Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Blood Product Inventory and Distribution interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Blood Product Inventory and Distribution Interview
Q 1. Explain the process of blood product inventory management, including tracking, storage, and expiration.
Blood product inventory management is a critical function ensuring the timely availability of life-saving components. It involves a sophisticated system of tracking, storage, and expiration management to maintain quality and prevent wastage. Think of it like managing a highly perishable, yet incredibly valuable, inventory – lives depend on its effective management.
Tracking: This starts the moment blood is collected. Each unit is assigned a unique identifier, meticulously recorded in a blood bank information system (BBIS). This system tracks the blood’s journey – from donation to processing, storage, and finally, transfusion. We use barcodes and RFID technology to automate this process, minimizing human error. Real-time tracking allows us to know the exact location and status of every unit at any given time.
Storage: Blood and its components require specific temperature and humidity conditions to maintain viability. Different products have different requirements (as discussed in the next question). We use sophisticated refrigerators and freezers with monitoring systems that alert us to any temperature deviations. Inventory is organized strategically to ensure efficient access and prevent cross-contamination.
Expiration: Each blood product has a limited shelf life. The BBIS automatically flags units nearing expiration, prompting staff to prioritize their use. We employ a first-in, first-out (FIFO) system to minimize waste. Near-expiration units are flagged for prioritization to hospitals with high demand.
Q 2. Describe the different blood product types and their specific storage requirements.
Blood products are diverse, each with unique characteristics and storage needs. Think of it like a specialized pharmacy with incredibly delicate products. Here are a few key examples:
- Packed Red Blood Cells (PRBCs): Stored at 1-6°C (34-43°F) for up to 42 days. These are crucial for restoring oxygen-carrying capacity in patients.
- Platelets: Stored at 20-24°C (68-75°F) with continuous gentle agitation for up to 5 days. Platelets are essential for clotting.
- Fresh Frozen Plasma (FFP): Stored at -18°C (0°F) or colder for up to 12 months. FFP is used to replace clotting factors.
- Cryoprecipitate: Stored at -18°C (0°F) or colder for up to 12 months. Cryoprecipitate is rich in clotting factors and fibrinogen.
The storage temperatures and durations are crucial; even slight deviations can compromise the integrity and safety of the blood products.
Q 3. How do you ensure the quality and safety of blood products throughout the distribution process?
Ensuring the quality and safety of blood products is paramount. We employ a multi-layered approach, starting from donor screening and extending throughout the entire process. It’s like building a chain of safety, where each link is equally important.
- Donor Screening: Rigorous screening processes minimize the risk of transmitting infectious diseases.
- Apheresis and Component Preparation: Advanced techniques ensure safe separation and processing of blood components.
- Storage and Transportation: Stringent temperature monitoring and validated transport systems prevent degradation.
- Testing and Quality Control: Multiple tests are conducted at various stages to detect abnormalities and ensure product quality. This includes testing for infectious diseases like HIV, Hepatitis B and C, and syphilis.
- Traceability and Documentation: Meticulous records are maintained throughout the entire blood product lifecycle, facilitating rapid recall and investigation should any issues arise.
Continuous monitoring and adherence to stringent guidelines, coupled with regular audits, are fundamental to ensuring that only safe and high-quality blood products reach patients.
Q 4. What are the key challenges in managing blood product inventory, and how would you address them?
Managing blood product inventory presents unique challenges. The perishable nature of the products, coupled with fluctuating demand, makes it a complex logistical operation.
- Perishability: Blood products have a limited shelf life, leading to potential wastage if not managed effectively.
- Demand Fluctuation: Demand varies significantly based on trauma incidents, scheduled surgeries, and seasonal factors.
- Inventory Tracking and Management: Maintaining an accurate inventory requires sophisticated systems and processes.
- Transportation and Logistics: Ensuring timely delivery while maintaining product integrity is crucial.
Addressing these challenges involves:
- Implementing advanced inventory management systems: Utilizing BBIS with real-time tracking and predictive analytics.
- Optimizing storage and distribution strategies: Employing efficient storage layouts and optimized delivery routes.
- Collaboration with healthcare facilities: Predictive modeling of demand based on historical data and hospital forecasts.
- Investing in training and education: Ensuring staff are proficient in proper handling and management of blood products.
Q 5. Explain your experience with blood bank information systems (BBIS) and related software.
