Unlock your full potential by mastering the most common Celiac Plexus Blocks interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Celiac Plexus Blocks Interview
Q 1. Describe the anatomical landmarks used for a Celiac Plexus Block.
Identifying the correct anatomical landmarks is crucial for a successful and safe Celiac Plexus Block. The procedure relies on the relationship between the celiac artery, the celiac plexus, and surrounding structures. We primarily use the abdominal aorta as our central landmark. The celiac artery arises directly from the aorta, and the celiac plexus lies posterior to it. Other important landmarks include the superior mesenteric artery (SMA), which lies slightly inferior to the celiac artery, and the vertebral bodies, palpable through the posterior abdominal wall.
Imagine the aorta as a central highway. The celiac artery is a major off-ramp, and the celiac plexus is a small town nestled behind that off-ramp. We use palpable landmarks like the vertebral bodies and the relationship between the arteries to precisely locate the plexus. The location varies slightly between individuals, but a thorough understanding of the typical anatomical relationships is essential for accurate needle placement.
Q 2. What are the indications for a Celiac Plexus Block?
Celiac plexus blocks are primarily indicated for managing chronic abdominal pain, especially pain originating from pancreatic cancer, chronic pancreatitis, or other visceral sources. They can also be used for pain management in patients with mesenteric ischemia or intractable abdominal pain related to other malignancies. It’s important to note that this is a palliative procedure; it doesn’t treat the underlying cause but provides pain relief. The block temporarily interrupts nerve signals traveling to the brain, which reduces the perception of pain.
- Pancreatic cancer pain
- Chronic pancreatitis pain
- Other abdominal malignancies with intractable pain
- Mesenteric ischemia (in select cases)
Q 3. What are the contraindications for a Celiac Plexus Block?
Several contraindications exist for a Celiac Plexus Block. These can be broadly categorized into absolute and relative contraindications. Absolute contraindications, where the procedure should not be performed, include active bleeding disorders, severe infection at the injection site, patient refusal, and known allergy to the local anesthetic used. Relative contraindications, where the benefits must outweigh the risks, include uncontrolled hypertension, severe cardiac disease, respiratory compromise, and significant patient comorbidity.
A thorough pre-procedural assessment is essential to identify and address these contraindications. For example, if a patient has a significant bleeding disorder, alternative pain management strategies must be considered. Similarly, patients with severe respiratory compromise might need careful monitoring during the procedure. The decision to proceed with a celiac plexus block should always be made after a careful risk-benefit analysis.
Q 4. Explain the different approaches used for Celiac Plexus Blocks (e.g., anterior, posterior).
There are two primary approaches for performing a Celiac Plexus Block: the anterior and posterior approaches. The anterior approach involves inserting the needle through the abdominal wall, guided by fluoroscopy or ultrasound, to reach the celiac plexus from the front. This approach is less commonly used due to the higher risk of visceral injury. The posterior approach is the preferred method, as it involves accessing the celiac plexus from behind the abdomen, usually guided by fluoroscopy. The needle is advanced along the vertebral bodies to reach the area behind the aorta. The specific technique within each approach can vary according to the surgeon’s preference and the patient’s anatomy.
The choice between approaches depends largely on factors such as the surgeon’s expertise, patient anatomy, and available imaging. The posterior approach is generally favored for its reduced risk of visceral injury, but both approaches require a high degree of precision and anatomical knowledge.
Q 5. What imaging modalities are used to guide a Celiac Plexus Block?
Imaging plays a crucial role in guiding the needle placement and ensuring accurate delivery of the anesthetic. Fluoroscopy is the most commonly used imaging modality. It provides real-time visualization of the needle’s trajectory and its relationship to the celiac artery and aorta. Ultrasound guidance is an increasingly popular alternative, offering advantages in radiation reduction. Both methods allow for precise needle placement, minimizing the risk of complications.
Imagine trying to navigate a complex maze without a map. Fluoroscopy and ultrasound act like those crucial maps, allowing the physician to safely and effectively reach the target area. They visualize the anatomical structures and allow for adjustments during the procedure to ensure optimal placement of the needle.
Q 6. Describe the typical needle placement and trajectory during a Celiac Plexus Block.
