Unlock your full potential by mastering the most common Catheterization Laboratory Procedures interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Catheterization Laboratory Procedures Interview
Q 1. Describe the steps involved in a diagnostic cardiac catheterization.
A diagnostic cardiac catheterization is a minimally invasive procedure used to visualize the heart’s chambers, valves, and coronary arteries. It involves inserting a thin, flexible tube (catheter) into a blood vessel, typically in the groin or wrist, and guiding it to the heart under fluoroscopic guidance (real-time X-ray imaging).
- Access Site Preparation: The chosen site is cleaned and sterilized. Local anesthesia is administered.
- Puncture and Catheter Insertion: A small incision is made, and a needle is used to puncture the artery. A guidewire is then inserted, followed by the catheter.
- Catheter Advancement: Using fluoroscopy, the catheter is carefully advanced through the vascular system into the heart chambers and coronary arteries.
- Angiography: Contrast dye is injected through the catheter, allowing for visualization of the heart structures and blood flow on the fluoroscopy screen. This imaging process is called angiography, and it provides detailed information about the heart’s function and any abnormalities.
- Data Acquisition and Analysis: Hemodynamic measurements (blood pressure, oxygen saturation) may be obtained. Images are recorded and analyzed by the cardiologist to identify blockages, valve problems, or other abnormalities.
- Catheter Removal and Closure: Once the procedure is complete, the catheter is removed, and pressure is applied to the access site to prevent bleeding. In some cases, a closure device may be used to facilitate hemostasis (stop bleeding).
Think of it like a plumber using a camera to inspect pipes – we’re using a catheter and contrast dye to ‘see inside’ the heart and its vessels.
Q 2. Explain the differences between right and left heart catheterization.
Right and left heart catheterizations differ in their approach and the structures they visualize.
- Right Heart Catheterization: This focuses on the right side of the heart (right atrium, right ventricle, and pulmonary arteries). It’s primarily used to assess pressure and oxygen saturation in these areas, providing information about pulmonary pressures and overall cardiac output. For example, it can detect pulmonary hypertension (high blood pressure in the lungs).
- Left Heart Catheterization: This involves accessing the left side of the heart (left atrium, left ventricle, and coronary arteries). It’s more complex, often requiring a selective catheterization of the coronary arteries (coronary angiography) to assess for blockages. This procedure helps diagnose coronary artery disease and is commonly performed before procedures like angioplasty or stenting.
Essentially, right heart cath looks at the blood flow from the heart to the lungs, while left heart cath focuses on the blood flow from the lungs to the body and the coronary arteries’ health. They can sometimes be done together, providing a comprehensive assessment.
Q 3. What are the potential complications of a cardiac catheterization?
Cardiac catheterization, while generally safe, carries potential complications. These can range from minor to life-threatening.
- Bleeding or Hematoma at the Puncture Site: This is relatively common and usually manageable with pressure. Severe bleeding is rare but can require surgical intervention.
- Arterial Thrombosis or Vasospasm: A blood clot can form at the puncture site or in the artery. Vasospasm (narrowing of the artery) can reduce blood flow. These are addressed with medication and sometimes procedures like angioplasty.
- Infection: Although rare with proper sterile technique, infection at the puncture site or more seriously, bloodstream infection, can occur. Antibiotics are used to treat infection.
- Stroke or Transient Ischemic Attack (TIA): Emboli (traveling clots or plaque) can dislodge during the procedure and cause a stroke or TIA. Careful technique and adequate anticoagulation help reduce this risk.
- Cardiac Arrhythmias: The catheter can sometimes irritate the heart’s electrical conduction system, leading to irregular heartbeats. These are generally transient and managed with medication.
- Allergic Reaction to Contrast Dye: Some patients are allergic to iodine-based contrast agents, leading to reactions ranging from mild rash to severe anaphylaxis, requiring immediate treatment.
- Kidney Damage: Contrast dye can be nephrotoxic (harmful to the kidneys), especially in patients with pre-existing kidney disease. Careful hydration and medication can help mitigate this.
These complications are carefully monitored, and measures are taken to minimize their occurrence. It’s crucial to obtain a thorough patient history and perform appropriate risk assessments before the procedure.
Q 4. How do you manage a patient experiencing a vasovagal reaction during a procedure?
A vasovagal reaction during a cardiac catheterization is characterized by a sudden drop in heart rate and blood pressure, often accompanied by nausea, vomiting, and fainting. It’s a reflex response, usually triggered by pain, anxiety, or the sight of blood.
- Immediate Actions: The procedure is immediately stopped. The patient is placed in a supine (flat) position with legs elevated to improve blood flow to the brain.
- Oxygen Administration: Supplemental oxygen is provided to increase oxygen levels in the blood.
