Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Assist with Clinical Trials and Research interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Assist with Clinical Trials and Research Interview
Q 1. Explain the phases of a clinical trial and their objectives.
Clinical trials are conducted in phases, each with specific objectives. Think of it like building a house: you wouldn’t build the roof before the foundation.
- Phase 0: This is a very early phase, sometimes called exploratory investigational new drug (IND) studies. It involves a very small number of participants and focuses on understanding the drug’s pharmacokinetics (how the body processes the drug) and pharmacodynamics (how the drug affects the body) at very low doses. This phase helps researchers determine if the drug behaves as expected before larger-scale trials.
- Phase 1: This phase primarily focuses on safety. A small group of healthy volunteers receive the drug to assess its safety, tolerability, and to identify potential side effects. Dosage ranges are explored.
- Phase 2: Here, the drug is given to a larger group of patients who have the condition the drug is intended to treat. The main goal is to determine if the drug is effective and to further evaluate its safety. Researchers begin to assess efficacy and to refine dosages.
- Phase 3: This is a large-scale trial involving hundreds or thousands of patients. The primary goal is to confirm the drug’s effectiveness, compare it to existing treatments, and monitor side effects. Data from Phase 3 is often used to support regulatory approval.
- Phase 4: This post-market surveillance phase occurs after the drug has been approved. It continues to monitor the drug’s long-term safety and effectiveness in a larger population. Researchers may explore additional uses for the drug.
For example, in a clinical trial for a new cancer drug, Phase 1 might involve 20 healthy volunteers to assess safety, Phase 2 might involve 100 cancer patients to assess efficacy, and Phase 3 might involve 1000 cancer patients to confirm the findings and compare it to a standard chemotherapy regimen.
Q 2. Describe your experience with Good Clinical Practice (GCP) guidelines.
Good Clinical Practice (GCP) guidelines are internationally recognized standards for designing, conducting, recording, and reporting clinical trials. They ensure the rights, safety, and well-being of trial participants are protected and that the data generated is credible and reliable. My experience with GCP encompasses all aspects, from protocol development and informed consent procedures to data management and safety reporting. I’ve been involved in audits and have consistently demonstrated adherence to GCP principles in all my projects. For instance, in a recent study, I ensured meticulous documentation of all procedures, which included documenting every deviation and ensuring appropriate regulatory reporting. My experience also extends to training research staff on GCP principles and implementing quality control measures throughout the study lifecycle to maintain GCP compliance. This includes conducting regular training sessions for staff members on the most recent GCP updates and protocols.
Q 3. How do you ensure data integrity in a clinical trial?
Data integrity is paramount in clinical trials. Compromised data can lead to inaccurate results, misleading conclusions, and even jeopardize patient safety. I ensure data integrity through a multi-faceted approach:
- Data Validation: Implementing robust data validation checks at every stage—from data entry to analysis—to identify and correct errors.
- Audit Trails: Utilizing electronic data capture (EDC) systems with comprehensive audit trails to track all data modifications and identify any unauthorized changes. For example, the system should track who made a change, when it was made, and what the change was.
- Source Data Verification: Comparing data entered into the EDC system against the original source documents (e.g., case report forms, lab reports) to ensure accuracy.
- Data Monitoring: Regularly monitoring data for inconsistencies, outliers, and other anomalies that could indicate data integrity issues. This includes using statistical methods to detect patterns that might suggest errors.
- Standard Operating Procedures (SOPs): Implementing and adhering to strict SOPs for data handling, storage, and archiving.
For example, if a data entry error is found, I ensure it’s documented, corrected, and justified with appropriate approvals. The original incorrect entry is not erased but retained within the audit trail.
Q 4. What are the key differences between a blinded and unblinded study?
The key difference between blinded and unblinded studies lies in who knows the treatment assignment of participants. Imagine a taste test: in a blinded study, you don’t know which sample is which until after you’ve tasted both; in an unblinded study, you know immediately which sample is which.
- Blinded (Masked) Study: The treatment assignment (e.g., placebo or drug) is concealed from participants, investigators, or both. This helps to minimize bias and improve the objectivity of the results. There are different levels of blinding: single-blind (participants are unaware), double-blind (both participants and investigators are unaware), and triple-blind (participants, investigators, and data analysts are unaware).
- Unblinded Study: Everyone knows which treatment each participant receives. These are often used in situations where blinding is impractical, such as surgical procedures.
