Cracking a skill-specific interview, like one for Caregiver Support and Education, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Caregiver Support and Education Interview
Q 1. Describe your experience developing and delivering caregiver training programs.
Developing and delivering caregiver training programs requires a multifaceted approach, blending pedagogical expertise with a deep understanding of caregiving challenges. My experience involves needs assessment, curriculum design, instructional delivery, and evaluation.
For example, I recently developed a program focused on dementia care, incorporating modules on communication strategies, managing challenging behaviors, and maintaining the dignity of the person with dementia. This involved extensive research on best practices and consultation with experienced dementia care professionals. The curriculum included interactive workshops, role-playing scenarios, and practical demonstrations of care techniques. Post-training evaluations consistently showed improved confidence and competence among participants.
Another program I designed addressed the unique needs of family caregivers for individuals with Parkinson’s Disease. This program focused on mobility assistance, medication management, and strategies for coping with emotional and physical demands. We employed a blended learning approach, combining online modules with in-person group sessions to cater to varied learning styles and time constraints.
Q 2. What methods do you use to assess caregiver competency?
Assessing caregiver competency involves a combination of methods to ensure a comprehensive understanding of their skills and knowledge. It’s not just about testing knowledge, but also observing practical application and evaluating their confidence and ability to handle challenging situations.
- Written Exams: These assess knowledge of caregiving techniques, safety procedures, and relevant medical information.
- Practical Demonstrations: Observing caregivers perform tasks such as transferring a patient, administering medication (under supervision), or providing personal care allows for assessment of their skills and adherence to safety protocols.
- Simulated Scenarios: Role-playing exercises or simulated emergency situations help evaluate problem-solving skills and quick decision-making under pressure.
- Performance-Based Assessments: Rating scales and checklists are used to objectively evaluate specific skills and behaviors during practical demonstrations.
- Self-Assessments and Reflective Journals: These provide insight into the caregiver’s self-awareness, strengths, and areas needing improvement.
For instance, to assess competency in medication management, we might use a combination of a written test on medication administration principles, followed by an observation of the caregiver correctly administering medication to a simulated patient, using a standardized checklist to track their performance.
Q 3. How do you address caregiver burnout and stress?
Caregiver burnout and stress are significant concerns that require proactive and comprehensive strategies. Addressing these issues is crucial for both the caregiver’s well-being and the quality of care provided.
- Education and Awareness: Educating caregivers about the signs and symptoms of burnout, stress management techniques, and available support services is essential.
- Support Groups: Providing opportunities for caregivers to connect with peers who share similar experiences fosters a sense of community and reduces feelings of isolation.
- Stress Management Techniques: Teaching relaxation techniques such as deep breathing, mindfulness, and yoga can help caregivers manage stress levels effectively.
- Respite Care: Arranging temporary relief for caregivers allows them to take breaks, recharge, and prevent burnout.
- Access to Professional Counseling: Connecting caregivers with mental health professionals can provide individualized support and coping strategies.
For example, we might incorporate a module on stress management techniques into our training program, including practical exercises and a referral list of local support services. We also organize regular support group meetings for caregivers to share their experiences and provide mutual support.
Q 4. Explain your approach to conflict resolution between caregivers and care recipients.
Conflict resolution between caregivers and care recipients requires a patient, empathetic, and structured approach. The goal is to foster understanding and find mutually agreeable solutions.
- Active Listening: Encouraging both parties to express their perspectives without interruption is essential.
- Empathy and Validation: Showing empathy and validating both the caregiver’s and care recipient’s feelings helps to de-escalate the situation.
- Identifying Underlying Issues: Determining the root cause of the conflict is crucial for finding effective solutions. This might involve communication difficulties, unmet needs, or differing expectations.
- Mediation and Negotiation: Facilitating communication and helping both parties negotiate a compromise is vital. This may involve creating a personalized care plan that incorporates the preferences of both individuals.
- Setting Clear Boundaries: Helping establish clear and respectful boundaries between the caregiver and care recipient is crucial for maintaining a healthy relationship.
For example, if a conflict arises between a caregiver and a care recipient regarding medication, I would facilitate a discussion to understand the care recipient’s concerns and anxieties. We would explore alternative medication administration methods that consider the recipient’s preferences while ensuring medication adherence.
