Cracking a skill-specific interview, like one for Cognitive rehabilitation using music-based interventions, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Cognitive rehabilitation using music-based interventions Interview
Q 1. Describe your experience with music-based interventions for cognitive rehabilitation.
My experience with music-based interventions in cognitive rehabilitation spans over 15 years, encompassing work with diverse populations experiencing various cognitive impairments. I’ve designed and implemented individualized music therapy programs for individuals recovering from stroke, traumatic brain injury (TBI), dementia, and other neurological conditions. This includes utilizing a wide range of musical approaches, from active music making (e.g., playing instruments, singing) to receptive music listening, tailored to specific cognitive deficits. For instance, I worked with a stroke survivor who had aphasia (difficulty with language) and used melodic intonation therapy (MIT) to improve their verbal fluency. In another case, I used rhythm and movement activities with a patient with Parkinson’s disease to enhance motor skills and cognitive function. My work is rooted in evidence-based practice, constantly informed by research and clinical outcomes.
Q 2. Explain the theoretical framework underlying your use of music in cognitive rehabilitation.
My approach is grounded in several theoretical frameworks. Neurological Music Therapy (NMT) is central, emphasizing the brain’s inherent plasticity and its response to musical stimuli. Music engages multiple brain regions simultaneously, activating neural pathways that might be otherwise dormant or impaired. This multi-sensory stimulation helps to bypass damaged areas and enhance cognitive function. Additionally, I integrate principles from cognitive psychology, focusing on attention, memory, and executive function. For example, using rhythmic cueing in memory tasks strengthens encoding and retrieval processes. The principles of emotional regulation and motivation are also crucial; music’s emotional power can engage clients, making the rehabilitation process more enjoyable and sustainable, which in turn improves compliance and outcomes.
Q 3. What assessment tools do you use to evaluate the cognitive abilities of your clients?
Assessment is crucial to tailoring effective interventions. I use a battery of tests depending on the individual’s needs and presenting problems. These may include standardized neuropsychological tests like the Montreal Cognitive Assessment (MoCA), the Mini-Mental State Examination (MMSE), or more comprehensive batteries depending on the suspected areas of impairment. I also utilize specific tests to assess areas relevant to music therapy goals, such as tests of attention, memory, and language. Furthermore, I always incorporate informal observations during music sessions to assess engagement, participation, and progress, using a structured observation checklist. The initial assessment guides the design and ongoing modification of the treatment plan.
Q 4. How do you adapt music interventions to meet the specific needs of individuals with different cognitive impairments?
Adaptability is paramount. The music chosen, the activities used, and the level of complexity are all carefully tailored. For someone with severe attention deficits, I might start with simple rhythmic exercises using percussion instruments, gradually increasing the complexity as their attention span improves. For individuals with memory impairments, I might utilize song recall tasks or structured musical improvisation exercises. Clients with aphasia might benefit from melodic intonation therapy, where they sing phrases to improve verbal output. The key is to make the music therapy sessions enjoyable and challenging enough to promote cognitive growth without causing frustration. The process involves constant assessment and modification based on the client’s response.
Q 5. What are the key components of a successful music therapy session for cognitive rehabilitation?
A successful music therapy session for cognitive rehabilitation is a balanced blend of elements. First, it must be goal-oriented, directly targeting specific cognitive deficits. Secondly, it needs to be engaging and motivating, using music that the client enjoys and finds relevant. Thirdly, it should involve active participation from the client to maximize the therapeutic benefit. Fourthly, it should be structured yet flexible, allowing for spontaneous interaction and adaptation. Finally, there needs to be a strong therapeutic relationship built on trust and rapport. Consider a session where we work on verbal fluency with MIT; I’ll start by selecting songs the client enjoys and then we’ll work gradually on reciting the lyrics, progressing to spontaneous phrase generation within a musical framework. The key is finding that sweet spot between challenge and engagement.
Q 6. How do you measure the effectiveness of your music-based interventions?
Measuring effectiveness involves a combination of methods. Pre- and post-intervention assessments using standardized cognitive tests provide quantifiable data on improvements in attention, memory, or language. I also track qualitative data through observations and client self-reports on their perceived improvements and satisfaction. For instance, I might compare MoCA scores before and after a course of therapy. Additionally, I monitor the client’s participation and engagement throughout the sessions, which reflects the effectiveness of the chosen music and activities. This multi-faceted approach provides a comprehensive picture of the intervention’s success.
