Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Assessment and Treatment of Depression in Older Adults interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Assessment and Treatment of Depression in Older Adults Interview
Q 1. Describe the diagnostic criteria for major depressive disorder in older adults according to DSM-5.
The DSM-5 diagnostic criteria for Major Depressive Disorder (MDD) apply to older adults, but with careful consideration of age-related changes. The core symptom is a persistently depressed mood or loss of interest or pleasure in activities for at least two weeks, accompanied by at least four other symptoms. These could include changes in weight or appetite, sleep disturbances (insomnia or hypersomnia), psychomotor agitation or retardation, fatigue or loss of energy, feelings of worthlessness or excessive guilt, diminished concentration or indecisiveness, and recurrent thoughts of death or suicide. It’s crucial to understand that some symptoms, like fatigue or sleep disturbances, are common in aging, so careful clinical judgment is required to distinguish these from MDD symptoms. For example, an older adult might report insomnia, but further investigation reveals that this is secondary to chronic pain, not a primary symptom of depression. The clinician must also be mindful of potential somatic masking of depressive symptoms, where physical complaints overshadow the emotional distress.
Q 2. What are the common presentations of depression in older adults that differ from younger populations?
Depression in older adults can present differently than in younger populations. While younger adults might experience sadness, irritability, and anger, older adults may present with more subtle or somatic symptoms. They might complain of physical aches and pains, fatigue, unexplained weight loss, or digestive problems without directly mentioning feelings of sadness or hopelessness. Cognitive slowing and memory problems can also be prominent, often mistaken for early dementia. For instance, an older adult might struggle with everyday tasks like paying bills or preparing meals, not because of cognitive decline, but because of depression-related apathy and lack of motivation. Another important difference is the increased prevalence of anxiety symptoms co-occurring with depression in older adults. This can lead to a more complex clinical picture, requiring a comprehensive assessment.
Q 3. Explain the role of physical health in assessing and treating depression in the elderly.
Physical health plays a significant role in both assessing and treating depression in older adults. Many medical conditions—such as hypothyroidism, cardiovascular disease, or vitamin deficiencies—can mimic or exacerbate depressive symptoms. Conversely, depression can worsen the management of chronic illnesses, leading to a vicious cycle. A thorough medical evaluation is essential to rule out or address any underlying medical issues that might contribute to depressive symptoms. For example, an older adult presenting with fatigue and low mood should undergo blood tests to check for anemia or thyroid problems. Treatment needs to be holistic, integrating medical management of physical conditions with psychological interventions to treat the depression. This collaborative approach, involving physicians, nurses, and mental health professionals, is crucial for effective care.
Q 4. Discuss the limitations of using standard depression screening tools in older adults.
Standard depression screening tools, while useful, have limitations in older adults. Many scales rely on self-report, which can be affected by cognitive impairment, physical limitations, or communication difficulties. Some items might be culturally inappropriate or not reflect the way older adults experience depression. For example, a question about loss of interest in social activities might be difficult to interpret if the individual has decreased mobility or reduced social networks due to age-related factors. Furthermore, some older adults might have difficulty understanding complex wording or scoring systems. Therefore, a comprehensive assessment should combine multiple methods, including clinical interviews, observation of behaviour, and information from family members or caregivers, in addition to using validated tools adapted for older adults, such as the Geriatric Depression Scale (GDS).
Q 5. How would you differentiate between depression and dementia in an older adult?
Differentiating between depression and dementia can be challenging but crucial for accurate diagnosis and treatment. Depression can mimic cognitive symptoms like memory problems and slowed thinking, but these symptoms in depression usually fluctuate and are often accompanied by mood disturbances and other depressive symptoms. In dementia, cognitive decline is usually progressive, persistent, and affects multiple cognitive domains (memory, language, executive function). Careful assessment includes thorough cognitive testing (e.g., Mini-Mental State Examination, MMSE), detailed history, and observation of behaviour. A crucial point is that depression can coexist with dementia, complicating the clinical picture further, requiring treatment strategies for both conditions simultaneously. For example, an older adult might show some memory impairment, but further assessment reveals a depressive mood, feelings of hopelessness, and sleep disturbance; these suggest a primary depressive disorder rather than dementia. However, it is crucial to rule out other causes of cognitive impairment before assuming depression as the primary issue.
