Cracking a skill-specific interview, like one for Bronchodilator Administration, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Bronchodilator Administration Interview
Q 1. What are the different types of bronchodilators?
Bronchodilators are medications that relax and open the airways in the lungs, making breathing easier. They are primarily used to treat conditions like asthma and COPD (Chronic Obstructive Pulmonary Disease). There are two main classes:
- Beta-2 agonists: These stimulate beta-2 receptors in the lungs, causing the muscles around the airways to relax. Examples include albuterol (short-acting) and salmeterol (long-acting).
- Anticholinergics: These block the action of acetylcholine, a neurotransmitter that causes airway constriction. Examples include ipratropium bromide and tiotropium.
Some medications combine both beta-2 agonists and anticholinergics for a synergistic effect, offering broader bronchodilation.
Q 2. Explain the mechanism of action of beta-2 agonists.
Beta-2 agonists work by binding to beta-2 adrenergic receptors located on the smooth muscle cells surrounding the airways. This binding triggers a cascade of intracellular events that ultimately lead to relaxation of the smooth muscle. Imagine it like this: the beta-2 agonist acts like a key, unlocking a door (the receptor) that initiates a process (the cascade) causing the airway muscles to loosen their grip, widening the airways and making it easier to breathe. This is achieved by increasing intracellular cyclic AMP (cAMP), which leads to smooth muscle relaxation.
Q 3. Describe the mechanism of action of anticholinergics.
Anticholinergics work by blocking the action of acetylcholine, a neurotransmitter that causes the muscles in the airways to constrict. Acetylcholine binds to muscarinic receptors in the airways, causing contraction. Anticholinergics, by blocking these receptors, prevent acetylcholine from binding, therefore preventing airway constriction. Think of it as a security guard preventing a key (acetylcholine) from opening a lock (muscarinic receptor) that would otherwise cause the airways to narrow. This leads to relaxation of the airway smooth muscle and improved airflow.
Q 4. What are the common side effects of albuterol?
Albuterol, a common short-acting beta-2 agonist, is generally well-tolerated, but side effects can occur. The most common include:
- Tremors: Often mild and temporary, these are felt most frequently in the hands.
- Nervousness or anxiety: This can range from mild jitters to more significant anxiety.
- Headache: A fairly common side effect.
- Increased heart rate (tachycardia): This is more likely at higher doses.
- Muscle cramps: Less common but possible.
It’s important to note that the severity of side effects varies significantly between patients, and many tolerate albuterol with minimal issues.
Q 5. What are the common side effects of ipratropium bromide?
Ipratropium bromide, an anticholinergic bronchodilator, generally has fewer side effects than beta-2 agonists. Common side effects, though usually mild, can include:
- Dry mouth: A very common side effect.
- Cough: Can be triggered by the dryness of the mouth and throat.
- Headache: Less frequent than with beta-2 agonists.
- Nausea: Relatively uncommon.
- Constipation: Less frequent.
Serious side effects are rare but can include urinary retention, especially in patients with pre-existing urinary problems.
Q 6. How do you assess a patient’s response to bronchodilator therapy?
Assessing a patient’s response to bronchodilator therapy involves a multi-faceted approach. We look at both subjective and objective measures:
- Subjective assessment: This involves asking the patient about their symptoms. Has their shortness of breath improved? Are they coughing less? Do they feel more comfortable breathing?
- Objective assessment: This typically includes measuring lung function using spirometry. We compare pre- and post-bronchodilator measurements (FEV1, for example). A significant increase in FEV1 (usually 12% or more) indicates a good response. We also observe the patient’s respiratory rate, heart rate, and overall clinical status.
It’s crucial to consider the patient’s baseline condition and individual response when evaluating treatment effectiveness. A holistic approach is necessary to ensure optimal patient care.
Q 7. What are the indications for using a short-acting bronchodilator?
Short-acting bronchodilators, like albuterol, are primarily used for the rapid relief of bronchospasm. Their indications include:
- Acute bronchospasm: Sudden wheezing or shortness of breath, often triggered by an allergen, exercise, or infection.