My experience with BBIS is extensive. I’ve worked with various systems, from legacy systems to modern, cloud-based solutions. I’m proficient in data entry, report generation, inventory management modules, and quality control features. For example, I’ve utilized BloodTrack and Hemos, both of which allowed for automated ordering, real-time inventory monitoring and detailed reporting. I’m adept at troubleshooting system issues, customizing reports, and training staff on system usage. I understand the importance of data integrity, compliance with regulatory standards, and seamless integration with other hospital systems.
Q 6. How do you prioritize blood product distribution based on urgency and need?
Prioritizing blood product distribution requires a structured approach that considers both urgency and clinical need. We follow a tiered system similar to emergency response protocols.
- Critical Patients: Patients with life-threatening conditions requiring immediate transfusion receive the highest priority.
- Urgent Patients: Patients with conditions requiring prompt transfusion but not immediately life-threatening.
- Routine Transfusions: Patients who need blood for scheduled procedures or ongoing treatments.
The BBIS helps in this process by generating reports that prioritize units based on blood type, component, and expiration date. It alerts us to critical shortages and facilitates efficient allocation of available units. We also work closely with hospitals to understand their immediate requirements.
Q 7. Describe your experience with blood product ordering, receiving, and reconciliation.
My experience encompasses the entire ordering, receiving, and reconciliation process. This is a cycle of meticulous attention to detail to maintain inventory accuracy.
- Ordering: We use the BBIS to generate orders based on projected demand and inventory levels. This involves collaborating with hospitals to understand their needs and ensuring timely orders. I use predictive analytics to forecast future demand.
- Receiving: Upon delivery, we verify the quantity and quality of each shipment, meticulously checking against the order details and examining the products for any damage or temperature deviations. Each unit is scanned and its arrival is logged into the BBIS.
- Reconciliation: This crucial step involves comparing the received quantity with the ordered quantity and adjusting the inventory accordingly. Discrepancies are investigated to ensure accuracy. We maintain a detailed record of all transactions, tracing each unit from donation to transfusion.
These steps are essential for maintaining an accurate inventory, preventing shortages, and ensuring the safe and efficient distribution of blood products.
Q 8. How do you handle discrepancies in blood product inventory?
Discrepancies in blood product inventory are a serious concern, requiring immediate attention to ensure patient safety and maintain accurate records. We use a multi-pronged approach to address these issues. First, we implement robust inventory management systems, often utilizing barcode scanning and real-time tracking. This allows for immediate detection of any inconsistencies between physical counts and the system’s records. Second, we conduct regular physical inventory checks, comparing our manual counts against the digital inventory to identify any discrepancies. Third, we investigate the root cause of any discrepancy. This may involve reviewing order forms, verifying blood component transfers between storage areas, and checking for any data entry errors. For example, if a unit of packed red blood cells is missing, we’d trace it back through its entire journey – from its arrival to its potential use or disposal – looking for evidence of misplaced labeling or accidental discarding. Finally, we implement corrective actions to prevent future discrepancies, such as staff training on proper inventory procedures, improved record-keeping practices, and regular equipment maintenance of our barcode scanning system. This methodical process ensures inventory accuracy and minimizes errors.
Q 9. Explain your understanding of blood product expiration and disposal procedures.
Blood product expiration is governed by strict guidelines to maintain safety and efficacy. Each blood component has a specific shelf life, clearly indicated on its label. For example, red blood cells generally have a shelf life of 42 days when stored at specific temperatures, while platelets have a shorter shelf life of 5 days. Once a product expires, it’s immediately removed from inventory and disposed of according to established protocols. These protocols typically involve returning the expired unit to the blood bank, where it’s segregated from usable products, documented, and then disposed of through licensed medical waste disposal services. This is crucial to prevent accidental use of outdated blood, which could have serious consequences for patients. We maintain meticulous records of expiration dates and disposal actions, ensuring complete traceability for both regulatory compliance and internal quality control.
Q 10. How do you maintain compliance with regulatory requirements related to blood product handling?