- Fluid Bolus: Intravenous fluids are administered to help restore blood volume and blood pressure.
- Medication: If the reaction is severe or doesn’t respond to initial measures, atropine (to increase heart rate) or other medications might be used.
- Monitoring: Vital signs (heart rate, blood pressure, oxygen saturation) are continuously monitored until the patient is stable.
The key is immediate recognition and prompt intervention. We need to act quickly to restore adequate blood flow to the brain and prevent complications.
Q 5. Describe your experience with different types of catheters and their applications.
My experience encompasses a wide range of catheters used in various cardiac procedures. The selection depends on the specific anatomy and the goals of the procedure.
- Judkins Catheters: These are commonly used for coronary angiography, designed to selectively engage the left and right coronary arteries. They come in various sizes and shapes for optimal access.
- Amplatz Catheters: These are more versatile and can be used for accessing various heart chambers and vessels. They’re frequently used for left heart catheterization.
- Pigtail Catheters: These are useful for pressure measurements and left ventriculography (imaging the left ventricle). Their curved tip makes them ideal for navigating the heart chambers.
- Multipurpose Catheters: Some catheters are designed with multiple ports or side holes, enabling simultaneous pressure measurements and contrast injections.
Each catheter has unique properties, and expertise lies in selecting the appropriate catheter for each individual patient and procedure, minimizing the risk of complications and achieving the best possible diagnostic or interventional results. For example, a very tortuous vessel might require a hydrophilic catheter to navigate easily.
Q 6. Explain the principles of hemodynamic monitoring during a catheterization.
Hemodynamic monitoring during catheterization provides real-time assessment of the heart’s function and circulatory system. It involves measuring various parameters to understand cardiac output, pressures, and oxygen saturation.
- Pressure Measurements: Catheters are positioned in specific locations within the heart chambers and great vessels to measure pressures (e.g., pulmonary artery pressure, left ventricular pressure). These pressures reflect the heart’s pumping ability and the resistance to blood flow in the circulatory system.
- Oxygen Saturation: Oxygen saturation measurements are obtained from different locations to determine the efficiency of oxygen uptake and delivery. Low oxygen saturation can indicate problems like shunts or pulmonary embolism.
- Cardiac Output: Various techniques, such as thermodilution, are used to measure the amount of blood pumped by the heart per minute. This reflects the overall efficiency of the heart.
Hemodynamic data helps guide diagnosis, treatment decisions, and the assessment of the procedure’s effects. For example, a sudden drop in blood pressure during a procedure might trigger immediate intervention. It’s like monitoring the vitals of a car engine to ensure it’s running smoothly.
Q 7. What are the safety protocols for radiation exposure in the cath lab?
Radiation safety is paramount in the catheterization laboratory. Both patients and staff are exposed to ionizing radiation during fluoroscopy. Protocols are implemented to minimize exposure while ensuring optimal image quality.
- Lead Aprons and Shields: Staff members wear lead aprons and thyroid shields to reduce radiation exposure. Lead shields may also be placed on the patient to protect specific areas.
- Pulse Fluoroscopy: Instead of continuous fluoroscopy, pulsed fluoroscopy delivers radiation in short bursts, significantly reducing the total radiation dose. This is routinely used whenever possible.
- Distance: Maintaining a safe distance from the radiation source is crucial. Staff are trained to move away when not actively involved in the procedure.
- Time Optimization: Procedures are designed to be as efficient as possible, minimizing the time the patient and staff are exposed to radiation.
- Radiation Monitoring: Dosimeters are worn by staff to monitor individual radiation exposure. Regular monitoring ensures that exposure levels remain within safe limits.
- Room Shielding: Cath labs are designed with shielding in the walls, floors, and ceilings to limit radiation leakage outside the room.
These protocols are vital for ensuring the safety of both patients and staff and are meticulously followed in every procedure. Regular training and adherence to these protocols are key to minimizing radiation risks.
Q 8. How do you assess a patient’s readiness for a cardiac catheterization procedure?
Assessing a patient’s readiness for cardiac catheterization involves a thorough evaluation encompassing several key areas. It’s like preparing for a delicate surgical procedure; you need to ensure the patient is in optimal condition to minimize risks and maximize the chances of a successful outcome.
- Medical History & Physical Exam: We meticulously review the patient’s medical history, focusing on conditions like bleeding disorders, allergies (especially to iodine-based contrast media), renal function, and previous cardiac procedures. A comprehensive physical exam assesses their overall health status.
- Laboratory Tests: Blood tests are crucial to evaluate renal function (creatinine, BUN), clotting factors (PT, PTT, INR), and hemoglobin levels. These help us determine the patient’s suitability for the procedure and anticipate potential complications.
