Are you ready to stand out in your next interview? Understanding and preparing for Case Management and Coordination interview questions is a game-changer. In this blog, we’ve compiled key questions and expert advice to help you showcase your skills with confidence and precision. Let’s get started on your journey to acing the interview.
Questions Asked in Case Management and Coordination Interview
Q 1. Describe your experience developing and implementing case management plans.
Developing and implementing case management plans involves a structured approach that ensures client needs are met efficiently and effectively. It begins with a thorough assessment of the client’s situation, identifying their goals, challenges, and available resources. This assessment informs the creation of a personalized plan outlining specific objectives, interventions, timelines, and responsible parties.
For example, in a case involving a young adult struggling with homelessness and substance abuse, the plan might include securing temporary housing, connecting them with addiction treatment services, enrolling them in job training programs, and establishing regular check-ins to monitor progress. The plan is then implemented, with regular monitoring and adjustments made based on the client’s responses and changing circumstances. I’ve successfully used this methodology in various scenarios, from supporting individuals with disabilities to managing complex family cases involving child welfare concerns. My plans always emphasize client autonomy and collaboration, ensuring they are active participants in the process.
Q 2. Explain your process for prioritizing cases with competing needs.
Prioritizing cases with competing needs requires a systematic approach that balances urgency, risk, and resource availability. I typically employ a prioritization matrix, considering factors such as the client’s risk level (e.g., imminent danger, potential for harm), the severity of their needs, and the availability of resources to address those needs.
For instance, a client experiencing a mental health crisis requiring immediate intervention would take precedence over a client needing long-term support services that can be scheduled later. I use a combination of risk assessment tools and clinical judgment to guide this process, ensuring that the most vulnerable clients receive timely attention. Transparency and communication with clients are paramount throughout this process.
Q 3. How do you handle conflicting priorities and competing demands on your time?
Conflicting priorities and competing demands are inherent in case management. To handle these effectively, I rely on robust time management techniques such as prioritizing tasks, scheduling appointments efficiently, and delegating when appropriate. I also establish clear boundaries and communicate expectations with stakeholders. For instance, I might use time blocking to dedicate specific periods to high-priority tasks and buffer time to address unexpected issues.
Furthermore, I utilize project management tools to track progress, identify potential bottlenecks, and allocate resources optimally. Open communication is key: proactive updates to clients and stakeholders keep everyone informed and minimize misunderstandings regarding expectations and timelines. Regular self-reflection and adjustment of my approach ensures that I maintain a sustainable workflow and manage my workload effectively.
Q 4. What methods do you use to track client progress and outcomes?
Tracking client progress and outcomes is crucial for evaluating the effectiveness of the case management plan and making necessary adjustments. I use a combination of methods, including regular client meetings, data collection through standardized assessments, and maintaining detailed case notes.
Specifically, I might employ outcome measurement tools to quantify progress toward specific goals, such as reduction in substance use or improvement in mental health symptoms. These data are documented meticulously, and trends are analyzed regularly to inform adjustments to the case management plan. Visual aids, such as graphs and charts, can help illustrate progress over time, enhancing client engagement and understanding. Furthermore, client feedback is actively solicited and incorporated into the evaluation process.
Q 5. How do you ensure adherence to legal and ethical guidelines in case management?
Adherence to legal and ethical guidelines is paramount in case management. I prioritize confidentiality, ensuring all client information is handled in accordance with relevant privacy laws and regulations (such as HIPAA). I am well-versed in the ethical principles governing the profession, including informed consent, client autonomy, and non-maleficence.
For example, before disclosing any information about a client, I obtain their consent unless legally mandated to do so. I continually engage in professional development to stay updated on evolving regulations and best practices. Ethical dilemmas are approached thoughtfully, considering the potential consequences of different actions and seeking guidance from supervisors or ethics committees when needed.
Q 6. Describe your experience with different case management software or systems.
My experience with case management software and systems includes proficiency with several platforms, including [mention specific software used, e.g., Salesforce Health Cloud, CaseWare, etc.]. I am comfortable navigating different interfaces, inputting and retrieving data, generating reports, and utilizing various features to support efficient case management.
I understand the importance of choosing the right system based on the specific needs of the organization and the clients served. For example, a system with robust reporting capabilities might be crucial for demonstrating program effectiveness to funders, while a system with integrated communication tools can enhance collaboration among team members. I am adept at learning new systems and adapting my approach to different technological environments.
Q 7. Explain how you maintain accurate and up-to-date client records.
Maintaining accurate and up-to-date client records is crucial for effective case management and legal compliance. I utilize a combination of strategies to ensure data accuracy, including double-checking entries, verifying information from multiple sources, and regularly reviewing records for completeness.
Electronic health records (EHR) systems provide a centralized location for storing and managing client information. I follow standardized documentation protocols to maintain consistency and clarity, employing clear and concise language. Regular data backups and security measures are employed to protect client confidentiality and prevent data loss. In addition to electronic records, I utilize secure physical storage for sensitive documents when necessary.
Q 8. How do you communicate effectively with clients, families, and other healthcare professionals?
Effective communication is the cornerstone of successful case management. I tailor my approach to each individual, considering their communication style, cultural background, and cognitive abilities. With clients and families, I prioritize active listening, empathy, and clear, concise language, avoiding medical jargon whenever possible. I use plain language and visual aids when necessary to ensure understanding. I always confirm comprehension through reflective listening and open-ended questions like, “Can you tell me in your own words what we discussed?”
