The thought of an interview can be nerve-wracking, but the right preparation can make all the difference. Explore this comprehensive guide to Assessment of Anorectal Dysfunction interview questions and gain the confidence you need to showcase your abilities and secure the role.
Questions Asked in Assessment of Anorectal Dysfunction Interview
Q 1. Describe the different types of anorectal manometry.
Anorectal manometry is a group of tests that measure the pressures within the rectum and anal canal. These tests are crucial for diagnosing various anorectal dysfunctions. There are several types, each offering slightly different information:
- Standard Manometry: This is the most basic form, using a pressure-sensitive catheter inserted into the rectum and anal canal. It measures resting pressures, squeeze pressures (during voluntary contraction), and rectal distension pressures. Think of it like a blood pressure cuff for your anus, measuring how well it holds pressure.
- High-Resolution Anorectal Manometry (HRAM): This is an advanced technique using a catheter with multiple sensors, providing a more detailed picture of pressure changes throughout the anal canal. It’s like having many blood pressure cuffs along the entire length, giving a much more precise graph.
- Barostat Manometry: This technique involves inflating a balloon within the rectum to measure the sensation of rectal distension. It helps assess rectal sensitivity and compliance, essentially determining how much the rectum can stretch before the urge to defecate is triggered.
- Electromyography (EMG): While not strictly manometry, EMG is often performed concurrently. This assesses the electrical activity of the anal sphincter muscles, giving insights into their function and coordination. This is like checking the ‘electrical signals’ that tell those muscles when to contract and relax.
The choice of technique depends on the clinical suspicion and the information needed for diagnosis.
Q 2. Explain the indications for performing anorectal manometry.
Anorectal manometry is indicated for a variety of anorectal disorders, all related to difficulties with defecation or continence. Some key indications include:
- Fecal incontinence: Manometry helps identify the underlying cause, such as weak sphincter muscles or impaired rectal sensation.
- Constipation: It can assess rectal evacuation dysfunction (difficulty emptying the rectum), such as impaired rectal sensation or weak expulsive forces.
- Obstructed defecation: Manometry can help determine if there are issues with rectal emptying or pelvic floor dysfunction.
- Anal fissures or fistulas: It can evaluate sphincter function and help in surgical planning.
- Pelvic floor dysfunction: Manometry, alongside other tests, helps assess the coordination of the pelvic floor muscles and their contribution to defecation.
- Evaluation of post-surgical outcomes (e.g., after rectal surgery): To monitor the success of the surgery and identify potential complications.
In essence, manometry helps pinpoint exactly *why* a patient is experiencing anorectal symptoms.
Q 3. What are the limitations of anorectal manometry?
Despite its value, anorectal manometry has certain limitations:
- Patient cooperation: The procedure requires patient cooperation and ability to follow instructions. This can be challenging in some patients, especially those with cognitive impairment or severe pain.
- Subjectivity: Some aspects of the test, like sensation assessment, involve subjective reporting from the patient.
- Lack of standardization: There isn’t complete standardization across different manometry systems and interpretation methods, leading to potential variations in results.
- Limited information about the anatomical structures: Manometry primarily provides functional information; it doesn’t visualize the anatomical structures involved.
- Invasive nature: The procedure involves inserting a catheter, which might cause some discomfort for the patient.
Therefore, the results should always be interpreted in conjunction with other diagnostic tests and the patient’s clinical history for the most accurate diagnosis.
Q 4. How do you interpret the results of anorectal manometry?
Interpreting anorectal manometry results requires expertise. It’s not simply looking at single numbers but rather analyzing the entire pressure profile, including resting pressures, squeeze pressures, and rectal sensation. For instance:
- Low resting pressures: May suggest sphincter weakness, potentially contributing to incontinence.
- Poor squeeze pressures: Could indicate sphincter dysfunction leading to difficulty in maintaining continence.
- Reduced rectal sensation: Suggests a diminished awareness of rectal distension, potentially contributing to constipation and/or incontinence.
- Abnormal coordination between sphincters and pelvic floor: Could indicate a functional defecation disorder.
The interpretation takes into account the entire clinical picture, including the patient’s symptoms and other findings from the physical exam. For example, a patient with low resting pressures might not necessarily have fecal incontinence if their squeeze pressure is strong enough to compensate.
Q 5. Describe the procedure for performing a defecography.
Defecography, also known as a dynamic pelvic floor study, is a radiographic imaging technique used to evaluate the anorectal anatomy and function during defecation. The procedure typically involves:
- Preparation: The patient may need to have a bowel preparation to ensure the rectum is clear.
- Barium Contrast: A barium paste is usually given to the patient rectally.
- Imaging: A series of X-rays are taken as the patient performs various maneuvers, including straining, attempting defecation, and resting.
- Fluoroscopy: A real-time X-ray imaging (fluoroscopy) is often used to capture the dynamic movement of the pelvic floor muscles and the anorectum.
This technique creates a video-like sequence showing the entire process of defecation, allowing clinicians to identify structural and functional abnormalities.
Q 6. What information does a defecography provide?
