Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Central Line Care interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Central Line Care Interview
Q 1. Describe the steps involved in inserting a central venous catheter.
Central venous catheter (CVC) insertion is a sterile procedure requiring meticulous technique to minimize complications. It typically involves these steps:
- Patient Preparation: This includes confirming the need for a CVC, obtaining informed consent, assessing the patient’s coagulation status, and performing skin antisepsis using chlorhexidine gluconate.
- Site Selection and Preparation: The appropriate site (internal jugular, subclavian, or femoral vein) is selected based on patient factors and procedural feasibility. The skin is meticulously prepared with an antiseptic solution.
- Local Anesthesia: Lidocaine is injected subcutaneously to numb the insertion site, enhancing patient comfort.
- Catheter Insertion: Using sterile technique, a needle is advanced into the chosen vein under ultrasound guidance (highly recommended) or anatomical landmarks. The catheter is then threaded over a guidewire into the superior vena cava.
- Catheter Fixation and Dressing: Once the catheter is in the optimal position (confirmed by chest x-ray), it is secured to the skin with sutures or a securement device. A sterile dressing is applied.
- Confirmation of Placement: A chest x-ray is essential to verify the catheter tip’s location and rule out pneumothorax or other complications.
- Post-Insertion Care: Initial assessment includes checking for bleeding, hematoma formation, and signs of infection. The insertion site is monitored closely.
Each step demands precision and adherence to sterile technique. A deviation from protocol can significantly increase the risk of complications.
Q 2. What are the different types of central venous catheters and their indications?
Various CVC types cater to different clinical needs. These include:
- Peripherally Inserted Central Catheters (PICCs): Inserted into a peripheral vein and advanced to the central venous system. Ideal for medium-term access (weeks to months).
- Central Venous Catheters (CVCs) placed via the internal jugular, subclavian, or femoral vein: Offers more immediate and larger bore access for rapid fluid administration and hemodynamic monitoring.
- Tunneled Catheters: The catheter is surgically tunneled under the skin to the insertion site, reducing the risk of infection for long-term use (months to years).
- Implantable Ports: Completely implanted under the skin with a subcutaneous port accessed via a needle puncture. Ideal for long-term chemotherapy administration or repeated blood draws.
Indications vary depending on the catheter type. PICCs are commonly used for administering antibiotics or chemotherapy. Internal jugular and subclavian CVCs are preferred for emergency situations requiring rapid fluid resuscitation or hemodynamic monitoring. Tunneled catheters and implantable ports are suitable for long-term therapy avoiding repeated needle sticks.
Q 3. Explain the process of selecting the appropriate site for central line insertion.
Site selection for CVC insertion is crucial. The choice depends on various factors, including:
- Patient Anatomy: Consider anatomical landmarks, body habitus, and the presence of any pre-existing conditions like neck masses or distorted anatomy.
- Clinical Need: The intended use of the CVC influences site selection. For example, frequent blood sampling may favor a more accessible site like the femoral vein.
- Risk of Complications: Internal jugular insertion generally carries a lower risk of pneumothorax compared to subclavian insertion. Femoral vein insertion has a higher risk of infection.
- Operator Experience: The physician’s comfort and experience with different insertion techniques significantly impact site selection.
Example: In a critically ill patient requiring immediate fluid resuscitation, the internal jugular vein might be the preferred site if accessible and anatomical landmarks are clear. In contrast, a patient needing long-term chemotherapy might benefit from an implantable port.
Q 4. How do you prevent catheter-related bloodstream infections (CRBSIs)?
Preventing catheter-related bloodstream infections (CRBSIs) is paramount. Strategies include:
- Strict Sterile Technique: Meticulous adherence to aseptic practices during insertion and dressing changes is critical. This includes proper hand hygiene, use of sterile gloves and drapes, and disinfection of the skin with chlorhexidine gluconate.
- Optimal Catheter Site Selection: Choosing a site with a lower risk of infection is vital (e.g., internal jugular over femoral).
- Appropriate Catheter Selection: Selecting the catheter with the smallest possible lumen diameter that meets clinical needs minimizes the risk of infection.
- Daily Chlorhexidine Bathing: Regular chlorhexidine skin cleansing around the catheter insertion site significantly reduces microbial colonization.
- Prompt Removal of Catheters: Once the clinical need for the CVC has been met, it should be promptly removed.
- Use of Impervious Dressings: Impervious dressings provide a barrier against microorganisms.
- Proper Catheter Securement: Secure the catheter appropriately to prevent accidental dislodgment and reduce the chance of skin irritation and infection.