Q 6. What are the ethical considerations in treating depression in older adults with cognitive impairment?
Ethical considerations in treating depression in older adults with cognitive impairment are paramount. Capacity to consent to treatment must be carefully evaluated. If the individual lacks capacity, decisions regarding treatment must be made by a legally authorized surrogate (e.g., family member) after careful consideration of the individual’s best interests and wishes expressed previously, if available. The treatment plan should be tailored to the person’s specific cognitive and functional abilities. Transparency and clear communication with the family and caregivers are crucial. Risks and benefits of various treatment options must be explained in a clear and understandable way. Confidentiality must be maintained, but information sharing may be necessary to coordinate care among different healthcare providers. For example, if an individual with dementia lacks capacity, a family member might make the decision about starting antidepressant medication. It is ethical to provide only treatment options that are least intrusive and still provide significant benefit.
Q 7. Describe the advantages and disadvantages of different antidepressant classes in older adults.
Several antidepressant classes are used in older adults, each with advantages and disadvantages. Selective Serotonin Reuptake Inhibitors (SSRIs) are often preferred due to a generally favorable side effect profile, but they can cause gastrointestinal issues, sexual dysfunction, and, in some cases, hyponatremia (low sodium levels) in older adults, who are more susceptible. Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) can be effective but carry a slightly higher risk of hypertension and may worsen urinary problems. Tricyclic antidepressants (TCAs) and monoamine oxidase inhibitors (MAOIs) are generally avoided in older adults due to their potential for significant side effects, particularly anticholinergic effects (e.g., constipation, dry mouth, confusion), which can be problematic in this population. Dosage adjustments are often necessary in older adults due to age-related changes in metabolism and drug interactions. Close monitoring of side effects and regular assessment of treatment response are crucial. The choice of antidepressant should be individualized based on the patient’s specific medical conditions, other medications, and preferences.
Q 8. How would you manage antidepressant side effects in an elderly patient?
Managing antidepressant side effects in older adults requires a delicate balance of efficacy and safety. Many commonly used antidepressants carry a higher risk of side effects in this population due to age-related changes in metabolism and organ function. For example, anticholinergic side effects like constipation, dry mouth, blurred vision, and urinary retention are more common and potentially debilitating in older individuals. Sedation, orthostatic hypotension (a sudden drop in blood pressure upon standing), and falls are also significant concerns.
My approach involves:
- Careful medication selection: I often prefer antidepressants with a lower risk of anticholinergic effects, such as sertraline or citalopram. Starting with low doses and gradually increasing them is crucial to minimize side effects.
- Monitoring and adjustment: Regular monitoring of vital signs, including blood pressure and heart rate, is essential. I closely track side effects and adjust the dosage or switch medications as needed. For instance, if a patient experiences significant constipation, I might add a stool softener.
- Non-pharmacological strategies: Addressing side effects can sometimes involve lifestyle modifications. For example, increasing fluid intake can help alleviate dry mouth, and implementing fall prevention strategies (like improving home safety) reduces the risk of falls associated with orthostatic hypotension or sedation.
- Patient education and collaboration: I emphasize open communication with my patients. Understanding the potential side effects and how to manage them is vital for adherence and safety. I encourage patients to report any new or worsening symptoms.
For example, I had a patient who experienced significant sedation with a higher dose of sertraline. We lowered the dose and added a short course of non-pharmacological sleep hygiene techniques. This approach significantly improved her daytime functioning while maintaining adequate antidepressant effects.
Q 9. Explain the role of psychotherapy in treating depression in older adults.
Psychotherapy plays a vital role in treating depression in older adults, often complementing medication. It helps individuals understand and address the underlying causes of their depression, develop coping skills, and improve their overall well-being. Unlike medication that primarily targets neurotransmitter levels, psychotherapy equips older adults with tools to actively manage their emotional and psychological health.
The benefits of psychotherapy extend beyond symptom reduction. It helps patients develop self-awareness, identify negative thought patterns, and learn more adaptive ways of thinking and behaving. It can also help to address potential contributing factors like grief, loss, social isolation, and medical comorbidities. Many older adults also find therapeutic value in simply having a supportive and non-judgmental relationship with a therapist.