Needle placement and trajectory are crucial aspects of a successful Celiac Plexus Block. During a posterior approach, which is most commonly used, the needle is inserted into the paravertebral space, usually at the level of the L1 vertebra. The needle is then advanced carefully, guided by fluoroscopy or ultrasound, towards the celiac artery. The aim is to deposit the local anesthetic in close proximity to the celiac plexus. The exact trajectory depends on individual patient anatomy but generally follows a path posterior to the aorta and anterior to the vertebral column. The precise needle placement is critical to ensure effective analgesia without causing damage to surrounding structures.
Think of it like carefully aiming an arrow. The target (celiac plexus) is small, and surrounding structures must be avoided. Fluoroscopy or ultrasound provides the essential guidance to hit the target accurately and safely.
Q 7. What local anesthetics are commonly used for a Celiac Plexus Block?
The choice of local anesthetic depends on various factors including patient-specific needs and physician preference. However, commonly used local anesthetics for a Celiac Plexus Block include lidocaine, bupivacaine, and ropivacaine. These are typically mixed with a steroid, such as dexamethasone, to prolong the analgesic effect. The concentration of the local anesthetic and the volume injected are adjusted according to the individual patient’s characteristics and the clinical context. Steroids are added to reduce the inflammatory response around the nerve roots, contributing to prolonged pain relief.
The selection is a balance between efficacy and safety. Bupivacaine, for example, offers longer-lasting analgesia, but lidocaine has a faster onset. The choice is tailored to achieve optimal pain relief with minimal side effects.
Q 8. What is the typical volume of local anesthetic used for a Celiac Plexus Block?
The volume of local anesthetic used in a celiac plexus block varies depending on several factors, including patient size, the specific technique used (anterior or posterior approach), and the clinician’s preference. However, a typical range would be between 20-40 mL. This volume is usually distributed across multiple injection sites to ensure optimal spread of the anesthetic around the celiac plexus. It’s crucial to remember that using excessive volume increases the risk of complications.
For example, a larger patient might require a slightly higher volume than a smaller one to achieve adequate spread. The concentration of the anesthetic also plays a role, with a higher concentration potentially requiring a smaller volume for the same effect. Always consult established guidelines and consider individual patient factors.
Q 9. How do you assess the effectiveness of a Celiac Plexus Block?
Assessing the effectiveness of a celiac plexus block primarily involves monitoring for pain relief in the target area, usually the abdomen. This can be subjective, relying on patient feedback, or objective, using pain scales. A successful block significantly reduces or eliminates pain associated with pancreatic cancer, chronic pancreatitis, or other visceral pain syndromes. Other indicators include a decrease in the need for analgesic medication and improvement in patient quality of life.
For instance, a patient reporting a significant decrease in their pain score from 8/10 to 2/10 after the block, combined with a reduction in opioid use, strongly suggests the procedure’s success. However, it’s important to remember that individual responses vary. Some patients may experience only partial relief, while others may have a complete resolution of their pain. Regular follow-up and careful documentation of the patient’s response are crucial.
Q 10. What are the potential complications of a Celiac Plexus Block?
Celiac plexus blocks, while generally safe, carry potential complications. These can be broadly categorized as vascular, neurological, or infectious. Vascular complications include hypotension (low blood pressure), retroperitoneal hematoma (bleeding), and rarely, arterial puncture. Neurological complications can include transient paresthesia (numbness or tingling), weakness, or even nerve damage. Infectious complications, though less common, include abscess formation or sepsis.
- Hypotension: This is a frequent complication due to the block’s effect on the sympathetic nervous system. It usually resolves with supportive measures.
- Pneumothorax: This is a rare but serious complication, particularly with the anterior approach, involving the accidental puncture of the lung.
- Retroperitoneal hematoma: This occurs when bleeding into the retroperitoneal space occurs from a vascular injury.
Careful patient selection, meticulous technique, and close monitoring are crucial in minimizing these risks. The use of fluoroscopy significantly improves the safety and efficacy of the procedure.
Q 11. How do you manage complications such as hypotension or pneumothorax during a Celiac Plexus Block?
Management of complications during a celiac plexus block requires immediate action. Hypotension is typically managed with intravenous fluids and, if necessary, vasopressors (medication to raise blood pressure). Close monitoring of vital signs is crucial. For a pneumothorax, supplemental oxygen and chest tube insertion might be necessary. Retroperitoneal hematomas are usually managed conservatively, with close monitoring for signs of worsening bleeding; occasionally, surgical intervention may be required.
