Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Chest X-ray Interpretation interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Chest X-ray Interpretation Interview
Q 1. Describe the proper technique for acquiring a posteroanterior (PA) chest X-ray.
Obtaining a proper posteroanterior (PA) chest X-ray is crucial for accurate interpretation. The patient should stand erect, facing the X-ray machine, with their shoulders rolled forward and their arms down at their sides. The chest should be positioned against the image receptor, ensuring the entire lung fields are included. The X-ray beam should enter the posterior aspect of the chest and exit the anterior aspect. Proper positioning is paramount to minimizing magnification and distortion of structures. This ensures the heart is not falsely enlarged due to angulation, and the lung apices are clearly visible. We’re aiming for a standardized view that allows for comparison across multiple images.
Key Steps:
- Patient stands erect, facing the cassette.
- Shoulders rolled forward to minimize scapular obscuration.
- Arms at sides, away from the chest.
- Chin slightly elevated to ensure the clavicles are not superimposed on the apices.
- Deep inspiration to fully expand the lungs.
- X-ray beam centered at the level of the mid-sternum.
Failure to adhere to these steps can lead to suboptimal images with technical artifacts that impede accurate interpretation. For example, a rotated image might show one lung field appearing larger than the other, potentially leading to a misdiagnosis.
Q 2. What are the key anatomical landmarks identified on a chest X-ray?
Several key anatomical landmarks are consistently identified on a chest X-ray. These landmarks are essential for orientation and aid in the systematic assessment of the various structures. Imagine it as a roadmap for your chest.
- Clavicles: These bones help to determine the location of the apices (uppermost parts) of the lungs.
- Sternum: Provides a midline reference point.
- Ribs: Used to assess the lung fields, and their appearance can help determine the presence of certain conditions. We also use them to count ribs to help assess lung volume.
- Vertebrae: These structures can be used as another midline reference, and their appearance can help rule out pathology in the spine.
- Diaphragm: The separation between the thorax and abdomen, its position is vital in evaluating lung expansion. We assess both hemidiaphragms for evenness.
- Heart: Its size and shape are important and assessed in relation to the thoracic cage.
- Hilar structures: These are the regions where the bronchi, pulmonary arteries, and veins enter and exit the lungs. Changes here can indicate pulmonary disease.
- Lung fields: The majority of the image, encompassing the lungs’ parenchyma and the interstitial spaces.
By systematically evaluating these landmarks, we can create a comprehensive assessment of the patient’s chest.
Q 3. Explain the differences between a PA and lateral chest X-ray.
PA and lateral chest X-rays are complementary views providing different perspectives of the thoracic structures. The PA view is the standard frontal projection, offering a view of the chest from front to back. The lateral view is taken from the side, typically the left side, providing a profile view. Think of it like taking a photo from the front and then from the side to get a fuller picture.
Key Differences:
- PA View: Provides optimal visualization of the heart size and shape, and the overall lung fields. The degree of magnification is minimized.
- Lateral View: Allows differentiation of anterior from posterior structures, crucial for identifying lesions located in specific lung segments, detecting subtle pneumothorax, and better assessing the mediastinum.
Using both views is essential for thorough assessment. A PA view alone might miss a small pneumothorax posterior to the lung; the lateral view allows visualization of this crucial aspect. Combining them provides a three-dimensional understanding of the chest.
Q 4. How do you identify pneumothorax on a chest X-ray?
Pneumothorax, or air in the pleural space, presents radiographically as a visceral pleural line that is separated from the parietal pleura, creating a lucent area without pulmonary markings. The key is to look for the air.
Identifying Features:
- Visceral pleural line: A thin, linear radiolucency separating the lung from the pleural space. This is the most reliable finding.
- Absence of lung markings: The area between the visceral pleural line and the chest wall appears lucent, lacking the normal vascular markings of the lung.
- Hyperlucency: The affected hemithorax may appear more radiolucent (darker) than the contralateral side. This is less specific than other findings.
- Lung collapse (atelectasis): In larger pneumothoraces, the lung can be compressed, leading to volume loss and shift of mediastinal structures.
It is important to remember that small pneumothoraces can be difficult to detect on a chest X-ray, and in these cases a CT scan may be necessary. Also, a patient with a pneumothorax may have other clinical findings that are consistent with this diagnosis, even in the absence of radiographic evidence.
Q 5. Describe the radiographic findings of pneumonia.
Pneumonia, an infection of the lung parenchyma, appears radiographically as an area of consolidation. This means the air spaces in the lungs are filled with fluid or inflammatory exudate, resulting in increased opacity.
Radiographic Findings:
- Consolidation: An area of increased density (whiteness) in the lung field, often with an air bronchogram sign (air-filled bronchi are visible within the consolidated area). This is indicative of the fluid filling the alveoli.