Example: A hospital might implement a standardized checklist for CVC insertion and care to reduce CRBSIs, including requirements for chlorhexidine skin antisepsis and daily assessment of the insertion site.
Q 5. What are the common complications associated with central lines, and how are they managed?
Central lines, while life-saving, carry potential complications:
- Catheter-Related Bloodstream Infections (CRBSIs): The most serious complication, requiring prompt treatment with antibiotics. Prevention strategies are crucial.
- Pneumothorax: Air entering the pleural space during insertion, particularly with subclavian vein access. Requires chest tube insertion.
- Hemothorax: Blood in the pleural space, also requiring chest tube insertion.
- Thrombosis: Formation of blood clots in the vein, requiring anticoagulation therapy.
- Air Embolism: Air entering the bloodstream, potentially leading to cardiac arrest. Immediate treatment is vital.
- Catheter Malposition: The catheter is not in the ideal location, requiring repositioning or removal.
- Mechanical Complications: Catheter breakage or kinking may lead to complications requiring prompt removal.
Management depends on the complication. CRBSIs require intravenous antibiotics, while pneumothorax or hemothorax requires chest tube drainage. Thrombosis might necessitate anticoagulation therapy. Catheter malposition or mechanical complications often require catheter removal and potential reinsertion.
Q 6. Describe your experience with different types of dressing changes for central lines.
Dressing changes for central lines are crucial to maintaining sterility and preventing infections. I have experience with several types:
- Transparent Dressings: Allow for visualization of the insertion site, reducing the need for frequent dressing changes. Examples include Tegaderm or OpSite.
- Gauze Dressings: Less expensive but require more frequent changes and don’t allow for visualization. These require careful technique to maintain a sterile field.
- Impervious Dressings: Offer a barrier to microorganisms. These dressings are especially important for higher-risk patients or during periods of higher infection risk.
The choice of dressing depends on patient-specific factors, including the risk of infection, the patient’s overall condition, and the type of catheter used. Proper technique is paramount for all dressing changes, and I always ensure careful hand hygiene, the use of sterile gloves, and the maintenance of a sterile field.
Example: In a patient with a compromised immune system, I’d use an impervious dressing to minimize the risk of infection.
Q 7. How do you troubleshoot a malfunctioning central line?
Troubleshooting a malfunctioning central line involves a systematic approach:
- Assess the Problem: Determine the nature of the malfunction (e.g., no blood return, difficulty flushing, catheter dislodgement).
- Check for Obstruction: Attempt to flush the catheter with a heparinized saline solution. If unsuccessful, consider using a thrombolytic agent (under appropriate circumstances and with physician consultation).
- Assess Catheter Position: Consider obtaining a chest x-ray to confirm proper catheter placement and rule out complications like migration or kinking.
- Inspect the Catheter and Dressing: Check for signs of infection, leakage, or damage to the catheter or dressing.
- Consider Underlying Conditions: Evaluate patient factors that might contribute to the malfunction (e.g., thrombosis or dehydration).
- Consult with Physician: If the problem persists despite troubleshooting attempts, consult with a physician to determine appropriate management, which may include catheter removal and reinsertion.
Example: If a central line is not flushing easily, I’d first attempt to flush it with heparinized saline. If unsuccessful, I’d consult the physician and request a chest X-ray to rule out a thrombus or other mechanical issues.
Q 8. Explain the importance of proper flushing techniques for central lines.
Proper flushing techniques for central lines are paramount to maintaining their patency and preventing complications like thrombosis and infection. Think of a central line as a delicate highway; regular flushing keeps the ‘traffic’ (blood and fluids) flowing smoothly. We use aseptic technique throughout the process.
The process typically involves using a prescribed flush solution (often heparinized saline or saline alone, depending on institutional protocols and the type of central line) and injecting it using a gentle, controlled push. The volume and type of flush solution are critical, and these parameters are usually dictated by the institution’s protocols and the specific catheter involved. For example, smaller lumen catheters may require a lower volume flush than larger ones to prevent pressure-induced complications. We avoid forceful flushing as it can damage the catheter or introduce air emboli into the bloodstream. Post-flush, we ensure no blood returns to the syringe, demonstrating successful clearance of the lumen. The entire process must be documented meticulously.
- Type of flush solution: Heparinized saline is common to prevent clotting, but saline alone might be used in certain situations (e.g., patients with heparin allergies). The choice depends on institutional guidelines and the patient’s specific needs.
- Flush volume: This is carefully determined to avoid exceeding the pressure limits of the catheter, reducing the risk of damage.
- Frequency of flushing: Flushing is performed regularly, the frequency varying depending on the line’s use and institutional guidelines. It’s usually done after medication administration and before discontinuation of the line.