Q 5. How do you adapt training materials for diverse learner needs?
Adapting training materials for diverse learner needs is critical for ensuring effective knowledge transfer and skill acquisition. This requires considering various learning styles, literacy levels, cultural backgrounds, and physical limitations.
- Multimodal Learning: Incorporating various learning modalities, including visual aids, hands-on activities, auditory presentations, and written materials, caters to diverse learning styles.
- Accessibility Considerations: Ensuring materials are accessible to individuals with disabilities, such as providing large-print versions, audio recordings, or sign language interpretation.
- Cultural Sensitivity: Using culturally appropriate language, imagery, and examples that resonate with the participants’ backgrounds.
- Differentiated Instruction: Offering varied activities and assignments tailored to individual learning needs and paces.
- Technology Integration: Utilizing technology such as online modules, interactive simulations, and mobile applications to enhance engagement and accessibility.
For instance, for a group with varying literacy levels, I might provide both written materials and audio recordings of the same content. I would also incorporate hands-on activities and visual aids to enhance understanding, ensuring all learners are engaged and can grasp the information effectively.
Q 6. Describe your experience with different caregiving models (e.g., person-centered care).
My experience encompasses various caregiving models, with a strong emphasis on person-centered care. This model prioritizes the individual’s preferences, choices, and autonomy, placing the care recipient at the center of the care planning process.
Person-Centered Care focuses on understanding the individual’s unique needs, values, and aspirations. It involves active listening, respecting their choices, and collaborating with them to create a personalized care plan. This contrasts with more traditional models that might prioritize efficiency or standardized procedures over individual preferences.
Other models I’ve worked with include family-centered care (involving the family in the care planning process), and team-based care (coordinating services from various professionals). Understanding these models and their nuances is crucial for adapting training programs to suit specific caregiving contexts and promoting holistic, effective care.
For example, in a training session on person-centered care, we might use case studies to illustrate how to tailor care plans to individual preferences and involve care recipients in decision-making processes.
Q 7. How do you ensure the safety and well-being of both the caregiver and care recipient?
Ensuring the safety and well-being of both the caregiver and care recipient is paramount. This necessitates a proactive and multi-pronged approach.
- Safety Training: Providing comprehensive training on safe patient handling techniques, medication administration, infection control, and emergency procedures.
- Risk Assessment: Conducting regular risk assessments to identify potential hazards in the care environment and develop strategies for mitigation.
- Ergonomic Practices: Educating caregivers on proper body mechanics and the use of assistive devices to prevent injuries.
- Mental Health Support: Providing access to mental health services for caregivers to address stress, anxiety, and burnout, which can impact safety.
- Communication and Collaboration: Fostering open communication and collaboration between caregivers, care recipients, and healthcare professionals to address concerns and prevent potential problems.
For instance, we might incorporate a practical demonstration on safe patient transfer techniques into our training program, emphasizing the importance of proper body mechanics and the use of assistive devices to prevent injuries. We would also discuss strategies for recognizing and responding to early signs of caregiver burnout, emphasizing the importance of seeking support to avoid potential safety compromises.
Q 8. What are some common challenges faced by caregivers, and how do you help them overcome them?
Caregiving is incredibly demanding, both emotionally and physically. Common challenges include:
- Physical Strain: Lifting, transferring, and providing personal care can lead to injuries.
- Emotional Toll: Witnessing a loved one’s decline, dealing with challenging behaviors, and experiencing isolation are significant stressors.
- Financial Burden: Medical expenses, lost wages, and the cost of caregiving supplies can create financial hardship.
- Lack of Time for Self-Care: Caregivers often neglect their own physical and mental health, leading to burnout.
- Social Isolation: Reduced social interaction and limited opportunities for respite can lead to feelings of loneliness and depression.
To help caregivers overcome these challenges, we employ a multi-pronged approach. This includes:
- Education: Providing training on safe patient handling techniques, managing challenging behaviors, and accessing available resources.
- Support Groups: Connecting caregivers with others facing similar challenges, fostering a sense of community and shared experience.
- Respite Care: Offering temporary relief to allow caregivers time for themselves, preventing burnout.
- Individualized Counseling: Providing emotional support and coping strategies to address stress and anxiety.