When communicating with other healthcare professionals, I use a more technical language appropriate for the setting. I employ a collaborative approach, sharing information clearly and concisely, utilizing tools like standardized care plans or secure electronic medical records to ensure consistency and efficiency. For example, if a client is experiencing a sudden decline, I would immediately communicate with the medical team through the appropriate channels, detailing the observations and suggesting potential solutions.
Regular updates to both clients and the healthcare team are essential. I maintain detailed documentation of all communication, ensuring a seamless flow of information throughout the care process.
Q 9. Describe your experience with crisis intervention and conflict resolution.
Crisis intervention and conflict resolution are integral to case management. My experience involves de-escalating volatile situations using calm, assertive communication. I’ve encountered situations ranging from family disputes to suicidal ideation. In one instance, a client became acutely agitated during a home visit due to unmet needs. I responded by acknowledging their feelings, offering immediate support, and collaborating with the mental health team to ensure immediate intervention and subsequent long-term solutions. Active listening, empathy, and a calm demeanor are crucial in these instances.
Conflict resolution often involves mediating disputes between family members or caregivers. I use a collaborative approach, facilitating open communication and helping parties find common ground. I help establish clear expectations and develop mutually agreeable plans. If necessary, I involve other professionals, such as therapists or social workers, to provide specialized support.
My approach relies heavily on understanding the root cause of the conflict and addressing underlying issues. This may involve exploring unmet needs, adjusting care plans, or providing access to additional resources. Documentation of all interventions and outcomes is meticulously maintained.
Q 10. How do you identify and address potential barriers to client success?
Identifying and addressing barriers to client success requires a proactive and holistic approach. I regularly assess clients’ needs across multiple domains – physical, mental, social, and environmental. These assessments help identify potential challenges like lack of transportation, financial constraints, limited social support, or inadequate housing. For example, a client might struggle to attend therapy appointments due to a lack of reliable transportation. I would immediately explore solutions, which may involve coordinating transportation services, adjusting appointment times, or exploring telehealth options.
Once barriers are identified, I create a plan of action that addresses each challenge systematically. This might involve connecting the client with community resources, advocating for necessary services, or collaborating with other professionals. I regularly reassess the effectiveness of interventions and make adjustments as needed. Success depends on a collaborative effort that includes regular communication and a commitment to supporting the client through any obstacle.
Q 11. What are your strategies for building rapport and trust with clients?
Building rapport and trust is crucial for effective case management. It’s built through consistent, reliable interactions. I begin by actively listening to the client’s concerns and validating their experiences. I ensure my interactions are respectful, empathetic, and non-judgmental. Demonstrating genuine care and concern goes a long way. I make a point to learn about the client’s preferences and goals, integrating their input into the care plan. For example, involving clients in the decision-making process regarding their treatment plan increases their sense of control and empowers them to take ownership.
Maintaining open communication is key. I provide regular updates and respond promptly to client inquiries. Honesty and transparency are paramount, even when delivering difficult news. Trust is earned over time through demonstrating competence, reliability, and a genuine commitment to the client’s well-being.
Q 12. Describe your experience collaborating with interdisciplinary teams.
Interdisciplinary collaboration is essential for successful case management. I have extensive experience working with diverse teams including physicians, nurses, therapists, social workers, and other healthcare professionals. I actively participate in team meetings, sharing relevant information and contributing to the development of integrated care plans. Effective communication is paramount in these collaborative efforts; using clear and concise language in team meetings and via electronic communication platforms is crucial for the efficient exchange of information. I use collaborative tools and techniques, such as shared electronic health records, to ensure consistent and efficient communication. For instance, during a care planning meeting, I’ll present a client’s holistic needs, drawing on my observations and input from various team members to create a comprehensive and well-coordinated care plan.
I understand the importance of each team member’s unique expertise and perspective, and I actively encourage open dialogue and the respectful exchange of ideas.
Q 13. How do you measure the effectiveness of your case management interventions?
Measuring the effectiveness of case management interventions is crucial for continuous improvement. I use a variety of methods, including tracking key performance indicators (KPIs) such as client progress towards goals, reduction in hospital readmissions, improvement in quality of life indicators, and client satisfaction. For example, if a client’s goal is to improve their medication adherence, I track their medication compliance through regular follow-ups and reviews. This data helps me quantify the efficacy of my interventions. Data is collected using various methods including client self-reporting, clinical observations and data from healthcare providers.
Client satisfaction surveys and feedback are also invaluable. Regular assessments of the client’s progress against their goals help to measure the impact and inform adjustments to the care plan as needed.
Q 14. What are your strategies for managing your own workload and stress levels?
Managing workload and stress is vital for both personal well-being and professional effectiveness. I utilize several strategies to maintain a healthy work-life balance and prevent burnout. Prioritization is crucial; I use techniques like time blocking and task lists to organize my day efficiently, focusing on the most urgent and important tasks first. I also proactively delegate tasks when possible and set realistic goals to avoid feeling overwhelmed. Regular breaks throughout the day are essential for maintaining focus and preventing fatigue.
Self-care is non-negotiable. This includes activities like exercise, healthy eating, and adequate sleep. I also prioritize activities that help me de-stress and recharge, such as spending time with family and friends, pursuing hobbies, or practicing mindfulness techniques.