Q 9. What are the indications for removing a central line?
Indications for central line removal are multifaceted and hinge on the patient’s clinical status and the catheter’s purpose. Essentially, once the need for venous access via the central line has passed, it should be removed. This principle aims to minimize the inherent risks associated with maintaining a central venous catheter, primarily infection.
- Completion of treatment: Once the intravenous therapy, parenteral nutrition, or other interventions requiring central venous access are complete, the line should be removed immediately.
- Development of infection: Any signs or symptoms of infection, such as redness, swelling, purulent drainage, or fever, necessitate immediate removal.
- Mechanical complications: Thrombosis, catheter malfunction (e.g., breakage, displacement), or kinking of the catheter are reasons for removal.
- Patient’s readiness for discharge: In anticipation of discharge, if the patient no longer requires central venous access, the line is removed to decrease the risk of infection or complications at home.
- Planned surgery: In some cases, central lines may need to be removed before specific surgeries.
The decision to remove a central line is never taken lightly and should be done by a skilled healthcare provider.
Q 10. Describe the procedure for removing a central line.
Central line removal is a procedure requiring meticulous aseptic technique to prevent infection. Imagine it like carefully detaching a very delicate and important wire. It requires precision and gentleness. Before removal, we confirm the order, check the patient’s identification, and ensure appropriate supplies are available.
- Preparation: Gather all necessary supplies: sterile gloves, gown, drapes, antiseptic solution, gauze pads, occlusive dressing, sharps container, and the removal kit (including the appropriate dressing).
- Assessment: Verify the correct line is being removed, check for any signs of infection or complications, assess the patient for any concerns.
- Antiseptic preparation: Thoroughly clean the insertion site with antiseptic solution using a concentric circular motion.
- Removal: Gently pull the catheter out in a smooth motion while maintaining tension, using the designated removal kit to ensure smooth, controlled extraction.
- Pressure: Firm but gentle pressure should be applied to the insertion site after removal with a sterile gauze pad to prevent bleeding and hematoma formation.
- Dressing: Once hemostasis is achieved, apply a sterile occlusive dressing, making sure that it’s securely attached.
- Disposal: Dispose of the catheter and other used supplies properly.
- Post-removal assessment: Regularly monitor the site for bleeding, hematoma formation, infection, or any other complications.
The entire process should be documented carefully. Post-removal monitoring is equally important.
Q 11. How do you assess the patency of a central line?
Assessing central line patency is crucial for ensuring that the line is functioning correctly and that medications and fluids can be delivered effectively. It’s like checking if a road is open and clear for traffic.
- Visual inspection: Observe for any signs of obstruction, kinks, or damage in the catheter or tubing. Blood return should be assessed at the time of insertion and before administration of medication.
- Aspiration of blood: Gently aspirate blood to check for flashback. The presence of blood indicates that the catheter is in the vessel. The absence may indicate dislodgement or obstruction. Remember that aspirating for blood return isn’t a definite indicator of patency in all cases, especially with lines that don’t routinely have blood return.
- Flush test: As discussed earlier, attempting a saline or heparinized saline flush can help assess patency. If there is resistance to flushing, this could indicate clotting or obstruction.
- Measurement of pressure: Some central lines allow for pressure measurement. High pressures suggest obstruction.
- Confirmation via imaging: If there is doubt about patency, imaging techniques (e.g., chest x-ray) might be used for confirmation.
The exact method of assessing patency may vary depending on the type of central venous catheter.
Q 12. What are the signs and symptoms of a central line infection?
Central line-associated bloodstream infections (CLABSIs) are serious and potentially life-threatening complications. Recognizing the signs and symptoms early is crucial for prompt treatment and improving patient outcomes.
- Local signs: Erythema (redness), swelling, tenderness, warmth, and purulent drainage at the insertion site are common local indicators.
- Systemic signs: Fever (often >100.4°F or 38°C), chills, hypotension, tachycardia, and altered mental status are common systemic manifestations.
- Laboratory findings: Positive blood cultures, elevated white blood cell count (leukocytosis), and increased inflammatory markers (e.g., C-reactive protein) often support the diagnosis.
It’s important to remember that CLABSIs can present subtly, so a high index of suspicion is necessary. Any suspicion should prompt immediate investigation, including blood cultures and assessment of the insertion site.
Q 13. What are the key elements of a central line care bundle?
A central line care bundle is a set of evidence-based best practices aimed at minimizing the risk of CLABSIs. These bundles are crucial in preventing these serious infections. It’s like having a multi-layered security system to safeguard the central line.