- Air bronchogram sign: The appearance of air-filled bronchi within a consolidated area. This is a key sign of pneumonia.
- Lobar or segmental distribution: Pneumonia often affects a specific lobe or segment of the lung.
- Possible pleural effusion: In some cases, associated pleural effusion (fluid collection in the pleural space) may be present.
The appearance of pneumonia can vary depending on the type of infection and its severity. For example, a bacterial pneumonia might present as a dense consolidation, while a viral pneumonia may have less defined, more diffuse changes. Therefore, correlating the radiographic findings with the clinical presentation is crucial for accurate diagnosis.
Q 6. How would you differentiate between a pleural effusion and a consolidation on a chest X-ray?
Differentiating between a pleural effusion and a consolidation on a chest X-ray requires careful attention to detail. Both conditions present with increased opacity, but their location and characteristics differ.
Key Differences:
- Pleural effusion: Fluid accumulation in the pleural space. Radiographically, this presents as blunting of the costophrenic angles (the sharp angles between the diaphragm and the rib cage), meniscus sign (a concave upper border of the fluid), and potential displacement of the mediastinum.
- Consolidation: Infiltration of the lung parenchyma, filling air spaces with fluid or exudate. Radiographically, this presents as an area of increased density within the lung field, often with an air bronchogram sign. It does not usually cause blunting of the costophrenic angles.
Meniscus sign: This is a very characteristic finding of a pleural effusion, where the superior edge of the fluid in the pleural space forms a concave curve. This sign is absent in consolidation. Imagine the fluid building up like water in a glass.
Sometimes, it can be challenging to distinguish completely. If uncertain, further imaging techniques (like a CT scan or ultrasound) may be needed.
Q 7. What are the characteristic findings of pulmonary edema on a chest radiograph?
Pulmonary edema, or fluid accumulation in the lungs’ interstitial and alveolar spaces, displays characteristic radiographic findings.
Characteristic Findings:
- Increased interstitial markings: These are the fine lines representing the connective tissue and blood vessels within the lungs; these become more prominent and numerous in edema. Imagine it as the lung’s network of tiny streets becoming flooded.
- Perihilar haze: A hazy opacification around the hilum (where the bronchi, arteries, and veins enter and exit the lungs). This indicates fluid accumulating in the central regions of the lung.
- Air bronchogram sign: Air-filled bronchi might be visible against a background of alveolar edema. It is crucial to note this can also appear in pneumonia.
- Kerley B lines: Short, horizontal lines near the periphery of the lung, representing thickened interlobular septa. These lines are quite specific to pulmonary edema.
- Bat wing pattern: In severe cases, a diffuse, symmetrical increased opacity resembling the shape of a bat’s wings can be observed, showing the fluid accumulating centrally around the hila.
The presence and severity of these findings depend on the extent and cause of the pulmonary edema. Correlating radiographic findings with clinical presentation and other lab results is critical for diagnosis and management.
Q 8. Explain how to assess cardiac size on a chest X-ray.
Assessing cardiac size on a chest X-ray involves evaluating the cardiothoracic ratio (CTR). The CTR is the ratio of the transverse diameter of the heart to the transverse diameter of the thorax at the level of the widest point of the cardiac silhouette. Ideally, it should be measured on a posteroanterior (PA) view, as an anteroposterior (AP) view can artificially enlarge the cardiac silhouette.
Steps to assess cardiac size:
- Identify the widest point of the cardiac silhouette: This is usually at the level of the right and left atria.
- Measure the transverse diameter of the heart: Draw a line across the widest part of the cardiac silhouette, measuring the distance between the lateral edges of the heart.
- Measure the transverse diameter of the thorax: Draw lines along the inner aspects of the ribs, measuring the distance between the inner edges of the right and left ribs at the same level as the cardiac measurement.
- Calculate the CTR: Divide the cardiac diameter by the thoracic diameter. A normal CTR is generally less than 0.5 (50%). A CTR above 0.5 suggests cardiomegaly (enlarged heart), but this needs to be interpreted considering the patient’s age, body habitus, and other clinical findings.
Example: If the transverse cardiac diameter is 10cm and the transverse thoracic diameter is 22cm, the CTR is 10/22 = 0.45, which is within the normal range.
It’s crucial to remember that factors like rotation of the chest X-ray can affect the accuracy of the measurement. A properly positioned PA chest X-ray is essential for accurate cardiac size assessment.
Q 9. How do you identify atelectasis on a chest X-ray?
Atelectasis, meaning the collapse or incomplete expansion of a lung or a segment of a lung, shows various appearances on a chest X-ray depending on the size and location of the affected area.
Key radiographic findings of atelectasis include:
- Increased opacity (whiteness): The affected lung area appears denser and whiter than the surrounding normal lung tissue.