For example, if a patient develops significant hypotension after the block, the procedure would be immediately halted. Intravenous fluids would be administered, and vital signs monitored closely. If the hypotension doesn’t respond, a vasopressor might be given. Similarly, if a pneumothorax is suspected, chest X-ray would be performed to confirm the diagnosis, followed by appropriate treatment, which may include chest tube placement.
Q 12. What are the post-procedure instructions for patients who undergo a Celiac Plexus Block?
Post-procedure instructions for patients who undergo a celiac plexus block are essential for ensuring a smooth recovery and minimizing complications. These typically include:
- Monitoring for pain relief: Patients are instructed to report any changes in their pain levels.
- Monitoring for complications: Patients should be aware of potential complications and instructed to seek immediate medical attention if they experience any significant bleeding, shortness of breath, or severe abdominal pain.
- Hydration: Adequate fluid intake helps prevent hypotension.
- Activity restrictions: Depending on the patient’s condition, activity may be restricted for a period.
- Medication: Patients may be prescribed pain medication to manage any residual pain.
- Follow-up appointments: Regular follow-up appointments are scheduled to monitor the block’s effectiveness and assess for any complications.
Clear and concise instructions, along with adequate patient education, are crucial for promoting a safe and successful outcome.
Q 13. Discuss the role of fluoroscopy in performing a Celiac Plexus Block.
Fluoroscopy plays a vital role in performing a celiac plexus block, significantly enhancing the safety and accuracy of the procedure. It provides real-time X-ray imaging, allowing the physician to visualize the needle’s position as it approaches the celiac plexus. This minimizes the risk of accidental puncture of major blood vessels or other critical structures. The use of contrast dye is often combined with fluoroscopy to confirm the precise location of the injection.
Without fluoroscopy, the procedure would be largely reliant on anatomical landmarks, which can be imprecise and may result in inadequate spread of the anesthetic or accidental injury. Fluoroscopy allows for precise needle placement, optimizing the block’s effectiveness while minimizing complications. It helps the practitioner to navigate safely through complex anatomical regions to ensure accurate delivery of the anesthetic to the celiac plexus.
Q 14. Explain the difference between a selective and a non-selective Celiac Plexus Block.
The difference between selective and non-selective celiac plexus blocks lies in the targeted area of the injection. A non-selective celiac plexus block aims to anesthetize the entire celiac plexus, affecting a broader area of innervation. This approach is simpler technically but can lead to more widespread effects, potentially causing more side effects. A selective celiac plexus block, on the other hand, targets specific branches of the celiac plexus, offering a more focused approach and potentially minimizing side effects.
Imagine targeting a specific area of a forest (selective), versus spraying the entire forest indiscriminately (non-selective). Selective blocks are preferred when a highly targeted approach is needed, often requiring specialized skills and advanced imaging techniques. They are used to reduce the risk of complications associated with more widespread anesthetic distribution, focusing on the specific nerves implicated in the pain rather than the entire plexus.
Q 15. How do you differentiate between technical failure and inadequate analgesia after a Celiac Plexus Block?
Differentiating between technical failure and inadequate analgesia after a celiac plexus block requires careful clinical assessment. Inadequate analgesia means the block worked technically, but the pain relief isn’t sufficient. This can be due to incomplete neurolytic effect, incomplete blockade of the celiac plexus branches, or the patient having a higher pain threshold than expected. Technical failure, on the other hand, means the block procedure itself didn’t go as planned. This might be due to needle misplacement, injection into an unintended location, or insufficient spread of the anesthetic/neurolytic agent.
We assess this by reviewing the procedure’s details: Did the needle reach the target area on fluoroscopy or ultrasound? Was the contrast media appropriately distributed? Did the patient experience any immediate or transient relief? Post-procedure pain scores and a comprehensive review of the patient’s medical history (including prior analgesic use and co-morbidities) are also crucial. We might consider repeat imaging to evaluate needle placement or further neurolytic procedures depending on our findings. If the block was technically successful but analgesia is insufficient, we will consider other pain management strategies including opioid supplementation, or other interventional techniques.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the advantages and disadvantages of different approaches to Celiac Plexus Blocks?