- Hand hygiene: Meticulous hand hygiene before and after any interaction with the central line is paramount.
- Chlorhexidine skin antisepsis: Using chlorhexidine gluconate for skin preparation before insertion significantly reduces the risk of infection.
- Maximal barrier precautions during insertion: Using a sterile gown, gloves, mask, and full drapes during insertion minimizes contamination.
- Optimal catheter site selection: Choosing appropriate insertion sites reduces the likelihood of contamination and complications.
- Daily review of line necessity: Regularly evaluating the need for the line ensures removal when it’s no longer necessary, reducing exposure time.
- Proper flushing and maintenance: Implementing consistent flushing protocols as discussed earlier is vital.
- Use of appropriate dressings: Using sterile, transparent dressings facilitates monitoring of the insertion site.
Adherence to these elements is critical to patient safety.
Q 14. Describe your experience with using ultrasound guidance for central line insertion.
Ultrasound guidance for central line insertion is a valuable technique that improves the success rate, reduces complications, and minimizes the number of attempts needed. It’s like having a map to navigate through the body’s vascular system, increasing accuracy and precision. I have extensive experience utilizing ultrasound during central line placement in a variety of clinical settings.
Ultrasound allows real-time visualization of the vessels, allowing precise needle placement into the target vein, minimizing the risk of arterial puncture, pneumothorax (lung collapse), or other complications associated with blind insertion. I am proficient in identifying the internal jugular vein, subclavian vein, and femoral vein using ultrasound guidance and placing catheters successfully using different approaches (e.g., Seldinger technique). This has led to reduced procedure time, fewer complications, and improved patient outcomes. The enhanced visualization also helps me avoid anatomical variations, improving the safety of the procedure. Post-insertion ultrasound confirmation helps to ensure the catheter’s correct placement before use.
During the procedure, I carefully assess the patient, obtain informed consent, prepare the insertion site with antiseptic solution, apply sterile drapes, and use aseptic technique meticulously. Then, I use the ultrasound to visualize the target vessel, guide the needle insertion, and confirm successful catheter placement. Post-procedure, I carefully secure the catheter, document the procedure thoroughly, and follow post-insertion care protocols. My skills in ultrasound-guided central line insertion have improved patient care and safety significantly over the years.
Q 15. How do you educate patients and families about central line care?
Educating patients and their families about central line care is crucial for ensuring successful treatment and preventing complications. My approach involves a multi-faceted strategy focusing on clear, concise communication tailored to the individual’s understanding. I begin by explaining, in simple terms, what a central line is, why it’s necessary for their treatment, and its potential benefits. I then thoroughly detail the care required, including:
- Hand hygiene: Emphasizing the importance of frequent and thorough handwashing before and after touching the line or dressing.
- Dressing changes: Explaining the frequency of dressing changes and the sterile technique used.
- Signs and symptoms of infection: Describing potential signs (redness, swelling, drainage) and instructing them to report any such symptoms immediately.
- Activity limitations: Advising on any restrictions on physical activity to prevent line dislodgement.
- Showering and bathing: Providing instructions on how to safely shower or bathe without compromising the line’s integrity.
- Medication administration: Explaining the process of medication administration through the central line, if applicable.
I use visual aids like diagrams and brochures to supplement my explanations and ensure comprehension. I always encourage questions and answer them patiently, ensuring the patient and family feel comfortable and confident in managing the central line. For example, I might show a patient a picture demonstrating proper handwashing technique. Finally, I provide written instructions and contact information for any follow-up questions or concerns.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the guidelines for managing central line-associated thrombosis?
Managing central line-associated thrombosis (CLAT) requires a proactive approach that combines prevention and timely intervention. Prevention strategies include ensuring proper catheter insertion technique, selecting the appropriate catheter size and material, maintaining adequate hydration, and using anticoagulant prophylaxis, as clinically indicated. Guidelines often recommend the use of low-molecular-weight heparin (LMWH) or unfractionated heparin (UFH) for patients at high risk of CLAT.
If CLAT is suspected (e.g., swelling, tenderness around the insertion site, or signs of venous occlusion on imaging), immediate action is critical. This involves:
- Assessment: Thorough clinical evaluation of the patient, including assessment of the insertion site and obtaining relevant imaging studies (e.g., ultrasound).
- Treatment: Initiating anticoagulation therapy as per institutional protocols and the severity of the thrombosis, often involving a careful titration of anticoagulants to balance the risk of bleeding against the benefit of preventing further clot formation.
- Catheter management: Depending on the severity and clinical scenario, this might involve leaving the catheter in place with anticoagulation, or removing the catheter and replacing it at a different site. The decision is made on a case-by-case basis, considering the patient’s clinical status and the necessity of continued intravenous access.