Finally, seeking support from colleagues or supervisors when needed is important. Open communication about workload and challenges fosters a healthy work environment and helps prevent burnout.
Q 15. How do you stay current with best practices in case management?
Staying current in case management requires a multi-pronged approach. It’s not just about reading the latest journal articles (though that’s important!), but actively engaging with the field.
- Professional Organizations: Active membership in organizations like the Commission for Case Manager Certification (CCMC) or the National Association of Social Workers (NASW) provides access to continuing education, webinars, and networking opportunities with other professionals. These often highlight emerging trends and best practices.
- Conferences and Workshops: Attending conferences and workshops allows for direct interaction with leading experts and exposure to innovative techniques. These events usually cover new legislation, technological advancements, and evolving approaches to complex cases.
- Peer Learning: Regular interaction with colleagues through case reviews, informal discussions, and participation in professional groups fosters a continuous learning environment. Sharing experiences and challenges allows for collective problem-solving and the adoption of effective strategies.
- Journal Articles and Research: Regularly reviewing peer-reviewed journals and research papers in case management and related fields (e.g., social work, public health) keeps me abreast of the latest evidence-based practices and research findings. This ensures my approach aligns with the most current and effective methods.
- Online Resources: Utilizing reputable online resources, such as government health websites and professional organization websites, provides access to updated guidelines, regulations, and best practice recommendations.
For example, I recently attended a webinar on the application of telehealth in case management, which significantly influenced my approach to remote client support.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe a situation where you had to adapt your approach to meet a client’s unique needs.
I once worked with a client who was experiencing both physical and mental health challenges, compounded by significant financial difficulties. A standard approach focusing solely on her physical rehabilitation wasn’t effective because her depression and financial stress were hindering her progress.
To adapt, I employed a holistic approach. I coordinated with her psychiatrist to ensure her mental health needs were addressed concurrently with her physical therapy. Furthermore, I connected her with social services to help her navigate the application process for financial assistance, including housing and food support. This integrated, multidisciplinary approach addressed the root causes of her challenges, leading to significantly improved outcomes compared to what a solely physical-therapy focused approach would have achieved. This experience underscored the importance of considering the interconnectedness of a client’s needs and tailoring interventions accordingly.
Q 17. How do you ensure client confidentiality and data security?
Client confidentiality and data security are paramount. My practice strictly adheres to HIPAA regulations and other relevant privacy laws.
- HIPAA Compliance: I am trained in HIPAA compliance and ensure all interactions, documentation, and data storage adhere strictly to these regulations. This includes secure electronic health records (EHRs), password protection, and limited access to sensitive information.
- Data Encryption: All electronic client information is encrypted both in transit and at rest to prevent unauthorized access.
- Secure Communication: I use secure communication channels, such as encrypted email and telehealth platforms, to protect sensitive information during client interactions.
- Physical Security: Physical files, if any, are stored in locked cabinets, and access is restricted to authorized personnel.
- Regular Training: I participate in regular training on data security best practices and emerging threats to stay informed about evolving security protocols.
Imagine a scenario where a client’s medical records are inadvertently accessed. The consequences could be devastating – both legally and ethically. Therefore, proactive measures are essential to prevent breaches and maintain client trust.
Q 18. Explain your understanding of different reimbursement models in healthcare.
Different reimbursement models in healthcare significantly impact case management. Understanding these models is crucial for effective resource allocation and service delivery.
- Fee-for-Service (FFS): In this model, providers are reimbursed for each service rendered. This can incentivize higher volume of services, but may not always align with value-based care.
- Capitation: Providers receive a fixed payment per member per month (PMPM), regardless of the services provided. This incentivizes preventative care and efficient resource management.
- Value-Based Care (VBC): Providers are reimbursed based on the quality of care and patient outcomes. This model encourages a focus on improving health and reducing costs.
- Episode-Based Payment: Providers receive a single payment for managing a specific episode of care, such as a surgical procedure or a course of treatment for a particular condition. This incentivizes efficient and coordinated care within a defined timeframe.
For example, in a capitated model, I might prioritize preventative interventions to reduce hospital readmissions, as this directly impacts my organization’s financial reimbursement. Understanding these models helps me to advocate for resources for clients and to make informed decisions regarding service utilization.
Q 19. Describe your experience with performance improvement initiatives in case management.
I’ve been involved in several performance improvement initiatives aimed at enhancing case management outcomes. These typically involve a structured, data-driven approach:
- Identifying Key Performance Indicators (KPIs): We begin by defining relevant KPIs such as client satisfaction scores, readmission rates, length of stay, and cost per case.
- Data Collection and Analysis: We systematically collect data on these KPIs to identify areas for improvement. This might involve analyzing EHR data, surveys, and other relevant sources.
- Root Cause Analysis: We use tools like fishbone diagrams or 5 Whys to understand the underlying causes of performance gaps.
- Intervention Implementation: Based on the analysis, we develop and implement interventions, such as new training programs, updated protocols, or improved communication strategies.
- Evaluation and Monitoring: We continuously monitor the impact of the interventions and make adjustments as needed. This iterative process is crucial for ensuring sustainability and continuous improvement.
In one project, we analyzed client satisfaction surveys and found a significant gap in communication. By implementing a new communication protocol and providing additional training, we significantly improved client satisfaction scores within six months.
Q 20. How do you utilize data analysis to improve case management outcomes?
Data analysis is crucial for improving case management outcomes. By examining data, we can identify trends, predict risks, and tailor interventions for optimal results.