In a blinded study of a new blood pressure medication, neither the participants nor the doctors would know who received the drug versus a placebo. This helps to prevent bias in assessing the treatment’s effectiveness. Unblinded studies are often used when testing the effectiveness of a surgical procedure where blinding is not feasible.
Q 5. Explain the process of informed consent in clinical trials.
Informed consent is a cornerstone of ethical clinical research. It ensures that participants voluntarily agree to participate in a trial after being fully informed of its purpose, procedures, risks, and benefits. The process involves several steps:
- Information Provision: Providing potential participants with a clear and concise explanation of the study, including its objectives, procedures, potential risks and benefits, alternative treatments, and their rights as participants. The information is presented in a language they understand.
- Understanding and Comprehension: Assessing the participant’s understanding of the information provided, answering any questions they have, and ensuring they comprehend the implications of participation.
- Voluntary Participation: Emphasizing that participation is entirely voluntary and that they are free to withdraw at any time without penalty.
- Documentation: Obtaining written consent from the participant, which is carefully documented and signed by both the participant and the investigator.
For example, before enrolling someone in a clinical trial testing a new pain medication, I would ensure they understand the potential side effects (e.g., nausea, drowsiness), the study’s procedures (e.g., blood draws, questionnaires), and their right to withdraw from the trial at any point without consequence. Their consent form would be reviewed with them carefully, ensuring they understand everything before signing.
Q 6. How do you handle protocol deviations in a clinical trial?
Protocol deviations are instances where procedures or activities differ from the approved clinical trial protocol. Handling them appropriately is crucial for maintaining data integrity and ensuring the safety of participants. My approach involves:
- Immediate Reporting: Any deviation is immediately reported to the appropriate personnel (e.g., study monitor, principal investigator).
- Documentation: Meticulous documentation of the deviation, including the reason for the deviation, the actions taken, and the impact on the study results.
- Investigation: Investigating the deviation to determine its cause and whether it necessitates corrective actions or modifications to the protocol.
- Risk Assessment: Assessing the potential impact of the deviation on the safety of participants and the validity of the study data.
- Corrective Actions: Implementing corrective actions to prevent similar deviations from occurring in the future. This might involve revising the protocol, retraining staff, or implementing improved quality control measures.
For instance, if a participant misses a scheduled visit, I would document this deviation, investigate the reason for the missed visit, and determine if it impacts the validity of their data. This information would be reported to the study monitor and necessary actions taken. I might implement a reminder system to reduce missed visits in the future.
Q 7. Describe your experience with electronic data capture (EDC) systems.
Electronic Data Capture (EDC) systems are software applications used to collect, manage, and analyze clinical trial data electronically. My experience with EDC systems includes:
- System Selection and Implementation: Participating in the selection and implementation of appropriate EDC systems based on the study requirements and budget.
- Data Entry and Management: Training study staff on the use of EDC systems and ensuring accurate and timely data entry.
- Data Validation and Cleaning: Utilizing EDC system features for data validation and cleaning to identify and correct errors.
- Query Resolution: Managing and resolving data queries, ensuring the consistency and accuracy of the data.
- Reporting and Analysis: Using EDC system reports for monitoring trial progress and generating clinical study reports.
I have extensive experience with several EDC systems like REDCap, Oracle Clinical, and Veeva Vault. For example, in a recent trial, I used REDCap to efficiently manage data from multiple sites, reducing errors and enhancing data quality. The built-in validation rules within the system helped prevent entry of invalid data, ensuring data integrity.
Q 8. What are your skills in data cleaning and validation?
Data cleaning and validation are crucial for the reliability and integrity of clinical trial data. My approach involves a multi-step process ensuring accuracy and consistency. This begins with identifying and correcting inconsistencies, such as missing values, outliers, and typographical errors. I use a combination of automated tools and manual review to detect these issues. For example, I might use R or Python with packages like dplyr and tidyr for automated cleaning, then visually inspect data using tools like Tableau or spreadsheets to identify any patterns that might signal errors missed by automated tools.
Validation involves verifying the data’s accuracy against predefined rules and standards. This often includes range checks (ensuring values fall within acceptable limits), consistency checks (comparing values across different fields), and plausibility checks (assessing whether the data makes logical sense). For example, if a patient’s age is recorded as 150, a plausibility check would immediately flag this as an error. Documentation is paramount throughout the process, ensuring complete traceability of all cleaning and validation steps, which is especially important for audit trails.