- Monitoring: Close monitoring of the patient’s response to treatment, including regular assessments of the insertion site, blood tests to evaluate anticoagulation, and repeat imaging if needed.
Documentation of all assessment findings, treatment decisions, and patient responses is crucial for quality improvement and legal considerations.
Q 17. How do you document central line care procedures?
Central line care procedures require meticulous documentation to ensure patient safety and adherence to best practices. Our documentation system includes a standardized electronic format that captures all essential information. This typically includes:
- Patient demographics and medical history: Basic patient identification information and relevant medical conditions.
- Date and time of insertion/removal: Precise record of central line insertion and removal times.
- Insertion site: Precise location of the central line insertion site.
- Catheter type and size: Detailed specifications of the implanted catheter.
- Dressing changes: Date, time, type of dressing material used, and any observations about the insertion site.
- Flush protocols: Type and volume of flush solution used and the frequency of flushing.
- Medication administration: Medications administered through the central line, including dosage, time, and route of administration.
- Complications: Any complications encountered during the procedure or subsequent care, including thrombosis, infection, or bleeding.
- Assessment and intervention: Regular assessment of the insertion site and any interventions taken in response to observations.
All entries must be clear, concise, accurate, and legible. Any deviations from standard protocols must be clearly documented and justified. This comprehensive record provides a complete picture of the patient’s central line care, which is essential for continuity of care, audit purposes, and legal protection.
Q 18. What is your experience with different types of central line access ports?
My experience encompasses a wide range of central venous access devices, including:
- Peripherally Inserted Central Catheters (PICCs): I’m proficient in PICC insertion, care, and management. PICCs are frequently used for long-term intravenous access and offer a less invasive alternative to surgically implanted central lines. Their longevity makes meticulous care essential to minimize risks such as infection and thrombosis.
- Tunneled Catheters: I have extensive experience with tunneled catheters, such as Hickman, Broviac, and Groshong catheters. These are surgically implanted and designed for long-term use. The tunneled portion reduces the risk of infection. I am comfortable with the specific care requirements associated with each type of tunneled catheter.
- Implanted Ports: I am familiar with the implantation, access, and maintenance of implanted ports. These completely subcutaneous devices offer long-term venous access with a reduced infection risk due to the lack of an external catheter. I understand the need for specialized needles for accessing these ports.
- Central Venous Catheters (CVCs): I have significant experience in the insertion and management of various CVC types, placed via the jugular, subclavian, or femoral veins. I understand the specific risks associated with each insertion site and the need for careful monitoring for complications such as pneumothorax or hemothorax.
My expertise extends to selecting the appropriate catheter type based on the patient’s individual needs, anticipated duration of therapy, and clinical circumstances. This decision-making process considers factors like the patient’s overall health, planned treatment, and risk factors for complications.
Q 19. Describe the process for obtaining informed consent for central line insertion.
Obtaining informed consent for central line insertion is a critical ethical and legal responsibility. The process begins with a thorough explanation of the procedure to the patient, using language they can understand. This explanation must cover:
- The purpose of the central line: Clearly stating why the central line is necessary and how it will benefit the patient.
- The procedure itself: Detailing the steps involved in the procedure, including the insertion site and the type of anesthesia used.
- Potential risks and complications: Openly discussing potential complications such as infection, bleeding, thrombosis, pneumothorax (collapsed lung), and air embolism.
- Alternative options: Explaining any alternative methods of treatment available, if applicable.
- Post-procedure care: Describing the aftercare required, including dressing changes and activity restrictions.
I ensure the patient has ample opportunity to ask questions and express concerns. I then provide written information about the procedure to reinforce verbal explanations. Once the patient fully understands the risks and benefits, I obtain their written consent. For patients who are unable to provide consent themselves (e.g., due to cognitive impairment or a medical emergency), I seek consent from their legally authorized representative. I meticulously document the entire consent process, including the date, time, and witnesses.
Q 20. How do you manage a patient experiencing an air embolism related to a central line?
Managing a patient experiencing an air embolism related to a central line is a critical emergency. The immediate actions involve:
- Clamping the catheter: Immediately clamping the central line to prevent further air entry.
- Positioning the patient: Placing the patient in a left lateral Trendelenburg position (left side lying with legs elevated), which helps to trap air in the right atrium.
- Administering oxygen: Providing supplemental oxygen to improve oxygenation.
- Monitoring vital signs: Closely monitoring vital signs (heart rate, blood pressure, oxygen saturation) for any changes.
