injections are not a cure for underlying conditions. They offer temporary pain relief and can aid in reducing inflammation, improving joint function, and promoting healing. They are often combined with other treatments such as physical therapy, orthoses, and lifestyle modifications.
Key Topics to Learn for Ankle and Foot Sprains and Injuries Management Interview
- Anatomy and Biomechanics: Understanding the intricate structure of the ankle and foot, including ligaments, tendons, bones, and muscles, and how they function during weight-bearing and movement.
- Common Sprains and Fractures: Differentiating between various types of ankle and foot sprains (e.g., inversion, eversion) and fractures, including their mechanisms of injury and clinical presentations.
- Diagnostic Imaging Interpretation: Analyzing X-rays, MRI, and CT scans to identify fractures, ligament tears, and other injuries accurately.
- Conservative Management: Detailed knowledge of RICE protocol (Rest, Ice, Compression, Elevation), bracing, taping techniques, and therapeutic exercises for non-surgical management.
- Surgical Management: Understanding various surgical procedures for ankle and foot injuries, including their indications, contraindications, and post-operative care.
- Rehabilitation and Recovery: Developing comprehensive rehabilitation plans, including range of motion exercises, strengthening programs, and functional activities to restore optimal mobility and function.
- Patient Assessment and Communication: Mastering effective patient history taking, physical examination techniques, and clear communication of diagnosis and treatment plans.
- Differential Diagnosis: The ability to distinguish between ankle and foot sprains and other conditions that might present similarly (e.g., nerve entrapment, tendonitis).
- Complication Management: Recognizing and addressing potential complications such as chronic pain, instability, infection, and delayed healing.
- Evidence-Based Practice: Staying current with the latest research and guidelines to ensure the best possible patient care.
Next Steps
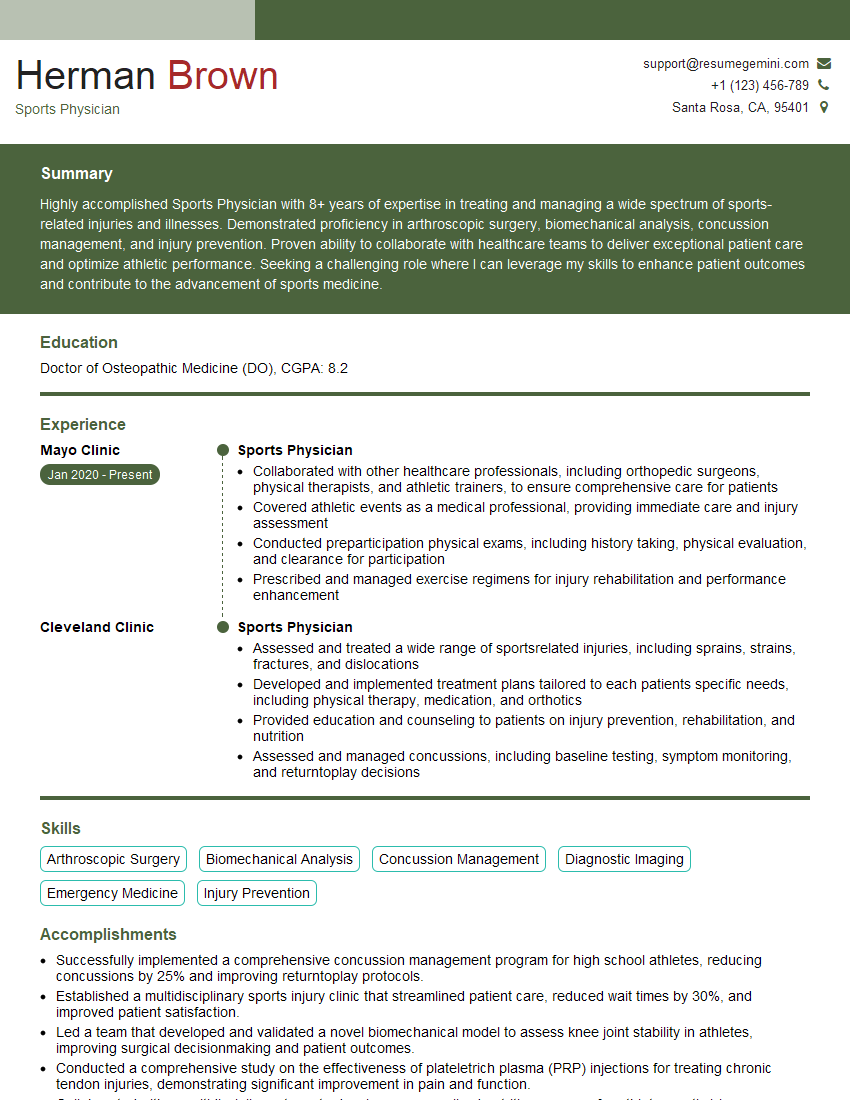
Mastering Ankle and Foot Sprains and Injuries Management is crucial for career advancement in orthopedics, sports medicine, and podiatry. A strong understanding of these concepts will significantly enhance your interview performance and open doors to exciting opportunities. To increase your chances of landing your dream job, create an ATS-friendly resume that highlights your skills and experience effectively. We highly recommend using ResumeGemini, a trusted resource for building professional resumes. ResumeGemini provides examples of resumes tailored to Ankle and Foot Sprains and Injuries Management, giving you a head start in showcasing your qualifications. Take the next step towards your successful career today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.