Q 9. How familiar are you with different types of clinical trial designs (e.g., randomized controlled trials, observational studies)?
I’m very familiar with various clinical trial designs. Randomized controlled trials (RCTs) are the gold standard, involving the random assignment of participants to different treatment groups (e.g., treatment vs. placebo) to compare their effectiveness. Observational studies, conversely, do not involve intervention or randomization. Instead, they observe the effect of a treatment or exposure in a real-world setting. These can be cohort studies (following a group over time), case-control studies (comparing individuals with and without a condition), or cross-sectional studies (observing at a single point in time).
My experience also includes understanding and applying other designs like parallel group designs, crossover designs (where each participant receives all treatments), factorial designs (investigating multiple treatments simultaneously), and adaptive designs (allowing for modifications during the trial based on accumulating data). Understanding the strengths and weaknesses of each design is vital for choosing the most appropriate approach given the research question and resource constraints.
Q 10. Explain your experience with case report form (CRF) completion and review.
Case Report Forms (CRFs) are the backbone of data collection in clinical trials. My experience encompasses the entire lifecycle of CRF management, from initial design and development to completion and review. I have hands-on experience with electronic data capture (EDC) systems, which significantly streamline the process. In my previous role, I helped design CRFs ensuring they were user-friendly and captured all necessary data elements for regulatory compliance.
During the completion phase, I’ve worked with investigators and research staff to ensure accurate and complete data entry. This includes providing training, addressing queries, and monitoring data quality. The review process involves meticulously examining the completed CRFs for completeness, consistency, and accuracy. This might involve identifying missing data, inconsistencies across data points, and outliers that require further investigation or clarification from the investigator. Data discrepancies often require careful follow-up to clarify the reported information and ultimately maintain high data quality.
Q 11. How do you manage adverse events (AEs) reported during a clinical trial?
Managing adverse events (AEs) is a critical aspect of clinical trial safety. My experience involves implementing a robust AE reporting and management system. This begins with timely identification of any unexpected or serious events reported by participants, investigators, or other study personnel. Once an AE is reported, it undergoes a thorough evaluation to determine its severity, causality (relationship to the study intervention), and expectedness (whether it’s a known side effect).
This often involves careful review of medical records, and communication with investigators to obtain more information when needed. Serious adverse events (SAEs) require immediate reporting to regulatory authorities and the study sponsor, adhering to strict timelines and reporting standards. Throughout this process, accurate documentation and careful tracking of AE details are essential for regulatory compliance and maintaining the safety of trial participants. Using a standardized system like MedDRA (Medical Dictionary for Regulatory Activities) for coding adverse events ensures consistency and facilitates data analysis.
Q 12. Describe your experience with regulatory submissions (e.g., IND, NDA).
I have significant experience supporting regulatory submissions, including Investigational New Drug (IND) applications and New Drug Applications (NDAs). This involves preparing and compiling the necessary documentation, ensuring it meets all regulatory requirements. For INDs, this includes preclinical data, manufacturing information, and the proposed clinical trial protocol. For NDAs, the submission is substantially larger and encompasses all the data generated from clinical trials, demonstrating the drug’s safety and efficacy.
My experience includes working closely with regulatory agencies like the FDA (in the US) or EMA (in Europe) to respond to queries, address concerns, and ensure a smooth submission process. This often involves navigating complex regulations, ensuring compliance with Good Clinical Practice (GCP) guidelines, and maintaining meticulous documentation throughout the entire submission process. Understanding the specific requirements for each agency and tailoring the submission accordingly is critical for success.
Q 13. What is your experience with statistical analysis in clinical trials?
Statistical analysis is fundamental to interpreting clinical trial results. I’m proficient in using statistical software like SAS and R to perform various analyses, including descriptive statistics, hypothesis testing, and survival analysis. My experience covers a broad range of statistical methods, from t-tests and ANOVA to regression analysis and more complex models.
I understand the importance of appropriate statistical methodologies depending on the study design and research question. For instance, I know when to use a paired t-test compared to an independent samples t-test. Furthermore, I am capable of interpreting the results, drawing meaningful conclusions, and presenting findings in a clear and concise manner. This also includes developing statistical analysis plans (SAPs) before the start of a trial, clearly outlining the intended statistical methods. A well-defined SAP ensures that the analysis is rigorous, transparent, and aligns with the study objectives.
