The right preparation can turn an interview into an opportunity to showcase your expertise. This guide to Collaboration with Educators and Medical Professionals interview questions is your ultimate resource, providing key insights and tips to help you ace your responses and stand out as a top candidate.
Questions Asked in Collaboration with Educators and Medical Professionals Interview
Q 1. Describe your experience developing and implementing collaborative projects between educators and medical professionals.
My experience in developing and implementing collaborative projects between educators and medical professionals spans over a decade. I’ve been involved in designing and delivering numerous continuing medical education (CME) programs, interprofessional education (IPE) initiatives, and curriculum development projects for healthcare settings. These projects typically involve bringing together medical doctors, nurses, pharmacists, allied health professionals, and educators from various disciplines. A key aspect of my approach is establishing clear project goals and timelines from the outset. For instance, in one project focused on improving diabetes management, we collaboratively defined learning objectives, developed engaging curriculum materials (including interactive simulations and case studies), and established methods for evaluating participant learning and program effectiveness. This involved numerous meetings, careful consideration of each profession’s perspectives, and iterative feedback loops.
Another example involved creating a simulation-based training program for emergency room staff to handle pediatric trauma cases. Here, collaboration with educators ensured the pedagogical approach was effective, while input from medical professionals guaranteed the clinical content’s accuracy and relevance. The success of these projects hinges on effective communication, shared decision-making, and mutual respect for the expertise each party brings to the table. We consistently used project management tools and regular check-in meetings to ensure we stayed on track and addressed any challenges proactively.
Q 2. How do you ensure effective communication and information sharing between educators and medical teams?
Effective communication and information sharing are crucial for success. I employ a multi-pronged approach. This includes establishing regular meetings – both formal and informal – using a variety of communication channels such as email, video conferencing (Zoom, Teams), and project management platforms (Asana, Trello). We create a central repository for all project-related documents and resources, ensuring everyone has access to the latest information. Using a shared online platform improves transparency and accountability. Further, I emphasize active listening and clear, concise communication, encouraging all participants to express their perspectives and concerns openly. This is particularly important when bridging the gap between educational theory and medical practice. For example, during a project focused on telehealth implementation, regular check-ins and the use of a shared online document facilitated quick issue resolution and minimized misunderstandings between educators developing the training materials and physicians integrating them into practice.
We also utilize various visual aids like flowcharts and diagrams to clarify complex information and processes. Finally, establishing clear communication protocols and roles upfront helps to avoid confusion and delays.
Q 3. Explain your approach to resolving conflicts or disagreements that may arise during collaborative projects.
Conflicts are inevitable in collaborative projects. My approach prioritizes open communication and respectful dialogue. First, I create a safe space for expressing differing opinions. I encourage active listening and reframing disagreements as opportunities for learning and improvement. Rather than focusing on assigning blame, I focus on identifying the root causes of the conflict and collaboratively seeking solutions. When necessary, I employ conflict resolution techniques such as mediation or facilitated discussions, ensuring a fair and impartial process. For example, in one project involving the design of a new healthcare curriculum, disagreements arose regarding the weighting of different learning objectives. Through facilitated discussions, we identified the underlying values and priorities of different stakeholders. This led to a compromise that satisfied all parties involved.
Documentation is also crucial. Maintaining clear records of decisions, agreements, and any unresolved issues facilitates accountability and prevents future misunderstandings. If a consensus cannot be reached, escalation protocols are defined and followed to ensure timely resolution.
Q 4. Describe a time you had to adapt a healthcare education program to meet the needs of a specific learning group.
In one instance, we developed a healthcare education program on palliative care for nurses working in a rural setting. The initial program, designed for urban hospital settings, was found to be irrelevant and impractical for the rural nurses, due to limited resources and different patient demographics. We needed to adapt it. Through interviews and focus groups with the target audience, we discovered their primary needs were focused on practical skills and decision-making in resource-constrained environments. We adjusted the program accordingly. We reduced the emphasis on theoretical frameworks and increased the focus on practical skills training through simulations, case studies reflecting their reality, and the incorporation of telehealth technologies. The revised curriculum utilized readily available resources and emphasized community engagement. This adaptation significantly improved participant engagement and learning outcomes.
Q 5. How do you assess the effectiveness of collaborative healthcare education initiatives?
Assessing the effectiveness of collaborative healthcare education initiatives is crucial. We use a multi-faceted approach combining qualitative and quantitative methods. Quantitative data includes pre- and post-tests to measure knowledge gain, surveys to assess participant satisfaction, and tracking of program participation rates. Qualitative data is gathered through focus groups, interviews with participants, and feedback from instructors and medical professionals. This provides a more nuanced understanding of the program’s impact. For instance, in the palliative care program mentioned earlier, we not only measured the nurses’ knowledge gain through pre- and post-tests, but we also conducted post-program interviews to ascertain how the training impacted their actual practice. We also tracked the number of patients they reported receiving improved care due to the improved knowledge and skill.