- Pre-exercise use: To prevent exercise-induced bronchoconstriction.
- Rescue medication: For quick symptom relief when needed, as opposed to long-term control.
They’re not intended for daily, long-term use to prevent symptoms; that’s the role of long-acting bronchodilators and other controller medications.
Q 8. What are the indications for using a long-acting bronchodilator?
Long-acting bronchodilators (LABAs) are prescribed for patients with chronic obstructive pulmonary disease (COPD) or asthma who experience persistent symptoms despite using other treatments. They provide long-lasting relief, preventing bronchospasm and improving airflow over several hours. The primary indication is to prevent symptoms and improve lung function in patients with moderate to severe COPD or asthma who require regular bronchodilation. This means they’re for people who have regular wheezing, coughing, or shortness of breath, not just for occasional flare-ups.
- COPD: LABAs are a cornerstone of COPD management, reducing exacerbations and improving quality of life. Think of it like regularly oiling a squeaky hinge – preventing the problem before it becomes severe.
- Asthma: In asthma, LABAs are used in combination with inhaled corticosteroids (ICS) to help prevent asthma attacks in patients with persistent symptoms. They work synergistically, where ICS reduces inflammation and LABAs relax the airways.
It’s crucial to remember that LABAs are not for immediate relief of acute bronchospasm; they are for long-term control of symptoms.
Q 9. Describe the proper technique for using a metered-dose inhaler (MDI).
Using a metered-dose inhaler (MDI) correctly is vital for effective medication delivery. Many patients struggle with proper technique, leading to poor symptom control. Here’s a step-by-step guide:
- Check the inhaler: Ensure it’s properly shaken and primed (if required).
- Attach a spacer (recommended): Spacers improve drug delivery, especially for children and older adults.
- Remove the cap and exhale fully: Completely empty your lungs before inhalation.
- Hold the inhaler correctly: Hold the MDI 1-2 inches from your mouth, or attach it to the spacer if using one.
- Start inhalation: Begin a slow, deep breath.
- Press the inhaler and continue inhaling: Press the inhaler while inhaling and continue breathing in slowly and deeply.
- Hold your breath: Hold your breath for 10 seconds to allow the medication to deposit in the lungs.
- Repeat if necessary: Follow your prescribed dosage instructions; you might need more than one puff.
- Rinse your mouth: After using some MDIs (especially corticosteroids), rinsing the mouth helps prevent oral thrush.
Think of it as a coordinated dance between the press of the inhaler and your breath. Smooth, deep breaths are key to getting the medicine where it needs to be.
Q 10. Describe the proper technique for using a dry powder inhaler (DPI).
Dry powder inhalers (DPIs) deliver medication as a dry powder without the need for a propellant. The technique is generally simpler than with MDIs but still requires proper execution:
- Load the device (if necessary): Some DPIs require loading a capsule or blister before use; follow the manufacturer’s instructions carefully.
- Exhale fully: Empty your lungs completely.
- Bring the inhaler to your mouth: Ensure a tight seal around the mouthpiece.
- Inhale forcefully and deeply: This creates the airflow necessary to release the medication from the device. Don’t be shy; a strong, deep inhalation is crucial.
- Hold your breath: Hold your breath for 5-10 seconds to allow the medication to settle in your lungs.
- Repeat if necessary: Follow your prescribed dosage instructions.
The key difference from MDIs is the forceful inhalation required to release the powder. Imagine blowing out birthday candles; you need that same powerful breath.
Q 11. What are the potential complications of bronchodilator administration?
While generally safe, bronchodilator administration can lead to several complications. These vary depending on the specific medication and the patient’s overall health:
- Tremors: Some bronchodilators, especially beta-agonists, can cause hand tremors, especially at higher doses.
- Tachycardia (rapid heart rate): This is a common side effect of beta-agonists, as they stimulate the heart.
- Headache: This can be a relatively mild side effect.
- Muscle cramps: Some patients experience muscle aches or cramps.
- Insomnia: Some bronchodilators can interfere with sleep.