Q 10. What types of psychotherapy are most effective for older adults with depression?
Several types of psychotherapy are effective for older adults with depression. The most commonly used and supported by research include:
- Cognitive Behavioral Therapy (CBT): CBT focuses on identifying and changing negative thought patterns and behaviors that contribute to depression. It’s particularly effective in teaching practical coping skills for managing symptoms.
- Problem-Solving Therapy: This approach helps individuals identify and resolve specific problems contributing to their depression. It’s often helpful for individuals experiencing situational depression related to life changes or challenges.
- Interpersonal Therapy (IPT): IPT focuses on improving interpersonal relationships that may be contributing to or exacerbating the depression. This is especially relevant for older adults who may be struggling with bereavement, social isolation, or relationship conflicts.
The choice of therapy depends on the individual’s specific needs and preferences. A thorough assessment is crucial to determine the most suitable approach. It’s also important to consider the patient’s cognitive abilities, physical limitations, and social support system when selecting and adapting a therapeutic intervention.
Q 11. Describe your approach to assessing suicidal ideation in an older adult.
Assessing suicidal ideation in older adults requires a sensitive and thorough approach. It’s crucial to remember that suicide risk can be masked or overlooked in this population. Older adults may be less likely to explicitly verbalize suicidal thoughts, instead presenting with subtle cues like hopelessness, withdrawal, or expressions of feeling like a burden.
My approach involves:
- Direct, open-ended questions: I use direct but empathetic language, such as, “Have you been having any thoughts of harming yourself?” or “Have you been feeling hopeless or like life isn’t worth living?”
- Assessing risk factors: I consider factors such as medical illnesses, social isolation, loss, history of previous suicide attempts, and access to lethal means.
- Behavioral observations: I pay close attention to nonverbal cues like changes in mood, appearance, or behavior.
- Collaboration with family and caregivers: When appropriate and with the patient’s consent, I involve family members or caregivers to gather additional information and assess the patient’s overall situation.
- Use of standardized assessment tools: Instruments like the Geriatric Depression Scale or the Patient Health Questionnaire-9 (PHQ-9) can help in the assessment.
If suicidal ideation is present, I prioritize safety planning and may involve hospitalization if the risk is considered imminent. It’s essential to be proactive and supportive, offering a safe and understanding environment for the patient to discuss their feelings.
Q 12. How would you manage a patient with depression and comorbid anxiety?
Managing depression and comorbid anxiety in older adults requires a comprehensive approach that addresses both conditions simultaneously. These two disorders often share overlapping symptoms and risk factors, making integrated management crucial for optimal outcomes.
My strategy usually involves:
- Medication management: Selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) are often effective in treating both depression and anxiety. The choice of medication depends on the specific symptoms and potential side effects. I may also consider adjunctive medications for anxiety symptoms if needed.
- Psychotherapy: CBT and other evidence-based psychotherapies can be highly effective in addressing both anxiety and depression. Techniques to manage anxiety, such as relaxation training or mindfulness-based stress reduction, are often incorporated.
- Lifestyle interventions: Encouraging regular exercise, adequate sleep, a healthy diet, and stress management techniques can have a positive impact on both depression and anxiety symptoms.
- Regular monitoring and adjustment: Close monitoring of symptoms is crucial to ensure the effectiveness of the treatment plan. Adjustments to medication or therapy may be necessary based on the patient’s response.
For example, a patient might benefit from CBT to address underlying anxiety, alongside an SSRI to improve mood and reduce both depressive and anxiety symptoms.
Q 13. How do you address the impact of depression on functional abilities in older adults?
Depression significantly impacts functional abilities in older adults, leading to decreased participation in activities of daily living (ADLs), social isolation, and a decline in overall quality of life. Addressing this impact is crucial for improving overall well-being and preventing further decline.
My approach involves:
- Functional assessment: I systematically assess the patient’s ability to perform ADLs, such as bathing, dressing, and eating, as well as instrumental activities of daily living (IADLs), such as managing finances or medication. This helps identify areas where support is needed.