Regular monitoring and evaluation are crucial, allowing for adjustments during and after implementation. This iterative process allows for continual program improvement. This data-driven approach is essential for demonstrating the value of collaborative initiatives to stakeholders and securing future funding.
Q 6. What strategies do you employ to build and maintain strong relationships with educators and medical professionals?
Building and maintaining strong relationships is paramount. This involves building trust and respect among all participants. I achieve this through clear communication, active listening, shared decision-making, and valuing diverse perspectives. I regularly acknowledge the contributions and expertise of all team members. This fosters a sense of collaboration and mutual respect. Informal interactions, such as team lunches or social events, create opportunities for relationship building outside the formal project context. Building rapport through personal connection goes a long way in resolving conflicts and ensuring project success. For example, I maintain open communication channels beyond formal meetings, ensuring quick responses to concerns. This ensures open lines of communication throughout the project’s lifecycle.
Regular feedback and recognition of individual accomplishments are also important for maintaining motivation and engagement.
Q 7. How do you navigate ethical considerations in collaborative healthcare education settings?
Ethical considerations are paramount in healthcare education. In collaborative settings, we must address issues such as patient confidentiality, data privacy, and conflict of interest. We establish clear ethical guidelines at the outset of each project, ensuring compliance with relevant regulations and professional standards. This involves obtaining appropriate ethical approvals for research or data collection activities. For example, in projects involving patient data, we ensure anonymization and de-identification of all data, maintaining patient privacy in accordance with HIPAA regulations.
Transparency is key. We ensure all participants understand their roles and responsibilities concerning ethical conduct. We also establish mechanisms for reporting and addressing ethical concerns that may arise during the project. Regular ethical reviews ensure that the project aligns with ethical principles throughout its lifecycle. This proactive approach is essential for maintaining integrity and trust in all collaborative endeavors.
Q 8. Describe your experience with implementing evidence-based practices in a collaborative setting.
Implementing evidence-based practices in collaborative settings requires a systematic approach. It starts with identifying a clear need or problem, then researching existing evidence to determine the most effective interventions. This often involves reviewing peer-reviewed literature, analyzing data from previous projects, and consulting with experts in the field.
For example, in a project addressing childhood obesity, we collaborated with educators and medical professionals to implement a school-based program incorporating physical activity and nutritional education. We based the program’s design on evidence from studies showing the effectiveness of these interventions. We tracked participation rates, BMI changes, and dietary improvements, constantly evaluating the program’s effectiveness and making data-driven adjustments. This iterative process, rooted in evidence and guided by collaboration, ultimately led to significant improvements in students’ health outcomes.
The key is continuous monitoring and evaluation to ensure the chosen practices remain effective and aligned with the latest research. This involves regular data analysis and open communication among all collaborators.
Q 9. Explain your understanding of different learning styles and how you adapt your teaching methods accordingly.
Understanding different learning styles is crucial for effective teaching. Learners process information differently; some are visual, some auditory, and others kinesthetic. Ignoring these differences can limit learning and engagement.
- Visual learners benefit from diagrams, charts, and videos.
- Auditory learners thrive with lectures, discussions, and audio recordings.
- Kinesthetic learners learn best through hands-on activities, experiments, and role-playing.
In my teaching, I adapt my methods by incorporating diverse learning modalities. For instance, during a session on patient communication, I might use a video demonstrating effective techniques for visual learners, lead a group discussion for auditory learners, and have participants practice role-playing scenarios for kinesthetic learners. This ensures that all learners have opportunities to engage with the material in a way that suits their individual learning preferences.
Q 10. How do you incorporate technology to enhance collaboration between educators and medical professionals?
Technology plays a vital role in enhancing collaboration between educators and medical professionals. Secure platforms like video conferencing (Zoom, Teams), project management tools (Asana, Trello), and shared document repositories (Google Drive, SharePoint) facilitate seamless communication and information sharing.
For example, we utilized a secure video conferencing platform to conduct weekly meetings with educators and medical professionals from different locations to discuss curriculum development, share patient case studies, and provide feedback on teaching modules. We used a shared document repository to store and collaboratively edit lesson plans, presentations, and assessment materials. This ensured everyone had access to the latest information and could contribute effectively regardless of their physical location. Furthermore, educational simulation software can provide realistic clinical scenarios for medical students and allied health professionals to practice and receive immediate feedback.
Q 11. Describe your experience with using data to inform decision-making in collaborative healthcare education projects.
Data-driven decision making is essential in collaborative healthcare education. We use data from various sources, including student performance metrics (exams, clinical evaluations), feedback surveys, and patient outcome data, to assess program effectiveness and make necessary changes.