Maintaining compliance with regulatory requirements is paramount in blood product handling. We adhere to strict guidelines set by agencies like the FDA (in the US) and equivalent bodies in other countries. This involves rigorous adherence to Good Manufacturing Practices (GMP), which cover all aspects of blood collection, processing, storage, and distribution. We maintain detailed records for every blood product, including donor information, testing results, processing details, storage conditions, and distribution records. These records are regularly audited both internally and by regulatory agencies to ensure ongoing compliance. Furthermore, we conduct regular staff training on current regulations and best practices. We emphasize the importance of proper handling techniques, such as maintaining appropriate temperatures, avoiding contamination risks, and adhering to strict labeling protocols. Non-compliance with even minor aspects can result in severe penalties, so our commitment to compliance is unwavering.
Q 11. What are the key performance indicators (KPIs) used to monitor blood bank efficiency?
Key Performance Indicators (KPIs) for blood bank efficiency are carefully selected to measure various aspects of our operations. These include:
- Inventory Turnover Rate: Measures how quickly blood products are used. A higher rate suggests efficient inventory management.
- Expiration Rate: Indicates the percentage of blood products that expire before use. A lower rate is desirable.
- Order Fulfillment Rate: Shows the percentage of blood product orders that are filled on time and in full. A high rate signifies efficient order processing.
- Blood Product Availability: Tracks the percentage of time that specific blood types or components are available to meet demand.
- Time to Issue: Measures the time it takes to process a blood request from order placement to delivery. A shorter time reflects improved efficiency.
- Error Rate: Tracks the number of errors in processing, storage, or distribution. A low error rate is critical for patient safety.
Q 12. How do you optimize blood product inventory levels to minimize waste and meet demand?
Optimizing blood product inventory levels is a complex balancing act between minimizing waste and ensuring sufficient supply to meet demand. We employ sophisticated forecasting models based on historical data, seasonal trends, and predicted demand to estimate future needs. This includes considering factors such as local demographics, hospital patient volumes, and scheduled surgeries. These predictions are refined using real-time data on blood product usage and incoming donations. We also utilize Just-in-Time (JIT) inventory strategies, aiming to minimize storage while ensuring adequate supply for immediate requirements. Regular collaboration with hospitals and transfusion services helps us accurately predict demand. Furthermore, we actively engage in blood drives and donor recruitment campaigns to ensure a consistent supply, reducing reliance on external sources. This integrated approach reduces waste by minimizing expiration while guaranteeing sufficient stock to meet patient needs.
Q 13. Describe your experience with blood product transportation and logistics.
Blood product transportation and logistics require specialized handling to maintain product integrity and patient safety. We use temperature-controlled vehicles equipped with GPS tracking and data loggers to monitor temperature fluctuations during transit. This ensures the blood products remain within the required temperature range throughout transportation. Delivery routes are carefully planned to minimize transit time and potential temperature excursions. We utilize specialized containers and packaging to protect blood products from shock and vibration. Moreover, we implement a rigorous chain-of-custody system, documenting each step of the transportation process, from pick-up to delivery, to ensure traceability and accountability. This system includes signatures, timestamps, and temperature readings at each transfer point. Real-time tracking allows for immediate response to any potential issues, such as vehicle breakdowns or temperature excursions, minimizing any risk to the blood products.
Q 14. How do you manage blood product recalls or emergencies?
Managing blood product recalls or emergencies requires a rapid and coordinated response. We have established protocols to handle such situations effectively. Upon receiving notification of a recall, we immediately identify the affected blood products in our inventory using our database system and batch numbers. These products are then quarantined and removed from circulation. We then trace all the affected units, notifying hospitals and transfusion centers that received them. This ensures immediate action to prevent their use. In case of emergencies, such as a sudden surge in demand following a major disaster, our established emergency response plan kicks in. This plan outlines procedures for rapidly mobilizing resources, coordinating with other blood banks, and prioritizing the distribution of blood products based on urgency. Regular drills and simulations help us refine our response capabilities and ensure seamless execution in critical situations. Communication is key during both recalls and emergencies, with rapid updates and transparent information shared with all stakeholders to ensure effective mitigation.
Q 15. Explain your experience with blood typing and crossmatching procedures.
Blood typing and crossmatching are crucial steps to ensure blood transfusion safety. Blood typing identifies the ABO (A, B, AB, O) and Rh (positive or negative) blood groups of both the donor and recipient. Crossmatching involves mixing a small sample of the recipient’s serum with the donor’s red blood cells to detect any incompatibility, preventing potentially fatal transfusion reactions.