- Notifying the physician: Immediately notifying the attending physician or other medical personnel for appropriate medical management.
- Supportive care: Providing supportive care as needed, including intravenous fluids and medications to stabilize the patient’s condition.
Depending on the patient’s response and the physician’s assessment, further interventions may be necessary, such as echocardiography to evaluate the extent of air embolism or decompression procedures in more severe cases. Prevention is crucial, requiring strict adherence to proper flushing techniques and careful insertion practices to minimize the risk of air embolism.
Q 21. Describe your experience with different types of central line dressing materials and their application.
My experience involves the use of various central line dressing materials, each selected based on the specific clinical situation and the patient’s needs. These include:
- Transparent semi-permeable dressings (e.g., Tegaderm): These allow for easy visualization of the insertion site, reducing the risk of undetected complications. They are suitable for short-term use and less complex scenarios.
- Hydrocolloid dressings: These provide a moist wound environment, which may be beneficial in certain cases. They offer good protection and absorption but do not allow for clear visualization of the insertion site.
- Gauze dressings: Traditional gauze dressings are sometimes used. They need to be changed frequently to maintain sterility and they can dry out and adhere to the insertion site.
- Impregnated gauze dressings: These combine the absorbency of gauze with antimicrobial properties for additional infection prevention.
Application involves strict adherence to aseptic technique to prevent contamination. The skin around the catheter insertion site is meticulously cleaned with an appropriate antiseptic solution (often chlorhexidine). The dressing material is then carefully applied to cover the insertion site completely, securing it firmly without causing undue pressure or irritation. The choice of dressing material and application technique is carefully documented within the patient’s medical record. Regular assessment of the insertion site and the dressing’s integrity is essential, with timely dressing changes being performed as needed to maintain sterility and prevent complications.
Q 22. What are your strategies for preventing dislodgement of central lines?
Preventing central line dislodgement is paramount to patient safety. My strategies focus on a multi-pronged approach encompassing meticulous insertion technique, secure stabilization, and diligent patient education.
- Securement Devices: I always utilize appropriate securement devices, ensuring they are correctly applied and regularly checked for tightness and integrity. This includes using chlorhexidine gluconate (CHG) impregnated dressings, which have been shown to reduce infection rates and potentially improve securement. For example, I’d carefully assess the patient’s anatomy and choose a device that minimizes tension on the line and allows for optimal patient mobility. Improper securement is a leading cause of dislodgement.
- Patient Education: I thoroughly educate patients and their families about the importance of avoiding activities that could put stress on the catheter, such as vigorous arm movements or pulling on the line. I provide written instructions and demonstrate proper techniques. A simple analogy I use is to compare the catheter to a delicate plant – it needs careful handling to thrive.
- Regular Assessments: Frequent assessment of the insertion site and securement device is crucial. I check for signs of infection, inflammation, or loosening. If any issues are detected, I immediately address them and document the findings.
- Appropriate Catheter Selection: The choice of catheter type and length is critical. Selecting a catheter that is appropriate for the patient’s anatomy and the duration of therapy significantly reduces the risk of dislodgement.
By combining these strategies, I significantly minimize the risk of central line dislodgement and ensure patient safety.
Q 23. How do you manage a patient with a suspected central line occlusion?
Suspected central line occlusion requires a systematic approach. My first step is always to assess the patient’s clinical status to rule out any immediate life-threatening complications. Then, I follow a series of steps:
- Confirm Occlusion: I attempt to flush the line with a saline solution to confirm whether the occlusion is mechanical (a clot or particulate matter) or functional (due to pressure or kinking).
- Gentle Aspiration: If flushing fails, I gently aspirate to see if any blood can be drawn.
- Thrombolytic Agents (if appropriate): If a clot is suspected, under physician order, I may administer a thrombolytic agent like urokinase or tissue plasminogen activator (tPA) to break up the clot. This is a physician-directed intervention.
- Mechanical Removal: If thrombolytics are ineffective, a mechanical method might be considered, such as using a guidewire to attempt to dislodge the occlusion. This is another physician-directed intervention and requires specialized training.
- Documentation: Throughout this process, meticulous documentation of all interventions, responses, and patient outcomes is essential.
It’s crucial to remember that unsuccessful attempts at restoring patency may necessitate line removal and placement of a new central line. Patient safety and comfort are paramount throughout this process.
Q 24. Describe your experience working with central line insertion teams.
My experience collaborating with central line insertion teams has been incredibly positive. I’ve worked closely with experienced physicians, nurses, and other healthcare professionals in various settings. This collaborative environment emphasizes best practices, evidence-based techniques, and the importance of a sterile field.