- Financial Assistance: Connecting caregivers with resources for financial aid, such as government programs or charitable organizations.
For example, we recently helped a caregiver who was struggling with the physical demands of caring for her elderly mother. Through our safe patient handling training, we taught her techniques to minimize strain on her back, preventing future injuries. We also connected her to a respite care program, allowing her to take much-needed breaks and recharge.
Q 9. What resources do you utilize to support caregivers?
Our caregiver support utilizes a wide range of resources to ensure comprehensive assistance. These include:
- Government Agencies: We collaborate with agencies like Medicaid and Medicare to connect caregivers with financial and healthcare resources.
- Non-profit Organizations: We partner with local and national charities that provide financial assistance, respite care, and caregiver support programs.
- Medical Professionals: We work closely with physicians, nurses, and therapists to ensure caregivers receive accurate medical information and support.
- Educational Institutions: We utilize resources from universities and colleges to develop evidence-based training materials and educational programs.
- Online Resources: We leverage credible online databases and websites to provide caregivers with up-to-date information on caregiving strategies, legal issues, and support services.
These resources allow us to offer a tailored approach to caregiver support, addressing the specific needs of each individual. For instance, if a caregiver is struggling financially, we connect them with relevant government assistance programs and non-profit organizations offering financial aid.
Q 10. How do you evaluate the effectiveness of your caregiver support and education initiatives?
We employ a multifaceted approach to evaluate the effectiveness of our caregiver support initiatives. This includes:
- Pre- and Post-Training Assessments: We measure improvements in caregiver knowledge, skills, and confidence levels through questionnaires and practical demonstrations.
- Caregiver Satisfaction Surveys: We regularly solicit feedback through surveys to assess satisfaction with our services and identify areas for improvement.
- Qualitative Feedback: We gather feedback through focus groups and individual interviews to gain deeper insights into caregiver experiences and challenges.
- Outcome Measures: We track key indicators such as caregiver burnout rates, patient health outcomes, and hospital readmissions to assess the overall impact of our interventions.
- Data Analysis: We use statistical analysis to identify trends and patterns in caregiver outcomes and service utilization to inform future program development.
For example, if our post-training assessments reveal a lack of improvement in a specific area, we revise our training materials and delivery methods to better address the identified gap.
Q 11. Explain your knowledge of relevant regulations and compliance standards for caregiver training.
My knowledge of relevant regulations and compliance standards is extensive. I am familiar with:
- HIPAA (Health Insurance Portability and Accountability Act): Understanding and adhering to patient privacy regulations is paramount in caregiver training.
- State and Federal Laws Governing Healthcare Providers: Compliance with relevant licensing and certification requirements for caregivers and training programs is crucial.
- OSHA (Occupational Safety and Health Administration) Standards: We ensure caregiver training includes safe patient handling techniques and infection control measures to protect both caregivers and patients.
- Regulations Regarding Background Checks and Criminal History Screening: Thorough background checks are essential for caregiver employment and safety.
- Continuing Education Requirements: We stay informed about ongoing changes in regulations and ensure our training programs reflect the latest best practices and standards.
For instance, we meticulously document all training activities and ensure all materials align with HIPAA guidelines, protecting sensitive patient information. This ensures not only compliance but also builds trust and confidence among both caregivers and patients.
Q 12. Describe your experience with developing and implementing care plans.
I have extensive experience in developing and implementing care plans. My approach involves:
- Needs Assessment: A thorough assessment of the patient’s physical, cognitive, emotional, and social needs, involving the patient, family, and healthcare team.
- Goal Setting: Establishing clear, measurable, achievable, relevant, and time-bound (SMART) goals that address the patient’s needs and improve their quality of life.
- Intervention Strategies: Identifying specific interventions to achieve the goals, considering evidence-based practices and patient preferences. This includes medication management, physical therapy, occupational therapy, and social activities.
- Caregiver Training: Educating the caregiver on how to implement the care plan effectively, emphasizing safety, communication, and emotional support.
- Ongoing Monitoring and Evaluation: Regularly reviewing the care plan’s effectiveness and making adjustments as needed based on the patient’s progress and changing needs.
For example, I worked with a patient with Parkinson’s disease, developing a care plan that focused on improving mobility, managing medication side effects, and providing emotional support to both the patient and their family. We tailored the plan’s execution based on regular feedback and ongoing assessment.