Celiac plexus blocks can be approached using several techniques, each with its own set of advantages and disadvantages. The two primary approaches are the antero-lateral and posterior approaches. The anterolateral approach, typically guided by fluoroscopy or ultrasound, involves needle insertion through the abdominal wall, aiming for the celiac plexus, usually using a less invasive technique. The posterior approach is generally performed under fluoroscopic guidance. It involves inserting the needle through the retroperitoneum under more direct vision. It sometimes requires a longer and more arduous trajectory that increases the chance of causing complications.
- Anterolateral Approach (fluoroscopy or ultrasound guided): Advantages include a less invasive procedure, shorter needle trajectory, and lower risk of pneumothorax. Disadvantages include the potential for vascular injury and difficulty visualizing the plexus as compared to the posterior approach.
- Posterior Approach (fluoroscopy guided): Advantages include better visualization of the celiac plexus and less chance of vascular puncture. Disadvantages include a more invasive procedure, longer needle trajectory, higher risk of pneumothorax or other organ injuries, and usually requires a longer patient recovery time.
The choice of approach depends on patient-specific factors (body habitus, previous surgeries), physician expertise, and available imaging technology. A careful risk-benefit analysis is crucial in selecting the best approach for each individual.
Q 17. Describe the role of ultrasound guidance in Celiac Plexus Blocks.
Ultrasound guidance has revolutionized celiac plexus blocks. It provides real-time visualization of anatomical structures, allowing for precise needle placement and minimizing the risk of complications. This is particularly helpful in the anterolateral approach. With ultrasound, we can clearly see the aorta, celiac artery, and surrounding structures, guiding the needle to the target with high accuracy. We can also visualize the spread of the injected contrast media, confirming the position and extent of the anesthetic/neurolytic effect.
Using ultrasound significantly improves the success rate, reduces the number of needle passes, and minimizes the incidence of complications, such as vascular puncture. Unlike fluoroscopy, which exposes patients to ionizing radiation, ultrasound is a non-ionizing imaging technique, making it safer in the long run. It is a safe, non-invasive, and cost-effective technique for performing celiac plexus blocks. In my practice, ultrasound is the preferred imaging modality for this procedure.
Q 18. How do you prepare a patient for a Celiac Plexus Block?
Preparing a patient for a celiac plexus block involves several key steps. This starts with a thorough discussion about the procedure, potential benefits, risks, and alternatives during the informed consent process. This includes discussing the possibility of an ineffective procedure as well as potential complications. The patient needs to be NPO (nothing by mouth) for at least 6 hours prior to the procedure to reduce the risk of aspiration. Pre-procedure laboratory tests (such as a complete blood count and coagulation profile) are important to rule out any contraindications and asses the patient’s overall health status. A venous line is typically placed to administer fluids and medication during the procedure. Prophylactic antibiotics are often considered, especially in patients with a history of infection or immunosuppression. The patient’s vital signs (blood pressure, heart rate, oxygen saturation) are continuously monitored. A pre-procedure analgesic dose can be given to minimize any anxiety
Q 19. What are the common side effects of a Celiac Plexus Block?
Common side effects of a celiac plexus block can range from mild to severe. Mild side effects include transient hypotension, nausea, and vomiting, often easily managed with supportive care. More serious complications, though less common, include retroperitoneal hematoma, injury to adjacent organs (such as the aorta, kidney, or pancreas), pneumothorax, and infection. Post-procedure pain at the injection site is also possible. These serious complications are managed depending on the severity; for example, a retroperitoneal hematoma might require surgical intervention, while pneumothorax requires chest tube placement. All patients are carefully monitored after the procedure for the occurrence and potential management of such complications.
Q 20. How would you manage a patient who experiences severe pain despite a Celiac Plexus Block?
Managing a patient experiencing severe pain despite a celiac plexus block requires a multi-modal approach. First, we reassess the procedure’s technical success through imaging (if needed) to rule out any technical issues. If the block was technically sound, we need to explore other potential pain sources: is the pain visceral or somatic in nature? Are there other contributing factors to the patient’s pain that the block might not have addressed? Second, we’d explore alternative pain management strategies such as adjusting the analgesic regimen (including opioids and adjuvant analgesics), considering other interventional procedures (e.g., a repeat celiac plexus block with a different approach, or a different interventional pain management strategy), or even referral to a pain management specialist. We’d need to evaluate the psychological aspects of the patient’s pain and address them with counseling, medication or other interventional strategies as needed.
Q 21. Describe the steps involved in obtaining informed consent for a Celiac Plexus Block.