Q 7. Describe your experience working with clients with traumatic brain injuries.
Working with TBI clients presents unique challenges and rewards. The nature and severity of cognitive impairments following TBI are highly variable, demanding individualized treatment plans. Common challenges include attention deficits, memory problems, executive dysfunction, and emotional lability. Music therapy can target these deficits using techniques like rhythmic entrainment to improve attention, melodic cues to aid memory, and structured improvisation to enhance executive functions. I often incorporate elements of sensory integration to manage sensory overload, which is common in TBI. For example, I might use calming music with a client experiencing anxiety or agitated behavior. Each case requires a careful assessment and a flexible, adaptive approach, focusing on gradual progress and building the client’s confidence and independence. Seeing clients regain cognitive function and improve their quality of life is incredibly rewarding.
Q 8. How do you address emotional challenges faced by clients during cognitive rehabilitation?
Addressing emotional challenges in cognitive rehabilitation is paramount because emotional well-being significantly impacts cognitive function. Many clients experience frustration, anxiety, or depression due to their cognitive difficulties. We use music as a powerful tool to regulate emotions. For example, if a client is feeling anxious during a memory task, we might incorporate calming, slow-paced music to reduce their stress response. Conversely, upbeat music can be used to boost motivation and engagement. We also create a safe and supportive therapeutic environment where clients feel comfortable expressing their feelings. This might involve active listening, validating their experiences, and helping them identify and utilize coping mechanisms through musical expression. Sometimes, simply allowing the client to choose the music they listen to during a session empowers them and creates a sense of control.
One client, recovering from a stroke, experienced intense frustration during language therapy. By incorporating music she enjoyed, we were able to create a more relaxed atmosphere, allowing her to focus better on the therapeutic tasks. The familiar melody also provided a scaffolding for her impaired language abilities.
Q 9. What are the ethical considerations you prioritize when using music in cognitive rehabilitation?
Ethical considerations are central to my practice. Firstly, informed consent is crucial. Clients must fully understand the nature of music-based interventions, their potential benefits and risks, and their right to withdraw at any time. Confidentiality is paramount; all client information remains strictly protected. I carefully select music appropriate for the client’s cultural background and personal preferences, avoiding potentially triggering material. Furthermore, I am mindful of power dynamics and maintain a therapeutic relationship based on respect, empathy, and collaboration. I regularly reflect on my practice to ensure I am providing ethically sound and culturally sensitive care. If I encounter ethical dilemmas, I consult with colleagues and relevant ethical guidelines.
Q 10. How do you collaborate with other healthcare professionals in a cognitive rehabilitation team?
Collaboration is key in cognitive rehabilitation. I work closely with neuropsychologists, occupational therapists, speech-language pathologists, and physicians. Regular team meetings allow us to share information about client progress, adjust treatment plans, and ensure a holistic approach. For example, I might collaborate with a speech-language pathologist to incorporate melodic intonation therapy for aphasia recovery, or with an occupational therapist to address fine motor skills during rhythm-based activities. We utilize shared electronic medical records to maintain clear communication and continuity of care. A strong, collaborative relationship among team members is essential for optimizing client outcomes.
Q 11. Describe your experience using specific musical techniques (e.g., melodic intonation therapy, rhythmic auditory stimulation) in cognitive rehabilitation.
Melodic Intonation Therapy (MIT) is effective for individuals with aphasia (language impairment). It uses melodies and intonations to facilitate spoken language recovery. We start with simple melodies, gradually increasing complexity as the client improves. Rhythmic Auditory Stimulation (RAS) utilizes rhythmic cues to improve motor function, often used for gait rehabilitation. We use rhythmic music to help clients synchronize their movements with the beat, improving coordination and balance. For example, I’ve used RAS with a client struggling with hemiparesis (weakness on one side of the body), using rhythmic drumming to improve their gait and reduce their reliance on assistive devices. The structured nature of these techniques provides a strong framework for cognitive restructuring and motor skill improvement.
Q 12. Explain how you incorporate music therapy into different stages of cognitive rehabilitation.
Music therapy is integrated throughout the different stages of cognitive rehabilitation. In the initial assessment phase, music is used to gauge the client’s cognitive strengths and weaknesses, preferences, and emotional state. During the intervention phase, music-based tasks are tailored to the client’s specific cognitive deficits. For instance, memory exercises could involve recalling song lyrics, and attention training might involve following musical rhythms. In the maintenance phase, music helps clients consolidate their gains, preventing relapse, and promoting long-term independence. We often create personalized playlists for clients to use at home, and encourage active engagement with music in their daily lives. For example, a client struggling with executive functions may benefit from practicing organizational skills by learning to play a musical instrument.