Q 14. How do you handle queries from investigators or sponsors during a clinical trial?
Handling queries from investigators and sponsors is a vital part of trial management. I approach this with a proactive and solution-oriented mindset. Effective communication is key; responding promptly and thoroughly is crucial for maintaining positive relationships and ensuring data integrity.
Queries often relate to protocol clarifications, data entry issues, AE reporting, or regulatory requirements. My approach involves carefully reviewing the query, gathering relevant information, and providing a clear, concise, and well-documented response. When needed, I consult with other members of the study team to ensure the response is accurate and comprehensive. This includes maintaining a clear audit trail of all queries and responses to ensure transparency and accountability throughout the trial. In some cases, queries might highlight issues requiring protocol amendments or other actions to maintain the trial’s integrity.
Q 15. Describe your experience with site selection and initiation.
Site selection and initiation are critical first steps in a clinical trial, determining its success. It involves identifying suitable research sites (hospitals, clinics) that meet specific criteria, such as having the right patient population, experienced investigators, and necessary infrastructure. This process begins with a thorough assessment of potential sites based on factors like geographic location, access to target patients, the site’s track record, and its capacity to handle the trial’s logistical demands.
For instance, a trial investigating a rare disease would necessitate sites with specialized expertise and access to a patient registry. My experience includes developing and managing detailed site selection criteria, negotiating site contracts, and overseeing the initiation visit to each selected site. This visit ensures all necessary regulatory documents are in place, staff are adequately trained, and systems are ready to enroll patients.
- Criteria Development: I’ve worked on developing detailed questionnaires to screen potential sites, considering factors beyond simple patient numbers, encompassing ethical review board (IRB) experience, data management capabilities and adherence to Good Clinical Practice (GCP) guidelines.
- Contract Negotiation: I’ve negotiated contracts with various sites, ensuring compliance with regulations and protecting the trial’s interests.
- Site Initiation Visit (SIV): I’ve led and participated in numerous SIVs, providing training, resolving issues, and ensuring a smooth transition to patient enrollment.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you ensure patient safety in a clinical trial?
Patient safety is paramount in clinical trials. It’s an ongoing process, not a one-time event. We implement comprehensive safety monitoring strategies starting from the design phase of the protocol. This includes rigorous informed consent processes, where potential participants understand the risks and benefits thoroughly. Data safety monitoring boards (DSMBs) are frequently utilized to independently review accumulating safety data and recommend actions to protect participants.
Throughout the trial, we actively monitor adverse events (AEs), serious adverse events (SAEs), and other safety signals. Any safety concerns are reported promptly to the appropriate regulatory authorities and the study sponsor. We also use safety databases and systems to track, analyze, and report these events efficiently. For example, if an unexpected serious adverse event emerges, we’d immediately halt enrollment, investigate the cause, and revise the study protocol if necessary – all in line with strict GCP guidelines. We follow procedures to report to the IRB and relevant regulatory authorities. This proactive approach ensures that the trial stops if a treatment is deemed unsafe.
Q 17. What is your experience with monitoring clinical trial sites?
My experience in monitoring clinical trial sites encompasses both remote and on-site monitoring activities. Remote monitoring involves reviewing data regularly, using electronic data capture (EDC) systems to identify potential discrepancies or trends that may signal problems at the site. On-site monitoring includes conducting site visits to observe study procedures, review source documents, verify data accuracy, and assess the overall conduct of the trial at each site.
For example, I’ve used EDC systems to track key data points like enrollment rates, adverse event reporting, and protocol deviations. Discrepancies are investigated promptly, and corrective actions are implemented. During on-site visits, I’ve observed researchers conducting examinations, reviewed patient medical records, and ensured adherence to standard operating procedures (SOPs). I’ve also provided on-site training and support to site staff, addressing concerns and maintaining a positive working relationship.
Q 18. How do you manage timelines and budgets in a clinical trial?
Managing timelines and budgets effectively in clinical trials is crucial for success. It necessitates meticulous planning, resource allocation, and ongoing monitoring. We create detailed project plans with clear milestones, timelines, and responsibilities. These plans typically use Gantt charts or other project management tools to visualize progress and identify potential delays. Regular progress meetings are essential to track budget spending, address roadblocks, and adjust the plan as needed.