Obtaining informed consent for a celiac plexus block is a crucial step that ensures patient autonomy and understanding. The process starts with a detailed explanation of the procedure, including its purpose, benefits, risks, and alternatives. This explanation should be clear, concise, and tailored to the patient’s understanding. We use lay terms avoiding medical jargon as much as possible. This conversation should allow the patient time to fully process the information. Potential complications are discussed in detail. The physician should make sure that the patient has had all their questions answered before proceeding. It’s essential to document the informed consent process completely, including who provided the explanation, the date, and the patient’s affirmation that they understand. If the patient is not competent to consent, appropriate legal authorities need to be engaged to obtain proper consent, typically a surrogate or family member.
Q 22. What is the role of opioids in conjunction with Celiac Plexus Blocks?
Opioids play a crucial role in Celiac Plexus Blocks (CPBs) primarily for analgesia, managing pain both during and after the procedure. We typically use them as part of a multi-modal analgesic approach. This means combining opioids with other pain-relieving medications, such as local anesthetics, NSAIDs, or even gabapentinoids, to achieve superior pain control with reduced side effects and lower opioid dosages. For example, a common approach might involve fentanyl or morphine administered intravenously before, during, and after the CPB. The specific opioid, dose, and route of administration are tailored to the individual patient’s needs and tolerance, always considering the risk of respiratory depression and other opioid-related adverse events.
The choice of opioid is influenced by several factors: the patient’s medical history (including allergies and potential drug interactions), the anticipated duration of pain relief needed, and the risk profile of the patient for respiratory complications. Post-procedurally, we carefully monitor patients for signs of respiratory depression, sedation, nausea, and vomiting. We titrate opioid doses as needed based on patient response and vital signs, ensuring adequate pain control while minimizing adverse effects. Ultimately, the goal is to provide effective pain management while maintaining patient safety and comfort.
Q 23. Discuss the use of neurolytic agents in Celiac Plexus Blocks.
Neurolytic agents are used in CPBs to achieve longer-lasting pain relief, often in cases of chronic, intractable abdominal pain unresponsive to other treatments. Unlike local anesthetics which provide temporary pain relief, neurolytic agents permanently damage or destroy nerve fibers, thus interrupting pain signals to the brain. This isn’t a first-line approach because of the irreversibility of the nerve damage. We only consider neurolysis in very select patients who have failed less invasive strategies and are experiencing severe, debilitating pain that significantly impacts their quality of life.
Common neurolytic agents include alcohol and phenol. The procedure is more complex and requires meticulous technique to avoid unintended nerve damage to adjacent structures. Pre-procedural imaging, such as fluoroscopy, is essential to ensure precise placement of the agent. Post-neurolysis, patients can experience a prolonged period of pain relief, but there is also a higher risk of complications, such as bowel dysfunction, which we thoroughly discuss with the patient prior to the procedure.
A key consideration in using neurolytic agents is the potential for incomplete blockade or even unintended effects. That’s why a thorough discussion of risks and benefits is crucial, emphasizing the irreversible nature of the procedure.
Q 24. How do you monitor patients after a Celiac Plexus Block?
Post-CPB monitoring is a critical aspect of patient care. It’s crucial to assess multiple factors to detect early warning signs of complications. We usually start by continuously monitoring vital signs (heart rate, blood pressure, respiratory rate, oxygen saturation) for at least 4-6 hours post-procedure. We carefully observe for signs of hypotension, respiratory depression (especially if opioids were used), and signs of infection at the puncture site. Patients are closely monitored for any signs of bowel dysfunction such as nausea, vomiting, paralytic ileus, or changes in bowel habits. We assess for pain levels regularly using validated pain scales and adjust pain management accordingly. Post-procedural imaging (such as a CT scan) might be considered in some cases, especially if there’s a suspicion of complications.
The duration of monitoring depends on several factors, including the patient’s overall health, the type of block (neurolytic vs. non-neurolytic), and the response to the procedure. Patients are usually discharged only when they are hemodynamically stable, pain is well-controlled, and bowel function has returned to baseline. They receive detailed post-procedure instructions, including dietary advice and instructions on reporting any concerning symptoms.
Q 25. What are the long-term outcomes associated with Celiac Plexus Blocks?