In a recent project focusing on improving diabetic patient management, we collected data on student knowledge pre- and post-intervention, patient HbA1c levels, and patient satisfaction scores. By analyzing this data, we identified areas where the program excelled and where improvements were needed. For instance, we discovered a knowledge gap in a specific area, prompting us to revise the curriculum and incorporate additional learning resources. This data-driven approach ensured our program was continuously refined and optimized to maximize its impact.
Q 12. How do you measure the impact of collaborative healthcare education programs on patient outcomes?
Measuring the impact of collaborative healthcare education programs on patient outcomes requires a multifaceted approach. We typically track key performance indicators (KPIs) directly related to patient health and well-being.
For instance, in a program focusing on improving stroke rehabilitation, we might measure patient functional independence, quality of life, readmission rates, and length of hospital stay. These metrics provide concrete evidence of the program’s effectiveness. We also incorporate patient feedback surveys to capture the patient perspective and ensure the program addresses their needs effectively. This comprehensive data collection and analysis allows us to demonstrate the value of our collaborative efforts in terms of tangible improvements in patient care.
Q 13. What experience do you have with curriculum development in a healthcare or educational setting?
My experience in curriculum development spans both healthcare and educational settings. I’ve been involved in designing and implementing curricula for various healthcare professions, including nursing, medical assisting, and physical therapy. This involves understanding learning objectives, selecting appropriate teaching methods, and creating assessments that accurately measure student learning.
For example, when developing a curriculum on patient safety, I collaborated with healthcare professionals to ensure the content was relevant and up-to-date. We incorporated real-world case studies, simulations, and interactive exercises to enhance student engagement and knowledge retention. The process involved iterative feedback loops with educators and practitioners to ensure the curriculum effectively prepared students for real-world practice.
Q 14. Describe your proficiency in using various communication technologies for collaborative work.
Proficiency in communication technologies is essential for successful collaborative work. I am adept at utilizing various platforms, including video conferencing tools (Zoom, Microsoft Teams, Google Meet), instant messaging (Slack, Microsoft Teams), project management software (Asana, Trello, Monday.com), and shared document platforms (Google Drive, SharePoint, Dropbox).
I understand the importance of selecting the appropriate tool for the task, ensuring secure communication channels, and following established protocols for information sharing. My ability to effectively communicate and collaborate across different technological platforms ensures seamless information flow and facilitates efficient teamwork, irrespective of geographical constraints.
Q 15. How do you ensure confidentiality and data security in collaborative healthcare projects?
Ensuring confidentiality and data security in collaborative healthcare projects is paramount. It requires a multi-layered approach encompassing technical, procedural, and ethical considerations. We must adhere strictly to regulations like HIPAA (in the US) and GDPR (in Europe).
- Technical Safeguards: This includes using encrypted communication channels (like secure email and video conferencing platforms with end-to-end encryption), robust access control systems (role-based access limiting data visibility to only those who need it), and secure data storage (cloud services with strong encryption and audit trails). For example, we might utilize a cloud platform like Microsoft Azure or AWS, configuring it with strict access permissions and data encryption at rest and in transit.
- Procedural Safeguards: This involves creating and strictly enforcing data handling protocols. This includes training all team members on data privacy best practices, implementing data breach response plans, and conducting regular security audits. For instance, we might establish clear guidelines on acceptable data sharing practices and regular training modules to ensure adherence.
- Ethical Safeguards: This is about fostering a culture of responsibility and accountability. It involves clearly defining data ownership and usage rights, obtaining informed consent from patients where necessary, and maintaining meticulous documentation of all data handling activities. For example, we might create a data governance board responsible for overseeing all data-related activities and resolving any ethical dilemmas.
A combination of these safeguards, regularly reviewed and updated, creates a robust system for protecting sensitive patient data.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What strategies do you use to manage multiple priorities and deadlines in a collaborative environment?
Managing multiple priorities and deadlines in a collaborative environment demands effective project management skills and tools. I typically employ a combination of strategies, focusing on clear communication, efficient task allocation, and proactive risk management.
- Prioritization Frameworks: I use methods like the Eisenhower Matrix (urgent/important) to categorize tasks and focus efforts on the most critical items first. This helps to avoid getting bogged down in less important tasks and ensures we meet the most pressing deadlines.
- Project Management Tools: I leverage tools like Asana, Trello, or Microsoft Project to track tasks, deadlines, and progress. These tools facilitate collaboration, enabling team members to update their progress in real-time and identify potential roadblocks proactively. For example, assigning specific tasks in Asana with due dates and designated owners aids in maintaining accountability.
- Regular Communication and Meetings: Frequent, concise check-in meetings help to monitor progress, identify potential delays, and make necessary adjustments. These meetings need clear agendas and well-defined action items. For example, a weekly team meeting focusing on key deliverables helps stay on track.