- Volume loss: The affected lung segment is smaller than normal, leading to crowding of the surrounding structures (e.g., vessels, bronchi). This can result in upward displacement of the diaphragm and shift of the mediastinum towards the affected side (in significant atelectasis).
- Shifting of fissures: Interlobar fissures may be displaced toward the area of atelectasis.
- Air bronchograms: In some cases, air-filled bronchi can be visualized within the consolidated atelectatic lung, appearing as tubular lucencies within the opacity; this is a hallmark of atelectasis.
- Crowding of blood vessels: Blood vessels may appear more densely packed in the affected region.
Example: A patient with right middle lobe atelectasis may show increased opacity in the right middle lung zone with a possible slight elevation of the right hemidiaphragm and crowding of the bronchovascular markings.
Differentiating atelectasis from other causes of opacities like pneumonia requires careful correlation with the clinical presentation and other imaging modalities.
Q 10. Describe the radiographic findings of a rib fracture.
A rib fracture appears as a lucency (dark line) interrupting the continuity of a rib’s cortices on a chest X-ray. The fracture line may be transverse, oblique, or comminuted (in multiple pieces).
Radiographic findings:
- Disruption of the cortical bone: A clear line of discontinuity is seen traversing the rib.
- Overlapping of rib fragments: Depending on the degree of displacement, there might be overlapping of the fractured rib fragments.
- Possible soft tissue swelling: If there’s significant trauma, soft tissue swelling adjacent to the fracture site might be visible.
Example: A patient presenting after a fall may show a clean transverse fracture of the 5th right rib. Careful inspection of each rib is necessary as the fracture may be subtle or obscured by overlying structures.
It’s important to note that in some cases, a rib fracture might not be clearly visible on a chest X-ray, especially if the fracture is nondisplaced or involves a small fragment. Additional imaging such as CT scan might be required for a definitive diagnosis.
Q 11. What are the key features of a tension pneumothorax?
Tension pneumothorax is a life-threatening condition where air enters the pleural space but cannot escape, leading to progressive lung collapse and circulatory compromise. It is a true emergency requiring immediate treatment.
Key radiographic features of a tension pneumothorax:
- Complete or near-complete collapse of the ipsilateral lung: The lung on the affected side appears significantly smaller or absent.
- Absence of lung markings in the affected hemithorax: The lung fields are hyperlucent (very dark) and lack normal vascular markings on the affected side.
- Tracheal and mediastinal shift: The trachea and mediastinal structures (heart, great vessels) are displaced away from the affected side towards the contralateral side, often significantly.
- Depressed hemidiaphragm: The diaphragm on the affected side can be slightly depressed.
Example: A patient with a right tension pneumothorax might show a completely collapsed right lung with a marked shift of the trachea and mediastinum to the left. The right hemithorax will be hyperlucent.
The presence of these findings is a radiological emergency demanding immediate medical intervention (needle decompression) before proceeding with further investigations.
Q 12. How would you differentiate between a nodule and a mass on a chest X-ray?
Differentiating between a nodule and a mass on a chest X-ray is based primarily on size.
Nodule: A small, rounded opacity usually less than 3cm in diameter.
Mass: A larger, rounded or irregular opacity greater than 3cm in diameter.
The distinction is important because masses are more likely to be malignant than nodules, although both can be benign or malignant.
Example: A 1.5cm well-defined opacity in the right upper lobe is considered a nodule, while a 4cm irregular opacity in the left lower lobe is considered a mass. Further imaging (CT scan, PET scan) and biopsy may be needed for characterization and diagnosis.
Other factors influencing interpretation include the lesion’s shape, margins (well-defined versus ill-defined), and presence of calcification. A spiculated nodule or mass is more suggestive of malignancy.
Q 13. Describe the radiographic appearance of pulmonary embolism.
Pulmonary embolism (PE), a blockage of blood vessels in the lungs, can be difficult to directly visualize on a chest X-ray. The chest X-ray may show indirect findings rather than the embolism itself. These findings are often nonspecific and may be absent.
Indirect radiographic findings suggestive of PE:
- Westermark sign: An area of oligemia (decreased vascularity) or a wedge-shaped opacity with a sharp border in the periphery of the lung, caused by local alveolar edema and atelectasis.
- Hampton hump: A wedge-shaped opacity at the periphery of the lung, often located in the lower lobes, suggestive of pulmonary infarction. This is a late finding.
- Pleural effusion: Fluid accumulation in the pleural space can be a consequence of pulmonary infarction.
- Elevated diaphragm: Possible secondary to pleural effusion or atelectasis.
Example: A patient suspected of having a PE might present with a Westermark sign, showing an area of reduced pulmonary vasculature in a segment of the right lung. However, absence of these findings doesn’t exclude a PE.