Long-term outcomes following CPBs are highly variable and depend on various factors, including the underlying condition, the type of block performed, and the individual patient response. For example, in patients with chronic pancreatitis, a successful CPB can significantly improve pain scores and quality of life for several months to even years, potentially reducing the need for opioid analgesics. However, the effect isn’t permanent in many cases. Some patients may experience a gradual return of pain over time and require repeat blocks or other interventional procedures.
Possible long-term complications include bowel dysfunction (constipation, diarrhea, or paralytic ileus), which can be significant, especially after neurolytic CPBs. Other rare but serious complications include retroperitoneal hematoma, infection, and injury to adjacent nerves or organs. The duration of pain relief after a CPB is unpredictable and can vary from weeks to years. It’s important to manage patient expectations about the long-term effects.
Q 26. How do you document a Celiac Plexus Block procedure?
Documentation of a CPB procedure is crucial for ensuring accurate medical record keeping and facilitating continuity of care. The documentation should be comprehensive and should include the following information:
- Patient demographics and medical history: including relevant co-morbidities.
- Indication for the procedure: clearly stating the reason for performing the CPB.
- Pre-procedure assessment: including vital signs, pain assessment, and any allergies.
- Procedure details: including the approach (e.g., anterior vs. posterior), the type of needle used, the volume and type of anesthetic/neurolytic agent injected, the fluoroscopy images, and any complications encountered.
- Post-procedure assessment: including vital signs, pain assessment, and any observed complications.
- Medication administered: including dosages and routes of administration.
- Patient education and discharge instructions: indicating what was discussed with the patient and the plan of care.
Accurate and detailed documentation is essential for quality assurance, medico-legal reasons, and for future management of the patient.
Q 27. Describe your experience with different types of needles used in Celiac Plexus Blocks.
The choice of needle for a CPB is crucial for achieving successful and safe placement, minimizing complications. We typically use a variety of needles depending on the approach and the specific anatomy of the patient. These include:
- 22-gauge or 25-gauge Chiba needles: These are often used for anterior approaches. Their smaller diameter reduces the risk of vascular injury.
- Longer, stiffer needles: For posterior approaches, longer needles with a stiffer shaft are often preferred to facilitate navigation through the tissues.
The needle choice also depends on the experience of the interventionalist and the preference of the physician. I personally have experience using both types and adjust my approach based on each patient’s individual anatomy and the specifics of their case. It is vital to ensure appropriate needle length to reach the celiac plexus without causing damage to nearby organs. Fluoroscopy is invaluable in visualizing needle placement and ensuring the accuracy of the injection.
Q 28. What are some alternative techniques to Celiac Plexus Blocks for similar indications?
Several alternative techniques exist for managing chronic abdominal pain, offering different approaches depending on the underlying cause and patient factors. These include:
- Radiofrequency ablation (RFA): This technique uses heat to destroy nerve tissue, providing pain relief in a more targeted manner than neurolytic CPBs. It allows for greater precision in targeting the specific nerves responsible for the pain.
- Spinal cord stimulation (SCS): This involves implanting a device that delivers electrical impulses to the spinal cord, interrupting pain signals. It’s a less invasive option compared to CPB but might not be effective for all types of abdominal pain.
- Medications: Various pharmacological strategies such as opioids, NSAIDs, gabapentinoids, and antidepressants play a critical role in pain management. These may be used alone or in conjunction with other interventions.
- Surgical interventions: In selected cases, surgery may be indicated to address the underlying cause of the pain, such as repairing an abdominal injury or removing a diseased organ.
The choice of alternative technique depends on the specific characteristics of the patient’s pain, their medical history, and the potential benefits and risks of each intervention. A multidisciplinary approach, involving gastroenterologists, pain specialists, and surgeons, is often most effective.
Key Topics to Learn for Celiac Plexus Blocks Interview
- Anatomy and Physiology: Thorough understanding of the celiac plexus, its branches, and its relationship to surrounding structures. This includes the location, innervation, and function of the celiac plexus.
- Indications for Celiac Plexus Block: Mastering the specific clinical scenarios where a celiac plexus block is indicated, including pancreatitis, cancer pain, and other visceral pain conditions. Consider the advantages and disadvantages compared to other pain management techniques.
- Procedure Technique: Detailed knowledge of the different approaches (e.g., anterior, posterior) used to perform a celiac plexus block. Understand the imaging guidance techniques (fluoroscopy, ultrasound) and the role of the interventionalist.
