The right preparation can turn an interview into an opportunity to showcase your expertise. This guide to Bipolar Disorder Treatment interview questions is your ultimate resource, providing key insights and tips to help you ace your responses and stand out as a top candidate.
Questions Asked in Bipolar Disorder Treatment Interview
Q 1. Describe the different types of bipolar disorder and their key diagnostic criteria.
Bipolar disorder is a serious mental illness characterized by extreme shifts in mood, energy, and activity levels. These shifts are far more intense and prolonged than those experienced in everyday life. The DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, 5th Edition) recognizes several types:
- Bipolar I Disorder: This involves at least one manic episode, which is a period of abnormally elevated, expansive, or irritable mood, lasting at least one week (or any duration if hospitalization is required). A major depressive episode is often, but not always, present.
- Bipolar II Disorder: This includes at least one major depressive episode and at least one hypomanic episode. Hypomania is a less severe form of mania, with elevated mood but not to the level that causes significant impairment or requires hospitalization.
- Cyclothymic Disorder: This involves numerous periods of hypomanic symptoms and periods of depressive symptoms that don’t meet the criteria for a major depressive episode. These symptoms persist for at least two years (one year in children and adolescents) and are not symptom-free for more than two months at a time.
Key Diagnostic Criteria generally involve assessing the presence and duration of manic or hypomanic episodes, along with the presence of depressive episodes and the exclusion of other potential causes. A comprehensive clinical interview and sometimes further diagnostic testing are crucial for accurate diagnosis.
Q 2. Explain the role of mood stabilizers in treating bipolar disorder.
Mood stabilizers are cornerstone medications in bipolar disorder treatment. Their primary role is to prevent extreme mood swings between mania and depression. They don’t just treat acute episodes; they aim to maintain mood stability over the long term, preventing relapses and improving the overall quality of life. This preventative effect is crucial in reducing the severity and frequency of episodes, which can greatly reduce the impact of the illness on a person’s life.
Q 3. Discuss the efficacy and side effects of commonly prescribed mood stabilizers (e.g., lithium, valproate, lamotrigine).
Several mood stabilizers have proven efficacy, but it’s crucial to remember that individual responses vary significantly. Let’s examine some common ones:
- Lithium: A highly effective mood stabilizer for both manic and depressive episodes, lithium works by influencing several neurotransmitter systems in the brain. Side effects can include weight gain, tremor, kidney problems, and thyroid issues. Regular blood tests are necessary to monitor lithium levels and prevent toxicity.
- Valproate (Depakote): Effective in treating manic episodes and preventing relapse, valproate also affects neurotransmitter systems. Side effects can include weight gain, hair loss, liver problems, and pancreatitis (though rare). Liver function tests are regularly monitored.
- Lamotrigine (Lamictal): Primarily used to prevent depressive episodes in bipolar disorder, lamotrigine works differently than lithium and valproate. Side effects are generally milder, with common ones including headache, rash (a rare but serious Stevens-Johnson syndrome can occur), and nausea. Careful titration (gradual dose increase) is essential to minimize the risk of rash.
The choice of mood stabilizer and dosage is personalized based on the individual’s specific symptoms, medical history, and response to treatment. Close monitoring by a psychiatrist is essential for managing both efficacy and potential side effects.
Q 4. What are the common comorbid conditions associated with bipolar disorder?
Bipolar disorder frequently co-occurs (comorbidity) with other mental health and physical health conditions. Common comorbid conditions include:
- Anxiety disorders: Generalized anxiety disorder, panic disorder, and social anxiety disorder are very common.
- Substance use disorders: Individuals with bipolar disorder may misuse alcohol or drugs to self-medicate their symptoms or cope with mood swings.
- Attention-deficit/hyperactivity disorder (ADHD): Overlapping symptoms of impulsivity and distractibility can make diagnosis challenging.
- Eating disorders: Changes in appetite and weight are frequent during mood episodes.
- Sleep disorders: Insomnia and other sleep disturbances are highly prevalent.
- Personality disorders: Especially borderline personality disorder.
Addressing these comorbid conditions is crucial for comprehensive treatment, as they can significantly impact the overall course of bipolar disorder and treatment outcomes.
Q 5. How do you differentiate bipolar disorder from other mood disorders (e.g., major depressive disorder, cyclothymia)?
Differentiating bipolar disorder from other mood disorders requires careful clinical evaluation. Key distinctions include:
- Bipolar disorder vs. Major Depressive Disorder (MDD): MDD involves persistent low mood, but lacks the periods of elevated mood characteristic of bipolar disorder. While someone with bipolar disorder can experience lengthy depressive episodes, the presence of a manic or hypomanic episode is the key differentiator.
- Bipolar disorder vs. Cyclothymic Disorder: Both involve mood swings, but in cyclothymia, these swings are less severe than in bipolar disorder. The symptoms in cyclothymia don’t meet the full criteria for manic or major depressive episodes, and the overall duration of symptoms is a crucial distinguishing factor.