Q 13. How do you incorporate technology into caregiver support and education?
Technology plays a vital role in enhancing caregiver support and education. We utilize:
- Online Learning Platforms: Providing convenient and accessible training materials through online modules, videos, and interactive exercises.
- Telehealth: Offering remote consultations with healthcare professionals, providing timely support and reducing the need for in-person visits.
- Mobile Apps: Utilizing apps that provide medication reminders, symptom tracking, and communication tools for caregivers and healthcare professionals.
- Wearable Sensors: Employing wearable technology to monitor patient vital signs and activity levels, providing real-time data for improved care management.
- Virtual Reality (VR) Simulations: Creating immersive training experiences that allow caregivers to practice skills in a safe and controlled environment.
For example, we’ve integrated a telehealth platform allowing remote consultations with nurses specializing in dementia care, providing caregivers with on-demand support and reducing feelings of isolation.
Q 14. What is your experience with different types of dementia and how do you adapt caregiving strategies accordingly?
My experience encompasses various dementia types, including Alzheimer’s disease, vascular dementia, Lewy body dementia, and frontotemporal dementia. Each type presents unique challenges, requiring tailored caregiving strategies. For example:
- Alzheimer’s Disease: Focuses on memory support, creating a structured and predictable environment, and managing behavioral changes with patience and understanding.
- Vascular Dementia: May involve managing physical limitations resulting from strokes and other vascular events, along with cognitive impairments.
- Lewy Body Dementia: Requires careful attention to fluctuations in cognitive function and potential sensitivity to certain medications. Visual hallucinations are also a common challenge.
- Frontotemporal Dementia: Often presents with behavioral and personality changes, requiring strategies to manage challenging behaviors and maintain a safe environment.
Adapting caregiving strategies involves understanding the specific cognitive and behavioral manifestations of each dementia type. We train caregivers to recognize early warning signs, adapt communication techniques, and utilize environmental modifications to improve the patient’s safety and quality of life. For instance, a caregiver caring for someone with Lewy body dementia might learn to create a calming environment, minimizing visual stimulation that could trigger hallucinations.
Q 15. How do you communicate effectively with families and care recipients?
Effective communication with families and care recipients hinges on active listening, empathy, and clear, concise language. I tailor my communication style to each individual’s needs and preferences, recognizing that some may prefer direct, factual information while others require more emotional support.
For example, when discussing a care plan with a family, I start by actively listening to their concerns and priorities. I then explain the plan in simple terms, avoiding medical jargon. I use visual aids like diagrams or flowcharts where appropriate to enhance understanding. For care recipients, I use person-centered language, ensuring they feel respected and involved in the decision-making process. Regular check-ins and open-ended questions help maintain open communication channels.
I also utilize various communication methods, including face-to-face meetings, phone calls, emails, and even video conferencing, depending on the situation and the individuals’ preferences. Documentation is crucial; I maintain detailed records of all communications to ensure consistency and accountability.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience with end-of-life care and support for grieving families.
My experience with end-of-life care emphasizes providing compassionate support to both the care recipient and their family. This includes facilitating open communication about wishes regarding end-of-life care, helping families navigate the emotional and practical challenges of this period, and connecting them with relevant resources such as hospice care and grief counseling.
I’ve worked with several families facing this difficult journey, helping them understand the dying process, offering practical support with paperwork and administrative tasks, and providing emotional support during the grieving process. One memorable instance involved supporting a family whose matriarch was receiving hospice care. We worked together to ensure she was comfortable and surrounded by loved ones. After her passing, I facilitated bereavement support groups, connecting the family with resources and other grieving individuals, providing them a safe space to share their emotions and experiences. It’s crucial to recognize that grief is individual and requires a personalized approach, allowing families to grieve in their own way and at their own pace.
Q 17. How do you promote teamwork and collaboration among caregivers?
Promoting teamwork and collaboration among caregivers is paramount to providing high-quality care. This involves establishing clear roles and responsibilities, ensuring open communication channels, and fostering a culture of mutual respect and trust. I facilitate regular team meetings where caregivers can share updates, discuss challenges, and brainstorm solutions collaboratively.