- Identifying High-Risk Clients: Analyzing data such as medical history, social determinants of health, and prior utilization patterns can help identify clients at high risk of adverse events. This allows for proactive interventions to prevent complications.
- Tracking Key Metrics: Regularly monitoring KPIs allows for timely detection of performance gaps and prompt corrective action. This might include tracking readmission rates, length of stay, and client satisfaction scores.
- Predictive Modeling: Using advanced analytics, we can develop predictive models to identify clients at high risk of specific outcomes, such as hospital readmission or exacerbation of chronic conditions. This allows for proactive management and targeted interventions.
- Resource Allocation: Data analysis informs resource allocation by identifying areas where resources are most effectively used to maximize positive impact on client outcomes.
For instance, by analyzing data on hospital readmissions, we identified a subgroup of clients with a specific chronic condition who were at particularly high risk. We then implemented a targeted intervention program focusing on medication adherence and lifestyle modifications, leading to a significant reduction in readmissions within that subgroup.
Q 21. Describe your experience with utilization management and resource allocation.
Utilization management and resource allocation are critical functions in case management. They ensure that clients receive the appropriate level of care at the most appropriate setting, while optimizing the use of available resources.
- Prior Authorization: I often assist in obtaining prior authorizations for services to ensure that the client’s insurance covers the necessary interventions. This process requires meticulous documentation and communication with insurance providers.
- Care Coordination: I facilitate communication among multiple healthcare providers to ensure that care is coordinated and that the client receives the most appropriate services at each stage of their care journey.
- Discharge Planning: I’m deeply involved in discharge planning, assessing the client’s needs and coordinating the transition to the appropriate post-discharge setting (e.g., home, rehabilitation facility, assisted living). This requires careful consideration of the client’s functional abilities and support systems.
- Resource Identification and Referral: I identify and refer clients to appropriate community resources, including social services, financial assistance programs, and support groups, to address their holistic needs.
For example, I recently worked with a client who required skilled nursing care following a hospital stay. Through careful coordination with the hospital discharge planner and the insurance provider, I secured authorization for skilled nursing facility placement, ensuring a smooth and safe transition for the client while optimizing resource utilization.
Q 22. How do you advocate for your clients’ needs within the healthcare system?
Advocating for my clients’ needs within the healthcare system is a core part of my role as a case manager. It involves acting as a liaison between the client, their family, and the various healthcare providers involved in their care. This requires strong communication, negotiation, and problem-solving skills.
My approach is multifaceted. First, I thoroughly understand my client’s needs and preferences, documenting their wishes and healthcare goals. This might involve using standardized assessment tools like the Katz Index of Independence in Activities of Daily Living (ADLs) or the Lawton Instrumental Activities of Daily Living (IADLs) scale to objectively assess functional capabilities. Then, I clearly articulate those needs to the healthcare team—physicians, nurses, therapists, social workers—ensuring everyone is on the same page. If there are disagreements or challenges in accessing services, I will actively negotiate and advocate, using data and evidence to support my client’s case. For instance, I might present data showing the positive impact of a specific therapy on a patient’s recovery, pushing for its approval despite potential cost considerations. Finally, I actively empower my clients to participate in their care decisions, helping them understand their options and express their needs effectively.
For example, I once advocated for a client needing a specific, expensive medication. The insurance company initially denied coverage. Through careful documentation of the patient’s condition and the benefits of the medication, along with appeals and conversations with the insurance company’s case manager, we successfully secured coverage, ensuring the client received the treatment they needed.
Q 23. Explain your understanding of different assessment tools used in case management.
Various assessment tools are crucial for effective case management, enabling me to accurately gauge a client’s needs and develop appropriate care plans. These tools can be broadly categorized into functional assessments, psychosocial assessments, and financial assessments.
- Functional Assessments: These tools evaluate a client’s ability to perform activities of daily living (ADLs), such as bathing, dressing, and eating, and instrumental activities of daily living (IADLs), such as managing finances and transportation. Examples include the Katz Index, Lawton IADL scale, and the Barthel Index. These help determine the level of assistance a client requires.
- Psychosocial Assessments: These tools assess the client’s mental health, emotional well-being, social support system, and coping mechanisms. Examples include standardized depression scales like the PHQ-9 or anxiety scales like the GAD-7, and social support questionnaires. Understanding this aspect is critical for creating holistic care plans.
- Financial Assessments: These evaluate a client’s financial resources and ability to afford healthcare services. This might involve reviewing income, assets, and insurance coverage. This is important to identify and secure necessary financial assistance.
The choice of assessment tools depends heavily on the individual client’s circumstances and the specific goals of the case management intervention. A comprehensive assessment usually involves a combination of these tools to paint a complete picture of the client’s needs.
Q 24. How do you handle situations where client needs exceed available resources?
When client needs exceed available resources, it’s essential to employ a strategic and creative approach. My first step is to fully document the client’s needs, clearly articulating the discrepancy between their requirements and the available resources. This documentation serves as the foundation for my advocacy efforts. Next, I explore all possible resource options, including public and private programs, charitable organizations, and community services. This might involve researching grant opportunities, applying for financial assistance programs, or connecting the client with relevant support groups.