- Targeted interventions: Based on the assessment, I may recommend interventions like occupational therapy to improve ADL performance, assistance with IADLs from family, friends, or home health aides, or adaptive equipment to enhance functional independence.
- Psychoeducation: Educating the patient and their caregivers about the link between depression and functional decline is crucial for motivation and adherence to treatment.
- Gradual increase in activity: Encouraging a gradual increase in physical activity and social engagement can improve mood and functional capacity, but must be tailored to individual physical limitations.
- Collaboration with other professionals: Working with other professionals, such as geriatricians, social workers, and occupational therapists, is crucial for a holistic approach.
For example, a patient with depression may struggle with meal preparation. We might refer them to a nutritionist or home-delivered meals service to help address this need and improve their overall well-being.
Q 14. Discuss the importance of involving family members in the treatment of depression in older adults.
Involving family members in the treatment of depression in older adults is often essential. They can provide invaluable support, insight, and practical assistance. However, maintaining patient confidentiality and respecting their autonomy remains paramount.
My approach involves:
- Gaining informed consent: Before involving family, I obtain explicit permission from the patient. I explain the purpose of involving family and clarify what information will be shared.
- Collaborative communication: I encourage open communication between the patient, family, and myself. This promotes a shared understanding of the illness, treatment plan, and progress.
- Education and support: I provide family members with information about depression, treatment options, and strategies for supporting their loved one.
- Caregiver burden assessment: I assess the burden on caregivers, addressing any challenges they face in providing care. This may involve referrals to caregiver support groups or respite care services.
- Addressing family dynamics: I address any underlying family dynamics that may be contributing to the patient’s depression or hindering their recovery.
Open communication and collaboration help build a strong support network for the patient, enhancing adherence to treatment and improving outcomes. It also empowers family members to become active participants in their loved one’s care.
Q 15. Explain your approach to medication management for an older adult with multiple comorbidities.
Medication management in older adults with multiple comorbidities requires a highly individualized approach, prioritizing safety and efficacy. We must carefully consider potential drug interactions, age-related physiological changes (like decreased renal and hepatic function), and the presence of other health conditions. For example, a patient with depression, heart failure, and diabetes might require a lower starting dose of an antidepressant, perhaps an SSRI like sertraline, and close monitoring for side effects like hyponatremia (low sodium) or QT prolongation (a heart rhythm issue). We’d also collaborate closely with other specialists, such as a cardiologist or endocrinologist, to ensure medication choices are safe and compatible with their existing treatment plans. Regular blood tests to monitor liver and kidney function are crucial. We also need to consider non-pharmacological approaches, like psychotherapy, which can be very effective in reducing medication side effects and overall burden. The goal is always to achieve symptom relief while minimizing risks and improving overall quality of life.
Starting low and going slow is paramount. We often begin with a low dose of an antidepressant and gradually increase it over several weeks, closely monitoring for both effectiveness and side effects. This phased approach is especially vital in older adults, who may be more susceptible to adverse drug reactions.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are some common barriers to accessing mental health care for older adults?
Several significant barriers hinder older adults’ access to mental health care. One major factor is the stigma associated with mental illness. Many older adults, influenced by societal attitudes from previous generations, are reluctant to seek help, believing depression is a sign of weakness or something they should simply ‘tough out’. Financial limitations are another significant hurdle, especially for those on fixed incomes who may not have adequate health insurance coverage or the resources to afford private therapy. Geographic isolation is also a critical issue, as many older adults live in rural areas with limited access to mental health professionals. Transportation challenges can also limit their ability to attend appointments. Furthermore, difficulty navigating the complex healthcare system adds to the barrier, especially if they have cognitive impairments or a lack of support systems.
- Stigma: Overcoming the shame and fear associated with mental illness.
- Financial Barriers: Ensuring affordable access to mental healthcare services.
- Geographic Limitations: Improving accessibility in rural and underserved areas.
- Navigational Challenges: Simplifying the healthcare system for easier access to needed services.
Q 17. How would you assess for substance abuse in an older adult presenting with depression?