- Medication Review: We carefully review the patient’s medication list, identifying potential interactions with contrast media or anesthetic agents. Some medications, like anticoagulants, may need to be adjusted prior to the procedure. For example, patients on warfarin require careful INR management before the procedure.
- Informed Consent: The patient’s understanding of the procedure, its benefits, risks, and alternatives is paramount. We ensure they have received a clear and comprehensive explanation and have given informed consent.
- NPO Status: Patients are typically required to be NPO (nothing by mouth) for a specified period before the procedure to minimize the risk of aspiration during the procedure. This is a critical aspect of patient preparation.
For instance, a patient with severely impaired renal function might require alternative approaches or a delay in the procedure to minimize the risk of contrast-induced nephropathy. Similarly, a patient with a history of bleeding disorders might require pre-procedural blood transfusions or other interventions to manage the risk of bleeding complications.
Q 9. What is your experience with post-procedure patient care in the Cath Lab?
Post-procedure care in the Cath Lab is critically important for ensuring patient safety and recovery. It’s like the aftercare for a delicate operation – we carefully monitor the patient and provide necessary support to ensure a smooth transition back to a stable state.
- Hemodynamic Monitoring: We closely monitor vital signs, including heart rate, blood pressure, and rhythm, looking for any signs of complications like bleeding or arrhythmias. Continuous monitoring using ECG and blood pressure cuffs is standard practice.
- Access Site Monitoring: We meticulously assess the arterial puncture site for any signs of bleeding or hematoma formation. Pressure dressings are applied and closely monitored to maintain hemostasis.
- Fluid Balance: Fluid status is carefully managed, especially in patients who have received large volumes of contrast media, to prevent dehydration or fluid overload. This is vital, especially in patients with renal insufficiency.
- Pain Management: Pain management is provided as needed to ensure patient comfort. Medication is often administered for pain and any discomfort at the puncture site.
- Patient Education: Before discharge, patients receive comprehensive instructions on activity restrictions, medication regimens, and signs and symptoms to watch out for. This empowers them to effectively manage their recovery.
One memorable instance involved a patient who developed a significant hematoma at the femoral artery access site. We immediately took steps to control the bleeding by applying direct pressure and subsequently called in interventional radiology for possible surgical repair if necessary. This highlights the importance of constant vigilance.
Q 10. Explain the role of contrast media in cardiac catheterization.
Contrast media plays a vital role in cardiac catheterization, acting like a spotlight that illuminates the heart’s intricate network of vessels. It’s a solution that is injected into the bloodstream to make the coronary arteries and other blood vessels visible under fluoroscopy (real-time X-ray imaging).
- Visualization of Coronary Arteries: The contrast medium allows us to visualize the coronary arteries, revealing blockages, narrowings (stenosis), or other abnormalities. This is crucial for diagnosing coronary artery disease.
- Guiding Catheter Placement: The contrast helps us precisely guide catheters into specific vessels, enabling interventions such as angioplasty or stent placement.
- Assessment of Blood Flow: By observing the flow of contrast, we can assess the blood flow through the coronary arteries and identify areas of impaired flow, or even measure pressure in various chambers of the heart.
Contrast media is typically iodine-based, and its choice depends on the patient’s renal function and overall health status. Patients with impaired renal function, for example, might require non-ionic, low-osmolar contrast agents to reduce the risk of contrast-induced nephropathy.
Q 11. Describe your experience with emergency situations in the cath lab (e.g., perforation, bleeding).
Emergency situations in the Cath Lab, while rare, demand immediate, decisive action. The team must be prepared to handle them swiftly and efficiently, acting as a well-coordinated unit. Think of it like a surgical team responding to an unexpected complication during surgery.
- Perforation: Vascular perforation is a serious complication that requires immediate management. This typically involves placing a vascular plug, applying manual pressure, or surgical repair to control bleeding. In most cases, the team responds promptly to the patient’s response to the procedure, using fluoroscopy to localize the perforation and decide on the correct course of action.
- Bleeding: Excessive bleeding from the arterial puncture site requires immediate pressure, potentially followed by surgical exploration if needed. Monitoring vital signs and managing blood loss are crucial.
- Arrhythmias: Cardiac arrhythmias can occur during or after the procedure. Prompt identification and treatment with medication or cardioversion may be necessary.
In one case, a patient experienced a perforation during a complex PCI procedure. The team reacted swiftly, employing a vascular closure device to seal the perforation and simultaneously managing the patient’s hemodynamic status. This rapid response prevented a major complication.
Q 12. How do you maintain sterility and asepsis in the cath lab?
Maintaining sterility and asepsis in the Cath Lab is paramount to prevent infection, a critical aspect of patient safety. It’s a high-stakes environment requiring meticulous attention to detail, similar to an operating room.