- Paradoxical bronchospasm: In rare cases, bronchodilators can cause a tightening of the airways, particularly if the inhaler technique is incorrect.
- Increased blood pressure: Especially with some beta-agonists.
These complications are usually dose-related and can be minimized with proper patient education and monitoring.
Q 12. How do you monitor for adverse effects of bronchodilator therapy?
Monitoring for adverse effects involves careful observation and questioning of the patient. It’s crucial to assess:
- Heart rate and rhythm: Regularly check the pulse for any irregularities or significant increases.
- Blood pressure: Monitor blood pressure, especially in patients with hypertension.
- Tremors: Observe for any hand tremors or other involuntary muscle movements.
- Symptoms: Ask the patient about any new or worsening symptoms, such as headaches, muscle cramps, palpitations, or shortness of breath.
- Patient education and feedback: The patient themselves are a primary source of information. Regular checks-ins during treatment are essential to ensure proper use and identify any emerging side-effects.
Regular follow-up appointments and detailed patient history are critical to effective monitoring. It’s a collaborative effort between the healthcare provider and the patient.
Q 13. What is the difference between rescue and maintenance bronchodilators?
The distinction between rescue and maintenance bronchodilators is crucial for effective asthma or COPD management. Think of it like having two different tools for a specific job:
- Rescue bronchodilators: These are used for quick relief of acute symptoms, like sudden wheezing or shortness of breath. They provide rapid, but short-lived, bronchodilation. Examples include short-acting beta-agonists (SABAs) like albuterol. This is like having a fire extinguisher – for immediate emergencies.
- Maintenance bronchodilators: These are used regularly to prevent symptoms and improve lung function over time. They offer long-lasting bronchodilation but do not provide immediate relief. LABAs and long-acting muscarinic antagonists (LAMAs) are examples. This is like routine maintenance – preventing the problem before it starts.
Both are often used together in patients with persistent symptoms; the rescue inhaler is for when symptoms flare up and the maintenance inhaler for day-to-day symptom control.
Q 14. How do you educate a patient on the proper use of their inhaler?
Patient education is paramount for effective bronchodilator therapy. Education should be tailored to the individual’s needs and understanding. Here’s a structured approach:
- Demonstrate the proper technique: Show the patient how to use their inhaler correctly, using a step-by-step approach with a spacer if needed.
- Use visual aids: Diagrams, videos, or even a demonstration doll can significantly enhance comprehension.
- Provide written instructions: Offer clear, concise written instructions that the patient can refer to later.
- Explain the medication’s purpose: Discuss why they are taking the medication and what to expect.
- Address potential side effects: Clearly explain potential side effects and what to do if they occur.
- Encourage questions: Create a safe and comfortable environment where patients can ask questions without feeling embarrassed.
- Schedule follow-up appointments: Regular follow-up appointments are crucial to assess effectiveness, adherence, and address any concerns.
- Assess understanding: Use teach-back methods; ask the patient to explain back to you how they will use the medication and what to expect.
Think of it like teaching someone to ride a bike; you demonstrate, provide guidance, and practice until they feel confident and safe.
Q 15. How do you determine the appropriate dose of a bronchodilator?
Determining the appropriate bronchodilator dose is crucial for effective treatment and minimizing adverse effects. It’s not a one-size-fits-all approach; it depends on several factors including the patient’s age, weight, severity of their respiratory condition (like asthma or COPD), the specific bronchodilator being used, and their overall health status. The prescribing physician will consider these factors and often start with a low dose, gradually increasing it as needed while closely monitoring the patient’s response. For example, a child with mild asthma will receive a much lower dose than an adult with severe COPD. The dose might also be adjusted based on how well the patient is responding – if their symptoms aren’t improving, the doctor might increase the dose, or if they experience side effects, the dose may be decreased or the medication changed.
This process often involves regular monitoring of lung function tests (like peak expiratory flow or spirometry) to assess the effectiveness of the treatment and guide dose adjustments. It’s a collaborative effort between the patient, their caregiver (if applicable), and the healthcare provider, requiring open communication about symptoms and any potential side effects.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the contraindications for bronchodilator use?