Defecography provides crucial information about the anatomy and function of the anorectum and pelvic floor during defecation. This includes:
- Anal canal anatomy: Identifies any abnormalities such as rectal prolapse, rectocele, enterocele, or intussusception.
- Pelvic floor muscle function: Evaluates the coordination and strength of the pelvic floor muscles during defecation.
- Anorectal angle: Assesses the angle between the rectum and anal canal, which plays a role in continence.
- Rectal evacuation: Evaluates how effectively the rectum empties during defecation.
- Perineal descent: Measures how much the perineum descends during straining, which can be indicative of pelvic floor dysfunction.
This detailed information helps in the diagnosis and management of various anorectal disorders.
Q 7. What are the contraindications for a defecography?
Defecography, while helpful, has some contraindications:
- Pregnancy: Radiation exposure is a concern during pregnancy.
- Allergy to barium: Some individuals may have allergies to barium, which is used as the contrast agent.
- Severe inflammatory bowel disease: The procedure may exacerbate symptoms in patients with severe inflammatory bowel disease.
- Recent rectal surgery: The procedure may be contraindicated immediately after rectal surgery due to the risk of complications.
- Inability to cooperate: Patients need to be able to follow instructions and actively participate in the procedure.
A careful assessment of the patient’s condition is essential before proceeding with defecography to ensure patient safety and the validity of the results.
Q 8. Explain the different types of endoanal ultrasound.
Endoanal ultrasound (EUS) is a valuable imaging technique used to assess the anorectal region. There are primarily two types: static and dynamic.
- Static Endoanal Ultrasound: This is the most common type. A probe is inserted into the rectum, providing a cross-sectional image of the anal sphincter complex. It’s like taking a snapshot of the muscles and tissues in that area. This allows us to assess the thickness and integrity of the internal and external anal sphincters, as well as identify any lesions or abnormalities.
- Dynamic Endoanal Ultrasound: This type of EUS adds another dimension by imaging the anal sphincter complex while the patient performs specific maneuvers, such as squeezing or straining. Think of it as a video recording of the muscles in action. This helps in evaluating the functionality of the sphincter muscles and identifying any dynamic defects or incoordination, which might be missed on a static scan. This is particularly useful in assessing patients with fecal incontinence.
Q 9. What are the indications for performing an endoanal ultrasound?
Indications for performing an endoanal ultrasound are varied but primarily focus on investigating symptoms and conditions affecting the anorectum. These include:
- Fecal incontinence: To assess the integrity and function of the anal sphincter muscles. For example, we use it frequently to look for sphincter tears or defects in patients who have experienced anal trauma during childbirth.
- Constipation: To evaluate the presence of anorectal malformations, strictures, or other structural abnormalities which could contribute to constipation.
- Anal pain: To investigate the presence of fissures, abscesses, fistulas, or other painful conditions.
- Rectal prolapse: To assess the severity of the prolapse and the involvement of the anal sphincter muscles.
- Pre-operative assessment: Before surgical procedures involving the anorectum, EUS provides crucial information to guide treatment planning, such as surgical repair of sphincter defects.
Essentially, any patient presenting with symptoms suggesting dysfunction of the anal sphincter complex or abnormalities of the anorectal anatomy would benefit from an EUS.
Q 10. How do you interpret the results of an endoanal ultrasound?
Interpreting EUS results requires expertise and a systematic approach. The images reveal the thickness and echogenicity (brightness on the ultrasound) of the sphincter muscles and identify any structural anomalies.
- Sphincter thickness: Reduced thickness indicates muscle damage or atrophy, often associated with incontinence.
- Echogenicity: Changes in echogenicity can suggest inflammation or scarring.
- Lesions: EUS can detect lesions such as fissures, fistulas, abscesses, or tumors.
- Dynamic assessment: In dynamic EUS, the coordinated contraction of the sphincter muscles during maneuvers is crucial. Poor or uncoordinated contraction might indicate neuromuscular dysfunction.
We look at the overall picture, correlating the imaging findings with the patient’s clinical presentation to form a diagnosis and guide treatment. It’s a bit like putting together a puzzle, where each piece of information from the images, patient history, and physical examination contributes to the whole picture.
Q 11. Describe the procedure for performing a rectal biopsy.
Rectal biopsy is a relatively straightforward procedure where a small tissue sample is taken from the rectal lining for pathological examination under a microscope.
- Preparation: The patient is typically given a cleansing enema to clear the bowel before the procedure. Local anesthesia is administered to numb the area.
- Insertion of the instrument: A specialized instrument (e.g., a biopsy forceps) is carefully inserted into the rectum via the anus.
- Tissue sampling: The instrument is used to obtain a small sample of rectal tissue. Multiple biopsies might be taken depending on the indication.
- Withdrawal: The instrument is then withdrawn, and pressure is applied to the area to control bleeding.
- Histopathological analysis: The collected tissue sample is then sent to a laboratory for histopathological examination. A pathologist analyzes the tissue under a microscope to look for any abnormalities.
Minor bleeding or discomfort is possible afterward, but it usually resolves quickly. Post-procedure instructions are provided to the patient.