For instance, if a delay is identified in the enrollment process, we would analyze the cause (e.g., recruitment challenges, administrative bottlenecks), propose solutions (e.g., increased marketing efforts, streamlined procedures), and update the project timeline and budget accordingly. This requires proactive risk management and clear communication with stakeholders, including the sponsor, investigators, and regulatory bodies.
Q 19. What is your experience with pharmacovigilance activities?
Pharmacovigilance (PV) is the science and activities relating to the detection, assessment, understanding and prevention of adverse effects or any other drug-related problem. My experience includes participating in the development and implementation of PV plans, reviewing individual case safety reports (ICSRs), and contributing to periodic safety updates for regulatory submissions. This involves close collaboration with medical monitors, data managers, and regulatory affairs teams.
For example, I’ve helped develop and maintain signal detection systems to proactively identify potential safety issues. I’ve also prepared and reviewed safety reports for regulatory agencies such as the FDA, utilizing MedDRA (Medical Dictionary for Regulatory Activities) for standardized coding of adverse events. This ensures that adverse events are reported accurately and consistently, facilitating prompt detection of safety signals and risk mitigation.
Q 20. Describe your experience with the development of clinical study protocols.
Developing clinical study protocols is a multifaceted process requiring a deep understanding of clinical research methodologies, regulatory guidelines, and therapeutic areas. It starts with defining the research question, selecting the appropriate study design, and establishing clear inclusion/exclusion criteria. A detailed description of the study’s methodology, including endpoints, assessments, and statistical analysis plan, is critical. The process often involves collaboration with statisticians, medical writers, and other experts to ensure the protocol is scientifically sound, ethically acceptable, and feasible.
For example, I’ve been involved in developing protocols for randomized controlled trials (RCTs), observational studies, and phase I-IV clinical trials, creating the framework for each study’s execution and ensuring the protocol aligns with GCP and regulatory requirements. A clear protocol minimizes ambiguity and ensures consistency in the conduct of the study across different sites.
Q 21. How proficient are you with relevant software (e.g., SAS, R, MedDRA)?
I’m proficient in several software applications commonly used in clinical research. My skills encompass using SAS for statistical analysis, including data cleaning, manipulation, and generation of tables, listings, and figures for regulatory submissions. I’m also experienced in using R for advanced statistical modelling and data visualization. Further, I have extensive experience with MedDRA, utilizing its standardized terminology for coding and reporting of adverse events, which is crucial for pharmacovigilance activities.
For example, I’ve used SAS to analyze data from large clinical trials, generating summary statistics, conducting hypothesis testing, and creating reports for regulatory filings. My proficiency in R enables me to perform more complex statistical analyses and data visualization. My proficiency with MedDRA allows for accurate and consistent coding of adverse events across studies, streamlining the process of safety reporting.
Q 22. Explain your understanding of ICH-GCP guidelines.
ICH-GCP (International Council for Harmonisation – Good Clinical Practice) guidelines are a set of ethical and scientific quality requirements for designing, conducting, recording, and reporting clinical trials that involve the participation of human subjects. They ensure the rights, safety, and well-being of trial participants are protected, and that the data generated are credible and reliable.
These guidelines cover a broad range of topics including:
- Ethical considerations: Informed consent, privacy, confidentiality.
- Study design and conduct: Protocol development, investigator selection, site monitoring.
- Data management: Case report form (CRF) design, data entry, data validation.
- Quality assurance and quality control: Auditing, inspection readiness.
- Reporting: Adverse event reporting, regulatory reporting.
In essence, ICH-GCP provides a framework for conducting high-quality clinical research that is ethically sound and scientifically rigorous. For example, strict adherence to GCP ensures that the results of a clinical trial can be trusted and used to inform clinical practice and regulatory decisions. Failure to follow GCP can lead to trial failure, regulatory action, and damage to the reputation of all involved.
Q 23. How do you prioritize tasks in a fast-paced clinical trial environment?
Prioritizing tasks in a fast-paced clinical trial environment requires a structured approach. I typically use a combination of techniques:
- Urgency and Importance Matrix (Eisenhower Matrix): This helps categorize tasks based on urgency and importance, allowing me to focus on high-impact, time-sensitive activities first. For instance, resolving a critical safety issue takes precedence over drafting a routine report.
- Project Management Software: Tools like Asana or Jira provide a visual representation of tasks, deadlines, and dependencies, allowing for efficient task allocation and tracking. This provides a clear overview of progress and facilitates proactive issue identification.