The intensity, duration, and specific symptoms experienced are crucial for diagnosis. A thorough history, symptom assessment, and sometimes even psychological testing are vital to arrive at the correct diagnosis.
Q 6. Outline the stages of bipolar disorder and the appropriate treatment strategies for each.
Bipolar disorder is often conceptualized in terms of stages, although the transition between stages can be gradual and not always clearly defined. Treatment strategies vary based on the stage:
- Euthymia (Stable Mood): This is the goal of long-term treatment. Strategies include continuing mood stabilizers, therapy (psychoeducation, CBT, family-focused therapy), regular monitoring, and lifestyle adjustments (sleep hygiene, stress management, healthy diet, exercise).
- Hypomania: Mild mood elevation, increased energy, and reduced need for sleep might not require medication changes, but close monitoring and consideration of medication adjustments are essential. Therapy is crucial to help manage potential risky behaviors.
- Mania: This requires immediate intervention. Hospitalization may be necessary to prevent harm to oneself or others. Treatment includes high doses of mood stabilizers (sometimes including antipsychotics), potentially benzodiazepines for short-term anxiety or agitation management, and close monitoring.
- Depression: Treatment might involve antidepressants (used cautiously and often in conjunction with mood stabilizers), therapy, and possibly other medications such as antipsychotics. The risk of switching to mania with antidepressants necessitates careful monitoring and potential adjustments to treatment plans.
The treatment approach is always individualized and tailored to the specific needs of each person.
Q 7. Describe your approach to managing acute manic episodes.
Managing acute manic episodes requires a multifaceted approach. The priority is to ensure safety and prevent harm. My approach would involve:
- Immediate Assessment: Thorough evaluation of the individual’s symptoms, risk for self-harm or harm to others, and medical status.
- Hospitalization (if necessary): For severe mania, hospitalization provides a structured environment, intensive monitoring, and rapid intervention.
- Medication Management: High doses of mood stabilizers, such as lithium or valproate, are often initiated or increased. Antipsychotic medication is usually added to quickly reduce symptoms and prevent further escalation.
- Supportive Care: This includes addressing basic needs (sleep, nutrition, hydration), engaging in activities that promote relaxation and reduce agitation, and ensuring adequate supervision.
- Psychoeducation: Helping the individual understand their illness and the importance of adherence to treatment.
- Family Involvement: Engaging family members in the treatment process through family-focused therapy or educational support.
- Gradual Dose Reduction: Once the acute phase has subsided, medication is gradually reduced under close clinical supervision to find the lowest effective dose that maintains stability.
The goal is to stabilize the mood, reduce symptoms, and prevent relapse. Regular follow-up care is essential for long-term management.
Q 8. Explain your approach to managing acute depressive episodes.
Managing acute depressive episodes in bipolar disorder requires a multifaceted approach prioritizing safety and symptom reduction. This involves a careful assessment to rule out other contributing factors, followed by a rapid and targeted intervention strategy.
Firstly, we need to evaluate the severity of the depression. Is the individual experiencing suicidal ideation? Are they able to meet their basic needs? This assessment guides the choice of treatment. For mild to moderate depression, psychotherapy, such as Cognitive Behavioral Therapy (CBT), may be sufficient, alongside monitoring and support. For moderate to severe depression, medication is crucial. This typically involves antidepressants, but the choice requires careful consideration due to the risk of triggering a manic episode. Sometimes, we might use an atypical antipsychotic medication or a mood stabilizer in conjunction with, or instead of, an antidepressant.
A common strategy is to start with a low dose of medication and gradually increase it under close monitoring. We meticulously track the patient’s mood, sleep, appetite, energy levels, and any other relevant symptoms. Regular appointments allow for quick adjustments to medication or therapy, ensuring optimal symptom management and minimizing potential adverse effects. In cases of severe depression with significant suicidal risk, hospitalization might be necessary to ensure safety and facilitate more intensive treatment, often involving daily monitoring and potentially intravenous medication.
For example, I recently worked with a patient experiencing a severe depressive episode. We started with a low dose of an atypical antipsychotic and a mood stabilizer. We also implemented CBT to address negative thought patterns and behavioral changes. Through weekly monitoring and medication adjustments, we saw significant improvement in just a few weeks. This approach demonstrates the importance of a collaborative, individualized treatment plan tailored to the specific needs of the patient.
Q 9. What are the different types of psychotherapy effective in treating bipolar disorder?
Several types of psychotherapy have proven effective in treating bipolar disorder. The goal isn’t just to manage symptoms but also to equip individuals with coping mechanisms and strategies for long-term stability.
- Cognitive Behavioral Therapy (CBT): This focuses on identifying and changing negative thought patterns and behaviors that contribute to mood instability. It helps individuals develop skills to manage stress, improve sleep hygiene, and regulate emotions.
- Interpersonal and Social Rhythm Therapy (IPSRT): This targets the disruption of social rhythms and interpersonal relationships, common in bipolar disorder. It helps patients establish regular sleep-wake cycles, mealtimes, and social routines, contributing to mood stabilization.