- Strict Sterile Techniques: All personnel follow strict sterile techniques, including hand hygiene, gowning, gloving, and the use of sterile drapes and instruments. This includes disinfection of all surfaces and equipment before and after the procedure.
- Environmental Control: The Cath Lab environment is strictly controlled to minimize airborne contamination. High-efficiency particulate air (HEPA) filtration systems are utilized to maintain air quality.
- Equipment Sterilization: All equipment used in the procedure, including catheters, guidewires, and other instruments, is properly sterilized or disinfected according to established protocols.
- Aseptic Techniques during Catheterization: Aseptic techniques are rigorously followed during catheter insertion and manipulation to prevent contamination of the vascular system.
We use a combination of antiseptic solutions such as chlorhexidine and povidone-iodine to ensure thorough disinfection of the patient’s skin at the access site and regularly assess the room’s sterilization.
Q 13. What is your understanding of fluoroscopy and its use in cardiac catheterization?
Fluoroscopy is an integral component of cardiac catheterization, providing real-time X-ray imaging that acts like a live roadmap guiding the procedure. It’s essential for visualization and precision.
- Real-time Imaging: Fluoroscopy allows continuous visualization of the heart and blood vessels during the procedure, enabling precise catheter placement and manipulation.
- Guiding Interventions: It guides the insertion and advancement of catheters, balloons, and stents during procedures like angioplasty and stent placement, ensuring accurate positioning.
- Assessment of Vessel Anatomy: Fluoroscopy helps assess the anatomy of the coronary arteries and other vessels, identifying areas of stenosis, occlusion, or other abnormalities. It essentially lets us see inside the body in real time.
- Monitoring Procedure Progress: We monitor the procedure’s progress using fluoroscopy, ensuring that the intervention is effective and that there are no complications.
Imagine trying to navigate a complex road system without a map – fluoroscopy provides that essential real-time map for navigating the intricate network of blood vessels within the heart.
Q 14. Describe your experience with various types of angioplasty.
Angioplasty involves widening narrowed or blocked arteries, often using balloons and stents. There are various types of angioplasty procedures, each tailored to specific needs.
- Percutaneous Coronary Intervention (PCI): This is the most common type, involving inflating a balloon catheter to compress plaque against the artery wall, restoring blood flow. Stents are often deployed to keep the artery open.
- Balloon Angioplasty: This is a simpler form of angioplasty using a balloon catheter to widen the artery. It is often combined with stent placement.
- Rotational Atherectomy: This technique uses a high-speed rotating burr to remove calcified plaque in severely calcified arteries.
- Directional Atherectomy: This technique uses a catheter with a cutting blade to shave away plaque from the artery walls.
- Laser Angioplasty: This uses lasers to vaporize plaque, although it’s less commonly used now.
I’ve extensive experience in all these techniques, having performed countless PCIs, including those involving complex lesions and bifurcations. A memorable case involved a patient with a severely calcified lesion in the left main coronary artery. We successfully deployed a drug-eluting stent using rotational atherectomy to prepare the vessel, restoring blood flow and improving the patient’s prognosis.
Q 15. How do you interpret hemodynamic data obtained during a cardiac catheterization?
Interpreting hemodynamic data during cardiac catheterization involves a systematic approach to understand the patient’s cardiovascular status. We analyze pressure waveforms (obtained from catheters placed in various heart chambers and vessels), flow measurements (obtained with thermodilution or other techniques), and calculated parameters (e.g., cardiac output, stroke volume, systemic vascular resistance).
For example, a low cardiac output might suggest heart failure, while elevated pulmonary capillary wedge pressure (PCWP) could indicate left-sided heart failure. Analyzing the shape of the pressure waveforms gives further clues. A ‘peaked’ left ventricular pressure waveform suggests hypertrophy, whereas a ‘flattened’ waveform might signify decreased contractility. We correlate this data with the patient’s clinical presentation and the angiographic findings to formulate a comprehensive picture of their condition. We meticulously compare pre- and post-intervention hemodynamic data to assess the effectiveness of the procedure.
Consider a patient with chest pain and suspected coronary artery disease. We might find elevated PCWP, low cardiac output, and depressed left ventricular ejection fraction (LVEF). Post-PCI, we’d expect to see improved LVEF, increased cardiac output, and possibly a decrease in PCWP if the intervention successfully relieved the coronary obstruction. These changes would indicate a positive response to the treatment.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What is your experience with stenting procedures?
I have extensive experience in various stenting procedures, including drug-eluting stents (DES) and bare-metal stents (BMS). My experience encompasses a wide range of coronary artery complexities, from simple lesions to bifurcation lesions and chronic total occlusions (CTOs). I am proficient in using various imaging modalities such as intravascular ultrasound (IVUS) and optical coherence tomography (OCT) to guide stent placement and optimize outcomes.