- Regular Team Meetings: Frequent communication and coordination with the team ensure everyone is aligned and potential roadblocks are identified early. This allows for proactive adjustments to the workflow, enabling us to stay on track.
- Risk Assessment: Identifying potential risks and challenges early helps in proactively implementing mitigation strategies. This helps ensure timely completion even in the presence of unexpected events.
For example, during a pivotal study with an impending deadline, I would prioritize tasks like data cleaning and safety reporting before less urgent tasks such as preparing presentations.
Q 24. What is your experience with subject recruitment and retention?
Subject recruitment and retention are critical to the success of any clinical trial. My experience involves developing and implementing comprehensive strategies to achieve these goals:
- Targeted Recruitment: Identifying and engaging with the appropriate patient population through various channels, such as collaborations with healthcare providers, online advertising, and community outreach programs. For example, for a trial focused on a rare disease, partnering with specialized clinics would be crucial.
- Effective Communication: Establishing clear and consistent communication with potential and enrolled participants, addressing their questions and concerns promptly and professionally. This could involve providing regular updates, easily accessible materials, and responsive customer service.
- Incentivize Participation: Offering reasonable compensation and providing participants with resources and support to encourage their continued involvement. This could include travel stipends, gift cards, or access to support services.
- Retention Strategies: Proactive monitoring and personalized engagement strategies to identify and address potential participant concerns, barriers, or adverse events that may lead to dropout. This might involve regular check-in calls, reminders for appointments, and prompt responses to queries.
In a recent trial, we experienced a high retention rate by implementing personalized communication strategies and a robust support system for participants. This involved regular phone calls and addressing any questions and concerns promptly.
Q 25. Describe your experience with quality control procedures in clinical trials.
Quality control (QC) is paramount in clinical trials to ensure data integrity and reliability. My experience involves implementing and overseeing various QC procedures throughout the trial lifecycle:
- Data Validation: Employing various techniques to identify and correct inconsistencies or errors in the data collected. This includes range checks, consistency checks, and plausibility checks.
- Source Data Verification (SDV): Comparing the data entered in the case report forms (CRFs) with the original source documents to confirm accuracy and completeness.
- Audits and Inspections: Participating in internal and external audits and inspections to ensure compliance with GCP guidelines and regulatory requirements. This involves thorough review of documents, processes and adherence to the protocol.
- SOP Development and Maintenance: Contributing to the development and ongoing maintenance of standard operating procedures (SOPs) that govern various aspects of the trial’s conduct and data management. This helps to maintain consistency across processes and operations.
For example, during a recent study, we implemented a double data entry system to minimize transcription errors and established a robust SDV process to ensure data accuracy. These measures ultimately led to high-quality data and a successful trial.
Q 26. How do you handle conflicts between investigators and sponsors?
Conflicts between investigators and sponsors can arise due to various reasons such as differing interpretations of the protocol, disagreements on data interpretation, or concerns about study conduct. My approach to resolving such conflicts involves:
- Open Communication: Facilitating open and transparent communication between all parties involved. Creating a safe environment for discussing concerns without fear of reprisal.
- Mediation and Facilitation: Acting as a neutral mediator to facilitate a constructive dialogue between the investigator and sponsor, helping them to understand each other’s perspectives and find common ground. This often involves active listening and identifying mutual objectives.
- Escalation Procedures: Having a clear escalation process defined in advance to address unresolved conflicts. This ensures a structured and timely approach to handling disagreements and involving appropriate stakeholders when necessary.
- Documentation: Maintaining a detailed record of all communications, decisions, and actions taken to ensure transparency and accountability.
In one instance, a conflict arose regarding the interpretation of a specific endpoint in a clinical trial. By facilitating discussions and clarifying the protocol definitions, we were able to reach a mutual understanding and avoid a significant delay in the trial timeline.
Q 27. Explain your understanding of blinding and unblinding procedures.
Blinding, also known as masking, is a technique used in clinical trials to prevent bias in the assessment of treatment effects. It involves concealing the treatment assignment (e.g., placebo or active treatment) from participants, investigators, or both. Unblinding is the process of revealing the treatment assignment after the completion of the trial or in certain predefined circumstances.
Types of Blinding:
- Single-blind: Only the participant is unaware of the treatment assignment.
- Double-blind: Both the participant and the investigator are unaware of the treatment assignment.