In my experience, I’ve performed and overseen thousands of these procedures, utilizing both manual techniques (tube testing) and automated systems. For example, I’ve troubleshooted discrepancies between ABO typing and Rh typing results, ensuring the correct blood type assignment. This involved meticulous re-testing, investigating potential technical errors, and considering rare blood group systems. Another example is resolving incompatible crossmatches by identifying the specific antibodies causing the reaction and selecting compatible blood units, potentially using antigen-negative units.
My expertise extends to managing the entire process, from sample collection and labeling to result interpretation and documentation, adhering to strict quality control measures and regulatory guidelines. This rigorous approach guarantees the safety and efficacy of every transfusion.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are your strategies for preventing blood product contamination?
Preventing blood product contamination is paramount. My strategies encompass a multi-layered approach, starting with meticulous adherence to aseptic techniques during collection, processing, and storage. This includes using sterile equipment, employing proper hand hygiene, and maintaining a clean and disinfected work environment.
We utilize a comprehensive system of quality controls, including regular testing for bacterial contamination, endotoxin levels, and other potential contaminants. Any deviation from established protocols triggers immediate investigation and corrective action. For instance, if a batch of blood shows bacterial contamination, the entire batch is immediately discarded and a root cause analysis is performed to prevent recurrence. We also implement robust inventory management to ensure FIFO (First-In, First-Out) to minimize the risk of outdated units. Finally, staff training is ongoing, emphasizing continuous improvement and attention to detail.
Q 17. How do you ensure the accuracy and integrity of blood product labeling?
Accurate and unambiguous labeling is non-negotiable for blood product safety. Our system uses automated labeling systems, which minimizes human error. The labels include essential information such as the donor’s unique identification number, blood group, Rh type, component type (e.g., red blood cells, plasma), expiration date, and any relevant testing results. Barcodes are incorporated for seamless tracking and verification throughout the entire process.
Regular audits are performed to ensure label accuracy and adherence to standards. This includes checks of label legibility, completeness, and consistency with the donor records. Any discrepancies immediately trigger a thorough investigation. We have implemented a system where all labeling is double-checked before the unit is released for distribution. For example, if a label is found to be incorrect, the entire unit is quarantined and investigations begin to identify where the error occurred.
Q 18. How do you track and manage blood product donations?
We employ a sophisticated database management system to track blood product donations from the initial donor registration to the final transfusion. This system records donor demographics, medical history, blood type, testing results, and the disposition of each unit. This data is essential for maintaining donor records, recalling units if needed, and conducting epidemiological studies. The system also manages inventory, informing us of blood product availability and expiration dates.
The system generates reports for various purposes, such as donor deferral tracking, blood type inventory summaries, and transfusion reaction reports. For instance, a report might show us a shortage of O-negative blood, alerting us to initiate donor recruitment campaigns. This integrated system, used in conjunction with barcode scanners, ensures accuracy and efficiency across all aspects of blood product management.
Q 19. What are your experience with different blood storage technologies (e.g., refrigeration, freezing)?
My experience encompasses various blood storage technologies. Refrigeration is the standard method for storing most blood components at 1-6°C, extending their shelf life. Freezing is employed for long-term storage of plasma and other components. We use controlled-rate freezers to minimize ice crystal formation, ensuring component viability.
I’m familiar with various technologies including automated refrigeration systems with temperature monitoring and alarm systems, freezers equipped with liquid nitrogen storage capacity, and specialized storage containers to maintain optimal conditions throughout the storage period. For example, we meticulously monitor temperature fluctuations in our refrigerators and freezers, and immediately address any anomalies to prevent damage to blood components. Regular equipment maintenance is also a vital aspect of ensuring the optimal preservation of blood products.
Q 20. Describe your experience in developing and implementing blood bank policies and procedures.
I’ve been actively involved in developing and implementing numerous blood bank policies and procedures, always ensuring alignment with regulatory standards (e.g., FDA guidelines) and best practices. This involves creating comprehensive written protocols for all aspects of blood bank operations, from donor selection and blood collection to component preparation, storage, and distribution.
For instance, I led the implementation of a new electronic inventory management system. This streamlined the workflow, reduced errors, and improved efficiency in tracking blood products. Another project involved the development and implementation of a new adverse event reporting system. This standardized the reporting process and facilitated better analysis of transfusion-related complications. The development of these policies requires careful consideration of various factors, including safety, efficiency, and compliance with regulatory requirements.
Q 21. How do you train staff on proper blood product handling techniques?