Q 13. How do you handle situations where a client shows little progress or exhibits resistance to music therapy?
If a client shows little progress or resistance, I first explore the underlying reasons. Is the music inappropriate for their preferences? Are they experiencing emotional distress impacting their engagement? Are the therapeutic goals realistic and achievable? I may adjust the music selection, the therapeutic approach, or the overall goals in collaboration with the client and the treatment team. We might introduce different musical genres or instruments, or explore non-musical approaches alongside music therapy. Open communication and a willingness to adapt the therapy are crucial in these situations. Building rapport and establishing a strong therapeutic relationship are essential for overcoming resistance. If challenges persist, consulting with other specialists might be needed to rule out other contributing factors.
Q 14. What are the common challenges in delivering music-based cognitive rehabilitation and how do you overcome them?
Challenges include access to resources, time constraints, and variability in client responses. Limited access to qualified music therapists or specialized equipment can be a barrier. Time constraints within a busy rehabilitation schedule can make it difficult to dedicate sufficient time to music therapy. Finally, client responses vary significantly. What works well for one client might be ineffective for another, requiring flexibility and adaptability. To overcome these challenges, I prioritize efficient use of time, collaborate effectively with other healthcare professionals, utilize readily available resources (such as simple instruments or pre-recorded music), and remain flexible and responsive to individual client needs. Ongoing professional development and collaboration are crucial in refining techniques and overcoming such obstacles.
Q 15. Describe your knowledge of various cognitive domains (attention, memory, executive function) and how music targets them.
Cognitive rehabilitation using music targets various cognitive domains. Let’s look at attention, memory, and executive function.
Attention: Music engages attentional processes through its inherent rhythmic and melodic structure. For instance, rhythmic tapping exercises can improve sustained attention, while following a complex musical score improves selective attention. We might use a simple melody initially, gradually increasing complexity to challenge the client’s ability to focus.
Memory: Music can enhance both short-term and long-term memory. For short-term memory, we might use melodic intonation therapy (MIT), where verbal information is encoded into a melody. This aids recall. Long-term memory is targeted by associating personal memories with specific songs or musical themes. A client with memory difficulties might find it easier to recall an appointment if associated with a specific song.
Executive Function: This encompasses planning, problem-solving, and cognitive flexibility. Music-based interventions such as improvisation or composing simple musical pieces necessitate planning and problem-solving, improving executive functions. For instance, a client might be asked to compose a short piece of music based on certain emotional cues, promoting cognitive flexibility.
The specific musical interventions are always tailored to the client’s individual needs and abilities.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain your experience developing individualized music therapy plans based on client assessments.
Developing an individualized music therapy plan begins with a comprehensive assessment. This includes a detailed cognitive evaluation, identifying strengths and weaknesses in different cognitive domains, alongside musical preferences and abilities. I use standardized cognitive assessments and tailor-made musical tests to understand the client’s musical background and preferences.
For example, a client with difficulty in sustained attention might benefit from initially focusing on simple, repetitive rhythmic activities. As their attention improves, the complexity of the music and tasks is increased gradually. For a client with memory challenges, melodic intonation therapy could be incorporated.
The plan outlines specific goals (e.g., improve attention span by 15%), target cognitive areas, chosen musical interventions, frequency of sessions, and progress monitoring methods. It’s a collaborative process, ensuring the client feels empowered and actively involved.
Q 17. Describe your familiarity with evidence-based practices in music therapy for cognitive rehabilitation.
My practice is grounded in evidence-based practices. I stay updated on research in music therapy for cognitive rehabilitation. This includes studies on the efficacy of various music-based interventions for specific cognitive impairments.
For example, the use of melodic intonation therapy (MIT) for aphasia is well-supported by research, demonstrating its effectiveness in improving verbal fluency. Similarly, research supports the use of rhythm-based interventions for improving motor skills and attention in individuals with Parkinson’s disease. I regularly consult peer-reviewed journals and attend conferences to ensure my interventions are aligned with the latest research findings and best practices.
Q 18. How do you document and report on the progress of clients undergoing music-based cognitive rehabilitation?