- Family-Focused Therapy (FFT): This involves educating family members about bipolar disorder and providing them with skills to support the individual effectively. It helps improve communication and reduce conflict within the family system, which can be crucial for relapse prevention.
- Psychoeducation: This is a crucial component of most therapies. It provides individuals and their families with a deep understanding of the illness, its triggers, and its management. It empowers patients to take an active role in their treatment and helps reduce stigma.
The choice of psychotherapy often depends on the individual’s specific needs and preferences. Sometimes, a combination of therapies is most effective. For instance, a patient might benefit from CBT to address negative thinking alongside IPSRT to stabilize their daily routines. The therapeutic relationship and the therapist’s expertise are also key factors in treatment success.
Q 10. How do you assess the risk of suicide in individuals with bipolar disorder?
Assessing suicide risk in individuals with bipolar disorder requires a thorough and sensitive approach. It’s not just about asking if they’re suicidal; it’s about understanding the depth and intensity of their thoughts and plans.
The assessment involves several components:
- Direct questioning: Openly asking about suicidal thoughts, plans, and intentions. Using specific questions, such as “Have you thought about harming yourself?” or “Have you developed a plan for suicide?”
- Assessing risk factors: Identifying factors that increase suicide risk, such as previous suicide attempts, hopelessness, impulsivity, substance abuse, recent significant losses, and access to lethal means. A history of manic episodes with impulsive behavior is a key consideration.
- Assessing protective factors: Identifying factors that may reduce suicide risk, such as strong social support, positive relationships, and a sense of purpose or hope.
- Clinical judgment: Integrating all information gathered to arrive at a professional clinical judgment about the level of risk. This considers the patient’s overall presentation, their current mental state, and their history.
Tools like standardized risk assessment scales can be helpful, but clinical judgment based on the individual’s unique circumstances remains essential. A high-risk assessment might necessitate hospitalization or intensified outpatient treatment, including close monitoring and potentially medication adjustments.
Q 11. Describe your strategies for relapse prevention in bipolar disorder.
Relapse prevention in bipolar disorder is a cornerstone of effective long-term management. It’s about empowering individuals to recognize early warning signs and implement proactive strategies to prevent mood episodes from escalating.
My strategies typically include:
- Medication adherence: Consistent medication is the most crucial aspect. We work together to find a medication regimen that’s tolerable and effective.
- Psychotherapy: Ongoing therapy, especially CBT and IPSRT, equips individuals with coping mechanisms and helps them manage stress and potential triggers.
- Lifestyle modifications: This includes regular sleep, healthy diet, regular exercise, stress management techniques (yoga, meditation), and limiting substance use. These factors significantly impact mood stability.
- Early warning sign identification: Working with the patient to identify their personal warning signs (e.g., sleep disturbances, increased irritability, racing thoughts) allows for prompt intervention before a full-blown episode develops.
- Crisis planning: Developing a detailed plan that outlines steps to take if early warning signs appear or if an episode begins. This may include contacting their therapist, psychiatrist, or loved ones, or having a pre-arranged safety plan in place.
- Regular monitoring: Consistent follow-up appointments allow for timely adjustments to treatment and early detection of potential problems.
For example, I work with patients to create personalized “mood trackers” where they record their mood daily, noting any changes or potential triggers. This self-monitoring is crucial for early intervention and preventing relapses. A proactive approach like this significantly improves outcomes.
Q 12. How do you work with patients and their families to develop a comprehensive treatment plan?
Developing a comprehensive treatment plan for bipolar disorder requires a collaborative effort involving the patient, their family (if they wish to be involved), and the treatment team. This is a shared decision-making process, emphasizing patient autonomy and ensuring everyone feels heard and understood.
The process involves:
- Assessment: A thorough evaluation to understand the patient’s history, current symptoms, and overall functioning. This includes a psychiatric evaluation, psychological testing (if necessary), and sometimes a family interview.
- Goal setting: Collaboratively establishing realistic and achievable goals. This might involve reducing the frequency and severity of mood episodes, improving overall functioning, enhancing social relationships, and improving quality of life.
- Treatment plan development: Designing a customized plan based on the assessment and goals. This includes medication management, psychotherapy, lifestyle changes, and relapse prevention strategies.
- Shared decision-making: Regularly reviewing and adjusting the treatment plan as needed, involving the patient and their family in the process. Flexibility and adaptation are crucial as the patient’s needs and circumstances change.
- Education and support: Providing education about bipolar disorder to both the patient and family, promoting understanding, reducing stigma, and building effective support systems.
Involving the family is particularly important, as their support and understanding are crucial for relapse prevention. I often hold family sessions to facilitate communication, address concerns, and equip the family with strategies to support their loved one effectively.
Q 13. Discuss the importance of medication adherence in managing bipolar disorder.
Medication adherence is paramount in managing bipolar disorder. Consistent medication significantly reduces the frequency and severity of mood episodes, improves overall functioning, and minimizes the risk of hospitalization and suicide. Non-adherence can lead to relapses, potentially resulting in severe consequences.