Staff training is a continuous process. Our program incorporates both theoretical and practical training modules, covering all aspects of blood product handling, including aseptic techniques, quality control procedures, safety protocols, and regulatory compliance.
We use a blend of classroom lectures, hands-on workshops, and simulated scenarios to ensure competence and proficiency. For example, staff regularly participate in mock emergency situations to practice their responses to various challenges, ensuring they are well-prepared to handle real-world occurrences. Regular competency assessments are conducted to evaluate staff skills and identify areas for improvement. This continuous training ensures staff are up-to-date on best practices and technological advancements in the field.
Q 22. What are the common causes of blood product shortages, and how can they be mitigated?
Blood product shortages are a critical concern in healthcare, stemming from a complex interplay of factors. Think of it like a supply chain – if one part falters, the entire system suffers.
- Decreased Donor Participation: Seasonal fluctuations, fear of needles, or lack of awareness can lead to insufficient donations. We’ve seen this especially during periods of public health crises.
- Limited Collection Resources: Insufficient blood donation centers or outdated equipment can hinder efficient blood collection. Imagine a single blood bank serving a large population – it’s easily overwhelmed.
- Blood Product Shelf Life: Blood components have limited shelf lives (red blood cells, for example, last around 42 days). Careful inventory management is essential to prevent expiry and wastage.
- Increased Demand: Major accidents, natural disasters, or surges in patient needs due to disease outbreaks all significantly increase demand, sometimes exceeding capacity.
- Transportation and Logistics: Maintaining a cold chain during transportation is critical. A breakdown in the system can render blood unusable, especially in remote areas.
Mitigation strategies involve a multi-pronged approach: Increased public awareness campaigns to encourage donations, efficient inventory management techniques utilizing data analytics (as discussed later), strategic partnerships with blood banks and hospitals, investment in advanced blood storage and transportation technologies, and robust disaster preparedness plans.
Q 23. Explain your experience with blood product traceability and documentation.
Blood product traceability and documentation are paramount for patient safety and regulatory compliance. It’s like a detailed patient record, but for the blood itself. Every unit of blood is assigned a unique identifier, tracked from donation to transfusion. My experience involves meticulous record-keeping, utilizing both electronic and paper-based systems (depending on the facility). This includes detailed information on the donor (health history, blood type, etc.), processing steps, storage conditions, and ultimately, the recipient. We employ software that integrates with hospital information systems (HIS), ensuring seamless data flow and facilitating real-time tracking. This helps us instantly identify the source of any potential issue, should a problem arise.
For example, if a transfusion reaction occurs, we can rapidly trace the blood unit back to the donor and the processing facility, identifying any potential contaminants or discrepancies. This is critical in preventing similar incidents in the future. We strictly adhere to regulatory standards such as ISO 15189 for medical laboratories and the FDA’s guidelines for blood establishments. Our documentation processes are regularly audited to ensure accuracy and compliance.
Q 24. How do you collaborate with other healthcare professionals to ensure efficient blood product management?
Efficient blood product management hinges on excellent collaboration. It’s a team sport, not a solo act. I regularly interact with:
- Physicians: To understand their anticipated needs and ensure the right blood products are available at the right time. This involves forecasting demand based on surgical schedules and patient conditions.
- Nurses: To ensure safe handling, administration, and monitoring of blood transfusions. Close communication is vital for timely feedback and issue resolution.
- Blood Bank Technicians: For coordinating blood collection, testing, and distribution. They are the heart of the operation, and clear communication ensures smooth operations.
- Laboratory Staff: For quality control testing and ensuring the integrity of blood products. Their work is critical to patient safety.
- Supply Chain Managers: To optimize procurement, storage, and transportation, minimizing waste and maximizing efficiency.
We utilize regular meetings, electronic communication platforms, and shared databases to facilitate seamless information sharing and collaborative decision-making. A proactive approach, involving regular forecasting and contingency planning, is essential to minimize disruptions.
Q 25. How do you utilize data analytics to improve blood product inventory management?
Data analytics plays a pivotal role in optimizing blood product inventory management. Think of it as using a powerful microscope to see patterns and trends invisible to the naked eye. We use various techniques:
- Predictive Modeling: Analyzing historical data (donation rates, transfusion patterns, seasonal variations) to forecast future demand. This allows us to proactively adjust inventory levels and avoid shortages.