I’m adept at pre-procedural planning, assessing lesion characteristics, selecting appropriate stent size and type, and meticulously deploying the stent to achieve optimal results. Post-stenting, I diligently evaluate the result angiographically and ensure proper stent expansion and apposition to the vessel wall. Furthermore, I am experienced in managing complications such as stent thrombosis or dissection.
For instance, in a recent case involving a complex CTO, the use of IVUS guided my approach, enabling successful revascularization. This approach helped to minimize trauma to the vessel wall and ensure optimal stent placement. Post procedure, we monitored the patient closely to manage potential risks like thrombus formation.
Q 17. Explain the role of the cath lab team and the responsibilities of each member.
The cath lab team functions as a highly coordinated unit. Each member plays a critical role in ensuring patient safety and procedural success.
- Cardiologist: Leads the procedure, interprets hemodynamic data, and makes crucial clinical decisions.
- Registered Nurse (RN): Monitors the patient’s vital signs, administers medications, assists with equipment, and maintains a sterile field.
- Cardiovascular Technologist (CVT): Operates the fluoroscopy unit, assists with catheter manipulation, manages equipment, and documents the procedure.
- Circulating Nurse: Prepares the room, maintains sterile supplies, monitors equipment functionality, and assists with patient care outside of the sterile field.
- Physician Assistant (PA) or Nurse Practitioner (NP): May assist with pre-procedure assessments, post-procedure care, and participate in the procedural aspects under the supervision of the cardiologist.
Effective communication and teamwork are essential. For instance, the CVT’s prompt identification of a potential equipment malfunction can prevent delays and mitigate risks. This rapid response by the team, demonstrates our commitment to patient care.
Q 18. Describe your experience with managing equipment malfunctions in the cath lab.
Managing equipment malfunctions is crucial in the cath lab. Our protocol emphasizes immediate action and systematic troubleshooting. The team is trained to identify the source of the malfunction quickly and implement appropriate solutions.
Examples include addressing power failures (using backup generators), managing fluoroscopy malfunctions (switching to alternative imaging modalities if necessary), or dealing with catheter or guidewire issues (having backup equipment readily available). We meticulously follow the manufacturer’s instructions for equipment maintenance and troubleshooting.
In one instance, a power surge caused a temporary loss of the fluoroscopy system. By quickly switching to backup power and utilizing the available backup equipment, we minimized the procedural delay and ensured patient safety. Documentation of such events is crucial for quality control and further preventative measures.
Q 19. How do you handle difficult or challenging patients in the cath lab?
Handling difficult patients requires patience, empathy, and effective communication. We use a combination of strategies, including clear and concise explanations of the procedure, addressing patient anxieties, and providing reassurance. For patients with complex medical histories or cognitive impairments, we might adjust our approach to accommodate their individual needs and ensure their comfort and understanding. We prioritize patient safety while maintaining a calm and professional demeanor.
For instance, a patient with severe anxiety might benefit from pre-procedural sedation and continuous reassurance during the procedure. If a patient is experiencing pain, we make prompt adjustments to provide appropriate analgesia. The key lies in open communication, individualized care, and a collaborative approach involving the patient’s family if appropriate.
Q 20. What are the common complications related to PCI (Percutaneous Coronary Intervention)?
PCI, while highly effective, carries potential complications. These can be categorized as:
- Vascular complications: Bleeding at the access site (hematoma, retroperitoneal hemorrhage), arterial dissection or perforation, pseudoaneurysm formation, arteriovenous fistula.
- Cardiac complications: Myocardial infarction (MI), coronary artery dissection or spasm, arrhythmias (bradycardia, tachycardia, ventricular fibrillation), stroke.
- Stent-related complications: Stent thrombosis (blood clot formation within the stent), in-stent restenosis (re-narrowing of the treated artery).
- Other complications: Contrast-induced nephropathy (kidney damage from contrast dye), allergic reactions to contrast dye, infection at the access site.
Minimizing these risks involves meticulous technique, proper patient selection, and appropriate post-procedural care, including antiplatelet therapy and close monitoring.
Q 21. Describe your experience with the use of intra-aortic balloon pumps (IABP).
My experience with intra-aortic balloon pumps (IABP) includes both pre- and post-PCI utilization. The IABP is a temporary circulatory support device used to improve cardiac output and myocardial perfusion in patients with severe heart failure. I’m proficient in IABP insertion and management, including monitoring the balloon inflation and deflation timing, and interpreting hemodynamic changes in response to IABP support.