Documentation is crucial. I maintain detailed session notes recording the client’s participation, responses to interventions, and observed progress. This includes qualitative observations (e.g., increased engagement, improved accuracy in tasks) and quantitative data (e.g., scores on cognitive tests administered before and after the intervention).
Reports are generated regularly, summarizing the client’s progress, challenges encountered, and modifications made to the treatment plan. These reports are shared with the client, their family, and other healthcare professionals involved in their care, ensuring transparency and collaborative management.
For example, I might use a standardized progress monitoring tool to track changes in attention span or memory performance over time, supplementing this with qualitative observations that enrich the overall understanding of the client’s progress.
Q 19. What are the contraindications for using music therapy in cognitive rehabilitation?
While generally safe, contraindications exist. Music therapy should be avoided or modified in cases where:
The client experiences severe auditory sensitivity or pain from certain sounds. We would need to adjust the volume or the type of music used.
The client has significant emotional distress that is not adequately addressed. The music therapy session might exacerbate the emotional distress unless handled appropriately by a trained professional.
The client has active medical conditions that could be negatively impacted by the activities involved in music therapy (such as heart conditions, impacting physical exertion during rhythmic activities).
A thorough assessment is crucial to identify and manage any potential contraindications. In such cases, modifications to the music therapy plan or referral to other specialists may be necessary.
Q 20. Describe your experience working with diverse populations in cognitive rehabilitation.
I have worked with a diverse range of populations, including individuals with traumatic brain injury, stroke, Alzheimer’s disease, Parkinson’s disease, and developmental disabilities. Each population presents unique challenges and requires a tailored approach.
For instance, working with individuals with Alzheimer’s requires utilizing familiar songs and engaging in simple, repetitive musical activities. In contrast, working with individuals post-stroke might involve more focused exercises targeting specific cognitive deficits like language or motor skills. Cultural sensitivity is paramount. I adapt my interventions to respect the client’s cultural background and musical preferences. I may incorporate music from their cultural heritage to enhance engagement and therapeutic benefits.
Q 21. How do you maintain your professional development in music therapy for cognitive rehabilitation?
Maintaining professional development is an ongoing commitment. I regularly attend conferences and workshops related to music therapy and cognitive rehabilitation. I actively participate in continuing education courses, focusing on the latest research findings and innovative therapeutic techniques.
I also engage in peer supervision and collaborate with other professionals in the field to share knowledge and best practices. Staying current with research articles in peer-reviewed journals ensures I’m using the most effective methods. These continuous learning opportunities ensure I provide the highest quality of care for my clients.
Q 22. Explain your understanding of the role of music in neuroplasticity.
Music’s role in neuroplasticity is profound. Neuroplasticity refers to the brain’s remarkable ability to reorganize itself by forming new neural connections throughout life. Music, with its multifaceted nature, acts as a powerful stimulus, engaging various brain regions simultaneously. This multi-sensory engagement – auditory processing, motor skills (if playing an instrument), emotional responses, and cognitive aspects like memory and attention – triggers a cascade of neural activity.
For instance, learning a new musical piece strengthens memory networks. Playing an instrument enhances fine motor skills and coordination, impacting motor cortex plasticity. Singing improves respiratory function and articulation, impacting speech areas. The emotional engagement through music can even modulate mood and reduce stress, influencing areas related to emotional regulation.
Think of it like this: just as regular exercise strengthens muscles, musical engagement strengthens neural pathways. The more frequently and intensely these pathways are activated through musical activities, the stronger and more efficient they become, leading to improved cognitive function.
Q 23. What are some limitations of music therapy for cognitive rehabilitation?
While music therapy offers significant benefits, certain limitations exist. Firstly, not all individuals respond equally to music. Musical preferences, pre-existing conditions, and the severity of cognitive impairment can influence the effectiveness of treatment. A client with profound aphasia, for example, might struggle to engage with even simple singing activities.
Secondly, music therapy is often time-consuming and requires a dedicated, trained therapist. This can present access challenges and financial constraints for some individuals. Furthermore, measuring the precise impact of music therapy on specific cognitive functions can be difficult, requiring robust assessment tools and longitudinal studies. Lastly, the subjective nature of the therapeutic experience makes standardized outcomes challenging to establish definitively across diverse populations.
For example, while I’ve seen incredible improvements in attention span in some clients using rhythmic drumming, others might experience minimal changes. Careful assessment and adaptation are crucial to overcome these limitations.
Q 24. How do you ensure the safety and well-being of your clients during music therapy sessions?