Chest X-rays are not the primary imaging modality for diagnosing PE. A CT pulmonary angiography (CTPA) is the preferred imaging technique.
Q 14. What are the different types of lung opacities seen on chest X-rays and how to differentiate them?
Lung opacities are areas of increased density on a chest X-ray, representing consolidation or increased tissue density within the lungs. Various types exist:
Types of lung opacities and differentiation:
- Consolidation: Homogenous opacity often associated with pneumonia, hemorrhage, or tumor. It obscures underlying lung markings. Differentiation: Pneumonia often presents with air bronchograms, while tumor might show irregular margins.
- Interstitial pattern: Linear or reticular opacities along the lines of lymphatics or interstitium, often associated with interstitial lung diseases (ILDs) such as sarcoidosis, fibrosis. Differentiation: Appearance of a ground glass opacity, reticular nodular pattern, or honeycombing helps determine the type of ILD.
- Nodules: Small, rounded opacities <3cm, seen in infections, granulomas, or tumors. Differentiation: Location, size, margins, and presence of calcification are key differentiating factors.
- Masses: Larger opacities >3cm, representing tumors, abscesses, or granulomas. Differentiation: Irregular margins and spiculation suggest malignancy.
- Ground-glass opacity (GGO): Diffuse haziness, obscuring but not completely obliterating lung markings, seen in acute lung injury, pulmonary edema, and some types of lung cancer. Differentiation: The pattern (e.g., patchy, diffuse) and clinical context are important for differentiating causes.
Example: A patient presenting with cough, fever, and a homogenous opacity with air bronchograms in the right lower lobe might be diagnosed with lobar pneumonia. A patient with progressive shortness of breath and diffuse reticulonodular pattern may have an interstitial lung disease.
Careful evaluation of the opacity’s distribution, shape, margin characteristics, the presence of air bronchograms, and clinical correlation are essential for differentiating between these lung opacities.
Q 15. Explain the role of the diaphragm in chest X-ray interpretation.
The diaphragm is a crucial landmark in chest X-ray interpretation, acting as a critical dividing line between the thoracic cavity (containing the lungs and heart) and the abdominal cavity. Its shape, position, and integrity provide valuable information about various respiratory and abdominal conditions.
- Shape and Position: Normally, the diaphragm is dome-shaped, with the right hemidiaphragm typically slightly higher than the left due to the presence of the liver. Significant asymmetry or flattening can suggest underlying issues such as atelectasis (lung collapse), pleural effusion (fluid in the pleural space), or pneumothorax (collapsed lung).
- Integrity: The diaphragm’s smooth, continuous contour should be easily visible. Irregularities, such as elevation or disruption, could indicate a diaphragmatic hernia (protrusion of abdominal contents into the chest cavity), trauma, or postoperative changes.
- Movement: While not directly assessed on a single static X-ray, the diaphragm’s movement during respiration is crucial for proper ventilation. Assessing multiple X-rays taken during inspiration and expiration can indirectly evaluate diaphragm function.
For example, a right-sided pleural effusion would cause the right hemidiaphragm to be depressed and obscured. Conversely, a pneumoperitoneum (free air in the abdomen) might lead to elevation of both hemidiaphragms.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you assess for the presence of free air under the diaphragm?
Free air under the diaphragm, also known as pneumoperitoneum, indicates a breach in the gastrointestinal tract or other abdominal organs allowing air to escape into the peritoneal cavity. It’s a serious condition requiring immediate attention.
Assessment involves carefully examining the area beneath the diaphragm on the chest X-ray. Look for:
- Crescent-shaped lucency: The most characteristic sign is a crescent of air outlining the upper border of the liver or the spleen (depending on the patient’s position). This air appears darker than the surrounding tissues.
- Air bubbles: You might observe small, irregular pockets of air scattered beneath the diaphragm.
- Elevated diaphragms: Although not specific to pneumoperitoneum, elevated diaphragms can also be associated with this condition.
It’s important to remember that the presence or absence of pneumoperitoneum in the absence of other clinical findings must be clinically correlated with the patient’s history and physical examination.
Q 17. What are the limitations of chest X-ray in diagnosing certain pathologies?
Chest X-rays are a valuable initial diagnostic tool, but they have limitations. They cannot visualize everything and their interpretation requires clinical correlation.
- Early-stage diseases: Subtle pathologies, such as early-stage lung cancer or interstitial lung disease, may not be readily apparent on a chest X-ray.
- Soft tissue differentiation: Chest X-rays are less sensitive in differentiating between soft tissue structures (e.g., distinguishing between different types of lung masses).
- Lack of functional information: A chest X-ray provides a static image and does not provide functional information about the lungs’ ability to ventilate or perfuse. Pulmonary embolism, for example, often goes undetected.