The reasons for non-adherence can be multifaceted, including:
- Side effects: Many mood stabilizers and antipsychotics can have side effects that make adherence challenging. Weight gain, drowsiness, or tremors are some common examples. Addressing these issues through medication adjustments or strategies to manage side effects is crucial.
- Cost: The cost of medication can be a significant barrier. We explore options to make medication affordable and accessible.
- Stigma: The stigma surrounding mental illness can make individuals reluctant to take medication.
- Misunderstandings about the illness: Lack of understanding of the illness and its treatment can lead to non-adherence. Education is key to improve adherence.
- Poor therapeutic alliance: A weak relationship with the healthcare provider can hinder adherence.
Therefore, addressing these barriers and fostering a strong therapeutic alliance is vital for improving medication adherence.
Q 14. What strategies do you use to improve medication adherence?
Improving medication adherence requires a proactive and multi-pronged approach tailored to the individual’s specific needs and challenges.
Strategies I employ include:
- Shared decision-making: Involving the patient in choosing medication and treatment strategies promotes a sense of ownership and control, increasing their commitment to adherence.
- Addressing side effects: Working collaboratively to find ways to manage or minimize side effects can significantly improve compliance. This may involve adjusting medication dosage, adding other medications to counteract side effects, or exploring non-pharmacological strategies.
- Medication reminders: Utilizing pill organizers, phone alarms, or apps to remind patients to take their medication.
- Support systems: Engaging family members or friends to provide support and reminders.
- Psychoeducation: Regularly educating the patient about their illness, medication, and the importance of adherence.
- Building a strong therapeutic relationship: Creating a trusting and supportive therapeutic environment fosters open communication and increases the patient’s willingness to adhere to their treatment plan.
- Utilizing technology: Employing apps or digital tools that facilitate medication tracking and provide reminders can enhance adherence.
A comprehensive approach that addresses both the medical and psychosocial aspects of non-adherence is essential for success. It’s often an iterative process, requiring flexibility and adaptation to meet the ever-evolving needs of the individual.
Q 15. How do you address challenges in managing treatment in patients with comorbid substance use disorders?
Comorbid substance use disorders significantly complicate bipolar disorder treatment. Addressing this requires a multifaceted approach focusing on both substance use and mood stabilization. We can’t effectively treat the bipolar disorder if the substance use remains uncontrolled, and vice-versa.
My strategy involves a collaborative care model. This includes:
- Integrated treatment: A coordinated approach where a psychiatrist, therapist, and addiction specialist work together. This ensures consistent monitoring and treatment adjustments across both disorders.
- Medication management: Careful selection of mood stabilizers with a low potential for abuse or interaction with substances. We might also utilize medications to help manage cravings and withdrawal symptoms.
- Motivational interviewing: This therapeutic technique helps patients explore their ambivalence towards change, fostering intrinsic motivation for recovery.
- Relapse prevention planning: Developing coping strategies for managing triggers and high-risk situations related to both substance use and mood episodes.
- Support groups: Connecting patients with peer support groups tailored to their specific needs (e.g., groups for individuals with both bipolar and substance use disorders).
For example, a patient might be prescribed a mood stabilizer like lamotrigine, while also participating in individual and group therapy to address their substance use. Regular drug screenings and close monitoring of mood symptoms are essential throughout this process.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your approach to managing patients who experience treatment resistance.
Treatment resistance in bipolar disorder is a significant challenge, but it doesn’t mean a lack of options. My approach involves a systematic process of optimization and augmentation:
- Careful medication review: We thoroughly examine the patient’s current medication regimen, including dosage, potential interactions, and adherence. Sometimes, a simple dosage adjustment or switch to a different medication within the same class can make a significant difference.
- Augmentation strategies: If a mood stabilizer alone isn’t effective, we may add other medications, such as antipsychotics or antidepressants, in a carefully planned manner. This requires close monitoring to prevent adverse effects.
- Psychotherapy: Cognitive Behavioral Therapy (CBT) and other forms of psychotherapy are crucial for developing coping skills and addressing underlying psychological factors contributing to mood instability.
- Electroconvulsive therapy (ECT): ECT remains a safe and effective treatment option for severe, treatment-resistant bipolar disorder, particularly in cases of rapid cycling or catatonia.
- Referral to specialist: If necessary, I would refer the patient to a specialist in treatment-resistant bipolar disorder for a second opinion and additional treatment options such as deep brain stimulation.
Consider a patient who has tried several mood stabilizers without significant improvement. We might then add an atypical antipsychotic, like quetiapine, while concurrently implementing CBT to help manage stressors and improve coping mechanisms.
Q 17. How do you incorporate patient preferences and values into treatment decisions?
Shared decision-making is paramount. Treatment should always align with the patient’s preferences and values. This means actively involving them in every stage of the process.
My approach includes:
- Educating the patient: Providing comprehensive information about their diagnosis, treatment options, potential benefits and risks, and long-term goals.
- Open communication: Creating a safe and trusting therapeutic alliance where patients feel comfortable expressing their concerns, preferences, and values.