- Triple-blind: The participant, investigator, and data analyst are unaware of the treatment assignment.
Unblinding Procedures: Typically involve a secure process managed by a designated individual or committee to prevent bias. It often involves a code-breaking system, where the treatment assignments are revealed only after the completion of the study or in exceptional circumstances, such as for serious adverse events.
The purpose of blinding is to minimize bias in assessing treatment effects. For instance, in a double-blind trial, neither the participant nor the investigator’s knowledge of the treatment assignment can influence their observations or assessments. Unblinding is crucial for analyzing the results, but it is typically delayed until the study is completed to maintain the integrity of the trial.
Key Topics to Learn for Assisting with Clinical Trials and Research Interviews
- Good Clinical Practice (GCP): Understand the fundamental principles and guidelines governing clinical trials, ensuring ethical conduct and data integrity. Consider practical applications like recognizing deviations from GCP and their implications.
- Regulatory Landscape: Familiarize yourself with relevant regulations (e.g., FDA, EMA) and their impact on trial design, conduct, and reporting. Think about how these regulations influence your daily tasks and decision-making.
- Clinical Trial Design and Methodology: Grasp the different phases of clinical trials, study designs (randomized controlled trials, observational studies), and statistical methods used in data analysis. Be prepared to discuss the strengths and weaknesses of various approaches.