I actively participate in pre-insertion assessments, ensuring that the patient is appropriately prepared and that all necessary equipment and supplies are available. During the insertion procedure, I maintain the sterile field, monitor the patient’s vital signs, and assist the physician as needed. Post-insertion, I’m responsible for securing the catheter, educating the patient and family about care, and monitoring for complications. I value the teamwork and expertise that a dedicated insertion team brings to ensuring safe and effective central line placement.
For instance, on one occasion, we used ultrasound guidance during a particularly challenging placement, resulting in a successful insertion without complications. This demonstrated the value of advanced techniques and collaboration within the team.
Q 25. How do you stay updated on best practices for central line care?
Staying updated on best practices for central line care is a continuous process. I utilize several strategies:
- Professional Organizations: I am an active member of professional nursing organizations like the Association of periOperative Registered Nurses (AORN) and the Infusion Nurses Society (INS), where I access guidelines, publications, and continuing education opportunities.
- Evidence-Based Literature: I regularly review peer-reviewed articles and journals focusing on central line care, infection prevention, and related topics. This allows me to stay abreast of the latest research findings and clinical advancements.
- Continuing Education: I participate in continuing education programs and workshops specifically focused on central line insertion, management, and complications. These provide opportunities to learn from experts and to refine my skills.
- Institutional Policies and Procedures: I meticulously review and follow our institution’s policies and procedures for central line care. These are often updated to reflect the latest evidence-based guidelines.
By actively pursuing knowledge through these channels, I maintain the highest standard of care for my patients.
Q 26. What is your approach to troubleshooting complications with central lines?
Troubleshooting central line complications requires a systematic and logical approach. My strategy involves carefully assessing the situation, identifying the specific complication, and then taking appropriate action.
- Assess the Situation: First, I thoroughly evaluate the patient’s clinical status, paying close attention to any signs or symptoms of complications, such as infection, occlusion, or bleeding.
- Identify the Complication: Once I’ve identified the issue, I consult the relevant literature and institutional policies to guide my actions.
- Implement Interventions: Interventions may range from simple measures, like repositioning the patient to relieve kinking or using a different technique to flush the line, to more complex interventions, such as administering medication under physician order or preparing for line removal.
- Document and Communicate: Throughout the process, I meticulously document all assessments, interventions, and the patient’s response. Effective communication with the healthcare team, including physicians, is critical for optimal patient management.
For example, if I detect signs of infection at the insertion site, I immediately report it to the physician and initiate infection control measures such as obtaining cultures, initiating antibiotic therapy (per physician order), and reinforcing the dressing.
Q 27. What role does the nurse play in preventing central line complications?
The nurse plays a crucial role in preventing central line complications. We are often the primary caregivers and are positioned to closely monitor patients and intervene early if complications arise.
- Strict Asepsis: Nurses are responsible for maintaining strict aseptic technique during central line dressing changes and all other procedures involving the catheter. This includes proper hand hygiene, using sterile gloves and supplies, and adhering to infection control protocols.
- Patient Education: Providing thorough patient education on proper care, recognizing signs of infection, and reporting any problems is critical.
- Monitoring: Continuous monitoring for signs of infection, occlusion, or dislodgement is crucial. This includes regular assessment of the insertion site, and the patient’s overall condition.
- Documentation: Accurate and timely documentation of all assessments, interventions, and the patient’s response is essential for continuity of care.
- Collaboration: Effective collaboration with the healthcare team, including physicians and other nurses, is vital for preventing and managing complications.
Through these actions, nurses significantly reduce the risk of central line complications and promote patient safety.
Q 28. Explain the importance of hand hygiene in central line care.
Hand hygiene is the cornerstone of preventing central line-associated bloodstream infections (CLABSIs). It’s the most effective and readily available method for reducing the spread of microorganisms.
Before and after any contact with the patient or the central line, healthcare providers must perform thorough handwashing with soap and water or use an alcohol-based hand rub. This simple yet crucial step significantly reduces the risk of transmitting bacteria from one surface to another. The duration of hand hygiene should be sufficient to ensure complete coverage of all surfaces.
Think of it this way: our hands can act as vectors, easily transferring harmful bacteria to the catheter insertion site. Consistent and correct hand hygiene breaks this chain of transmission, protecting patients from potentially life-threatening infections. It’s a simple yet highly impactful intervention.
Key Topics to Learn for Central Line Care Interview
- Insertion Techniques: Understanding various insertion methods, including the Seldinger technique, and their associated complications. Consider the anatomical considerations and potential risks involved.