- Risk Management: Proactive identification and mitigation of potential risks, like unforeseen delays or resource constraints, is crucial. This involves regularly reviewing the project plan and developing contingency plans for addressing potential problems.
By combining these approaches, we can effectively manage multiple priorities, ensure timely completion of tasks, and deliver successful collaborative projects.
Q 17. How familiar are you with relevant health and education regulations and policies?
I am very familiar with relevant health and education regulations and policies. My understanding encompasses both federal and state/local regulations in the US, as well as international standards like GDPR. This knowledge is crucial to ensure ethical and legal compliance in all collaborative projects.
- HIPAA (Health Insurance Portability and Accountability Act): I have a thorough understanding of HIPAA’s privacy and security rules concerning protected health information (PHI). This includes knowledge of permitted disclosures, patient rights, and breach notification requirements.
- FERPA (Family Educational Rights and Privacy Act): I am well-versed in FERPA’s guidelines for protecting student educational records. This includes understanding the limits on disclosing student information without consent.
- GDPR (General Data Protection Regulation): I am familiar with GDPR’s requirements for data protection and privacy, especially relevant in international collaborations.
- State and Local Regulations: I understand that specific regulations vary by state and locality, and I always ensure compliance with the relevant laws for each project.
This knowledge allows me to design and execute collaborative projects that are legally sound and ethically responsible, prioritizing the privacy and rights of all stakeholders.
Q 18. Describe your experience working with diverse populations in a healthcare or educational setting.
I have extensive experience working with diverse populations in both healthcare and educational settings. This experience has taught me the importance of cultural sensitivity, adaptability, and inclusive communication.
- Healthcare: In previous roles, I worked on projects involving patients from various socioeconomic backgrounds, ethnicities, and levels of health literacy. This required me to tailor communication strategies, ensuring clear and accessible information regardless of the individual’s background. For instance, I adapted materials into multiple languages and utilized simpler language to improve understanding.
- Education: My experience in education involved collaborating with educators and students from diverse cultural and linguistic backgrounds. This required understanding different learning styles and implementing culturally relevant teaching methods. This included incorporating diverse perspectives into curriculum materials and adapting teaching methods to match learning styles of diverse student populations.
Understanding and respecting the diverse needs and experiences of each individual is fundamental to fostering effective collaboration and achieving positive outcomes.
Q 19. How do you facilitate interprofessional teamwork among medical professionals and educators?
Facilitating interprofessional teamwork between medical professionals and educators requires a structured approach focusing on communication, shared goals, and mutual respect.
- Establish Clear Goals and Roles: Defining a shared vision and clearly outlining the roles and responsibilities of each team member ensures everyone understands their contribution to the overall project. This also helps avoid conflicts or misunderstandings.
- Foster Open Communication: Regular meetings and clear communication channels, such as dedicated project management software, are crucial. These channels must be used for updates, sharing of ideas, and addressing concerns openly and honestly.
- Promote Mutual Respect and Understanding: Recognizing the unique expertise and perspectives of each profession is paramount. This involves creating an environment of mutual respect where professionals from different backgrounds feel comfortable sharing their knowledge and expertise.
- Conflict Resolution Strategies: Developing strategies for addressing disagreements or conflicts is essential. This includes facilitating respectful discussions, encouraging active listening, and finding common ground. Using a mediator if necessary is also vital.
By emphasizing clear communication, shared goals, and mutual respect, we can cultivate a collaborative and effective interprofessional team.
Q 20. How do you incorporate feedback from educators and medical professionals to improve collaborative projects?
Incorporating feedback from educators and medical professionals is crucial to improving collaborative projects. I employ various methods to ensure feedback is gathered effectively and implemented constructively.
- Regular Feedback Mechanisms: Implementing formal feedback mechanisms like surveys, focus groups, and individual interviews allows for systematic collection of feedback throughout the project lifecycle. This is critical for iterative improvements.
- Constructive Feedback Sessions: Facilitating structured feedback sessions that encourage open discussion and critical analysis of the project’s progress and challenges. Using feedback methodologies like the ‘Start-Stop-Continue’ framework provides a structured approach.
- Actionable Implementation: Transforming feedback into actionable steps requires careful analysis and prioritization. Not all feedback is equally important, and understanding what needs immediate action and what can be addressed later is key. Documenting these decisions helps track progress.
- Transparent Communication: Communicating the implemented changes and the rationale behind them to all stakeholders ensures transparency and builds trust. This keeps everyone informed and fosters a sense of shared ownership.
A cycle of continuous feedback, analysis, and improvement ensures projects are refined to meet the needs and expectations of all stakeholders.
Q 21. Describe your experience with developing and delivering training programs for healthcare professionals or educators.
I have extensive experience developing and delivering training programs for both healthcare professionals and educators. This involves a needs assessment, curriculum development, and effective delivery techniques.