Several contraindications exist for bronchodilator use. These are situations where the benefits of using the medication are significantly outweighed by the potential risks. For example, a known hypersensitivity or allergy to a specific bronchodilator is a major contraindication. Patients with severe cardiovascular disease, especially those with tachyarrhythmias (irregular heartbeats), may need to use bronchodilators cautiously, as some can increase heart rate. Similarly, patients with hyperthyroidism (overactive thyroid) or uncontrolled diabetes might also require careful monitoring when using certain bronchodilators due to potential interactions. Certain bronchodilators are also contraindicated during pregnancy and breastfeeding, requiring careful consideration of risks and benefits. It’s absolutely critical to review the patient’s complete medical history and current medications before administering any bronchodilator to avoid potentially dangerous interactions or adverse effects.
Q 17. What is the role of a spacer device in bronchodilator administration?
Spacer devices are invaluable aids in bronchodilator administration, particularly with metered-dose inhalers (MDIs). MDIs deliver medication as a fine mist, but coordinating inhalation with actuation can be challenging, especially for children, the elderly, or individuals with impaired coordination. A spacer acts as a reservoir, catching the medication mist and allowing the patient to inhale it more slowly and completely. This ensures more medication reaches the lungs and less is deposited in the mouth or throat. Think of it like a practice target for the inhaler. The spacer makes it easier to hit the target (lungs) instead of missing completely.
Using a spacer significantly improves drug delivery and reduces the risk of side effects like oral thrush (a fungal infection in the mouth). Different spacers are available, some with face masks for infants and young children. The choice of spacer depends on the patient’s age and ability to use an inhaler.
Q 18. How do you manage a patient experiencing bronchospasm?
Managing a patient experiencing bronchospasm requires prompt and decisive action. Bronchospasm is a sudden constriction of the airways, causing significant breathing difficulty. The first step is to assess the severity of the bronchospasm: how distressed is the patient? Are they wheezing? What is their respiratory rate? Oxygen saturation levels need to be monitored. Immediate treatment usually involves administering a short-acting beta-agonist bronchodilator, such as albuterol via nebulizer or MDI (with a spacer if appropriate), to relax the airway muscles. In severe cases, intravenous bronchodilators may be required. Supplemental oxygen is also crucial to ensure adequate oxygenation. If the bronchospasm is not responding to initial treatment, or if the patient’s condition deteriorates, more advanced interventions may be necessary, such as intravenous corticosteroids or even mechanical ventilation.
Monitoring vital signs (heart rate, respiratory rate, blood pressure, oxygen saturation), continuous ECG monitoring, and close observation for any signs of respiratory distress are essential. The patient’s response to treatment must be carefully assessed, and further interventions should be initiated if needed.
Q 19. What are the nursing considerations for administering bronchodilators?
Nursing considerations for administering bronchodilators are multifaceted and require attention to detail. Before administration, it is critical to verify the patient’s identity, confirm the correct medication and dose, check for any allergies or contraindications, and assess the patient’s respiratory status (e.g., respiratory rate, breath sounds, oxygen saturation). Proper technique in administering the medication is crucial – ensuring the patient uses a spacer correctly with an MDI or appropriately utilizes a nebulizer. After administration, carefully observe the patient for any side effects like tachycardia (rapid heart rate), tremors, nervousness, or increased blood pressure. Document all observations and the patient’s response to the medication. Education is vital; patients need clear instructions on medication use, including the proper technique and potential side effects. Regular follow-up is essential to evaluate treatment effectiveness and make necessary adjustments.
Q 20. How do you document the administration of a bronchodilator?
Accurate documentation of bronchodilator administration is crucial for maintaining a comprehensive medical record and ensuring continuity of care. The documentation should include the date and time of administration, the name and dose of the medication, the route of administration (e.g., MDI, nebulizer, intravenous), the patient’s response to the medication (e.g., improvement in respiratory rate, reduction in wheezing, increase in peak expiratory flow), and any observed side effects. Any additional interventions taken should also be recorded (e.g., oxygen administration, additional medication). It’s helpful to note the patient’s subjective report of their symptoms before and after medication administration. Clear, concise, and accurate documentation is paramount for legal and clinical reasons.