Q 12. What are the indications for performing a rectal biopsy?
Indications for a rectal biopsy include:
- Suspicion of malignancy: If a rectal mass or lesion is identified, a biopsy is necessary to confirm the diagnosis of cancer or other neoplasms.
- Inflammatory bowel disease (IBD): Rectal biopsy helps in differentiating between ulcerative colitis and Crohn’s disease, two common IBDs.
- Rectal bleeding: If the cause of rectal bleeding is not apparent through other investigations, a biopsy can help identify the source, such as polyps or other lesions.
- Infections: Rectal biopsies are sometimes used to diagnose infections or other inflammatory conditions affecting the rectum.
In essence, whenever there is a suspicion of pathology within the rectal wall, a biopsy provides a definitive diagnosis.
Q 13. How do you assess for fecal incontinence?
Assessing fecal incontinence requires a multi-faceted approach combining history taking, physical examination, and specialized investigations.
- Detailed history: The nature, frequency, and severity of incontinence episodes are assessed. We want to know what types of stool are being lost (liquid, solid), if there’s any urgency, and whether particular foods or activities trigger episodes. We also investigate any contributing factors like previous surgeries or neurological conditions.
- Physical examination: This includes a digital rectal examination to assess sphincter tone, perianal sensation, and any abnormalities.
- Anorectal physiology tests: These tests quantify sphincter function and rectal sensation. Examples include anal manometry, which measures pressure within the anal canal during various maneuvers, and electromyography, which assesses the electrical activity of the sphincter muscles.
- Endoanal ultrasound: As mentioned earlier, EUS helps identify structural abnormalities in the anal sphincter complex.
The findings from these investigations are combined to determine the underlying cause of incontinence and plan appropriate management.
Q 14. How do you assess for constipation?
Assessing constipation involves understanding the patient’s bowel habits, identifying any potential causes, and utilizing appropriate diagnostic tools.
- History: We thoroughly explore bowel habits, including frequency, consistency of stools, straining efforts, and the use of laxatives. We also take a detailed medical history, including medications, dietary habits, and any relevant medical conditions.
- Physical examination: A digital rectal examination assesses stool consistency, presence of fecal impaction, and anal sphincter tone. An abdominal exam may identify abdominal masses or distension.
- Investigations: Based on the initial assessment, further investigations may be ordered. These could include colonoscopy (to visualize the colon and rule out structural causes) or other imaging tests (like abdominal X-rays) to identify obstructive causes.
- Anorectal physiology tests: In some cases, anal manometry can assess the efficacy of rectal evacuation. A defecography, a type of X-ray that shows how the rectum empties, might be utilized in cases of severe constipation.
The comprehensive evaluation allows us to differentiate between various types of constipation (e.g., slow transit, outlet obstruction) and tailor the treatment accordingly.
Q 15. How do you assess for anal fissure?
Assessing for anal fissures involves a careful history and physical examination. The patient will typically present with severe, sharp pain during defecation, often described as a tearing sensation. Bright red blood on the stool or toilet paper is also common.
The physical exam begins with a visual inspection. A fissure is usually seen as a longitudinal tear in the anal canal, often located posteriorly at the 6 o’clock position. A sentinel tag (a small skin tag at the anal margin) and/or a hypertrophied anal papilla (a swollen tissue near the fissure) may also be present. Digital rectal examination (DRE) is usually performed to assess the anal sphincter tone. While DRE is helpful to assess the sphincter, it’s important to do this gently to avoid causing further pain. In some cases, anoscopy (insertion of a short, rigid scope) may be needed for better visualization, especially if the fissure is not readily visible.
Example: A patient presents with sharp pain during bowel movements and bright red blood on the stool. Visual inspection reveals a small tear at the 6 o’clock position. This strongly suggests an anal fissure.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you assess for hemorrhoids?
Hemorrhoid assessment also begins with a thorough history focusing on symptoms like bleeding (bright red blood), pain, itching, and prolapse (bulging). Patients might describe a feeling of incomplete evacuation or a lump near the anus.
The physical exam involves careful inspection of the anal area. Internal hemorrhoids are located above the dentate line (the line separating the upper and lower parts of the anal canal) and are usually not visible unless prolapsed. External hemorrhoids are below the dentate line and can be seen as swollen, bluish masses. Digital rectal exam helps to palpate for internal hemorrhoids, particularly those that are not prolapsed. Anoscopy or proctoscopy (a more flexible scope) may be used for a more detailed examination of the anal canal and rectum.
Example: A patient complains of painless bright red blood with bowel movements and a feeling of fullness in the rectum. On examination, internal hemorrhoids are seen protruding from the anus.
Q 17. How do you assess for rectal prolapse?
Rectal prolapse is diagnosed through a combination of history and physical examination. Patients usually present with a feeling of a bulge or mass protruding from the anus, often accompanied by mucus discharge, bleeding, and straining during defecation. They may also report incomplete bowel evacuation and fecal incontinence.