I utilize tools like shared calendars and communication platforms to streamline information sharing and coordination of care. Conflict resolution skills are essential; I mediate disagreements fairly and help caregivers find common ground. Regular training and professional development opportunities help build team cohesion and enhance individual skills. I often use a team-based approach, emphasizing that we’re all working towards a common goal: the well-being of the care recipient. Building a strong team dynamic allows us to address the complex needs of care recipients more effectively and efficiently.
Q 18. Describe a time you had to deal with a challenging caregiver situation. How did you handle it?
One challenging situation involved a family caregiver who was experiencing burnout due to the overwhelming demands of caring for a loved one with Alzheimer’s disease. The caregiver was exhibiting signs of stress, neglecting their own self-care, and becoming increasingly frustrated.
My approach involved a multi-pronged strategy. First, I actively listened to their concerns and validated their feelings. I then helped them identify specific stressors and develop strategies to manage them. This involved connecting them with respite care services, educating them about community resources, and helping them establish a realistic care plan that incorporated realistic breaks and self-care routines. We also explored stress management techniques like mindfulness and meditation. Throughout this process, I maintained open communication, offering ongoing support and encouragement. The caregiver’s well-being is inextricably linked to the quality of care the recipient receives; addressing caregiver burnout is crucial for both.
Q 19. What are your strategies for managing time effectively in a demanding caregiving environment?
Effective time management in the demanding caregiving environment relies on prioritization, planning, and delegation. I utilize tools like daily planners and scheduling apps to organize tasks and appointments. I prioritize tasks based on urgency and importance, focusing on those that directly impact the care recipient’s well-being. I break down large tasks into smaller, manageable steps to avoid feeling overwhelmed.
When possible, I delegate tasks appropriately, enlisting the help of family members, volunteers, or other caregivers. I also set realistic expectations, recognizing that not everything can be accomplished in a day. Scheduling regular breaks and self-care activities is crucial for preventing burnout and maintaining long-term sustainability. Time management isn’t just about efficiency; it’s about ensuring a balanced approach that safeguards the well-being of both the caregiver and the care recipient. Setting boundaries is equally important.
Q 20. How do you maintain confidentiality and protect the privacy of clients and their families?
Maintaining confidentiality and protecting the privacy of clients and their families is a cornerstone of my professional ethics. I adhere strictly to all relevant privacy regulations and organizational policies. This involves securing client records, limiting access to sensitive information to authorized personnel only, and using secure communication methods.
I never discuss client information with unauthorized individuals, even family members unless explicitly authorized by the client. I use coded identifiers when discussing clients in group settings, and I ensure all electronic records are password-protected and stored securely. Transparency and clear communication with clients about how their information is being used and protected are vital. I regularly review and update my understanding of privacy laws and regulations to ensure best practices are followed consistently.
Q 21. How do you stay current with best practices in caregiver support and education?
Staying current with best practices in caregiver support and education is an ongoing commitment. I regularly participate in professional development activities, such as attending conferences, workshops, and webinars. I subscribe to relevant journals and professional organizations’ publications.
I actively engage in online learning platforms and professional networks to stay informed about the latest research, evidence-based practices, and emerging trends in the field. Networking with colleagues and experts is vital for sharing knowledge and best practices. I also actively seek feedback from clients and families to refine my approach and ensure I am meeting their needs effectively. Continuous learning and adaptation are essential in this dynamic field to provide the highest quality of care and support.
Q 22. What are your professional development goals related to caregiver support and education?
My professional development goals center around enhancing my expertise in trauma-informed caregiving and expanding my skills in utilizing technology for caregiver support. I aim to become certified in a specific trauma-informed caregiving methodology, such as the Sanctuary Model, to better support caregivers dealing with the emotional and psychological impact of caregiving. Concurrently, I want to improve my proficiency in using telehealth platforms and digital tools to reach a wider audience and provide more accessible resources. This includes developing online modules and webinars to complement in-person training, creating a user-friendly online support forum, and learning to analyze data collected through these digital platforms to further refine our support services. Ultimately, my goal is to create a more comprehensive and effective support system for caregivers, leveraging both traditional and modern approaches.
Q 23. Describe your experience with documentation and record-keeping for caregiver support programs.