If resources remain limited, I prioritize the client’s most urgent needs. This often involves using a needs prioritization framework, focusing on those needs that pose the most significant risk to the client’s health and well-being. Negotiation and collaboration with healthcare providers are key. I might discuss alternative treatment options or explore ways to optimize existing resources. I may also work to advocate for policy changes or systemic improvements that could address the resource gap in the long term.
For example, I once encountered a client needing extensive home healthcare after a stroke, but their insurance only covered a limited number of hours. To bridge the gap, I collaborated with the local volunteer organization, securing additional support for the client’s personal care and transportation needs, enabling them to stay safely at home.
Q 25. Describe your experience with discharge planning and transition of care.
Discharge planning and transition of care are critical components of my role, ensuring a smooth and safe transition for clients leaving a healthcare setting. It begins long before the actual discharge date. Early assessment is crucial. I assess the client’s physical, psychosocial, and environmental needs to identify potential challenges they may face at home. This involves collaborating with the medical team to understand the client’s prognosis, treatment plan, and any ongoing medical needs.
Next, I develop a comprehensive discharge plan which outlines the necessary services and support, including medication management, rehabilitation therapies, home healthcare, and social services. I coordinate with the client’s family or caregivers to ensure they understand and can provide the necessary support. I also arrange for necessary equipment and supplies to be delivered to their home before discharge. Finally, I ensure a thorough handover of care to the post-discharge team, providing all relevant information to ensure continuity of care. This includes coordinating with home healthcare agencies and medical providers for ongoing care and follow-up appointments.
For instance, for a client transitioning from acute rehabilitation to home, I collaborated with the rehab team to devise a home exercise program, arranged for home health nursing visits to manage medications and wound care, and ensured the necessary mobility equipment was delivered before the client returned home.
Q 26. How do you ensure seamless transitions of care between different healthcare settings?
Seamless transitions of care require meticulous planning and proactive communication between healthcare providers and settings. It’s about creating a cohesive system rather than a series of isolated events. I begin by establishing strong communication links with all parties involved in the client’s care—from hospital physicians and nurses to primary care providers, specialists, and home healthcare agencies. This might involve attending care team meetings, facilitating regular communication, and using electronic health record systems effectively.
A standardized discharge summary is crucial. It includes essential information on the client’s condition, medications, treatment plan, and ongoing needs, providing all relevant providers with a shared understanding. This is crucial for consistent and coordinated care. I also leverage technology such as telehealth platforms to maintain ongoing monitoring and support, even after discharge, thereby ensuring the client feels supported. I make sure the client and their caregivers are fully informed and involved in the process. This proactive and communicative approach minimizes risks and ensures smooth transitions.
For example, I helped a client transition from a hospital to a skilled nursing facility and then to home. Through regular communication and coordinated care planning, I ensured all providers had access to the latest updates on the client’s condition and that they were all working towards the same goals, ultimately leading to a smooth and efficient transition.
Q 27. Describe your experience in developing and implementing a new case management program.
My experience in developing and implementing a new case management program involved a multi-step process. It began with a thorough needs assessment to identify gaps in service and understand the target population’s needs. This involved analyzing existing data, conducting surveys, and interviewing stakeholders, including clients, healthcare providers, and community leaders. The needs assessment guided the design of the program’s goals and objectives, ensuring it addressed identified needs effectively.
Next, I developed a comprehensive program design, outlining the program’s structure, services, and processes. This involved specifying the types of assessments to be used, the criteria for client selection, the methods for case management, and the mechanisms for monitoring and evaluation. Crucial to this was securing buy-in and collaboration from all stakeholders. This required active communication, presenting data clearly, and addressing concerns collaboratively. Implementation involved recruiting and training staff, establishing protocols, and securing necessary resources, including funding, technology, and physical space. Finally, a robust evaluation plan, including both quantitative and qualitative measures, was incorporated from the outset to ensure the program’s effectiveness and make any necessary adjustments.
For example, I was instrumental in developing a new case management program for individuals with chronic heart failure, improving access to appropriate home healthcare, reducing hospital readmissions, and improving patient quality of life. The success of this program was due to careful planning, stakeholder involvement, and the use of data-driven decision-making.
Key Topics to Learn for Case Management and Coordination Interview
- Case Assessment and Prioritization: Understanding how to quickly assess client needs and prioritize tasks based on urgency and impact. Practical application: Describing your methodology for handling competing deadlines and multiple client cases simultaneously.
- Resource Allocation and Management: Efficiently allocating resources (time, personnel, budget) to achieve optimal outcomes. Practical application: Providing examples of how you’ve successfully managed limited resources to meet challenging client needs.
- Communication and Collaboration: Effectively communicating with clients, colleagues, and other stakeholders. Practical application: Discussing strategies for fostering strong working relationships and resolving conflicts.
- Documentation and Reporting: Maintaining accurate and thorough records, preparing concise and informative reports. Practical application: Explaining your experience with various case management software and reporting systems.
- Regulatory Compliance and Ethical Considerations: Adhering to relevant laws, regulations, and ethical guidelines. Practical application: Describing how you ensure client confidentiality and maintain professional boundaries.
- Problem-Solving and Decision-Making: Identifying and resolving complex case-related issues. Practical application: Sharing examples of successful problem-solving strategies used in previous case management roles.
- Technology Proficiency: Demonstrating familiarity with relevant case management software and technologies. Practical application: Highlighting your skills with specific software (mentioning names without linking) and your ability to adapt to new technologies.