The physical examination involves inspecting the anus with the patient straining or bearing down. The prolapse appears as a reddish, mucosal-lined mass protruding from the anus. The degree of prolapse (partial or complete) is noted. DRE is essential to assess the extent of rectal prolapse and the tone of the pelvic floor muscles. Additional imaging studies such as defecography (x-ray of the rectum during defecation) may be required to assess the severity and to guide treatment planning.
Example: A patient reports a feeling of something coming out of their rectum during bowel movements. On examination, a circumferential mass of rectal mucosa is visualized protruding from the anus during straining. This is indicative of rectal prolapse.
Q 18. What are the common causes of anorectal dysfunction?
Anorectal dysfunction encompasses a wide range of conditions with diverse causes. Common factors include:
- Constipation: Chronic constipation leads to straining during bowel movements, increasing pressure on the anorectal structures and contributing to hemorrhoids, fissures, and prolapse.
- Pelvic floor dysfunction: Weakness or incoordination of the pelvic floor muscles can cause fecal incontinence, rectal prolapse, and difficulty with defecation.
- Pregnancy and childbirth: The increased pressure on the pelvic floor during pregnancy and the trauma of childbirth can weaken pelvic floor muscles and contribute to anorectal dysfunction.
- Aging: Weakening of the pelvic floor muscles is a natural consequence of aging, increasing susceptibility to anorectal problems.
- Inflammatory bowel disease (IBD): Conditions like Crohn’s disease and ulcerative colitis can lead to inflammation and damage to the anal canal and rectum, causing fissures and other problems.
- Trauma: Anorectal trauma due to injury or surgery can also contribute to dysfunction.
- Neurological disorders: Certain neurological conditions affecting the nerves controlling bowel function can lead to incontinence and other anorectal problems.
Q 19. What are the treatment options for anorectal dysfunction?
Treatment options for anorectal dysfunction depend on the specific condition and its severity. Approaches include:
- Lifestyle modifications: Increasing fiber intake, drinking adequate fluids, and establishing regular bowel habits are crucial for managing constipation and preventing straining.
- Medical therapy: Medications such as stool softeners, laxatives, and topical creams might be prescribed to alleviate symptoms like pain and inflammation.
- Surgical interventions: Procedures like hemorrhoidectomy, fissurectomy, and rectal prolapse repair are considered for severe cases that haven’t responded to conservative treatment.
- Biofeedback therapy: Biofeedback helps patients learn to control their pelvic floor muscles, improving bowel function and reducing symptoms of incontinence and constipation.
Q 20. Describe the different types of biofeedback used in the treatment of anorectal dysfunction.
Biofeedback utilizes technology to provide patients with real-time feedback on their pelvic floor muscle activity. This allows them to learn how to contract and relax these muscles effectively. In anorectal dysfunction treatment, several types of biofeedback are employed:
- Surface electromyography (EMG) biofeedback: Sensors placed on the skin near the anus detect muscle activity, which is displayed visually or auditorily. This helps patients learn to strengthen and coordinate their pelvic floor muscles.
- Internal anal sphincter pressure biofeedback: A small catheter is inserted into the rectum to measure the pressure within the anal canal. This provides more precise feedback on anal sphincter function and helps patients learn to control anal sphincter pressure.
- Rectal balloon biofeedback: A small balloon is inserted into the rectum, and the patient learns to control their pelvic floor muscles to maintain a certain level of pressure within the balloon. This type of biofeedback is particularly useful for managing fecal incontinence.
Example: A patient with fecal incontinence undergoes surface EMG biofeedback, where sensors monitor their pelvic floor muscle contractions during simulated defecation. Visual feedback helps the patient learn to strengthen these muscles and improve sphincter control.
Q 21. Explain the role of diet in the management of anorectal dysfunction.
Diet plays a significant role in managing anorectal dysfunction, especially conditions related to constipation. A high-fiber diet is crucial for promoting regular bowel movements and preventing straining. Fiber adds bulk to the stool, making it easier to pass. Increasing fluid intake helps to soften the stool, further facilitating easy passage.
Foods to include: Fruits, vegetables, whole grains, legumes.
Foods to limit or avoid: Processed foods, red meat, dairy (if intolerance is present), foods low in fiber.
Example: A patient struggling with chronic constipation is advised to increase their intake of fruits and vegetables like apples, bananas, and broccoli, along with whole grains like oats and brown rice. Adequate fluid intake is also emphasized.
Q 22. What are the potential complications of anorectal surgery?
Anorectal surgery, while often highly effective, carries a range of potential complications. These can be broadly categorized into early and late complications. Early complications, occurring within the first few weeks post-surgery, might include wound infection, bleeding, hematoma formation (a collection of blood outside blood vessels), and pain. Late complications, developing weeks or months later, can be more varied and potentially more serious. These can include stricture formation (narrowing of the anal canal), fecal incontinence (inability to control bowel movements), fistula formation (an abnormal connection between the bowel and skin), and recurrent symptoms. The risk of these complications varies depending on the specific procedure performed, the patient’s overall health, and surgical technique. For example, a sphincteroplasty, aiming to repair a damaged anal sphincter, might lead to a higher risk of incontinence compared to a simpler procedure like hemorrhoid removal. Minimizing these risks involves meticulous surgical technique, appropriate patient selection, and careful post-operative management, including diligent wound care and pain control.