Assessing for substance abuse in an older adult with depression requires a sensitive and comprehensive approach. It’s important to remember that substance abuse can mask or exacerbate depression, creating a complex interplay. My assessment would involve a detailed history, including questions about alcohol use (frequency, amount, type), use of prescription medications (both prescribed and obtained without prescriptions), and use of illicit drugs. I would use validated screening tools such as the CAGE questionnaire for alcohol and similar tools for other substances. It’s crucial to ask these questions directly, without judgment, creating a safe space for open conversation. Physical examination should assess for signs of malnutrition, liver damage, or other substance-related health problems. Laboratory tests might be ordered to confirm or rule out substance use. The information gathered is then used to develop a treatment plan that addresses both the depression and the substance use issue, perhaps with referral to specialized addiction services.
Remember, older adults may be less likely to report substance use due to fear of judgment, or even be unaware they have a problem. A gentle and empathetic approach is crucial for obtaining accurate information.
Q 18. Discuss the role of social support in managing depression in older adults.
Social support plays a vital role in managing depression among older adults. Strong social connections provide a buffer against the negative impacts of life stressors and promote emotional well-being. Individuals with strong social networks tend to have better coping mechanisms and experience fewer depressive symptoms. Conversely, social isolation and loneliness are strongly associated with an increased risk of depression in older adults. Interventions that enhance social support may involve connecting individuals with support groups, encouraging participation in community activities tailored to their interests and abilities, and facilitating connections with family and friends. For some, this might mean home visits from social workers or volunteers to provide companionship and assistance with daily tasks. Ultimately, a supportive network helps individuals feel valued, connected, and less alone, which is critical for recovery.
Q 19. How would you address the impact of bereavement on an older adult’s mental health?
Bereavement can significantly impact an older adult’s mental health, sometimes triggering or worsening depression. The grief process is highly individual, but prolonged or complicated grief can lead to persistent sadness, loss of interest in activities, and feelings of hopelessness. My approach involves actively listening to their experiences, validating their feelings, and providing emotional support. I’d help them understand that their grief is a normal reaction to loss and emphasize that it’s okay to feel a range of emotions. Cognitive Behavioral Therapy (CBT) techniques can be beneficial in managing maladaptive thoughts and behaviors associated with grief, helping them develop healthier coping strategies. I’d also assess for signs of complicated grief, such as intense yearning for the deceased or persistent difficulty functioning. In cases of complicated grief, specialized therapy might be recommended.
It’s essential to acknowledge the uniqueness of each individual’s grief and avoid pressuring them to ‘move on’. Patience and understanding are crucial during this challenging time.
Q 20. What are the key components of a comprehensive geriatric assessment for depression?
A comprehensive geriatric assessment for depression goes beyond a simple diagnosis and involves a holistic evaluation of the individual’s physical, psychological, and social functioning. It considers age-related changes and the impact of multiple comorbidities. Key components include:
- Detailed history: Including medical history, medication list, social history, family history of mental illness, and recent life events (e.g., bereavement, loss of independence).
- Mental status examination: Assessing cognitive function, mood, thought content, and perception.
- Physical examination: Ruling out physical conditions that may mimic depression.
- Functional assessment: Evaluating activities of daily living (ADLs) and instrumental activities of daily living (IADLs) to assess independence.
- Social assessment: Exploring social support networks and identifying sources of isolation or loneliness.
- Diagnostic assessment using standardized questionnaires: Such as the Geriatric Depression Scale (GDS) or Patient Health Questionnaire-9 (PHQ-9), these provide objective measures of depressive symptoms.
- Laboratory tests: As indicated to rule out medical causes of depressive symptoms or to monitor medication side effects.
The goal is to create a comprehensive picture of the individual’s situation and develop a tailored treatment plan that addresses all contributing factors.
Q 21. Describe your experience with different types of cognitive behavioral therapy (CBT) techniques.
My experience encompasses various CBT techniques for older adults, adapting the approach to suit their cognitive abilities and preferences. These include:
- Cognitive Restructuring: Identifying and challenging negative or distorted thought patterns that contribute to depression. For example, an older adult who blames themselves for a recent fall might be guided to reframe this thought, considering external factors such as slippery surfaces.