- Inventory Optimization: Employing algorithms to determine optimal stock levels, minimizing wastage while ensuring adequate supply. We might use software that considers blood type distribution, shelf life, and anticipated demand.
- Demand Forecasting: Using statistical models to predict future demand, considering factors such as surgical schedules, seasonal trends, and local health events.
- Performance Monitoring: Tracking key metrics like blood product utilization rates, expiry rates, and turnaround times to identify areas for improvement.
The insights gained help us to refine our processes, improve resource allocation, and minimize costs while ensuring patient safety. For example, if we identify a consistent oversupply of a specific blood type, we can adjust our donor recruitment strategies.
Q 26. Explain your experience with different inventory management systems (e.g., FIFO, LIFO).
Inventory management systems are crucial for maintaining the quality and availability of blood products. The choice of system depends on various factors such as storage space, product shelf life, and demand patterns. I’ve worked extensively with both FIFO (First-In, First-Out) and LIFO (Last-In, First-Out) methods.
- FIFO (First-In, First-Out): This is the preferred method for blood products due to their limited shelf life. The oldest units are used first, minimizing the risk of expiry. It’s like managing a refrigerator – you consume the oldest items first to prevent spoilage.
- LIFO (Last-In, First-Out): While less common for blood products, LIFO might be used in certain situations, such as for components with longer shelf lives. However, meticulous tracking is crucial to avoid using expired products.
In practice, we implement robust inventory tracking systems that record the date of receipt and expiry of every blood unit, automatically flagging units nearing expiration. We use barcodes and RFID tags for efficient tracking and management, ensuring adherence to the FIFO principle.
Q 27. Describe your experience with quality control testing of blood products.
Quality control testing is non-negotiable for blood products. It’s the cornerstone of patient safety, ensuring that only safe and effective products are used. My experience includes oversight and participation in various quality control procedures:
- Blood Typing and Crossmatching: Accurate determination of blood type and compatibility is crucial to prevent adverse transfusion reactions. Automated systems enhance accuracy and speed.
- Antibody Screening: Identifying the presence of unexpected antibodies in donor blood which could trigger complications in recipients.
- Infectious Disease Testing: Rigorous testing for infections such as HIV, Hepatitis B and C, syphilis, and other relevant pathogens is performed on all donated blood.
- Bacterial Testing: Checking for the presence of bacteria in blood units to prevent infections.
- Sterility Testing: Ensuring the sterility of blood bags and components to avoid contamination.
We maintain strict quality control protocols and follow standardized operating procedures (SOPs), which are regularly reviewed and updated in accordance with the latest guidelines. This includes regular calibration of equipment, ongoing staff training, and participation in external quality assessment programs.
Q 28. How do you manage the budget for blood product acquisition and storage?
Managing the blood product budget involves careful planning and resource allocation. It’s a balancing act between ensuring sufficient supply and responsible fiscal management. We:
- Develop annual budgets: Forecasting anticipated demand and factoring in cost fluctuations for blood products, supplies, equipment maintenance, personnel costs, and storage expenses.
- Negotiate contracts with suppliers: To secure favorable pricing and consistent supply of high-quality blood products.
- Monitor expenditures: Regularly tracking expenses against the budget to identify areas for potential savings or cost overruns.
- Utilize inventory management software: To optimize stock levels, minimize waste, and reduce storage costs.
- Explore cost-effective alternatives: Where appropriate, exploring cost-effective strategies without compromising quality or safety.
We regularly review and analyze our budget to identify inefficiencies and explore opportunities for cost savings, always keeping patient safety as our top priority.
Key Topics to Learn for Blood Product Inventory and Distribution Interview
- Blood Product Types and Characteristics: Understanding the different types of blood products (red blood cells, platelets, plasma, etc.), their storage requirements, shelf life, and compatibility issues is crucial.
- Inventory Management Systems: Learn about various inventory management techniques, including FIFO (First-In, First-Out), and how technology plays a role in tracking, managing, and optimizing blood product inventory levels.
- Distribution Logistics and Chain of Custody: Familiarize yourself with the entire process of blood product distribution, from the blood bank to the hospital, including transportation, temperature control, and maintaining accurate documentation.
- Quality Control and Assurance: Understand the importance of adhering to strict quality control measures throughout the entire process to ensure blood product safety and efficacy. This includes proper handling, storage, and testing procedures.