- Client Advocacy and Support: Effectively advocating for clients’ needs and providing emotional support. Practical application: Describing how you build trust and rapport with clients to achieve positive outcomes.
Next Steps
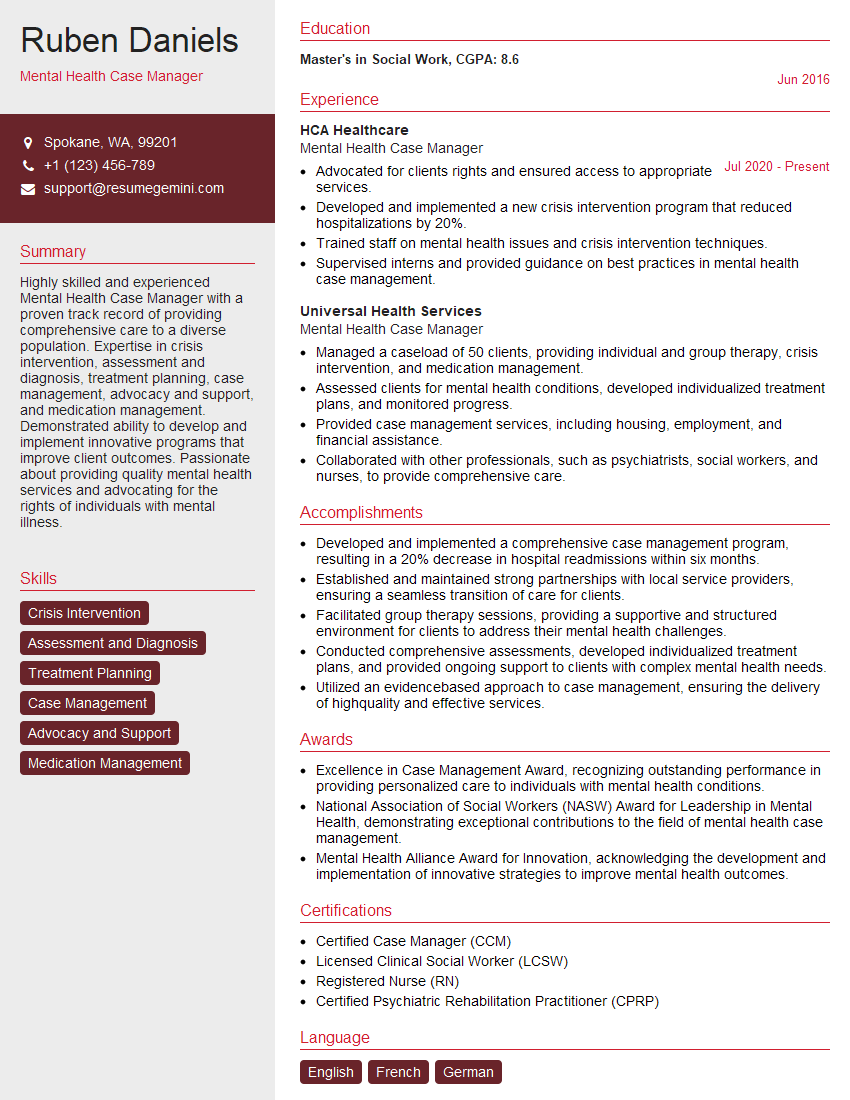
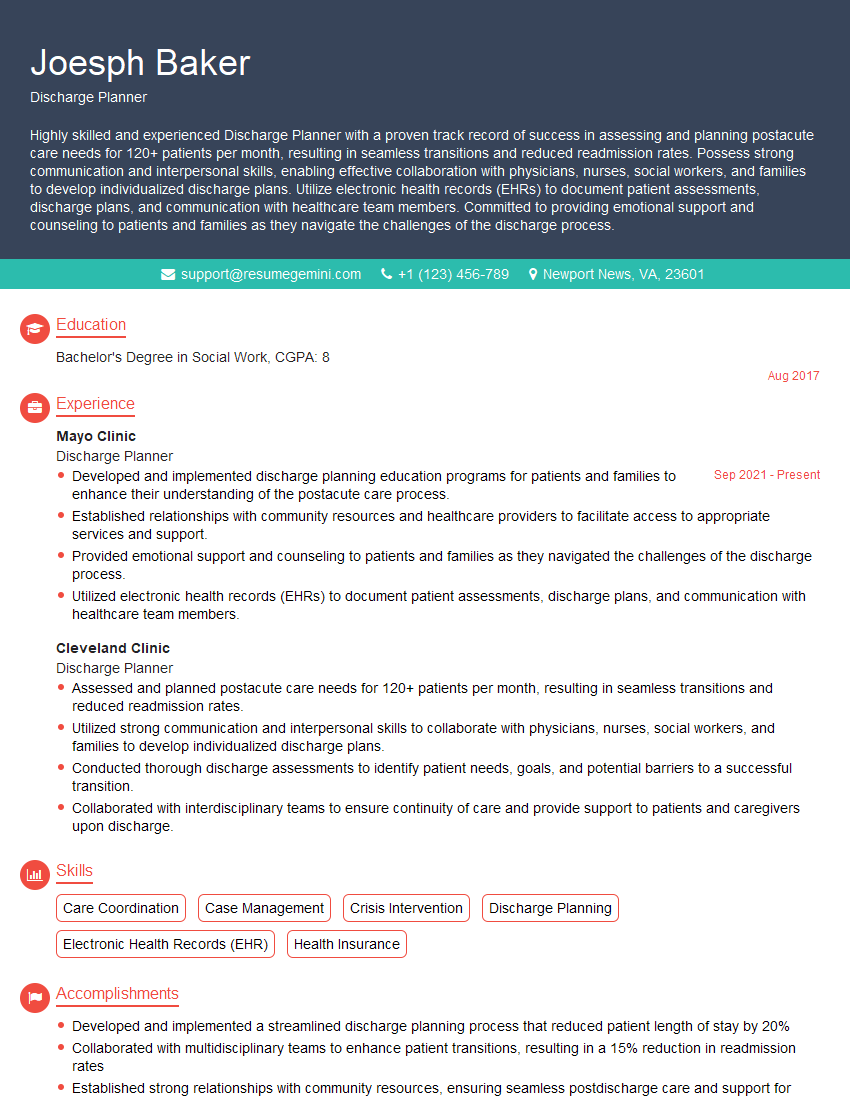
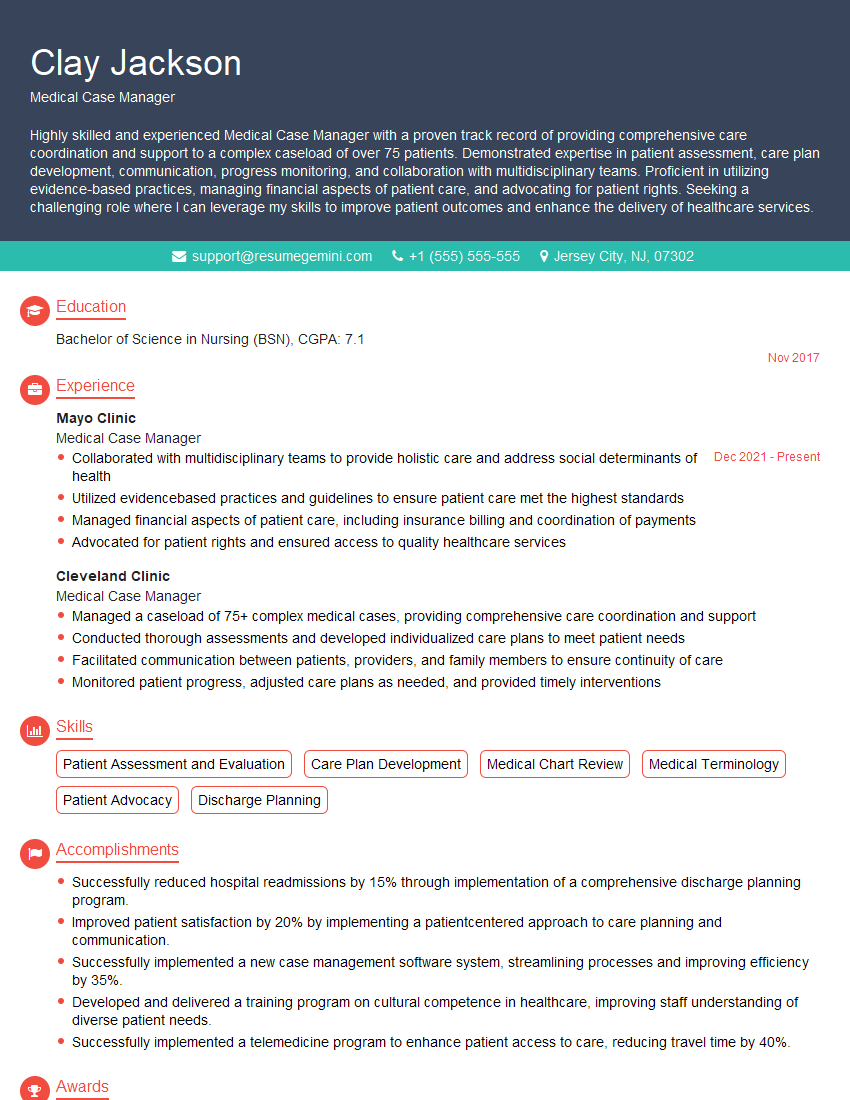
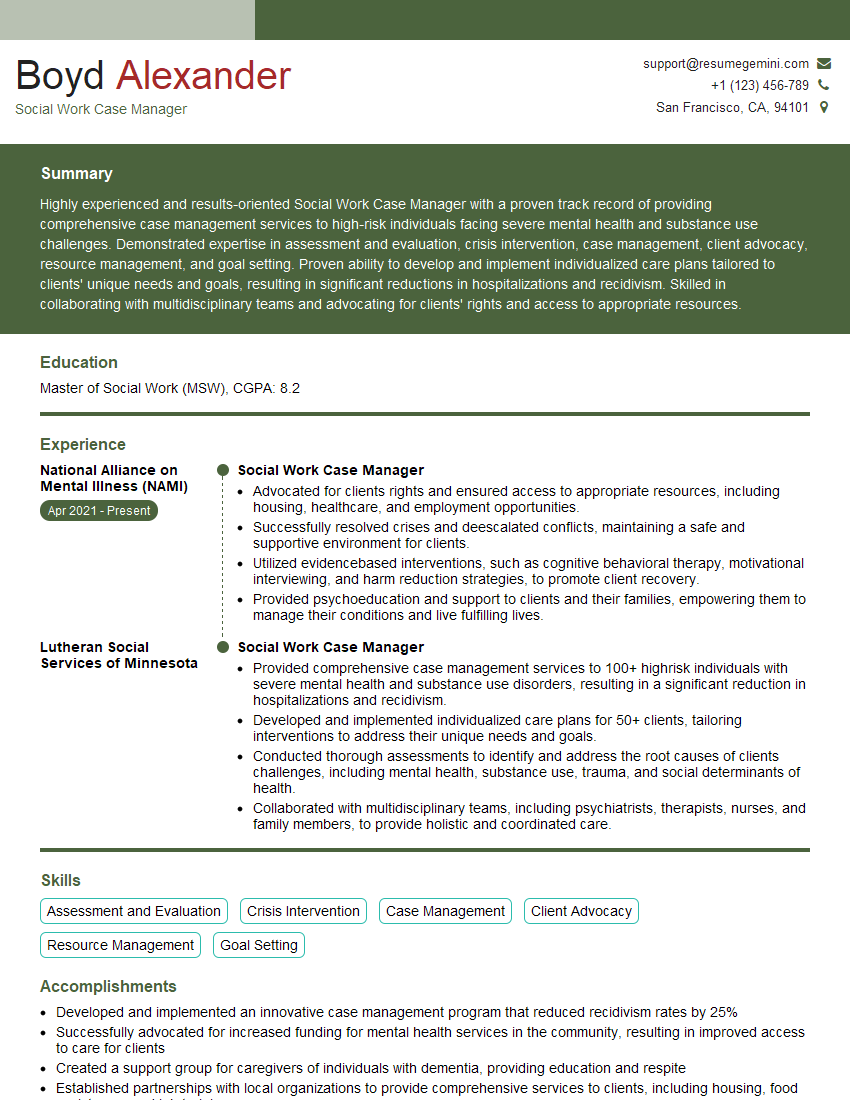