- Overlapping structures: Overlapping structures of the heart, great vessels, and lungs can obscure underlying abnormalities.
- Radiation exposure: There is a small but inherent risk of radiation exposure associated with X-ray imaging.
For instance, a subtle nodule may only be detectable by computed tomography (CT) scan. Similarly, the diagnosis of pulmonary embolism requires pulmonary angiography or CT pulmonary angiography.
Q 18. Describe your experience with interpreting pediatric chest X-rays.
Interpreting pediatric chest X-rays requires specialized knowledge due to the anatomical and physiological differences in children compared to adults. The interpretation should take into account the child’s age, size, and developmental stage. Key differences include:
- Lung field appearance: Infants and young children have relatively larger lung volumes and different lung markings. The thymus gland, which is usually larger in children, can be mistaken for a mass.
- Rib cage shape: The rib cage is more horizontal in infants and young children.
- Heart size and shape: The cardiac silhouette appears larger in proportion to the thorax in children.
- Positioning: Obtaining optimal positioning can be more challenging in children.
I have extensive experience in interpreting pediatric chest X-rays, having worked in both hospital and community settings. I regularly consult on cases involving suspected pneumonia, congenital heart defects, and other childhood respiratory illnesses. I approach these cases with a heightened awareness of the normal variations seen in the pediatric population.
Q 19. How do you approach a chest X-ray with multiple findings?
A chest X-ray with multiple findings necessitates a systematic approach to avoid overlooking crucial information. I use a structured approach:
- Systematic review: I begin by systematically evaluating each aspect of the chest X-ray, starting with the bones (ribs, clavicles, spine), soft tissues, lung fields, heart size, and diaphragm.
- Prioritize findings: I determine which findings are most critical. For example, a large pneumothorax would supersede a subtle finding like a small nodule.
- Correlate with clinical data: The findings are correlated with the patient’s symptoms, medical history, and laboratory results. This is essential for accurate interpretation.
- Differential diagnosis: Based on the prioritized findings and clinical data, I formulate a list of possible diagnoses.
- Formulate a report: A concise report detailing the findings, their interpretation, and the differential diagnosis is written for the referring physician.
For instance, if a patient presents with pneumonia symptoms and their X-ray reveals consolidation, pleural effusion, and a small nodule, I would initially prioritize the consolidation and effusion which are consistent with pneumonia. The nodule would then be further investigated using more sensitive imaging techniques. This systematic approach ensures that all findings are considered but that the most urgent concerns are addressed first.
Q 20. Explain your workflow for interpreting a chest X-ray report.
My workflow for interpreting a chest X-ray report involves several key steps:
- Review the clinical information: I begin by carefully reviewing the patient’s clinical history, symptoms, and the reason for ordering the chest X-ray.
- Analyze the X-ray: I systematically assess all aspects of the X-ray, checking for any abnormalities, focusing on the technical quality of the image, the position of the patient, and any artifacts.
- Identify key findings: Once identified, I use established criteria and differential diagnoses for each finding.
- Correlation: I carefully correlate findings with clinical data, considering the likelihood and implications of various diagnoses.
- Report writing: I compile a detailed report that clearly describes the identified findings, the diagnostic reasoning, and appropriate recommendations. The report is structured and includes relevant technical information such as the date of the study and the patient’s position during the imaging.
Throughout the process, I maintain a high level of accuracy and precision and always maintain up to date knowledge on current guidelines and best practices in chest radiology.
Q 21. How do you ensure accuracy and efficiency in your chest X-ray interpretations?
Accuracy and efficiency in chest X-ray interpretation are paramount. I ensure both through a combination of strategies:
- Continuing medical education: I regularly participate in continuing medical education courses and conferences to stay updated on the latest advancements in radiology and chest disease.
- Structured approach: Following a systematic approach to image analysis prevents missing crucial details.
- Quality control measures: I adhere to strict quality control measures, regularly reviewing my own interpretations and participating in peer review processes to improve accuracy and consistency.
- Utilizing technology: Advanced image processing software and artificial intelligence tools can aid in identifying subtle findings and improving efficiency.
- Consultation when needed: I am not afraid to seek advice from senior radiologists or colleagues for complex cases or when uncertainty exists.
By combining these strategies, I strive to provide accurate and timely chest X-ray interpretations to improve patient care.
Q 22. Describe your experience with using radiology information systems (RIS) and PACS.