- Collaborative goal setting: Working with patients to set realistic and achievable treatment goals that reflect their priorities and values.
- Regular review and adjustment: Continuously monitoring treatment efficacy and patient satisfaction, and adjusting the treatment plan as needed. We might need to adjust if side effects are too difficult to manage or if the patient is struggling with adherence.
For example, if a patient strongly prefers avoiding antipsychotics due to concerns about side effects, we’ll explore alternative strategies like optimizing mood stabilizers and emphasizing psychotherapy. The treatment plan should be a partnership, not a prescription.
Q 18. What are the ethical considerations when treating individuals with bipolar disorder?
Ethical considerations in bipolar disorder treatment are multifaceted and critically important.
- Informed consent: Patients must fully understand their diagnosis, treatment options, potential risks, and benefits before making decisions about their care.
- Beneficence and non-maleficence: We must always act in the best interest of the patient while minimizing potential harm. This involves careful medication selection and monitoring for side effects.
- Autonomy: Respecting the patient’s right to make their own decisions about their treatment, even if those decisions differ from clinical recommendations.
- Confidentiality: Protecting the patient’s privacy and ensuring that their personal information is not disclosed without their consent.
- Justice and equity: Ensuring that all patients have access to high-quality care, regardless of their socioeconomic status, race, or other demographic factors. This often requires advocating for better access to mental health services.
Ethical dilemmas can arise, such as when a patient lacks insight into their illness and refuses necessary treatment, or when a patient’s decisions pose a risk to themselves or others. These require careful consideration and potentially involving legal and ethical consultation.
Q 19. How do you ensure confidentiality and maintain the privacy of patient information?
Maintaining patient confidentiality is an absolute ethical and legal imperative. My practice adheres strictly to HIPAA regulations and other relevant privacy laws.
Specific strategies include:
- Secure storage of records: All patient records are stored in secure electronic health records (EHR) systems with appropriate access controls.
- Limited access to information: Only authorized personnel involved in the patient’s care can access their information.
- Privacy protection in communication: All communications, both electronic and paper-based, are handled with utmost care to prevent unauthorized disclosure. This includes using secure messaging systems and encrypting sensitive information.
- Patient authorization for disclosure: Information is only shared with other healthcare providers or family members with the patient’s explicit written consent, except in situations where disclosure is legally mandated (e.g., mandated reporting of harm to self or others).
- Data breach preparedness: We have protocols in place to address any potential data breaches, including reporting procedures and strategies to mitigate harm to patients.
It’s essential to routinely review and update our security protocols and staff training to ensure ongoing compliance with privacy regulations.
Q 20. Explain the role of family-focused therapy in the treatment of bipolar disorder.
Family-focused therapy (FFT) plays a vital role in managing bipolar disorder, especially given its impact on family dynamics. It’s based on the understanding that family relationships often significantly influence the course of the illness and recovery.
In FFT, we work with both the patient and their family to:
- Improve communication: We teach families effective communication techniques to reduce conflict and improve understanding.
- Educate about bipolar disorder: This helps families understand the symptoms, causes, and treatment of the illness, reducing stigma and improving support.
- Develop coping strategies: We equip families with strategies to manage crises, prevent relapse, and support the patient during challenging times.
- Enhance problem-solving skills: Families learn to collaboratively solve problems and address challenges that arise in their interactions.
- Foster a supportive environment: The goal is to build a supportive and understanding family environment that facilitates recovery.
For instance, FFT might involve family sessions where we address communication issues between a patient and their spouse, educating the family on effective strategies to support the patient during manic episodes and providing them with tools to manage stress within the family system.
Q 21. What are some strategies for managing the side effects of mood stabilizers?
Mood stabilizers, while crucial for managing bipolar disorder, can have significant side effects. Managing these side effects is essential for treatment adherence and overall well-being.
Strategies include:
- Careful medication selection: Choosing medications with a more favorable side effect profile whenever possible. This might involve weighing the benefits of a particular medication against the potential risks, considering the patient’s individual circumstances and preferences.
- Dosage adjustments: Starting with a low dose and gradually increasing it as tolerated, closely monitoring for side effects.
- Pharmacological interventions: Adding other medications to manage specific side effects. For example, if a patient experiences weight gain with a particular mood stabilizer, we might add a medication to help manage that. Other side effects might be mitigated by addressing them through changes in diet or other lifestyle modifications.
- Non-pharmacological interventions: Lifestyle modifications can significantly impact side effects. For example, regular exercise can counter weight gain and improve mood, while adequate sleep can help reduce fatigue.
- Patient education and support: Providing patients with detailed information about potential side effects and strategies for managing them. Offering emotional support and encouragement can be invaluable during this process.
For example, if a patient experiences significant weight gain with lithium, we might adjust the dose or explore alternative mood stabilizers. Simultaneously, we encourage increased physical activity and a healthy diet to mitigate the weight gain. Close monitoring and open communication between the patient and the clinical team are key.
Q 22. Discuss the role of electroconvulsive therapy (ECT) in the treatment of bipolar disorder.