We use IABPs selectively in patients with cardiogenic shock or severe left ventricular dysfunction who require temporary circulatory support. For example, in a patient with acute MI and cardiogenic shock, the IABP can temporarily augment cardiac output while awaiting definitive treatment. Monitoring IABP functioning involves observing the waveform, ensuring proper timing, and assessing the patient’s response to support. We carefully monitor for complications like leg ischemia, infection, and bleeding at the insertion site.
Q 22. Explain the principles of rotational atherectomy.
Rotational atherectomy is a minimally invasive procedure used to treat severely calcified coronary arteries. Imagine a clogged pipe – rotational atherectomy uses a small, diamond-coated burr attached to a catheter to mechanically break up the calcium deposits (the blockage) in the artery. This allows blood flow to be restored. The burr spins at high speed, effectively ‘grinding’ away the calcium, improving the ability of subsequent balloon angioplasty to expand the vessel. This technique is particularly beneficial for patients with heavily calcified lesions that are difficult to treat with conventional balloon angioplasty alone.
The principles revolve around the precise controlled abrasion of calcified plaque. The speed and pressure of the burr are carefully managed to minimize vessel damage. Post-procedure, a balloon angioplasty is typically performed to further optimize the artery’s diameter and ensure optimal blood flow.
Q 23. What is your experience with different types of closure devices?
My experience encompasses a wide range of vascular closure devices, from manual compression techniques to advanced automated systems. I’m proficient with collagen-based plugs, vascular suturing devices, and various types of mechanical closure devices. The choice of closure device is patient-specific, dependent on factors like access site size, anatomical considerations, and the patient’s overall health. For example, a patient with a history of bleeding disorders might require a more robust closure device like a suture-mediated closure system. Conversely, a younger, healthier patient with a smaller access site might be a candidate for a collagen plug. I meticulously assess each patient’s condition to select the most appropriate and safest closure technique. The use of these devices greatly reduces the risk of hematoma and helps achieve faster hemostasis, which ultimately leads to improved patient outcomes and shorter recovery times. I regularly evaluate the efficacy and safety profiles of newer closure technologies to ensure I’m utilizing the best available methods.
Q 24. Describe your familiarity with different types of imaging modalities used in the Cath Lab.
In the cath lab, we utilize various imaging modalities to visualize the coronary arteries and guide catheter manipulation. Fluoroscopy is the cornerstone of our imaging, providing real-time X-ray images. Intravascular ultrasound (IVUS) offers cross-sectional images of the artery’s lumen, allowing for precise assessment of plaque characteristics and the effectiveness of interventions. Optical coherence tomography (OCT) provides even higher resolution images, essentially showing us a microscopic view of the artery wall. We also employ pressure wire technology to measure pressure gradients within the coronary vessels, providing crucial information about the hemodynamic effects of lesions and the success of interventions. Choosing the right imaging modality depends on the clinical situation and the specific information required. For example, IVUS is crucial in assessing the extent of a lesion after rotational atherectomy while OCT provides the details about plaque composition.
Q 25. How do you ensure patient safety and comfort during a prolonged procedure?
Patient safety and comfort are paramount during prolonged procedures. We employ several strategies. First, we use meticulous sterile technique to minimize infection risk. We monitor vital signs closely throughout the procedure. Second, we utilize appropriate sedation and analgesia to keep the patient comfortable and minimize discomfort. Third, we maintain clear communication with the patient, explaining the process and answering any questions they have. Regular breaks for repositioning and adjusting the patient’s comfort levels are vital. For procedures requiring extended times, careful fluid management and temperature control are crucial, along with proactive measures to prevent complications such as hypotension or arrhythmias. Regularly checking for signs of discomfort or anxiety and adjusting the sedation protocol are key to ensure the patient is as comfortable as possible throughout the entire duration of the procedure. Our team’s focus is always on minimizing discomfort while ensuring the best clinical outcome.
Q 26. Describe your experience with documenting procedure details and patient outcomes.
Accurate and comprehensive documentation is a critical aspect of my work. I meticulously document all aspects of the procedure, including pre-procedural assessments, procedure steps, medications administered, imaging findings, complications (if any), and post-procedural assessments. The documentation adheres to standardized reporting formats and includes the use of standardized terminology and coding systems. We carefully record patient demographics, relevant medical history, procedural indications, device specifics, and post-procedure care instructions. Patient outcomes are tracked through follow-up appointments, where we review the patient’s progress, evaluate complications and provide any necessary additional care, all of which is meticulously recorded in the medical record. This rigorous documentation ensures continuity of care, facilitates quality control, and serves as a legal record of the procedure. Patient data is handled in accordance with all relevant regulations regarding privacy and confidentiality.
Q 27. What are the latest advancements in cardiac catheterization techniques and technology?