My experience with Radiology Information Systems (RIS) and Picture Archiving and Communication Systems (PACS) is extensive. RIS is the heart of radiology administration, managing patient demographics, scheduling, and report generation. I’m proficient in using RIS to access patient history, relevant clinical information, and to efficiently order and track imaging studies. PACS, on the other hand, is the digital library for medical images. I’m highly skilled in using PACS to view, manipulate, and interpret chest X-rays, utilizing tools like windowing and level adjustments to optimize image visualization. I’m comfortable with various PACS interfaces and understand the importance of efficient workflow within these systems for timely reporting and patient care. For example, I regularly use PACS’s annotation tools to highlight key findings directly on the images and to measure distances or angles for more precise analysis.
In a typical workflow, I’d first access the patient’s information in the RIS, review their clinical history and referring physician’s request, then use the RIS-PACS integration to retrieve the chest X-ray images. After interpretation, I’d use the RIS to generate a comprehensive report that clearly communicates my findings back to the referring physician.
Q 23. How do you stay updated on the latest advancements in chest X-ray interpretation?
Staying current in chest X-ray interpretation requires a multifaceted approach. I regularly attend conferences and workshops hosted by organizations like the American College of Radiology (ACR) and the Radiological Society of North America (RSNA) to learn about the latest techniques and research findings. These conferences provide valuable opportunities to network with colleagues and learn from experts in the field. I actively subscribe to and read peer-reviewed journals such as Radiology, AJR American Journal of Roentgenology, and Chest. These publications often feature cutting-edge research and clinical studies, shaping our understanding of various pathologies. Moreover, I utilize online resources like medical news websites and educational platforms which offer continuing medical education (CME) credits to maintain my certifications. Finally, participation in internal quality assurance meetings and case reviews within my institution fosters continuous learning and improvement in interpretation skills.
Q 24. Explain your understanding of radiation safety protocols.
Radiation safety is paramount in my practice. I adhere to the principles of ALARA (As Low As Reasonably Achievable) to minimize patient radiation exposure. This involves ensuring proper imaging techniques are used, selecting the lowest radiation dose appropriate for the clinical question, and utilizing optimal image processing techniques to enhance image quality without requiring repeat exposures. I’m familiar with various shielding techniques and follow protocols for protecting patients, especially pregnant women and children. I am also knowledgeable about radiation safety regulations and guidelines set by regulatory bodies like the FDA and local health departments. This includes understanding and following protocols for disposal of contaminated materials. For example, I would always confirm patient details to ensure correct imaging parameters are used, and I would shield any non-necessary body parts during the procedure. I would also always carefully review the images after the scan to ensure the proper dose was given. Regular audits and adherence to departmental protocols are critical for maintaining a safe environment.
Q 25. Describe a challenging case in chest X-ray interpretation and how you approached it.
One challenging case involved a patient presenting with subtle opacities in the lung fields on their chest X-ray. The opacities were not clearly defined and could have been indicative of several conditions, including pneumonia, pulmonary edema, or even malignancy. The patient’s clinical history was not entirely helpful in differentiating between these possibilities. My approach involved a systematic review of the images, paying close attention to the distribution, morphology, and density of the opacities. I then carefully reviewed the patient’s medical history, including their symptoms, vital signs, and relevant lab results. I correlated this information with the imaging findings.
Due to the uncertainty, I collaborated with other specialists, including the pulmonologist and oncologist, to assess the findings and discuss alternative diagnostic approaches. We decided to perform additional imaging, including a CT scan, which provided higher resolution images, improving the visualization of the subtle findings and giving a clearer picture of the underlying disease process. Ultimately, the additional imaging and clinical information allowed us to reach a conclusive diagnosis which, in this case, was an early-stage lung cancer. This case highlighted the importance of collaborative teamwork, thorough clinical correlation, and the use of additional imaging modalities when faced with challenging or ambiguous radiographic findings.
Q 26. How do you communicate findings to referring physicians?
Communicating findings to referring physicians requires clarity, conciseness, and accuracy. My reports always begin with a brief summary of the key findings in plain language, avoiding overly technical jargon unless absolutely necessary. I follow a structured approach: identifying the main abnormalities, describing their location, size, and appearance, and then correlating these imaging findings with the clinical information. I also offer an interpretation of the findings in terms of their potential clinical significance, proposing possible diagnoses when appropriate. For instance, rather than writing ‘consolidation in the right lower lobe,’ I might write ‘there is an area of increased density in the right lower lung consistent with pneumonia.’ I use the RIS to generate reports that are easy for clinicians to interpret and are well-organized. I ensure that my reports answer the specific questions posed by the referring physician and provide recommendations for next steps in patient management. If there’s uncertainty, I clearly state that in the report, suggesting additional investigations as needed. I’m always available to answer questions and clarify any doubts the referring physician may have.
Q 27. How do you handle discrepancies or uncertainties in your interpretations?