Documentation and record-keeping are crucial for maintaining the integrity and accountability of caregiver support programs. My experience involves utilizing electronic health records (EHRs) and custom-designed databases to track caregiver participation in programs, progress notes, and outcome measures. This includes documenting initial assessments, identifying caregiver needs, tracking attendance at workshops and support groups, and recording any significant events or changes in the care recipient’s condition. We meticulously document all communication with caregivers, including phone calls, emails, and in-person meetings, ensuring comprehensive and accurate records. For example, we use a standardized system to track a caregiver’s stress levels, coping mechanisms, and access to resources. This rigorous documentation process ensures continuity of care, facilitates collaboration with other professionals, and provides vital data for program evaluation and improvement. We strictly adhere to HIPAA regulations to protect caregiver privacy and confidentiality.
Q 24. How do you handle difficult conversations with caregivers or family members?
Difficult conversations require empathy, active listening, and a structured approach. I begin by creating a safe and comfortable environment where the caregiver feels heard and respected. I use active listening techniques, such as reflecting back what I hear to ensure understanding and build rapport. For example, if a caregiver expresses frustration about a lack of support, I acknowledge their feelings (“I understand this is incredibly challenging, and it’s perfectly reasonable to feel frustrated”). Then, I collaboratively explore the root cause of the problem, seeking to find solutions together. If the conversation involves conflict, I facilitate a calm and respectful dialogue, focusing on finding common ground and solutions rather than placing blame. Sometimes, it’s necessary to involve other members of the interdisciplinary team, such as a social worker or therapist, for additional support. My primary goal is to find a mutually acceptable outcome that supports the caregiver and their loved one.
Q 25. What is your understanding of different learning styles and how do you adapt your teaching accordingly?
Understanding different learning styles is fundamental to effective teaching. I recognize that learners process information differently; some are visual learners, others auditory, and some kinesthetic. My approach incorporates various teaching methods to cater to these diverse learning styles. For visual learners, I utilize presentations with clear visuals, diagrams, and handouts. For auditory learners, I incorporate group discussions, lectures, and audio recordings. Kinesthetic learners benefit from hands-on activities, role-playing, and demonstrations. For instance, when teaching about medication management, I might provide a handout with clear instructions (visual), give a verbal explanation (auditory), and have the caregivers practice using a medication organizer (kinesthetic). Regularly assessing learning preferences through informal observation and feedback enables me to adjust my approach and ensure everyone can grasp the material effectively.
Q 26. Explain your approach to mentoring and coaching caregivers.
My approach to mentoring and coaching caregivers emphasizes building a supportive and trusting relationship. I start by actively listening to the caregiver’s concerns and goals. Then, I collaboratively develop a personalized plan that addresses their specific needs and challenges. This plan might involve identifying specific skill-building opportunities, connecting the caregiver with community resources, or providing emotional support. Regular check-ins and constructive feedback are essential components of the mentoring process. I use reflective questioning techniques to encourage self-reflection and problem-solving. For example, instead of offering direct solutions, I might ask questions like, “What strategies have you already tried?” or “What are some potential obstacles you anticipate?” This approach empowers caregivers to take ownership of their learning and development, fostering long-term success and resilience. I also create opportunities for peer-to-peer support and mentorship, as sharing experiences can be incredibly powerful.
Q 27. How do you promote self-care among caregivers?
Promoting self-care is a critical aspect of caregiver support. I emphasize the importance of self-care as a necessary component for maintaining physical and mental well-being. This involves integrating practical strategies into our programs. We offer workshops on stress management techniques, such as mindfulness meditation and deep breathing exercises. We also encourage caregivers to engage in activities they enjoy, emphasizing the importance of setting aside time for personal pursuits and hobbies. Furthermore, I connect caregivers with community resources that offer respite care and support services, allowing them to take breaks from their caregiving responsibilities. Finally, we normalize the challenges of caregiving and create a sense of community where caregivers can openly share their experiences and learn from each other. The message is clear: prioritizing self-care is not selfish; it’s essential for sustaining their well-being and their ability to provide effective care.
Q 28. Describe your experience working with interdisciplinary teams to support caregivers.