- Behavioral Activation: Encouraging engagement in pleasurable activities and social interactions to increase positive mood and reduce avoidance behaviors. This could involve gradually increasing participation in enjoyable hobbies or social gatherings.
- Problem-Solving Therapy: Developing skills to effectively address challenging life situations and reduce feelings of helplessness. For instance, if a patient is struggling with financial difficulties, we might work collaboratively to explore potential solutions.
- Relaxation Techniques: Incorporating mindfulness, meditation, or deep breathing exercises to manage stress and anxiety. These techniques can be particularly beneficial in reducing sleep disturbances associated with depression.
I tailor the pace and intensity of CBT to the individual’s needs, ensuring a comfortable and engaging therapeutic experience. The emphasis is on collaboration, empowerment, and building self-efficacy.
Q 22. Explain your understanding of the role of neurotransmitters in depression.
Depression is intricately linked to imbalances in neurotransmitters, the chemical messengers in our brain. These imbalances disrupt communication between brain cells, affecting mood, sleep, appetite, and other functions. Key neurotransmitters involved include serotonin, norepinephrine, and dopamine.
Serotonin is often associated with feelings of well-being and happiness. Low serotonin levels are frequently implicated in depression. Imagine serotonin as a key that unlocks feelings of calm and contentment. If there aren’t enough keys, the door to positive emotions remains locked.
Norepinephrine plays a role in alertness and focus. Low levels can contribute to fatigue, lack of motivation, and difficulty concentrating, common symptoms of depression. Think of norepinephrine as the engine that drives energy and focus. A weakened engine leads to sluggishness and a lack of drive.
Dopamine is related to pleasure, reward, and motivation. Reduced dopamine levels can lead to anhedonia (loss of interest in pleasurable activities), a hallmark of depression. Dopamine is like the reward system in our brain; if it malfunctions, we lose the motivation to pursue things that normally bring us joy.
Understanding these neurotransmitter systems is crucial for selecting appropriate treatments, as antidepressants primarily work by modulating the levels or activity of these neurochemicals.
Q 23. Discuss the use of electroconvulsive therapy (ECT) in treating severe depression in older adults.
Electroconvulsive therapy (ECT) is a safe and effective treatment for severe depression in older adults, especially when other treatments have failed. It involves passing brief electrical currents through the brain, inducing a controlled seizure. This seizure seems to reset brain activity, improving symptoms.
While the exact mechanism isn’t fully understood, it’s believed to impact neurotransmitter systems and brain plasticity, ultimately alleviating depressive symptoms. It’s important to emphasize that modern ECT is significantly different from its portrayal in older media. It’s administered under anesthesia with muscle relaxants, minimizing discomfort and potential side effects.
In older adults, ECT can be particularly beneficial because it’s often rapid-acting, which is important for individuals experiencing acute suicidal ideation or severe functional impairment. However, it’s essential to carefully assess the individual’s overall health and cognitive status before considering ECT, and to carefully monitor for any side effects, such as temporary memory issues, which are usually mild and resolve quickly.
The decision to use ECT is made collaboratively with the patient, their family (if desired), and a multidisciplinary team.
Q 24. How do you monitor treatment efficacy and make adjustments as needed?
Monitoring treatment efficacy involves a multifaceted approach. We utilize various tools including regular assessments of mood, sleep, appetite, and energy levels using standardized rating scales such as the Geriatric Depression Scale (GDS) or the Hamilton Depression Rating Scale (HAM-D).
We also track functional capacity – how well the individual is able to perform daily activities. Regular discussions with the patient and their caregivers provide vital qualitative information. Changes in medication dosage or treatment strategies are made based on the response to treatment and potential side effects. For example, if the GDS scores show minimal improvement after four to six weeks of a specific antidepressant, we may increase the dosage, switch to a different medication, or add another treatment modality, like psychotherapy.
Regular blood tests may also be necessary to monitor for potential adverse effects of medication. Continuous monitoring and open communication with the patient are paramount to optimizing treatment outcomes and ensuring patient safety.
Q 25. What are the warning signs of medication interactions in the elderly concerning antidepressants?