Discrepancies or uncertainties in interpretations are handled with a structured and cautious approach. When I encounter ambiguous findings, I critically re-evaluate the images, scrutinizing various aspects, including image quality, technique, and potential artifacts. I may consult image processing tools to further enhance visualization of subtle details. I then meticulously review the patient’s clinical history, laboratory results, and other relevant medical records. To resolve uncertainties, I may seek a second opinion from a colleague. Consulting with other specialists (pulmonology, cardiology, etc.) is also beneficial, particularly in complex cases. If the uncertainty persists despite these measures, I clearly state the ambiguity and the range of possible diagnoses in my report, while highlighting the need for further investigation such as additional imaging (CT, MRI), blood tests, or other diagnostic procedures to arrive at a definitive diagnosis. Transparency and collaboration are key in such situations.
Q 28. Describe your experience with quality assurance and quality control in chest X-ray interpretation.
Quality assurance and quality control are integral to my practice. I participate actively in departmental quality assurance meetings, where we review cases, discuss interpretation discrepancies, and address any identified shortcomings in our procedures. We use various metrics to assess the quality of our interpretations, including regular audits to ensure adherence to departmental protocols and guidelines. This involves analyzing error rates and identifying areas requiring improvement. Moreover, regular participation in continuing medical education (CME) activities and peer-reviewed journal reading help keep me abreast of current best practices and guidelines. We also implement regular quality control measures for the imaging equipment itself, ensuring calibration and optimal functioning to reduce variability and artifacts in image quality. Maintaining these standards helps ensure patient safety, improves the accuracy of our diagnoses, and enhances the overall quality of care.
Key Topics to Learn for Chest X-ray Interpretation Interview