Working with interdisciplinary teams is paramount in comprehensive caregiver support. My experience includes collaborating with physicians, nurses, social workers, therapists, and other healthcare professionals to develop coordinated care plans. Effective communication and shared decision-making are central to this collaborative approach. We utilize regular team meetings to discuss individual caregiver cases, share updates, and address any concerns. For instance, if a caregiver is struggling with managing their loved one’s medication, we may involve a pharmacist to provide specialized training and support. A shared electronic health record system ensures efficient information sharing and promotes seamless communication among team members. This collaborative model ensures that caregivers receive holistic support, addressing both their practical and emotional needs, ultimately leading to better outcomes for both the caregiver and the care recipient. This coordination minimizes redundancies and ensures comprehensive support.
Key Topics to Learn for Caregiver Support and Education Interview
- Understanding Caregiver Needs: Explore the diverse emotional, physical, and social needs of caregivers, including stress management, burnout prevention, and coping mechanisms.
- Effective Communication Strategies: Practice active listening, empathy, and clear communication techniques to build rapport and trust with caregivers. Consider role-playing scenarios to hone these skills.
- Resource Navigation & Referral: Familiarize yourself with available community resources, support groups, and relevant government programs. Practice identifying appropriate resources based on specific caregiver needs and situations.
- Educational Program Development & Delivery: Understand the principles of adult learning and develop strategies for creating engaging and effective educational materials and workshops tailored to caregivers. Consider different learning styles and accessibility needs.
- Legal & Ethical Considerations: Become familiar with relevant laws and regulations pertaining to privacy, confidentiality, and caregiver rights. Understand ethical dilemmas and decision-making processes in caregiving contexts.
- Assessment & Evaluation: Learn methods for assessing caregiver needs, evaluating the effectiveness of support programs, and measuring program outcomes. This might include quantitative and qualitative data analysis techniques.
- Collaboration & Teamwork: Understand the importance of collaborating with interdisciplinary teams, including healthcare professionals, social workers, and other support staff. Discuss your experience working effectively in team settings.
Next Steps
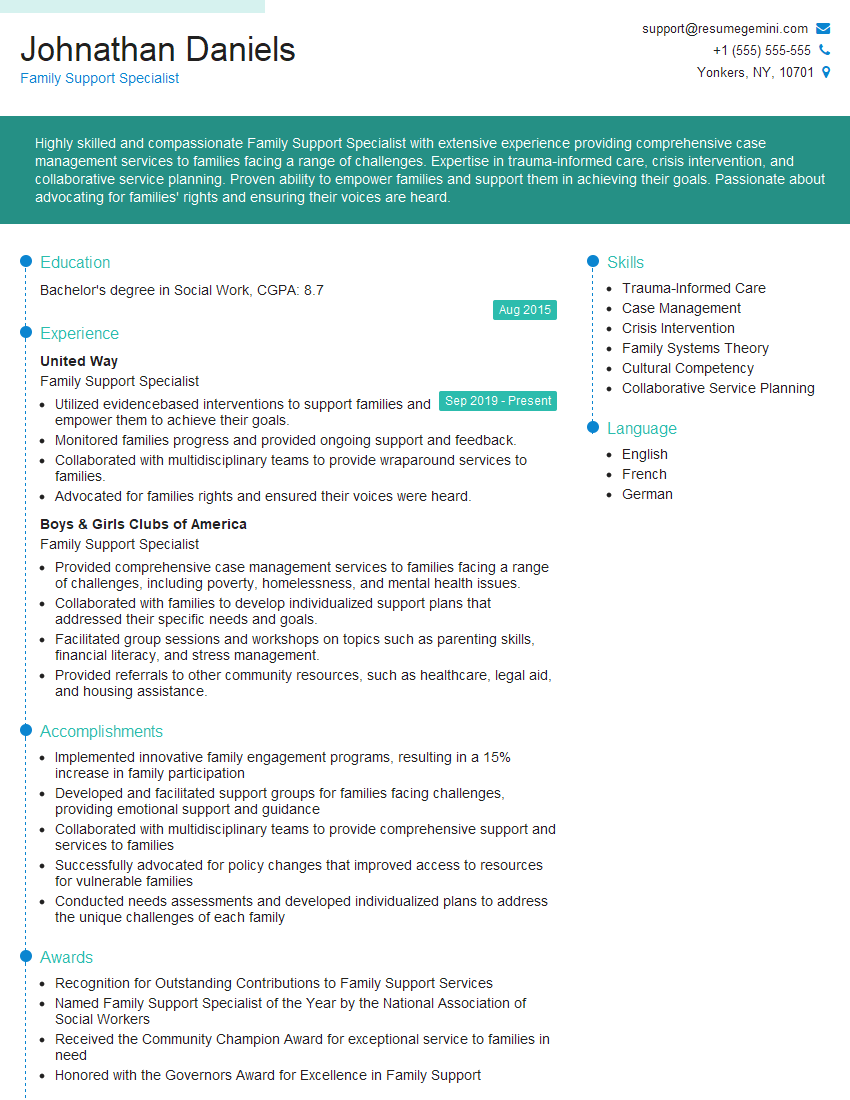
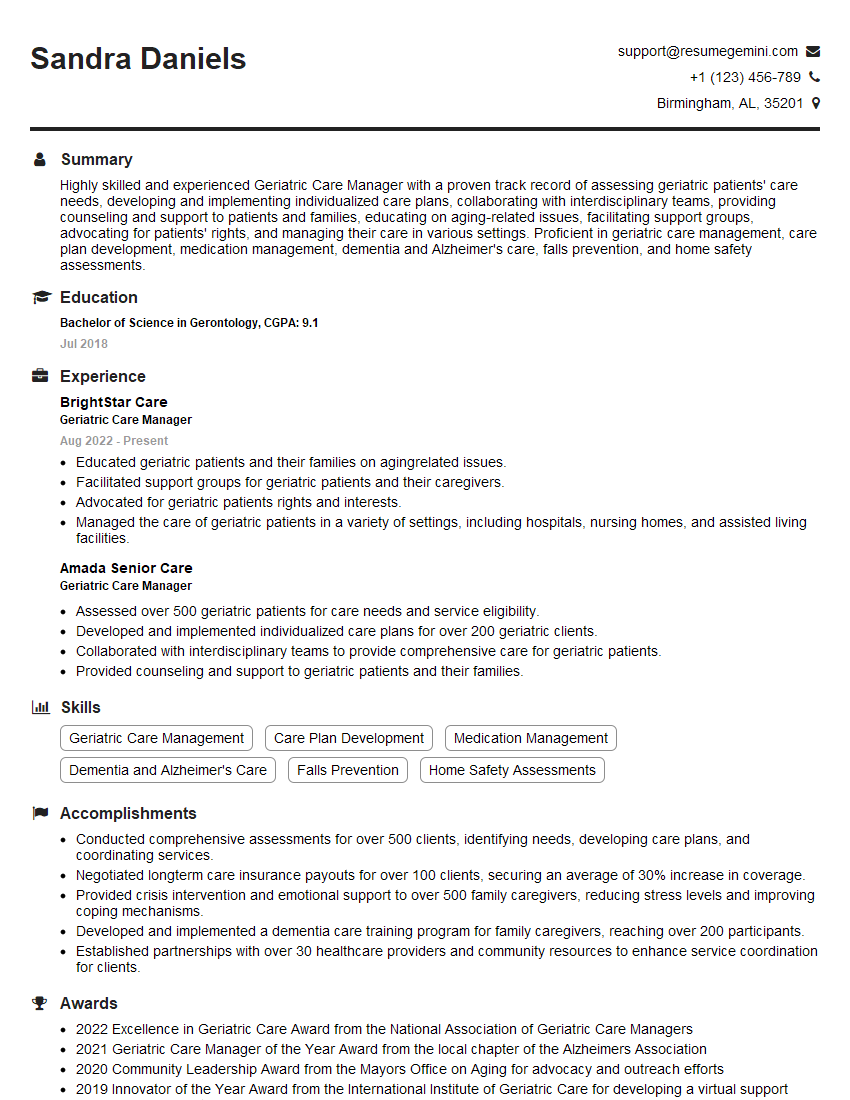
Mastering Caregiver Support and Education opens doors to rewarding careers with significant impact. To maximize your job prospects, create an ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource to help you build a professional and impactful resume, ensuring your application stands out. We provide examples of resumes tailored to Caregiver Support and Education to guide you through the process. Investing time in crafting a strong resume is a crucial step toward securing your dream role.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.