Q 23. How do you counsel patients on lifestyle modifications for anorectal dysfunction?
Counseling patients on lifestyle modifications for anorectal dysfunction is crucial for long-term success. This is a highly individualized process, tailored to the specific condition and the patient’s needs. For example, patients with constipation are advised to increase fiber intake through dietary changes, such as adding more fruits, vegetables, and whole grains. Adequate fluid intake is also emphasized to help soften stools and prevent straining. Regular exercise can also help stimulate bowel movements. For patients with fecal incontinence, we discuss strategies for bowel management, including regular toileting habits, pelvic floor muscle exercises (Kegel exercises), and potentially the use of absorbent products. Furthermore, we address dietary adjustments to manage stool consistency, and we may recommend biofeedback therapy, a technique to help patients regain voluntary control over their pelvic floor muscles. In all cases, open communication and patient education are paramount. We encourage patients to keep a bowel diary to track their symptoms and response to lifestyle changes, allowing for adjustments to the plan as needed. This collaborative approach empowers patients and improves the chances of successful management.
Q 24. How do you manage post-operative pain following anorectal surgery?
Post-operative pain management after anorectal surgery is critical for patient comfort and recovery. We employ a multimodal approach, combining different pain relief strategies. This usually starts with local anesthetic infiltration during surgery. Post-operatively, patients typically receive a combination of oral analgesics (pain relievers), such as acetaminophen or NSAIDs (nonsteroidal anti-inflammatory drugs), and potentially opioids for more severe pain, especially in the immediate post-operative period. We carefully monitor patients for pain levels and adjust medications accordingly. We also emphasize the use of warm sitz baths, which can soothe the affected area and reduce discomfort. We may also prescribe stool softeners to prevent straining during bowel movements, which can exacerbate pain. The goal is to achieve adequate pain control without significant side effects. Regular follow-up appointments allow us to assess the effectiveness of the pain management strategy and make necessary adjustments. In some cases, we may refer patients to pain specialists for more complex pain management needs.
Q 25. What are the long-term outcomes of treatment for anorectal dysfunction?
The long-term outcomes of treatment for anorectal dysfunction vary depending on the specific condition and the treatment approach. For example, surgery for hemorrhoids often provides long-lasting relief, although recurrence is possible. In cases of anal fissures, conservative management often resolves symptoms, but surgical intervention may be necessary for chronic cases. The success rates of sphincteroplasty for fecal incontinence are variable, with some patients experiencing significant improvement in continence while others see only modest benefits. Biofeedback therapy can be quite effective in improving bowel control in patients with fecal incontinence or other anorectal dysfunctions. Long-term follow-up is essential to monitor patients for recurrence of symptoms, the development of complications, and the overall success of treatment. Regular communication with the patient is key in ensuring that they are able to adapt lifestyle modifications and maintain long term improvement. This highlights the importance of a holistic approach to management, blending medical interventions with patient education and lifestyle changes.
Q 26. Describe your experience with different types of anal sphincteroplasty.
My experience encompasses various types of anal sphincteroplasty, each tailored to specific anatomical defects and patient needs. Overlapping Sphincteroplasty is a common technique used to repair damage to the internal anal sphincter. I’ve performed several of these procedures, achieving satisfactory results in the majority of cases. This often involves overlapping the damaged portions of the muscle to achieve better closure and continence. Posterior Sphincteroplasty focuses on the posterior aspect of the sphincter, which is frequently affected in conditions like obstetric anal sphincter injuries. I’ve found this to be effective in improving continence, but meticulous surgical technique is crucial to minimize complications such as incontinence. The choice of technique is highly individualized and depends on factors like the extent and location of the sphincter defect and the patient’s overall health. I always discuss the potential benefits and risks of each procedure with patients before making a decision.
Q 27. Describe the management of a patient presenting with severe anal fissure and severe pain.
Managing a patient presenting with a severe anal fissure and severe pain requires a multifaceted approach. Immediate pain relief is paramount. This often involves high-potency topical anesthetics, such as lidocaine, to numb the area and provide immediate comfort. We also prescribe stool softeners to prevent painful bowel movements. A warm sitz bath several times a day can also significantly reduce pain and inflammation. In many cases, these conservative measures, combined with high-fiber diet, are sufficient to heal the fissure. However, for chronic or severe cases that fail to respond to conservative treatment, surgical options such as lateral internal sphincterotomy (cutting a small portion of the internal anal sphincter) might be considered. This procedure aims to reduce muscle spasm and promote healing. Careful patient selection and post-operative management are crucial to minimize risks and maximize the chances of a successful outcome. Pain management is an ongoing part of the care, and we often re-evaluate the treatment plan and adjust pain medication as needed.
Q 28. Describe the differential diagnosis for a patient presenting with fecal incontinence.