- Systematic Approach to Image Analysis: Mastering a structured approach to reviewing CXRs, including a consistent order of examination (e.g., airways, bones, soft tissues, etc.).
- Pathology Recognition: Developing proficiency in identifying common pathologies such as pneumonia, pneumothorax, pleural effusions, atelectasis, and cardiomegaly. This includes understanding the characteristic radiographic appearances of each condition.
- Differential Diagnosis: Building the skill to generate a list of possible diagnoses based on image findings, considering the patient’s clinical presentation when available.
- Image Quality Assessment: Understanding the factors affecting image quality (e.g., overexposure, underexposure, motion artifact) and their impact on interpretation.
- Anatomical Knowledge: Possessing a strong understanding of thoracic anatomy, including the location and appearance of key structures on a CXR.
- Technical Aspects of X-ray Production: A basic grasp of how X-rays are produced and the principles of image formation will enhance your understanding of image limitations and artifacts.
- Ethical Considerations and Reporting: Understanding the importance of accurate and concise reporting, and the ethical implications of misinterpretation.
- Case-Based Learning: Practice interpreting a wide range of CXRs, focusing on building your diagnostic reasoning skills.
- Communication Skills: Prepare to clearly and concisely explain your findings and reasoning to both technical and non-technical audiences.
Next Steps
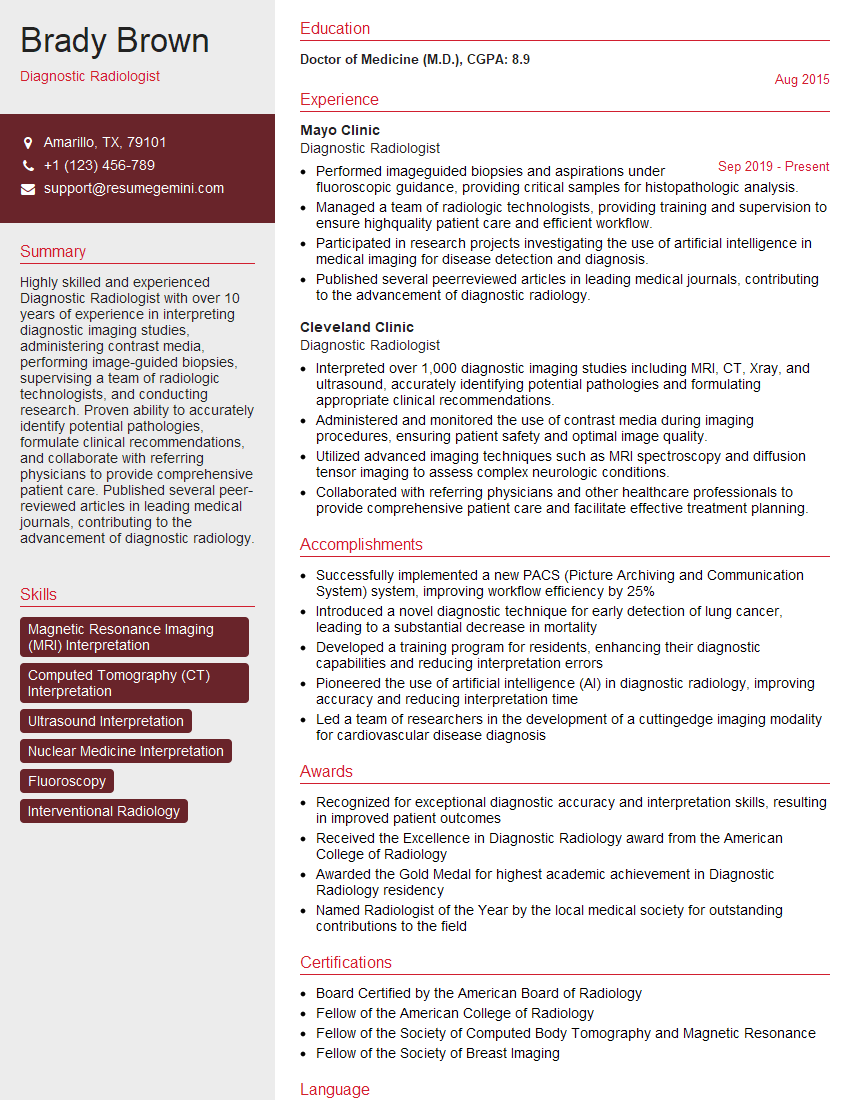
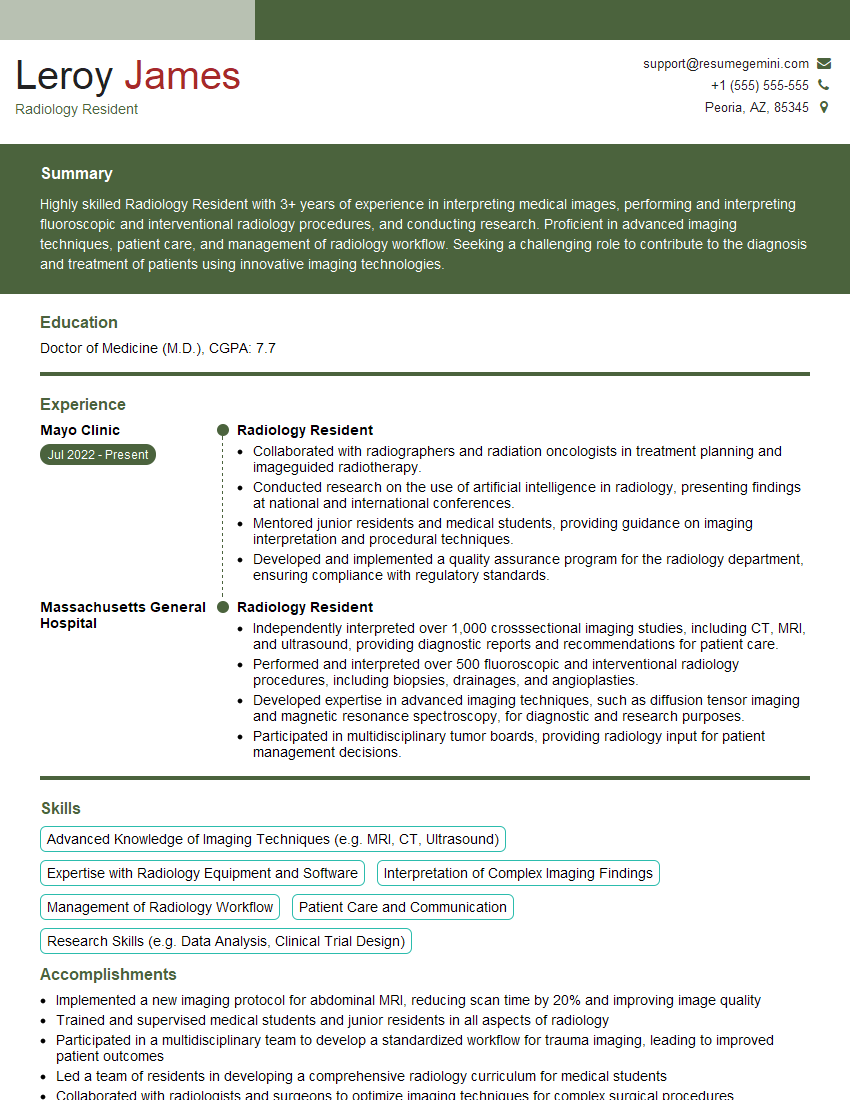
Mastering chest X-ray interpretation is crucial for career advancement in radiology and related fields. It demonstrates a high level of clinical skill and diagnostic competence, opening doors to specialized roles and increased responsibilities. To maximize your job prospects, create an ATS-friendly resume that highlights your expertise. ResumeGemini is a trusted resource to help you build a professional and impactful resume. They provide examples of resumes tailored to Chest X-ray Interpretation to guide you. Take the next step and build a resume that reflects your skills and experience – you deserve to be seen!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.