Example entry: 10/26/2024, 14:00: Albuterol 2.5mg via MDI with spacer. Patient reported improved breathing and reduced wheezing 15 minutes post-administration. No side effects noted.
Q 21. What are the different routes of administration for bronchodilators?
Bronchodilators can be administered through several routes, each with its own advantages and disadvantages. The most common routes are:
- Metered-dose inhalers (MDIs): These handheld devices deliver a measured dose of medication as a fine mist. They’re portable and convenient but require good coordination to use effectively.
- Nebulizers: These devices transform liquid medication into a fine mist that the patient inhales via a face mask or mouthpiece. They’re especially useful for patients who have difficulty using MDIs.
- Intravenous (IV) administration: This route is used in emergency situations for severe bronchospasm when rapid relief is needed. IV administration bypasses the lungs and directly enters the bloodstream.
- Oral administration: Some bronchodilators, like theophylline, are available in oral form, although this route generally has a slower onset of action compared to inhaled medications.
The choice of administration route depends on the patient’s specific needs, the severity of their condition, and the type of bronchodilator being used.
Q 22. Discuss the importance of patient education regarding bronchodilators.
Patient education is paramount in ensuring the safe and effective use of bronchodilators. Without proper understanding, patients may not adhere to their treatment plan, leading to poor symptom control and potential exacerbations.
My approach involves explaining the medication’s purpose, how it works (in simple terms, avoiding complex medical jargon), the correct dosage and timing, and potential side effects. I use visual aids like inhaler technique videos and written instructions tailored to the patient’s literacy level. I always encourage patients to ask questions and address any concerns they may have. For example, I might explain that a bronchodilator helps to relax the muscles around the airways, making it easier to breathe, like easing the tension on a kinked garden hose. I would also emphasize the importance of regular use, even when feeling well, to prevent future problems. I always confirm their understanding by having them repeat back the instructions or demonstrate the correct inhaler technique.
Q 23. Describe a situation where you had to troubleshoot a problem with bronchodilator administration.
I once had a patient who was experiencing minimal relief from their albuterol inhaler, despite using it correctly as demonstrated. The first step was to review the patient’s medication history, confirming the prescription was current and correct. I then explored the potential factors contributing to poor response: inadequate dosage, incorrect inhaler technique (despite initial demonstration), concurrent illnesses affecting lung function, or non-compliance with the prescribed regimen.
Through further questioning, I discovered the patient was using their inhaler less frequently than prescribed, fearing side effects. I addressed their concerns by discussing the benefits versus risks, emphasizing that the potential benefits of consistent use outweighed the minimal side effects they had experienced. We also revisited the correct inhaler technique, using a spacer to improve delivery. This improved adherence, combined with correct technique and the reassessment of the treatment plan, led to a significant improvement in the patient’s symptoms.
Q 24. How do you handle a patient who is unable to use their inhaler correctly?
Incorrect inhaler technique is a common issue. My approach is patient-centered and involves demonstration, repetition, and positive reinforcement. I would begin by observing their current technique to identify the areas needing improvement. I then demonstrate the correct technique step-by-step, using a spacer if needed. This often involves a slow, deep breath, holding the breath for a few seconds after inhalation, and proper coordination of actuation and breathing.
I utilize visual aids, such as diagrams or videos, to further enhance their understanding. We practice the technique repeatedly until they achieve proficiency, offering constructive feedback and encouragement throughout the process. For patients with dexterity challenges, I explore alternative delivery methods like a nebulizer or discuss potential assistive devices. If needed, I involve the patient’s family members or caregivers to ensure consistent support at home.
Q 25. What are the common respiratory conditions that benefit from bronchodilator use?
Bronchodilators are beneficial in managing a variety of respiratory conditions characterized by airway narrowing or obstruction. These include:
- Asthma: A chronic inflammatory condition causing airway narrowing and bronchospasm.