Fecal incontinence can have a diverse range of underlying causes, necessitating a thorough differential diagnosis. It’s crucial to consider both anorectal and extra-anorectal factors. Anorectal causes include anal sphincter injuries (often from childbirth or trauma), internal or external anal sphincter disorders, rectal prolapse (protrusion of the rectum), and anismus (difficulty relaxing the anal sphincter). Extra-anorectal factors include neurological disorders such as stroke or multiple sclerosis affecting bowel control, inflammatory bowel disease (such as Crohn’s disease or ulcerative colitis) causing rectal inflammation, and certain medications that can have laxative effects. A comprehensive assessment includes a detailed history of bowel habits, a thorough physical examination, and often, specialized investigations such as anorectal manometry (measuring anal pressures) and defecography (imaging of bowel evacuation). This systematic approach ensures that we identify the root cause of fecal incontinence and can tailor the most effective management strategy for each individual patient. For example, a patient with anismus would benefit from biofeedback therapy, while a patient with a neurological disorder might require focused medication management and possibly supportive devices.
Key Topics to Learn for Assessment of Anorectal Dysfunction Interview
- Patient History & Examination: Thoroughly understanding how to obtain a comprehensive patient history, focusing on bowel habits, symptoms, and past medical history. Mastering the techniques of a thorough anorectal physical examination, including digital rectal examination and anoscopy.
- Physiological Testing: Gaining a solid grasp of the principles and interpretation of anorectal physiological tests, such as anorectal manometry, endoanal ultrasound, and defecography. Understand the indications, limitations, and clinical relevance of each test.
- Differential Diagnosis: Develop your ability to differentiate between various anorectal disorders, including functional disorders like fecal incontinence and constipation, and structural abnormalities like rectal prolapse and anal fissures. Practice formulating differential diagnoses based on clinical presentations.
- Treatment Strategies: Familiarize yourself with a range of conservative and surgical treatment options for common anorectal disorders. This includes understanding the rationale behind each treatment modality and its potential benefits and risks.