Safety and well-being are paramount. Before commencing any music therapy session, I conduct a thorough assessment of the client’s physical and cognitive abilities. This includes reviewing medical history, current medications, and any potential physical limitations. I create a safe, comfortable, and accessible environment, free from hazards. If a client exhibits signs of fatigue, discomfort, or distress, I adjust the session accordingly or terminate it if necessary.
For clients with physical limitations, I adapt instruments or activities to ensure their safety and comfort. For example, a client with limited mobility might use adapted percussion instruments or participate in listening and singing activities rather than playing demanding instruments. Throughout the session, I monitor the client’s vital signs (if necessary), provide frequent breaks, and maintain clear communication to ensure they are comfortable and engaged.
I also involve family members or caregivers in the process, explaining session goals and providing them with resources to support the client’s well-being both during and after the sessions.
Q 25. Describe your proficiency in musical instruments and your ability to adapt your approach based on client preferences.
I am proficient in several instruments, including piano, guitar, and various percussion instruments. This allows me to adapt my approach to individual client preferences and abilities. If a client enjoys singing, we might focus on vocal exercises and song-based activities. If they prefer instrumental music, we can explore playing various instruments, from simple rhythm instruments to more complex melodic instruments. The key is to build on the client’s strengths and interests to enhance engagement and motivation.
For instance, one client with limited fine motor control enjoyed playing simple hand drums, while another with excellent vocal skills thrived with singing therapeutic songs. My adaptability ensures that every session is tailored to the individual needs and capabilities of the client, optimizing the effectiveness of the intervention.
Q 26. How do you create a therapeutic and supportive environment for clients during music-based interventions?
Creating a therapeutic and supportive environment is crucial. This involves establishing a trusting relationship with the client, ensuring confidentiality, and fostering a non-judgmental atmosphere. The session space should be comfortable, well-lit, and appropriately equipped with instruments and assistive devices if needed. I use calming music or ambient sounds to create a relaxing ambiance.
I actively encourage client participation, tailoring the session to their individual pace and preferences. Positive reinforcement and encouragement are crucial elements of my approach. I actively listen to the client’s verbal and non-verbal cues, adapting the session as needed to ensure their comfort and engagement. I believe a supportive, empathetic approach greatly contributes to a positive therapeutic experience.
Q 27. Describe your experience with technology-assisted music therapy approaches for cognitive rehabilitation.
I have extensive experience integrating technology into music therapy for cognitive rehabilitation. This includes utilizing music software for creating personalized playlists, music notation software for composition and improvisation exercises, and brain-computer interfaces (BCIs) for assessing and training neural responses to music. For example, I’ve successfully used apps that allow clients to create their own personalized music using simple interfaces, fostering creativity and improving cognitive function.
Furthermore, I utilize virtual reality (VR) technology to enhance immersion in therapeutic musical activities. VR can create engaging and stimulating environments that are impossible to replicate in a traditional setting, particularly beneficial for clients with limited mobility or attention span. I am constantly exploring and evaluating new technologies to enhance the effectiveness and accessibility of music therapy interventions.
Q 28. How do you adapt your communication style to meet the individual needs and communication abilities of clients?
Adapting my communication style is crucial. I assess each client’s communication abilities and preferences before initiating therapy. This involves observing their verbal and non-verbal cues, understanding their cognitive limitations, and determining the most effective way to communicate therapeutic goals and instructions. For clients with aphasia, I may use visual aids, gestures, and simple language. For clients with cognitive impairments, I utilize repetitive cues and structured activities.
I also involve family members or caregivers to gain further insight into the client’s communication patterns and preferences. Building a strong rapport through clear, empathetic communication ensures trust and fosters collaboration, allowing the client to actively participate in their therapeutic journey. I find that patience, flexibility, and creative communication strategies are essential for working with diverse populations.
Key Topics to Learn for Cognitive Rehabilitation using Music-Based Interventions Interview
- Neurological Foundations: Understanding the impact of music on brain plasticity and cognitive function. Explore the neural pathways involved in music processing and their relationship to cognitive skills.
- Therapeutic Approaches: Mastering various music-based techniques for cognitive rehabilitation, including melodic intonation therapy (MIT), rhythmic auditory stimulation (RAS), and music therapy for attention and memory deficits. Consider different musical styles and their applications.
- Assessment & Treatment Planning: Learn to conduct thorough assessments of cognitive abilities and tailor music-based interventions to individual patient needs and goals. This includes identifying appropriate assessment tools and documenting progress.