- Regulatory Compliance: Be prepared to discuss relevant regulations and standards governing blood product inventory and distribution, demonstrating your knowledge of best practices and legal requirements.
- Demand Forecasting and Supply Chain Optimization: Explore methods used to predict blood product demand and strategies for optimizing the supply chain to meet patient needs efficiently and effectively. This might involve analyzing historical data and using predictive modeling techniques.
- Emergency Preparedness and Disaster Response: Understand how blood product inventory and distribution systems are adapted and managed during emergencies or natural disasters, prioritizing patient care under pressure.
- Ethical Considerations and Patient Safety: Discuss the ethical aspects of blood product allocation and distribution, emphasizing the importance of equitable access and patient safety as paramount concerns.
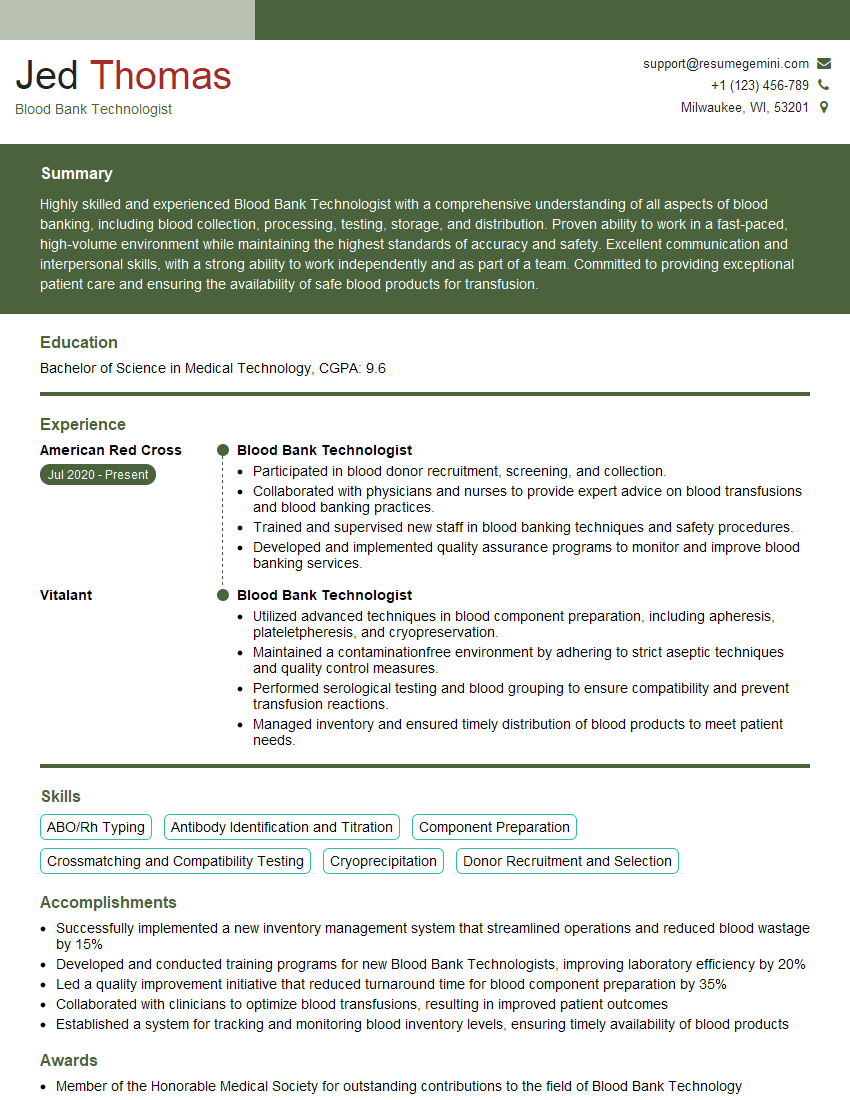
Next Steps
Mastering Blood Product Inventory and Distribution demonstrates critical organizational skills and a commitment to patient care—highly valuable assets in today’s healthcare landscape. This expertise opens doors to rewarding careers with significant growth potential. To maximize your job prospects, it’s essential to present your skills effectively. Creating an ATS-friendly resume is key. ResumeGemini is a trusted resource that can help you build a professional and impactful resume, ensuring your qualifications shine. Examples of resumes tailored to Blood Product Inventory and Distribution are available to help you craft the perfect application.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.