- Needs Assessment: Before developing any training, I conduct a thorough needs assessment to understand the knowledge gaps and training requirements of the target audience. This involves surveys, interviews, and reviewing existing materials.
- Curriculum Design: Using the needs assessment, I design a clear, well-structured curriculum. This involves defining learning objectives, selecting appropriate training methods (lectures, workshops, simulations, online modules), and creating engaging learning materials. Adult learning principles like active participation and real-world applications are key.
- Training Delivery: I adapt my delivery style to suit different audiences and learning preferences. I leverage interactive techniques like group discussions, case studies, and role-playing to ensure active participation and knowledge retention. Post-training assessments are crucial for evaluating effectiveness.
- Evaluation and Feedback: I consistently evaluate the effectiveness of the training programs through surveys, assessments, and observations. This feedback is used to refine the program and ensure it meets the evolving needs of participants.
My training programs are tailored to the specific needs of the audience, making them engaging, effective, and impactful.
Q 22. How do you handle situations where there is a conflict between educational goals and medical needs?
Resolving conflicts between educational goals and medical needs requires a delicate balance of empathy, clear communication, and a shared understanding of the patient’s best interests. It’s crucial to remember that education shouldn’t compromise necessary medical care, and vice-versa. A collaborative approach, involving all stakeholders – educators, medical professionals, and ideally, the patient or family – is essential.
Prioritization: We must carefully assess the urgency of both the educational and medical needs. Is immediate medical intervention necessary, potentially delaying educational activities? Or can educational elements be integrated into the medical care plan, such as incorporating learning opportunities during recovery time?
Flexibility and Adaptation: Rigidity in either approach is detrimental. We might need to adjust the educational plan to accommodate the patient’s current condition, breaking down learning into smaller, manageable sessions or employing alternative methods like audio learning if visual learning is compromised.
Open Communication: Regular communication between all parties keeps everyone informed of changes and progress. This might involve daily briefings, shared online documentation, or regular meetings. For example, I once worked with a child recovering from surgery who was struggling to keep up with schoolwork. We worked with the medical team to create a personalized learning plan that incorporated short, engaging activities that could be easily modified based on the child’s energy level and pain tolerance.
Q 23. Explain your understanding of the importance of shared decision-making in healthcare education.
Shared decision-making (SDM) is paramount in healthcare education because it empowers patients and their families, fosters trust and collaboration, and leads to better health outcomes. When educators and medical professionals engage in SDM, they actively involve patients in the development of their healthcare plan and educational strategies. This process respects patient autonomy and preferences, leading to increased adherence to treatment and learning plans.
Improved Compliance: Patients are more likely to follow treatment plans and engage in educational activities when they feel a sense of ownership and control.
Enhanced Trust: SDM demonstrates respect for the patient’s experience and knowledge, building rapport and trust between patients, educators, and clinicians.
Better Outcomes: Collaborative decision-making results in personalized approaches that better cater to the individual needs and preferences of the patient. For example, in a diabetes management program, SDM could involve discussions about preferred learning styles, dietary preferences, and lifestyle choices, resulting in a more effective and sustainable education plan.
Q 24. How would you address a situation where a medical professional disagrees with an educator’s approach to patient education?
Addressing disagreements requires a diplomatic approach that prioritizes the patient’s best interests and respects the expertise of both the medical professional and the educator. The key is to move away from a confrontational stance and embrace a collaborative problem-solving mindset.
Facilitated Discussion: I would organize a meeting involving all relevant parties, including the patient or guardian if appropriate. The goal isn’t to determine who is right or wrong, but rather to find common ground and a solution that benefits the patient.
Focus on Evidence and Patient Needs: The discussion should focus on the evidence-based rationale behind each approach and how it meets or doesn’t meet the specific needs of the patient. We might need to review relevant research or consult other specialists.
Compromise and Negotiation: Finding a compromise that integrates the strengths of both approaches is crucial. For instance, if a medical professional believes that certain educational activities are too taxing for a recovering patient, the educator might modify the approach to focus on shorter learning sessions or employ alternative methods.
Documentation: Any agreements reached must be documented clearly and shared with all stakeholders. This ensures that everyone is on the same page and facilitates consistent care.
Q 25. Describe a time you successfully negotiated a compromise to achieve a shared goal in a collaborative healthcare project.
In a project focused on improving diabetes education for underserved communities, a disagreement arose between the educators who favored group workshops and the medical professionals who preferred one-on-one counseling due to literacy concerns within the target population. Instead of choosing one approach, we explored a hybrid model.
We successfully negotiated a compromise that involved a series of introductory group workshops focusing on basic diabetes management. These workshops incorporated visual aids and simplified language. Following these group sessions, individual follow-up counseling was offered to address individual needs and literacy levels. This combination leveraged the strengths of both approaches, resulting in increased patient engagement and improved health outcomes. The compromise required mutual understanding, active listening, and a willingness to adjust our initial plans for the benefit of the project’s goals.