Electroconvulsive therapy (ECT) is a treatment option for severe cases of bipolar disorder, particularly during acute manic or depressive episodes that haven’t responded to medication or other therapies. It involves a brief controlled seizure induced by electrical stimulation of the brain under general anesthesia. While it might sound drastic, ECT is remarkably effective and relatively safe when administered by experienced professionals.
ECT’s role isn’t as a first-line treatment, but rather a last resort for individuals experiencing life-threatening symptoms. It’s particularly helpful in situations where rapid symptom reduction is critical, such as severe suicidal ideation or catatonia.
The mechanism by which ECT works isn’t entirely understood, but it’s thought to influence neurotransmitter systems and brain plasticity, potentially resetting disrupted neural pathways that contribute to mood disorders. Common side effects are short-term memory loss and confusion, which generally resolve within weeks. However, careful monitoring and supportive measures are essential to minimize these.
Q 23. Describe your understanding of the stages of grief and how it relates to bipolar disorder.
The Kübler-Ross model of grief – denial, anger, bargaining, depression, and acceptance – offers a helpful framework, although it’s crucial to remember it’s not a rigid linear process. People experiencing bipolar disorder can navigate these stages in a non-linear, sometimes intense way, and these emotions aren’t necessarily directly caused by a loss but rather a manifestation of the illness itself.
For example, a manic episode might involve denial of the disorder’s severity, followed by anger at perceived limitations or restrictions. Depressive episodes can obviously mirror the depression stage of grief intensely. Even during periods of relative stability, fluctuating mood can cause individuals to revisit stages of the grief process related to the impact of the disorder on their lives, relationships, and future aspirations. Understanding this connection helps clinicians provide compassionate support and tailor treatments to address both the emotional turmoil and the underlying bipolar condition. It’s important to avoid pathologizing normal grief responses in the context of bipolar disorder, as both can co-exist.
Q 24. How do you communicate effectively with patients and their families about bipolar disorder?
Effective communication is paramount in bipolar disorder treatment. I prioritize a collaborative approach, fostering a safe and non-judgmental environment. I begin by actively listening to the patient and their family, validating their experiences and concerns, without medical jargon whenever possible. I use clear, simple language, explaining the disorder and treatment options in terms they can understand.
With patients, I emphasize self-management skills like mood tracking, stress reduction techniques, and adherence to medication plans. Open discussion of potential side effects and realistic expectations about treatment outcomes is essential. With families, I provide psychoeducation about bipolar disorder, dispel myths, and encourage supportive behavior while setting realistic expectations for the patient’s recovery. Regular check-ins, both individually and with families, help to monitor progress and adjust strategies as needed. Collaboration is key—it’s a team effort.
Q 25. What are the long-term goals of treatment for bipolar disorder?
Long-term goals for bipolar disorder treatment are multifaceted and patient-centered. They extend beyond simply stabilizing mood swings to encompass improved quality of life and overall well-being. This includes:
- Achieving and maintaining euthymia (a stable mood): This is the cornerstone, minimizing mood swings and reducing the severity of manic and depressive episodes.
- Improving psychosocial functioning: This involves enhancing interpersonal relationships, vocational skills, and social engagement.
- Preventing relapse and hospitalization: Strategies like medication adherence, lifestyle changes, and early intervention can drastically minimize these risks.
- Enhancing self-management skills: Equipping patients with the tools to recognize their triggers, monitor their mood, and proactively manage symptoms.
- Promoting resilience and coping mechanisms: Building patient confidence in their ability to navigate challenges and manage their condition effectively.
Ultimately, the goal is to help patients live fulfilling and productive lives despite their diagnosis. This may look different for each individual, but the core aim remains consistent: maximizing their overall well-being.
Q 26. Describe your experience working with diverse populations and addressing cultural considerations in bipolar disorder treatment.
Working with diverse populations requires cultural sensitivity and humility. It’s vital to understand how cultural backgrounds, beliefs, and practices can influence a patient’s experience with bipolar disorder and their engagement with treatment. For instance, some cultures may stigmatize mental illness, leading to reluctance to seek help. Others might attribute symptoms to spiritual or supernatural causes, potentially impacting the acceptance of Western medical interventions.
I address this by actively listening to patients’ narratives and incorporating their cultural perspectives into the treatment plan. I might collaborate with community leaders or cultural mediators to build trust and facilitate effective communication. I also make sure to offer culturally appropriate resources and materials. For example, I might provide materials in multiple languages or connect patients with culturally competent support groups. Flexibility and respect for individual differences are essential for achieving positive treatment outcomes in a diverse patient population. Ultimately, understanding and respecting the whole person – not just their diagnosis – is fundamental.
Q 27. How do you stay up-to-date on the latest research and best practices in bipolar disorder treatment?
Staying current in this rapidly evolving field requires a multifaceted approach. I regularly attend professional conferences and workshops, focusing on advancements in psychopharmacology, psychotherapy, and brain stimulation techniques. I actively engage with leading journals, subscribing to publications such as the American Journal of Psychiatry and the Archives of General Psychiatry. I also participate in continuing medical education (CME) courses and regularly review updated clinical guidelines.