- Practical Application: Develop proficiency in designing and implementing music therapy sessions, adapting techniques based on patient responses, and effectively utilizing various musical instruments and technologies.
- Evidence-Based Practice: Familiarize yourself with current research and evidence supporting the effectiveness of music-based interventions for various cognitive impairments. Be prepared to discuss relevant studies and their implications for practice.
- Ethical Considerations: Understand the ethical implications of music therapy practice, including confidentiality, informed consent, and cultural sensitivity.
- Interdisciplinary Collaboration: Discuss the importance of collaborating with other healthcare professionals (e.g., neurologists, occupational therapists, speech therapists) in a holistic rehabilitation approach.
- Case Study Analysis: Prepare to analyze case studies involving music-based interventions, demonstrating your ability to critically evaluate treatment approaches and outcomes.
Next Steps
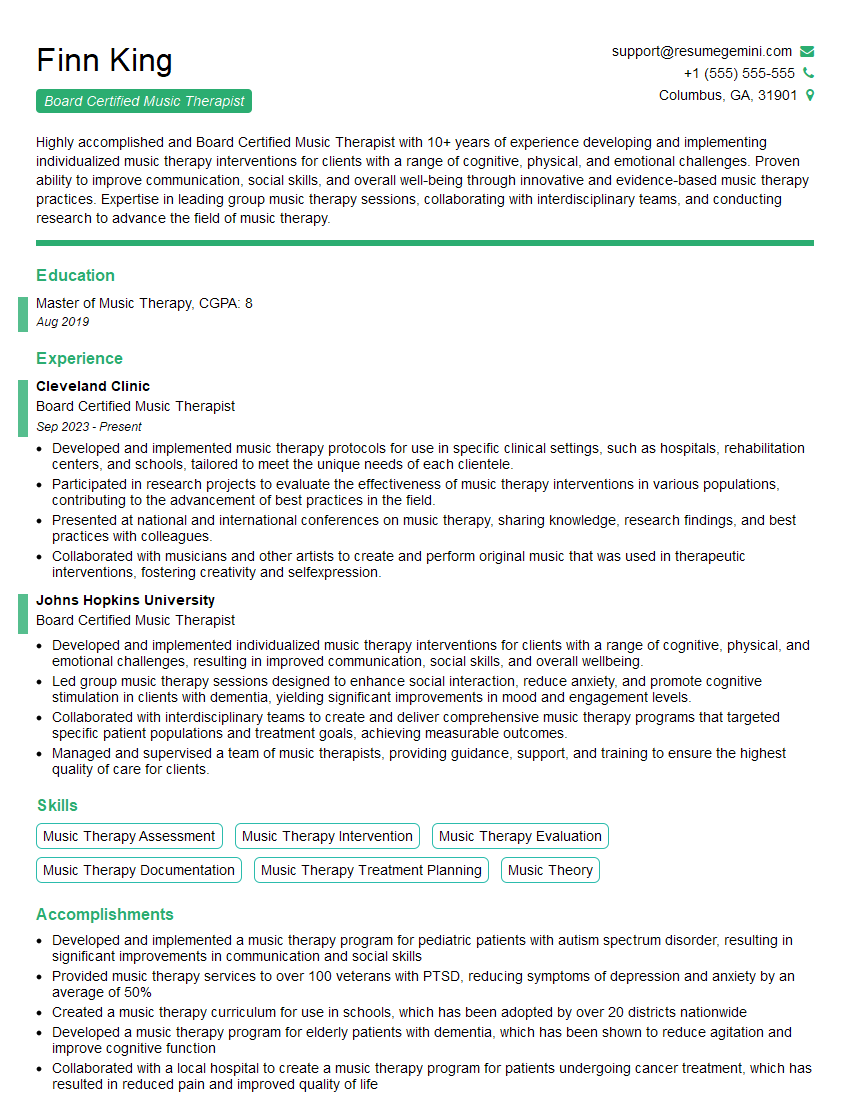
Mastering cognitive rehabilitation using music-based interventions opens doors to a rewarding career with significant impact on patients’ lives. To maximize your job prospects, it’s crucial to present your skills and experience effectively. Creating an ATS-friendly resume is key to getting noticed by potential employers. ResumeGemini is a trusted resource that can help you build a professional and impactful resume. They offer examples of resumes tailored specifically to Cognitive Rehabilitation using Music-Based Interventions, ensuring your application stands out.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.