- Data Management and Analysis: Learn about data collection methods, database management systems, and basic statistical concepts relevant to clinical trial data. Prepare examples demonstrating your proficiency in handling and interpreting clinical data.
- Research Ethics and Patient Safety: Understand the ethical considerations involved in research, including informed consent, data privacy, and risk management. Discuss situations requiring ethical decision-making and problem-solving.
- Project Management Skills: Highlight your ability to manage tasks, timelines, and resources effectively within a clinical research setting. This includes organization, communication, and collaboration skills.
- Specific Therapeutic Areas (if applicable): If you have experience in a specific area (e.g., oncology, cardiology), be ready to discuss your expertise and related research methodologies.
Next Steps
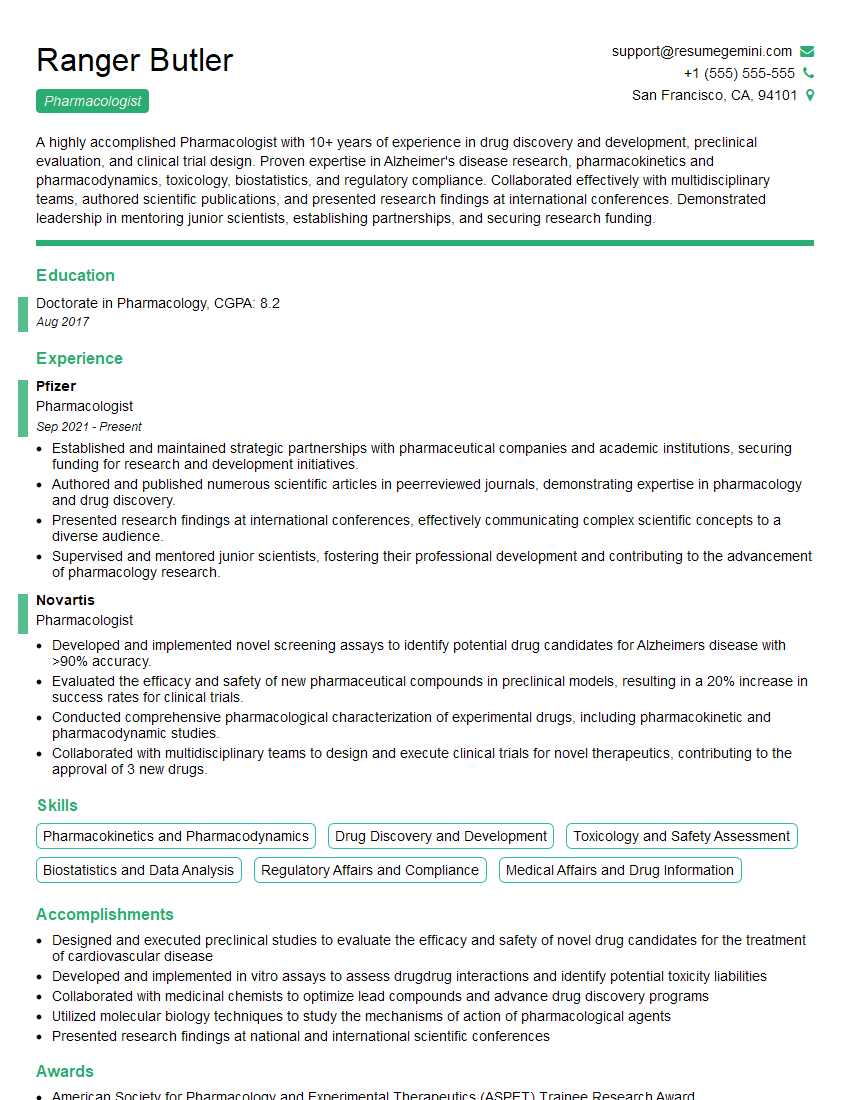
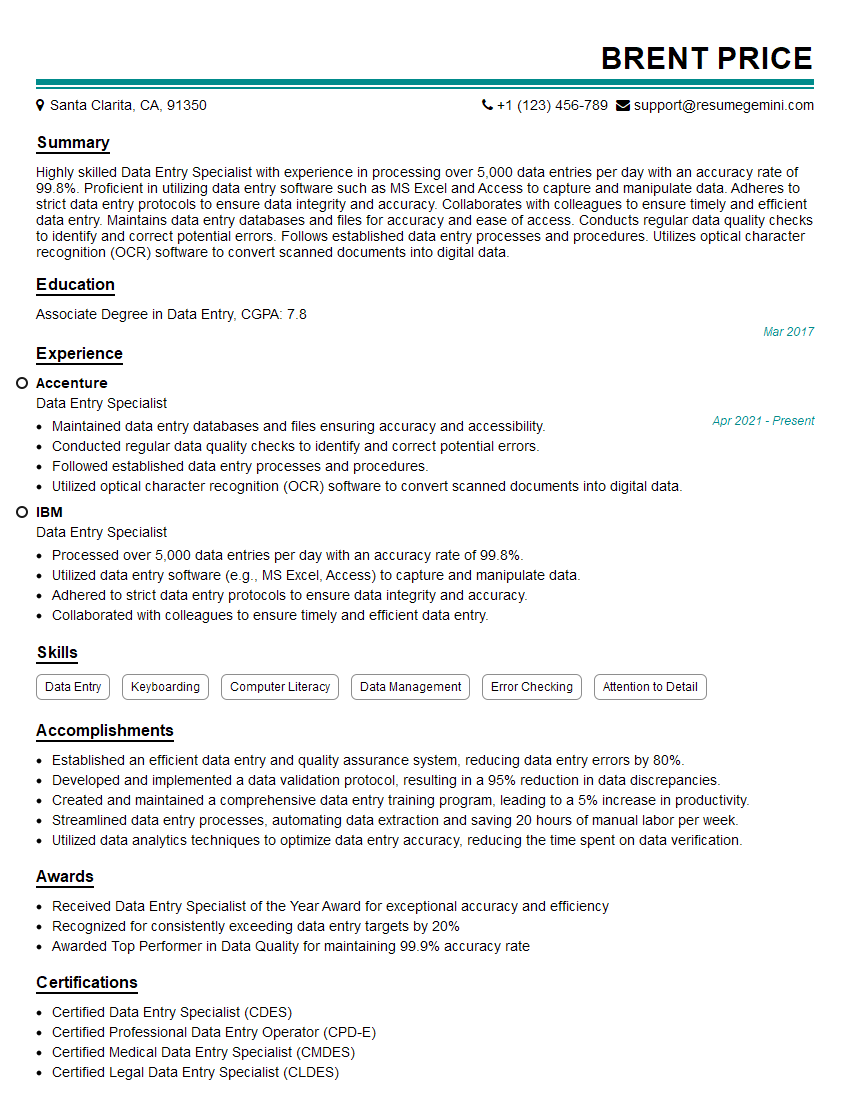
Mastering the intricacies of assisting with clinical trials and research significantly enhances your career prospects within the pharmaceutical and biotechnology industries. It opens doors to diverse roles and opportunities for professional growth and development. To maximize your job search success, create a compelling and ATS-friendly resume that highlights your skills and experience effectively. We strongly recommend using ResumeGemini, a trusted resource, to build a professional resume that stands out. ResumeGemini provides examples of resumes tailored to assisting with clinical trials and research, helping you craft a document that showcases your qualifications effectively.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.