Older adults are particularly vulnerable to medication interactions due to age-related changes in metabolism and organ function. Many medications commonly used in older adults, such as those for hypertension, heart conditions, or pain management, can interact with antidepressants.
Warning signs of these interactions might include:
- Increased drowsiness or confusion
- Falls or dizziness
- Changes in heart rate or blood pressure
- Gastrointestinal problems (nausea, vomiting, constipation)
- Cognitive impairment or worsening depression
- Bleeding tendencies (with some antidepressants)
It’s crucial to obtain a complete medication history, including over-the-counter medications and supplements, and to carefully monitor for these signs. Regular review of medications and close collaboration with other healthcare providers are essential to minimize the risk of harmful interactions.
Q 26. Describe your approach to communicating complex medical information to an older adult with depression.
Communicating complex medical information to an older adult with depression requires patience, empathy, and a tailored approach. We avoid using medical jargon; instead, we use plain language and simple explanations, checking for understanding at every step.
I prefer a collaborative approach, encouraging the patient to ask questions and participate actively in the decision-making process. Visual aids, such as diagrams or written summaries, can be incredibly helpful in clarifying concepts. Involving family members or caregivers, if the patient agrees, can also be supportive. It’s crucial to consider cognitive impairments that may be present, adjusting the pace and complexity accordingly and providing ample time for processing information.
For example, instead of saying, “We need to titrate your SSRI dosage,” I would explain, “We need to gradually increase your medication dose to find the right amount for you.”
Q 27. How do you handle a situation where an older adult is resistant to treatment?
Resistance to treatment is common, especially in older adults who may have experienced previous negative healthcare experiences or have concerns about side effects. The key is to understand the reasons behind the resistance.
A collaborative and empathetic approach is vital. I start by actively listening to the patient’s concerns and addressing them with respect. I might explore their fears regarding medication side effects, cost, or perceived loss of independence.
We may consider alternative treatment options, such as psychotherapy or lifestyle interventions like exercise or social engagement, incorporating their preferences wherever possible. We work together to develop a treatment plan that fits their lifestyle, values, and goals. If the resistance stems from a lack of understanding, reiterating information using simple language and visual aids, with patience and repeated explanations, can be helpful. In some cases, involving a trusted family member or friend can facilitate communication and improve treatment adherence.
Q 28. Explain your familiarity with resources and support systems available for older adults with depression.
Numerous resources and support systems are available for older adults with depression. These include:
- Mental health professionals: Psychiatrists, psychologists, and social workers specializing in geriatric mental health.
- Support groups: Connecting with others facing similar challenges can reduce feelings of isolation and provide valuable emotional support.
- Community-based organizations: Many organizations provide counseling, case management, and assistance with daily living needs.
- Healthcare providers: Primary care physicians and specialists play a crucial role in identifying and managing depression.
- Family and friends: Strong social support networks can make a significant difference in an older adult’s recovery.
- Online resources: Reputable websites and helplines offer information, support, and guidance.
I always ensure that my patients are aware of and connected with appropriate resources based on their individual needs and preferences. This includes providing information about local support groups, mental health clinics, and relevant online resources.
Key Topics to Learn for Assessment and Treatment of Depression in Older Adults Interview
- Differential Diagnosis: Understanding and differentiating depression from other conditions common in older adults (e.g., dementia, medical illnesses, medication side effects). This includes learning about relevant assessment tools and their limitations.
- Geriatric Assessment Tools: Proficiency in utilizing standardized assessments like the Geriatric Depression Scale (GDS), PHQ-9, and others relevant to older adults, understanding their strengths and weaknesses, and interpreting the results.
- Treatment Approaches: Familiarity with various treatment modalities including psychotherapy (e.g., cognitive behavioral therapy (CBT), problem-solving therapy), pharmacotherapy (considering medication side effects and interactions), and non-pharmacological interventions (e.g., exercise, social engagement).
- Ethical Considerations: Understanding the ethical challenges related to capacity, consent, and decision-making in older adults with depression, including the role of family members and caregivers.
- Practical Application: Developing a case conceptualization and treatment plan for a hypothetical patient, considering the unique challenges presented by aging and comorbidities.