- Communication & Patient Care: Practice explaining complex medical information clearly and compassionately to patients. Develop your skills in counseling and managing patient expectations.
- Ethical Considerations: Understand the ethical implications involved in the assessment and treatment of anorectal dysfunction, including patient confidentiality and informed consent.
- Advanced Imaging Techniques: Explore your understanding of advanced imaging modalities like MRI and their role in the assessment of complex anorectal conditions.
Next Steps
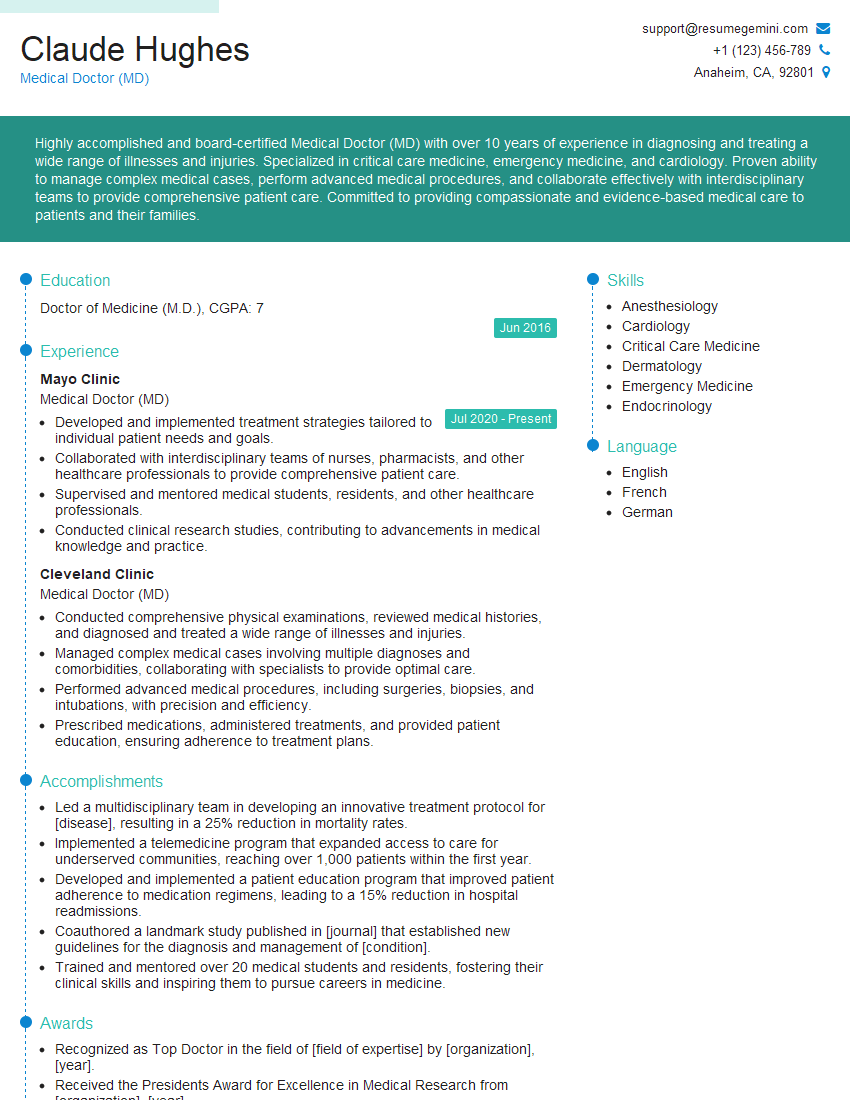
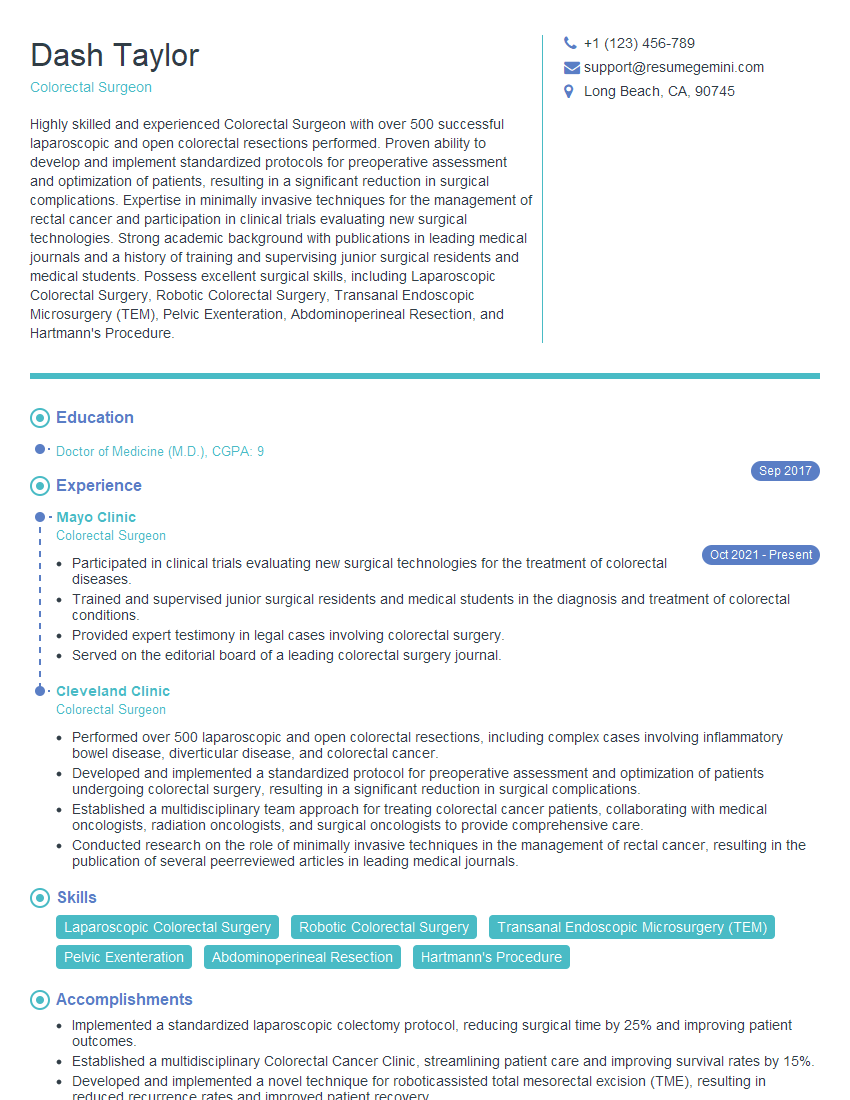
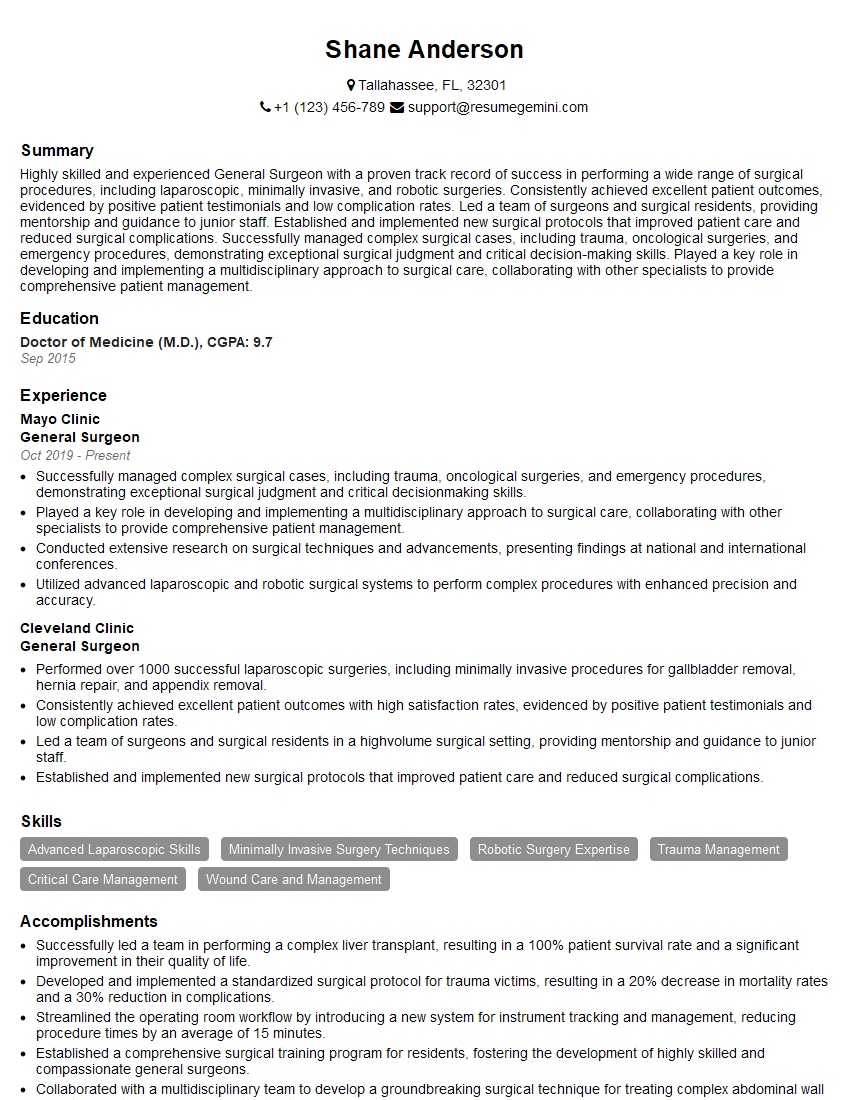
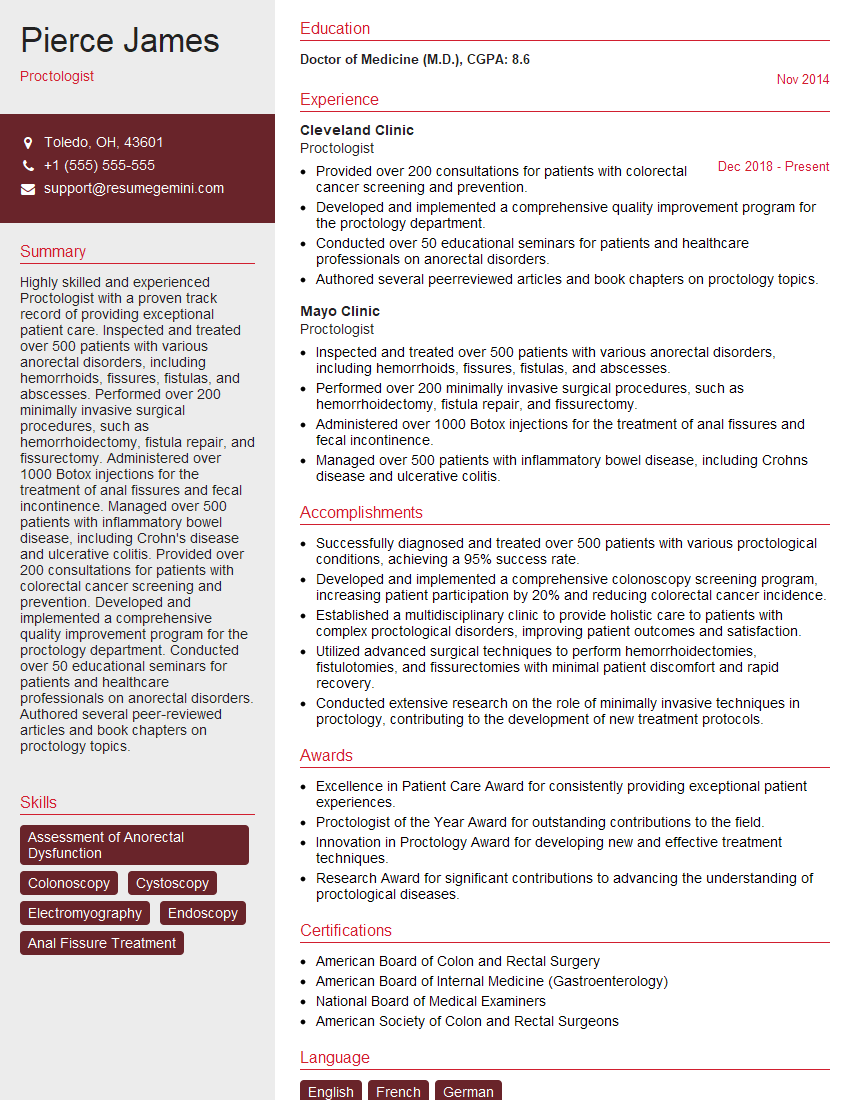
Mastering the assessment of anorectal dysfunction is crucial for career advancement in gastroenterology, colorectal surgery, and related fields. A strong understanding of these concepts demonstrates a high level of clinical competence and problem-solving skills, making you a highly desirable candidate. To enhance your job prospects, create an ATS-friendly resume that effectively highlights your skills and experience. ResumeGemini is a trusted resource to help you build a professional and impactful resume. They offer examples of resumes tailored to Assessment of Anorectal Dysfunction to help you get started.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.