- Chronic Obstructive Pulmonary Disease (COPD): An umbrella term encompassing chronic bronchitis and emphysema, characterized by airflow limitation.
- Bronchitis: Inflammation of the bronchial tubes, often resulting in coughing and mucus production.
- Emphysema: A condition where the alveoli (air sacs) in the lungs are damaged, leading to reduced lung elasticity.
- Cystic Fibrosis: A genetic disorder affecting the lungs and other organs, leading to thick mucus build-up.
The choice of bronchodilator and treatment regimen depends on the specific condition, severity, and individual patient factors.
Q 26. Explain the differences between nebulized and inhaled bronchodilators.
Nebulized and inhaled bronchodilators both deliver medication to the airways, but they differ in their delivery method and suitability for various patients.
- Inhaled bronchodilators (MDIs and DPIs) utilize pressurized metered-dose inhalers (MDIs) or dry powder inhalers (DPIs). MDIs deliver medication as a mist, requiring coordination of inhalation and actuation. DPIs deliver medication as a dry powder via inhalation. They are generally portable and convenient but require proper technique for effective delivery.
- Nebulized bronchodilators use a nebulizer machine that converts liquid medication into a fine mist inhaled through a mouthpiece or facemask. Nebulizers are often preferred for patients with severe respiratory distress or those unable to effectively use inhalers. They are less portable than inhalers.
The choice between nebulized and inhaled bronchodilators depends on the patient’s ability to use an inhaler, the severity of their condition, and their overall clinical status.
Q 27. How do you verify a patient’s identity before administering medication?
Patient safety is paramount. I always verify a patient’s identity using at least two identifiers before administering any medication. This typically involves checking the patient’s wristband against their chart, confirming their name and date of birth verbally. In some settings, a bar code scanner is used to electronically confirm the patient’s identity.
This two-identifier system minimizes the risk of medication errors by ensuring that the medication is administered to the correct individual. I meticulously review the medication order to confirm the correct drug, dose, route, and frequency before proceeding.
Q 28. How do you ensure the safety and efficacy of bronchodilator administration?
Ensuring the safety and efficacy of bronchodilator administration involves a multifaceted approach encompassing medication knowledge, correct technique, and careful monitoring.
- Medication Knowledge: I thoroughly review the medication’s properties, potential side effects, interactions, and contraindications.
- Correct Technique: I use the appropriate method for administration based on the patient’s condition and capabilities, confirming proper inhaler technique or ensuring the nebulizer is functioning correctly.
- Monitoring: I carefully monitor the patient’s response to the medication, observing for improvements in respiratory status, such as reduced shortness of breath, wheezing, or improved oxygen saturation levels. I also observe for adverse effects, like increased heart rate or tremors.
- Documentation: I meticulously document the medication administration, including the time, dose, route, response, and any observed side effects.
This meticulous approach contributes to both the safety and effectiveness of treatment, optimizing patient outcomes while minimizing risks.
Key Topics to Learn for Bronchodilator Administration Interview
- Understanding Bronchodilator Mechanisms: Explore the pharmacological actions of various bronchodilators (e.g., beta-agonists, anticholinergics) and their effects on the respiratory system. Consider the differences in onset and duration of action.
- Medication Administration Techniques: Master the proper techniques for administering bronchodilators via different routes (e.g., Metered Dose Inhalers (MDIs), Dry Powder Inhalers (DPIs), nebulizers). Practice explaining the steps clearly and demonstrating your understanding of correct patient education.
- Patient Assessment and Monitoring: Discuss the importance of pre-administration assessments (e.g., respiratory rate, heart rate, lung sounds) and post-administration monitoring to evaluate treatment effectiveness and identify potential adverse effects.
- Adverse Effects and Complications: Be prepared to discuss common side effects of various bronchodilators and how to recognize and manage them. Understand the implications of incorrect administration or patient non-compliance.
- Medication Interactions: Explore potential interactions between bronchodilators and other medications frequently used in respiratory care. Demonstrate an understanding of drug interactions and their management.