Cardiac catheterization is a rapidly evolving field. Recent advancements include the development of smaller, more flexible catheters, leading to reduced patient discomfort and complications. There have been significant improvements in imaging technology, such as fractional flow reserve (FFR) and instantaneous wave-free ratio (iFR) which enhance the ability to assess lesion significance. Transradial access (accessing the artery via the wrist instead of the groin) has gained significant traction, reducing access site complications. The introduction of bioabsorbable stents, which dissolve over time, represents a major advancement, eliminating the need for long-term presence of a foreign body. Finally, there’s ongoing research into new drug-eluting stents that deliver medication more effectively and with fewer side effects.
Q 28. How do you stay current with best practices and advancements in cardiac catheterization?
Staying current requires a multifaceted approach. I actively participate in continuing medical education (CME) activities, attending conferences, and workshops. I regularly review medical journals and publications related to interventional cardiology. Membership in professional organizations like the Society for Cardiovascular Angiography & Interventions (SCAI) provides access to the latest guidelines and research. I actively participate in case reviews and discussions with colleagues to share experiences and learn from others. Furthermore, I regularly assess and adopt new technologies and techniques within our laboratory, focusing on methods that are shown to improve patient outcomes and adhere to evidence-based guidelines.
Key Topics to Learn for Catheterization Laboratory Procedures Interview
- Cardiac Catheterization Techniques: Understanding various catheterization approaches (radial, femoral, etc.), including pre-procedure preparation, procedural steps, and post-procedure care.
- Hemodynamic Monitoring and Interpretation: Mastering the ability to interpret pressure waveforms, analyze hemodynamic data, and recognize abnormalities during procedures.
- Electrophysiology Studies: Familiarize yourself with the principles and techniques involved in EP studies, including mapping, ablation, and pacing.