Furthermore, I maintain professional memberships with organizations like the American Psychiatric Association (APA) to receive updates and benefit from the wealth of resources they provide. Keeping abreast of the latest research allows me to deliver the most effective and up-to-date care, ensuring that my patients benefit from the newest evidence-based treatments.
Q 28. Describe a challenging case involving a patient with bipolar disorder and how you addressed it.
One challenging case involved a young adult patient who presented with rapid cycling bipolar disorder, characterized by frequent and unpredictable shifts between manic and depressive episodes. She was resistant to medication, citing concerns about weight gain and other side effects. Her treatment history was complex, with previous hospitalizations and failed attempts at various medication regimens. She was also struggling with substance abuse.
My approach involved collaboratively developing a treatment plan that prioritized her concerns. We explored alternative medication options with fewer side effects, alongside engaging her in psychotherapy focused on coping mechanisms and relapse prevention. We also incorporated motivational interviewing to address her substance use. Regular check-ins, open communication, and a willingness to adjust the plan as needed were key. While complete resolution of her symptoms hasn’t been achieved, we’ve successfully reduced the frequency and intensity of her mood swings. This case highlighted the importance of patient-centered care, flexibility, and a multidisciplinary approach in tackling complex presentations of bipolar disorder.
Key Topics to Learn for Bipolar Disorder Treatment Interview
- Mood Stabilizers: Understanding the mechanisms of action, therapeutic uses, and side effects of common mood stabilizers (Lithium, valproate, lamotrigine, etc.). Consider practical application in case selection and medication management.
- Antipsychotics: Knowledge of atypical antipsychotics’ role in managing manic and depressive episodes, including their efficacy, side effects, and potential interactions with other medications. Be prepared to discuss practical application in acute and maintenance phases.