Q 26. How do you ensure that all participants in a collaborative project feel valued and respected?
Creating a collaborative environment where all participants feel valued and respected requires conscious effort and clear communication. This begins with setting the tone from the outset of the project.
Inclusive Planning: Engaging all stakeholders in the planning phase ensures that everyone’s perspectives and concerns are considered from the start. This includes ensuring diverse representation within the team.
Active Listening and Respectful Communication: Creating space for all voices to be heard, valuing different opinions, and employing active listening strategies during meetings and discussions are vital. Interrupting or dismissing someone’s contribution undermines their sense of value.
Recognition and Appreciation: Acknowledging individual and team accomplishments, both large and small, fosters a positive and motivating environment. This can be as simple as a verbal thank you or a formal acknowledgment during project updates.
Fair Distribution of Work and Responsibilities: Ensuring that the workload is distributed equitably, based on individual capabilities and expertise, promotes a sense of fairness and reduces feelings of being overburdened or undervalued.
Q 27. What are your strategies for fostering a culture of continuous improvement in collaborative healthcare education?
Fostering a culture of continuous improvement in collaborative healthcare education relies on a commitment to reflection, feedback, and adaptation. It’s not a one-time event but an ongoing process.
Regular Feedback Mechanisms: Establishing mechanisms for receiving feedback from all participants, including patients, educators, and medical professionals, is vital. This could involve surveys, focus groups, or individual feedback sessions.
Data-Driven Improvement: Regularly tracking and analyzing project outcomes, such as patient satisfaction, knowledge gained, and behavior changes, provides crucial data to inform improvements. This might involve examining patient surveys, assessing learning outcomes via testing or observation, and tracking adherence to treatment plans.
Professional Development Opportunities: Providing opportunities for professional development related to collaboration, communication, and educational best practices keeps the team engaged and improves their skills. This could involve workshops, conferences, or online training.
For example, in one project, we analyzed patient feedback and realized that our educational materials were too complex for some participants. We subsequently simplified the materials and incorporated more visual aids, leading to significantly better patient understanding and satisfaction.
Q 28. Describe your experience with documenting and reporting on the outcomes of collaborative projects.
Thorough documentation and reporting on collaborative projects are essential for demonstrating impact, improving future projects, and ensuring accountability. The method of documentation depends on the project’s size and complexity, but some key elements are consistent.
Project Plan and Timeline: A detailed project plan outlining goals, timelines, and responsibilities helps to track progress and identify any potential delays.
Meeting Minutes: Detailed minutes from all meetings document decisions, agreements, and action items.
Data Collection and Analysis: A robust system for collecting and analyzing relevant data is crucial for evaluating project outcomes. This might include patient satisfaction surveys, test scores, and health records.
Final Report: A comprehensive final report summarizes the project’s activities, outcomes, and any lessons learned. This report should be accessible to all stakeholders and should be formatted for easy understanding and dissemination.
For instance, in a recent project, we used a shared online platform to track progress, collect data, and share documentation with all stakeholders. This centralized approach greatly improved transparency and facilitated seamless collaboration.
Key Topics to Learn for Collaboration with Educators and Medical Professionals Interview
- Understanding Diverse Perspectives: Learn to appreciate the unique viewpoints and priorities of educators and medical professionals, recognizing their distinct professional languages and communication styles.
- Effective Communication Strategies: Practice clear, concise, and empathetic communication techniques tailored to different audiences. This includes active listening, adapting your message, and providing constructive feedback.
- Shared Goal Setting & Project Management: Explore methodologies for collaboratively defining project goals, assigning roles and responsibilities, and managing timelines effectively across interdisciplinary teams.
- Conflict Resolution & Negotiation: Develop strategies for proactively addressing disagreements and navigating conflicting priorities within a collaborative environment. Learn to find mutually beneficial solutions.
- Data Sharing & Confidentiality: Understand the ethical and legal considerations related to sharing sensitive information, complying with HIPAA and FERPA regulations where applicable, and maintaining patient/student privacy.
- Technological Proficiency: Familiarize yourself with common technologies used in educational and medical settings for collaboration (e.g., electronic health records, learning management systems). Understand their limitations and benefits.
- Advocacy & Interprofessional Collaboration: Explore the importance of advocating for patients/students and working effectively within interprofessional teams to improve health outcomes and educational experiences.
- Ethical Decision-Making in Collaborative Settings: Understand the ethical frameworks that guide collaborative decisions in complex situations involving educators and medical professionals.