- Anesthesia and Pharmacology: Familiarity with the anesthetic agents and adjuvants commonly used in celiac plexus blocks. Understand the mechanisms of action and potential complications related to the choice of medications.
- Complications and Management: Be prepared to discuss potential complications, such as bleeding, infection, and nerve injury. Understand the preventative measures and management strategies for these complications.
- Post-Procedure Care: Outline the necessary post-procedure monitoring and instructions for patients undergoing a celiac plexus block, including pain management and potential side effects.
- Case Studies and Problem-Solving: Prepare to discuss real-world case studies and demonstrate your ability to troubleshoot common challenges encountered during the procedure and post-procedure care.
Next Steps
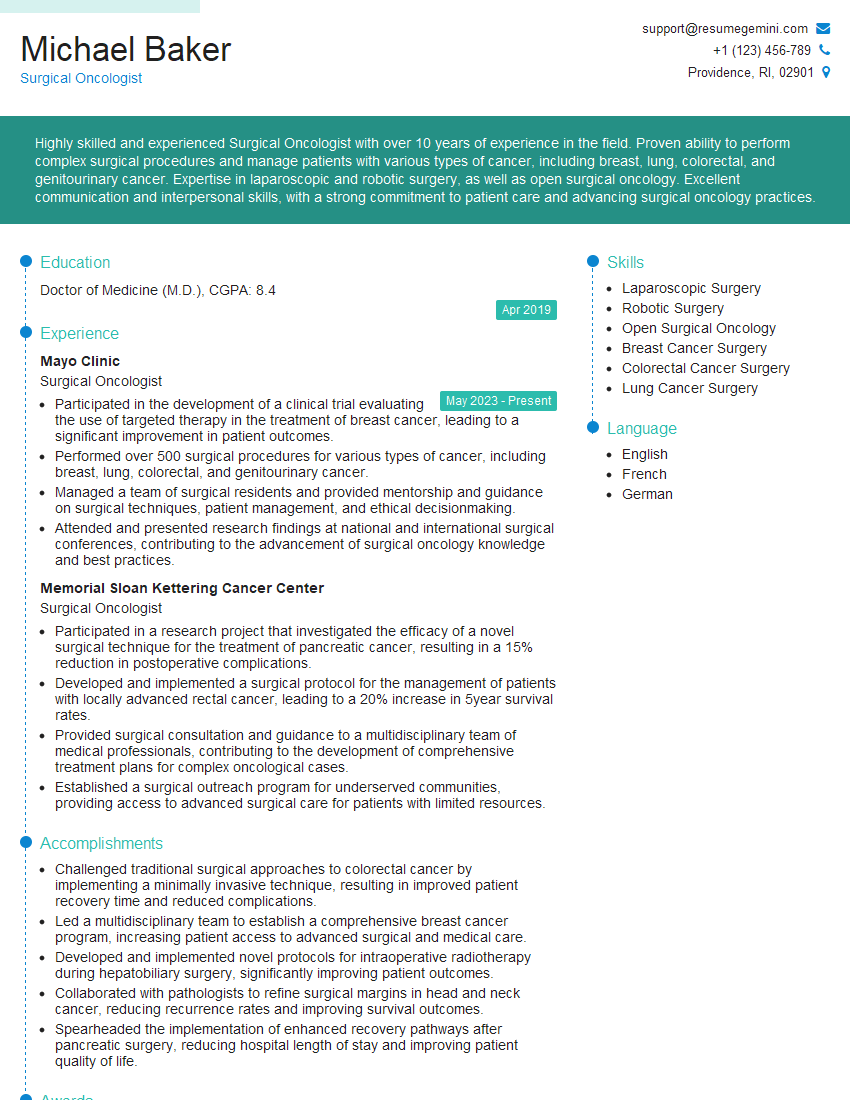
Mastering Celiac Plexus Blocks demonstrates a high level of expertise in interventional pain management, significantly enhancing your career prospects in anesthesiology, radiology, or pain medicine. To maximize your job search success, a strong, ATS-friendly resume is crucial. ResumeGemini is a trusted resource that can help you craft a professional and impactful resume that highlights your skills and experience. ResumeGemini provides examples of resumes tailored to Celiac Plexus Blocks and interventional pain management to guide you through the process. Take the next step towards your dream career – build a winning resume today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.