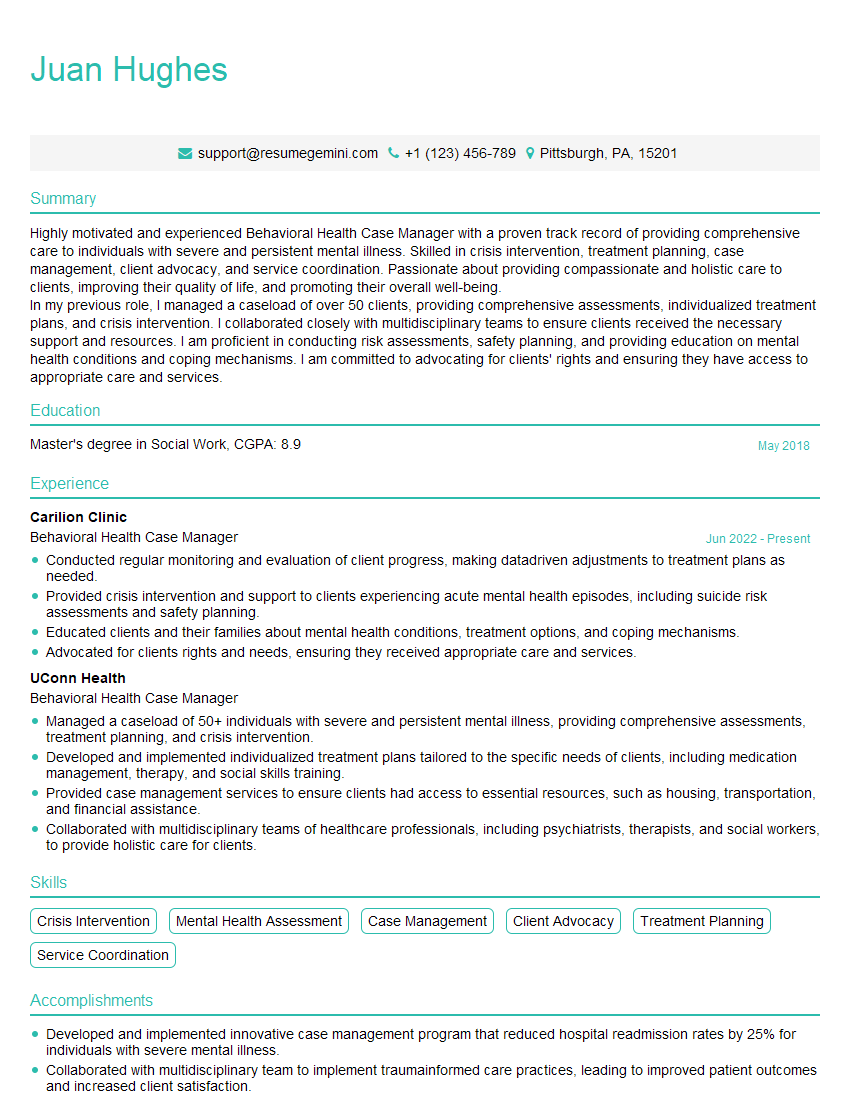
Mastering Case Management and Coordination is crucial for career advancement in various fields, opening doors to leadership roles and increased responsibility. An ATS-friendly resume is key to getting your application noticed by recruiters. To make your resume stand out, leverage ResumeGemini, a trusted resource for creating professional, impactful resumes. ResumeGemini provides examples of resumes tailored to Case Management and Coordination, helping you showcase your skills and experience effectively. Take the next step towards your dream career – build a compelling resume that highlights your expertise in this dynamic field.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.