- Legal and Ethical Considerations: Review relevant legal and ethical guidelines related to medication administration, including patient confidentiality, informed consent, and medication safety protocols.
- Troubleshooting Common Issues: Be prepared to discuss solutions for common problems encountered during bronchodilator administration, such as difficulty with inhaler technique or medication delivery system malfunctions.
Next Steps
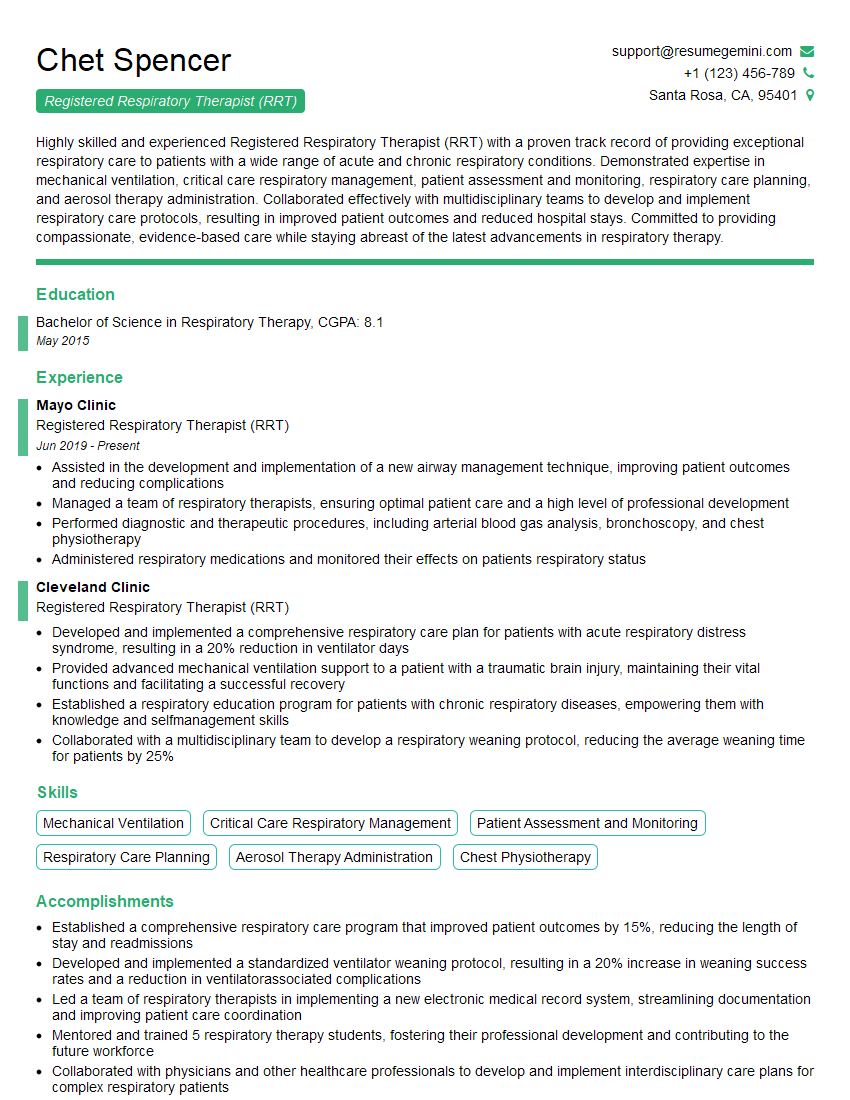
Mastering bronchodilator administration is crucial for advancing your career in respiratory care, demonstrating your competence and commitment to patient well-being. A well-crafted resume is your first impression on potential employers. Make it count! Building an ATS-friendly resume significantly increases your chances of getting noticed. ResumeGemini is a trusted resource that can help you create a compelling and effective resume tailored to your skills and experience. We provide examples of resumes specifically designed for candidates in Bronchodilator Administration to help you get started. Invest time in crafting a professional resume that showcases your expertise – your future career depends on it!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.