- Infection Prevention and Control: Mastering aseptic techniques, proper hand hygiene, and the use of sterile drapes and dressings. Be prepared to discuss strategies for minimizing CLABSI (Central Line-Associated Bloodstream Infections).
- Dressing Changes and Maintenance: Familiarize yourself with different dressing types and their application, as well as the frequency and procedures for dressing changes. Understand the importance of maintaining a sterile environment.
- Troubleshooting and Complications: Be ready to discuss common complications such as occlusion, air embolism, and infection. Prepare to explain your approach to identifying, managing, and preventing these issues.
- Catheter Selection and Management: Understand the different types of central venous catheters, their indications, and appropriate care based on the catheter type and patient needs. Discuss criteria for catheter removal.
- Patient Education and Communication: Explain your approach to effectively communicating with patients and families about central line care, including pre- and post-insertion care instructions and recognizing signs of infection.
- Legal and Ethical Considerations: Be prepared to discuss informed consent, documentation requirements, and the legal implications of central line care.
- Evidence-Based Practice: Demonstrate an understanding of current guidelines and best practices in central line care, citing relevant research and professional organizations.
Next Steps
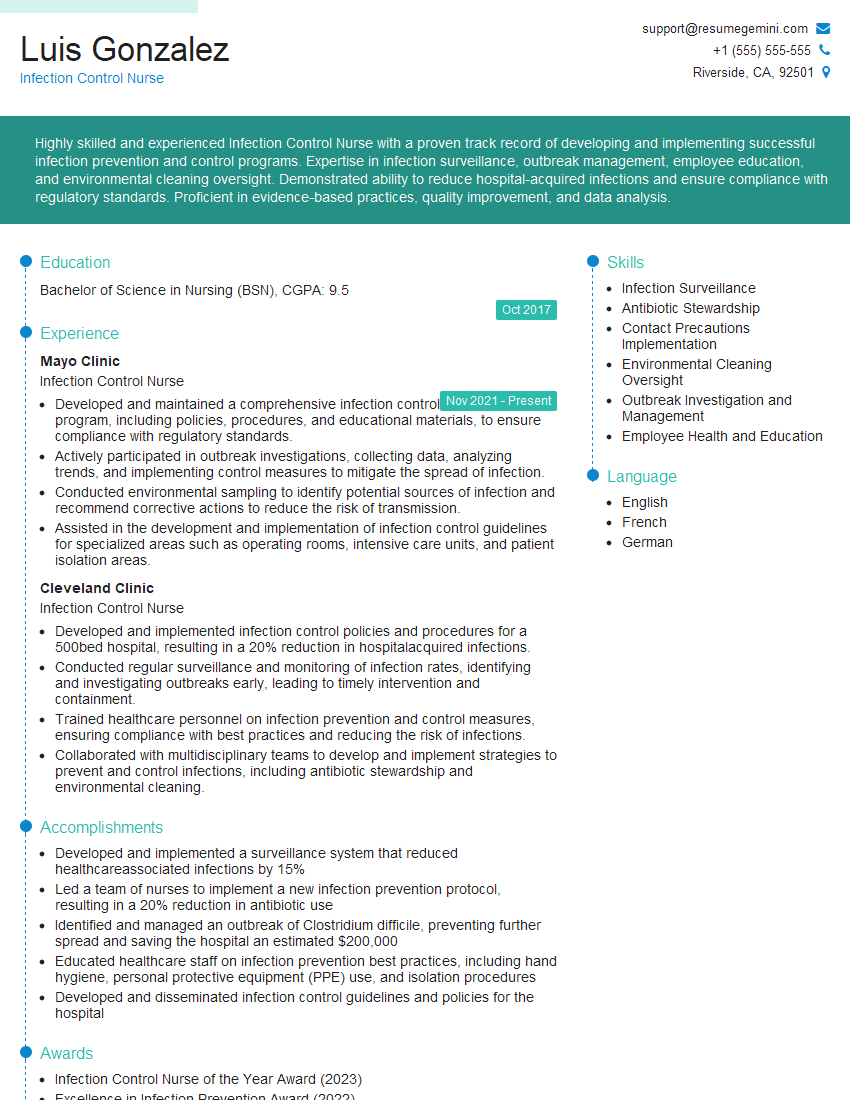
Mastering Central Line Care demonstrates a commitment to patient safety and advanced nursing skills, significantly enhancing your career prospects in critical care and other specialized areas. To maximize your chances of landing your dream role, a well-crafted, ATS-friendly resume is essential. ResumeGemini is a trusted resource that can help you build a professional resume that highlights your skills and experience effectively. Examples of resumes tailored to Central Line Care are available to help you create a compelling application.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.