Next Steps
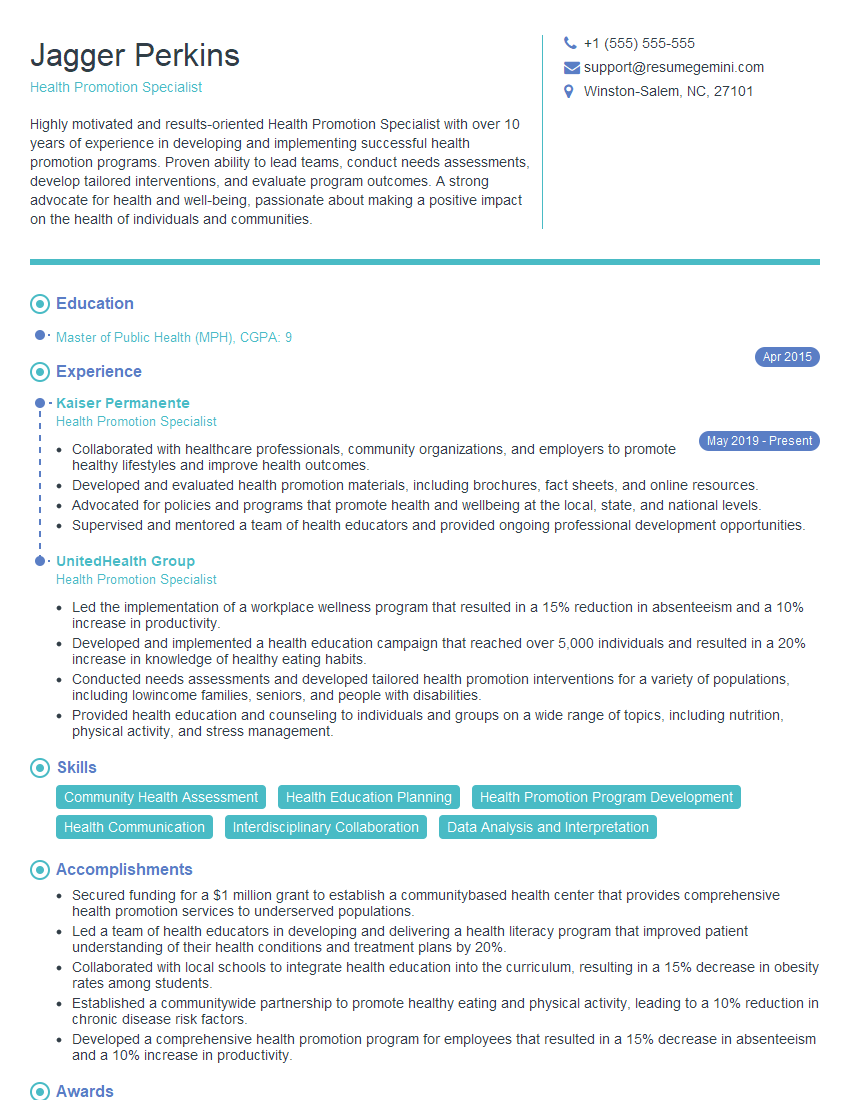
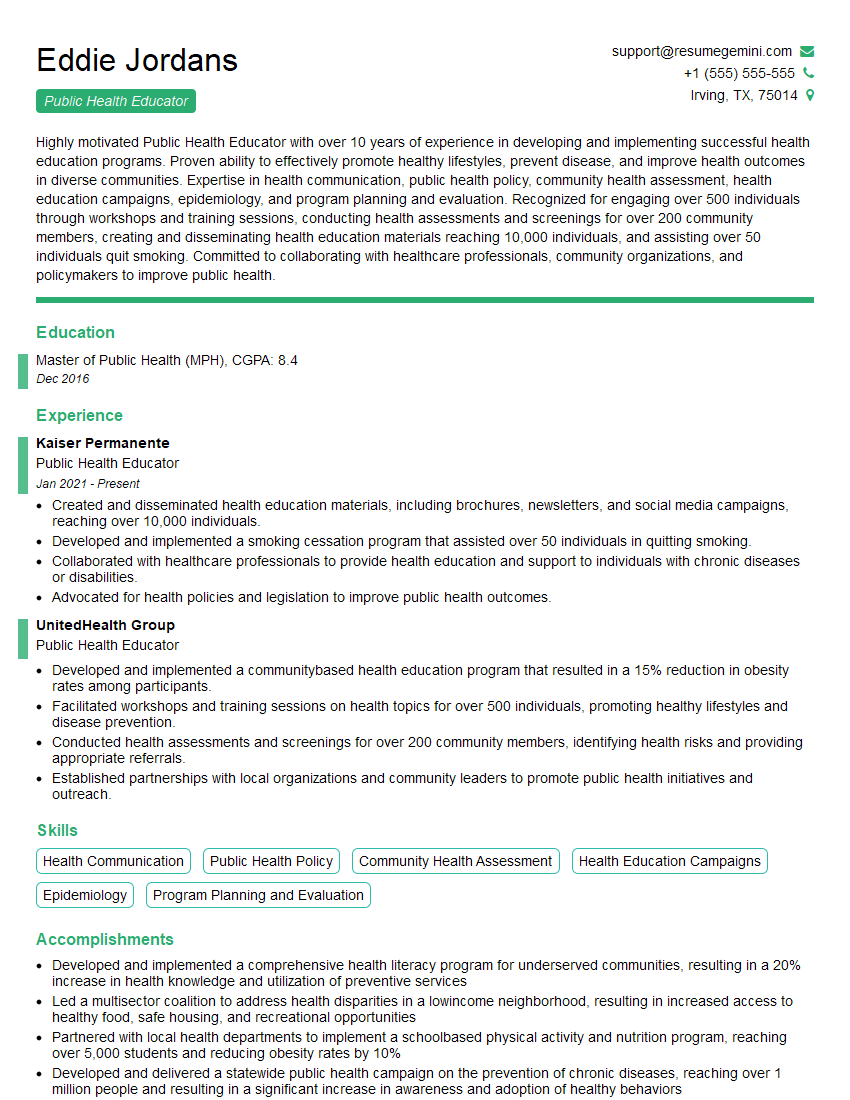
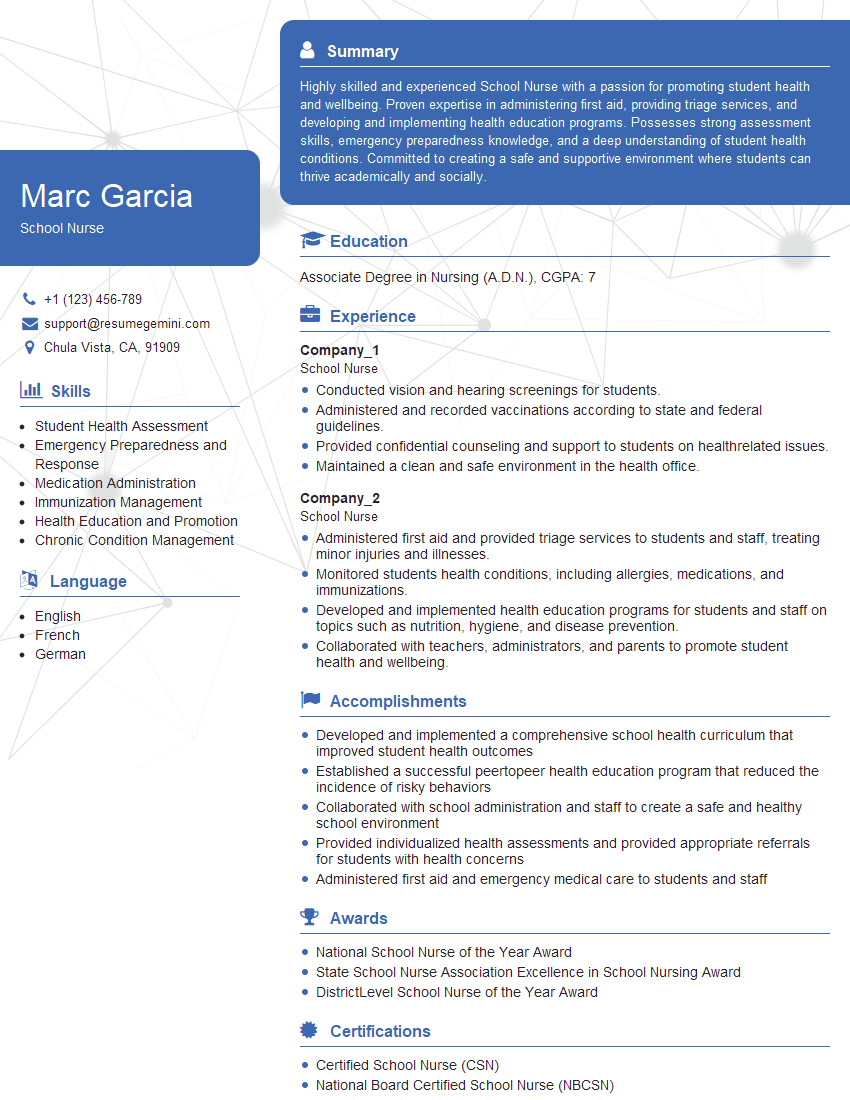
Mastering collaboration with educators and medical professionals is crucial for career advancement in many fields. It demonstrates essential soft skills and a deep understanding of interdisciplinary teamwork, significantly enhancing your value to any organization. To maximize your job prospects, it’s vital to create a strong, ATS-friendly resume that effectively showcases these skills. ResumeGemini is a trusted resource for building professional resumes that get noticed. We provide examples of resumes tailored to highlight experience in collaboration with educators and medical professionals, helping you present your qualifications in the best possible light. Take the next step in your career journey – build a standout resume with ResumeGemini today.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.