- Psychotherapy: Familiarity with various therapeutic approaches like Cognitive Behavioral Therapy (CBT), interpersonal and social rhythm therapy (IPSRT), and family-focused therapy (FFT). Discuss their effectiveness in managing symptoms and improving overall functioning. Consider how you would integrate these approaches in a treatment plan.
- Diagnostic Criteria & Assessment: A thorough understanding of DSM-5 criteria for Bipolar I and II disorders, including differential diagnosis from other conditions. Practice conducting a comprehensive assessment considering patient history, symptoms, and psychosocial factors.
- Treatment Planning & Monitoring: Ability to develop individualized treatment plans based on patient needs and preferences. Discuss strategies for monitoring treatment efficacy and adjusting medication or therapy as needed. Include practical considerations like adherence and relapse prevention.
- Crisis Management & Stabilization: Knowledge of strategies for managing acute manic or depressive episodes, including hospitalization criteria and crisis intervention techniques. Discuss ethical considerations in decision-making during crises.
- Long-Term Management & Relapse Prevention: Understanding the importance of long-term treatment adherence, strategies for relapse prevention, and the role of patient education and support systems.
- Ethical Considerations & Cultural Competency: Awareness of ethical dilemmas in the treatment of bipolar disorder, such as informed consent, patient autonomy, and confidentiality. Demonstrate understanding of cultural factors that influence treatment approaches and outcomes.
Next Steps
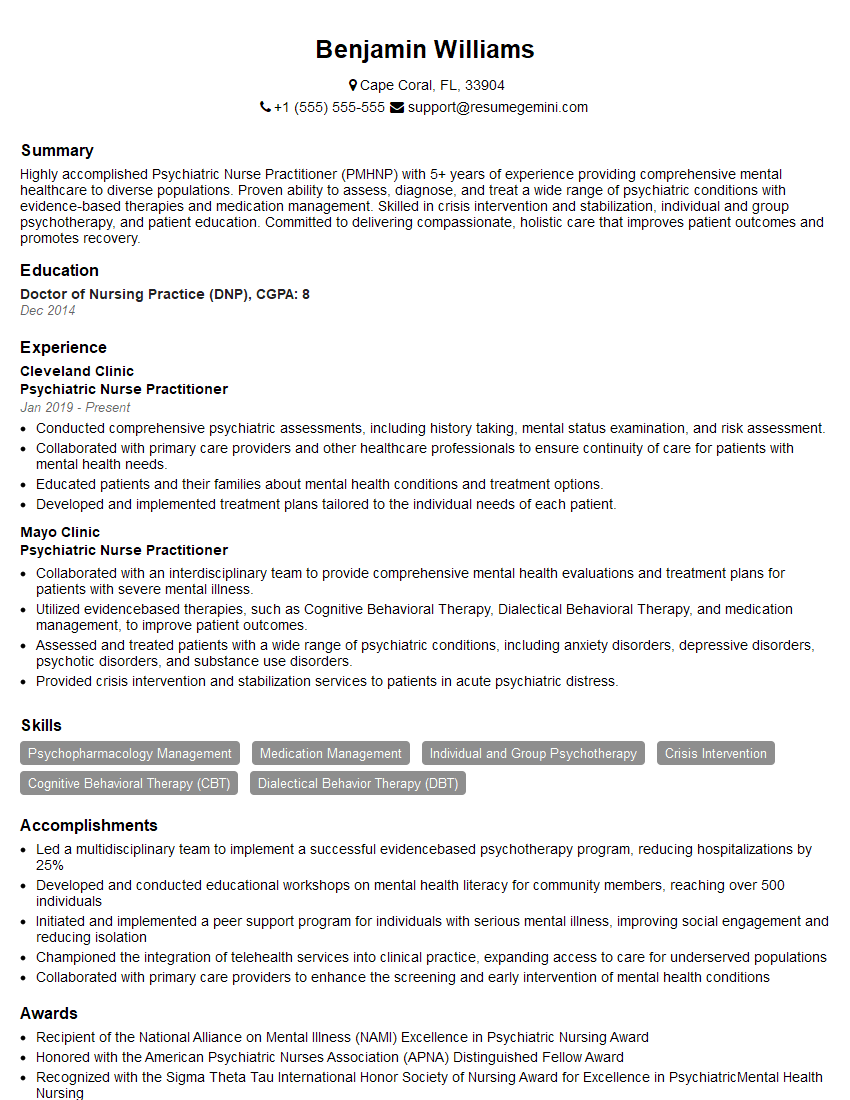
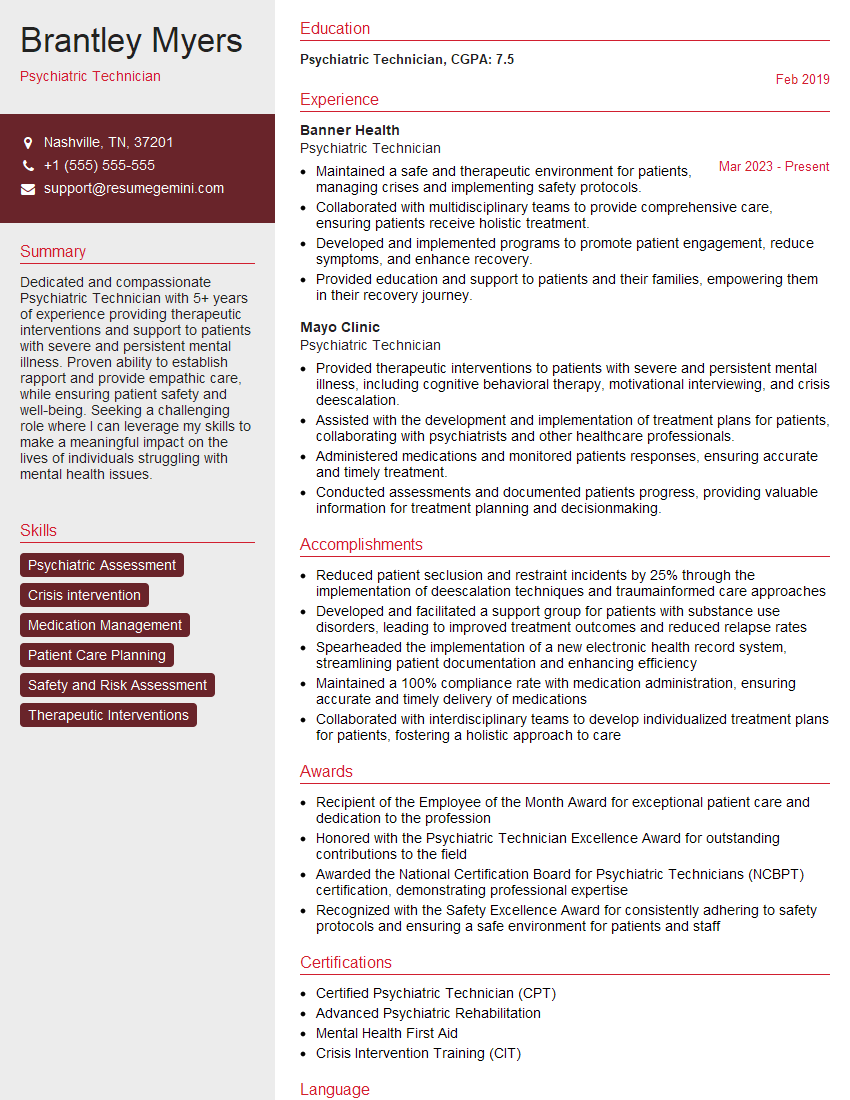
Mastering Bipolar Disorder Treatment significantly enhances your career prospects in mental health. A strong understanding of these key areas demonstrates expertise and professionalism, opening doors to advanced roles and increased earning potential. To maximize your job search success, creating an Applicant Tracking System (ATS)-friendly resume is crucial. ResumeGemini is a trusted resource to help you build a compelling and effective resume that highlights your skills and experience. Examples of resumes tailored to Bipolar Disorder Treatment are available to guide you. Invest time in crafting a strong resume – it’s your first impression to potential employers.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.