- Angiography and Interventions: Gain a solid understanding of coronary angiography, angioplasty, stenting, and other interventional procedures, including troubleshooting common complications.
- Image Acquisition and Interpretation: Develop proficiency in interpreting fluoroscopic images, understanding image artifacts, and optimizing image quality for optimal procedural outcomes.
- Sterile Technique and Infection Control: Demonstrate a thorough understanding of maintaining a sterile field, proper hand hygiene, and infection control protocols within the catheterization lab.
- Emergency Management: Prepare to discuss your knowledge of managing various complications, such as bleeding, perforation, or allergic reactions, during and after procedures.
- Patient Safety and Communication: Highlight your understanding of patient assessment, communication skills, and the importance of teamwork in a high-pressure environment.
- Equipment and Technology: Demonstrate familiarity with the various types of equipment used in the cath lab, including monitors, catheters, and imaging systems.
- Regulatory Compliance and Documentation: Understand the importance of accurate documentation and adherence to regulatory guidelines and hospital policies.
Next Steps
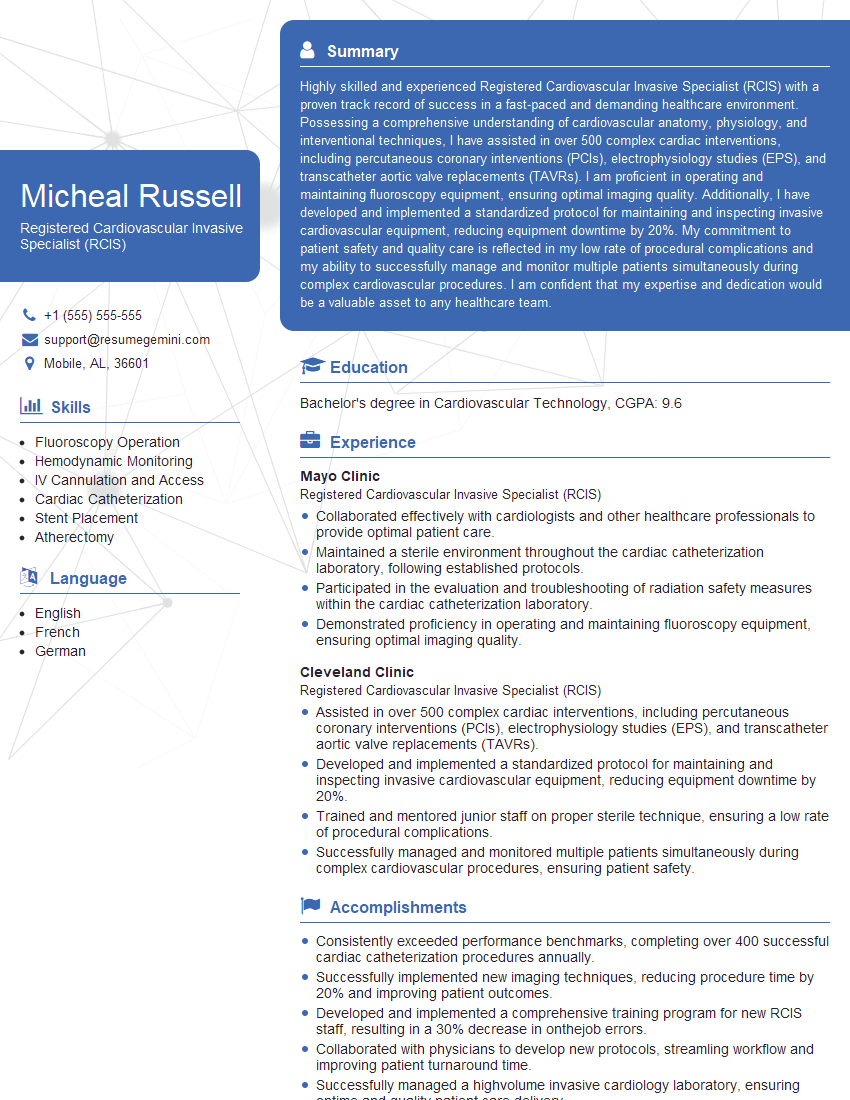
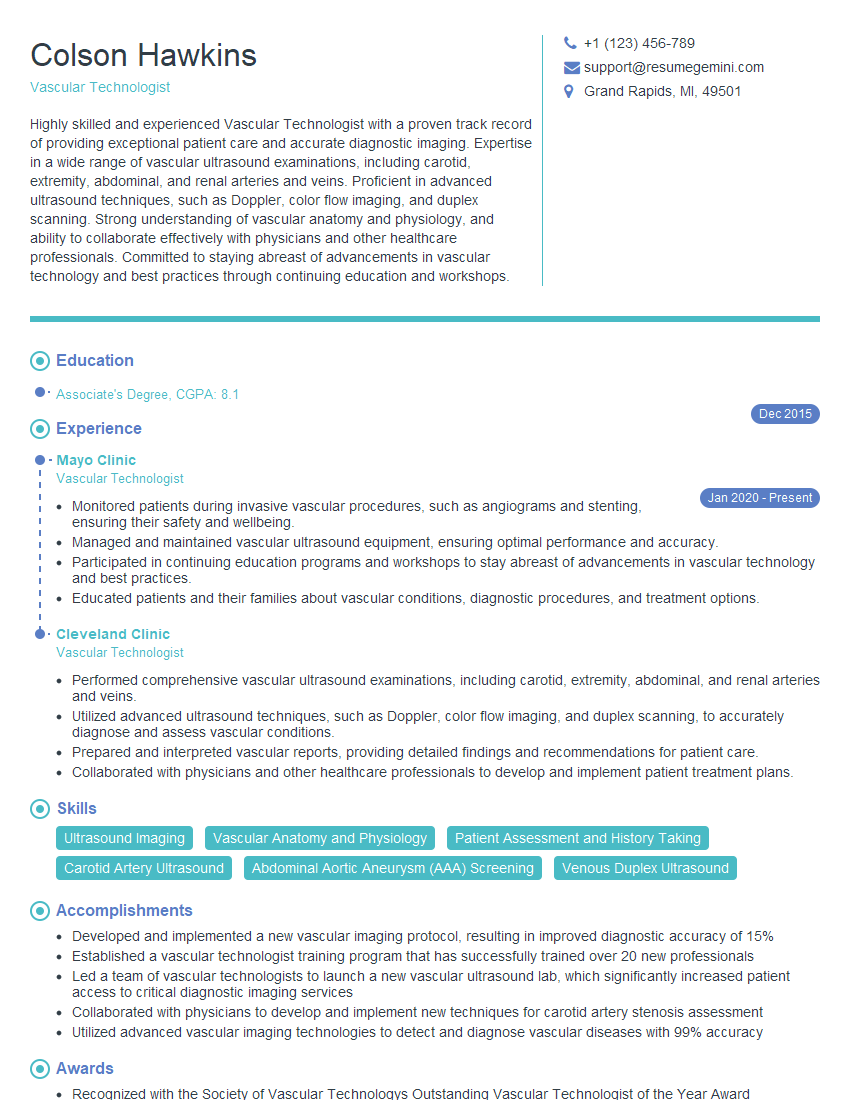
Mastering Catheterization Laboratory Procedures is crucial for a successful and rewarding career in interventional cardiology. A strong understanding of these procedures will significantly enhance your job prospects and open doors to exciting opportunities for growth and advancement. To increase your chances of landing your dream job, it’s essential to present your skills and experience effectively through a well-crafted, ATS-friendly resume. ResumeGemini is a trusted resource that can help you build a professional and impactful resume tailored to the specific requirements of Catheterization Laboratory positions. Examples of resumes tailored to Catheterization Laboratory Procedures are available to guide you through the process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.