- Cultural Competence: Recognizing and addressing the impact of cultural factors on the presentation, assessment, and treatment of depression in older adults from diverse backgrounds.
- Suicide Risk Assessment: Proficiently assessing and managing suicide risk in older adults, including the implementation of safety planning and collaborative care.
- Collaboration and Care Coordination: Understanding the importance of collaboration with other healthcare professionals (e.g., physicians, nurses, social workers) and family members in providing comprehensive care.
- Monitoring Treatment Response and Adjustment: Strategies for ongoing assessment of treatment efficacy and making necessary adjustments based on patient response and progress.
Next Steps
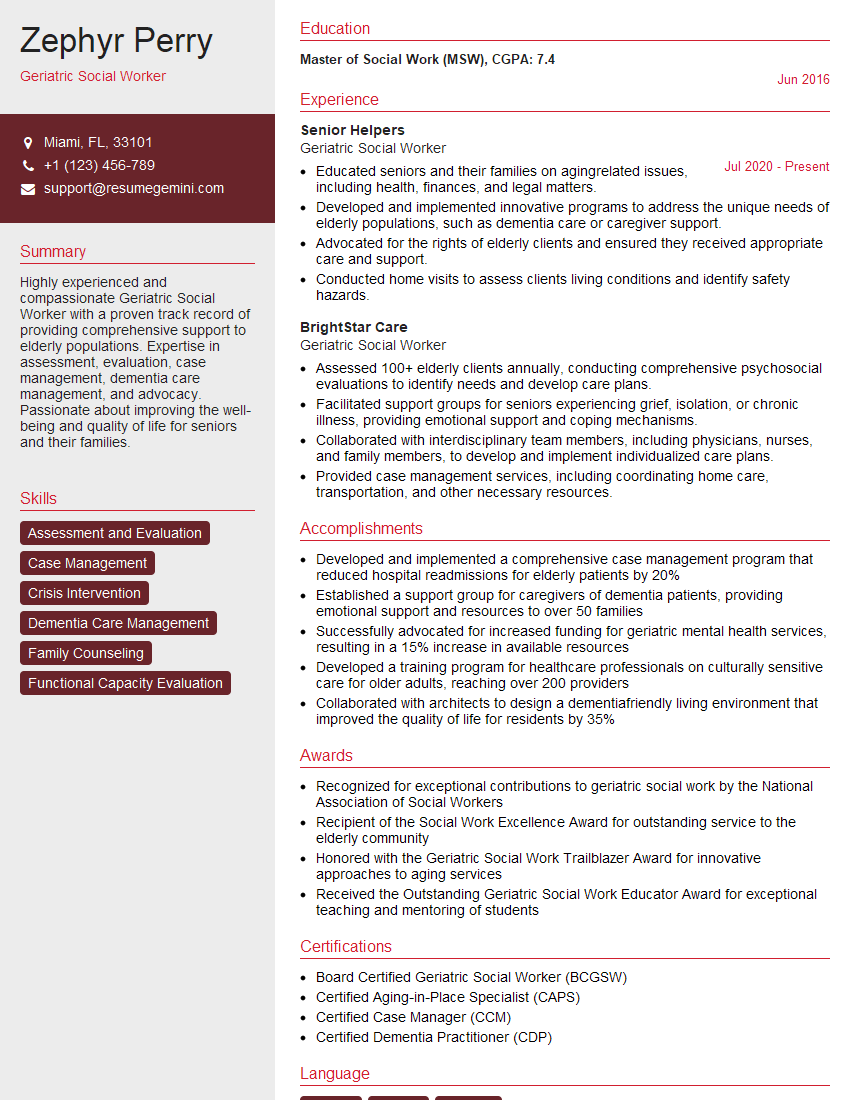
Mastering the assessment and treatment of depression in older adults is crucial for career advancement in geriatric mental health. It demonstrates a specialized skill set highly valued by employers. To maximize your job prospects, focus on creating a compelling and ATS-friendly resume that highlights your expertise. ResumeGemini is a trusted resource that can help you build a professional resume tailored to your skills and experience. We offer examples of resumes specifically designed for professionals in Assessment and Treatment of Depression in Older Adults to help guide you in showcasing your qualifications effectively.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.