Cracking a skill-specific interview, like one for Collaborative Care with Medical Professionals, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Collaborative Care with Medical Professionals Interview
Q 1. Describe your experience implementing a collaborative care model in a healthcare setting.
In a previous role, I spearheaded the implementation of a collaborative care model for patients with depression and anxiety within a primary care setting. This involved integrating behavioral health specialists—specifically, licensed clinical social workers (LCSWs)—directly into the primary care team. We structured the model around a care manager who screened patients, identified those needing mental health support, and coordinated care between the primary care physician (PCP) and the LCSW. We used a shared electronic health record (EHR) system to facilitate seamless communication and documentation. The impact was remarkable. We saw a significant decrease in the number of patients requiring referral to outside specialists, shorter wait times for mental health services, and a demonstrable improvement in patient outcomes as measured by standardized depression and anxiety scales. This success was largely due to proactive care coordination and the establishment of clear communication protocols among team members.
Q 2. Explain the role of a care coordinator in improving patient outcomes within a collaborative care team.
The care coordinator is the linchpin of a successful collaborative care model. Think of them as the conductor of an orchestra, ensuring all instruments (healthcare professionals) play in harmony to achieve optimal patient outcomes. Their role encompasses several key responsibilities: patient screening and identification of mental health needs; scheduling and facilitating appointments with the behavioral health specialist; monitoring patient progress through regular check-ins; acting as a liaison between the PCP and the specialist, ensuring consistent communication and shared decision-making; tracking medication adherence and coordinating referrals to other necessary services; and educating patients about their condition and treatment plan. Effective care coordination reduces fragmentation of care, improves adherence to treatment plans, and ultimately leads to better patient outcomes—improved mental health, reduced hospitalizations, and enhanced quality of life.
Q 3. How do you manage conflicting priorities and competing demands within a collaborative care setting?
Managing conflicting priorities in a collaborative care setting requires a structured and organized approach. We employ several strategies: Prioritization frameworks such as the Eisenhower Matrix (urgent/important) help us focus on the most critical tasks first. Regular team meetings, using agendas and clear time allocation, allow for transparent discussion of competing demands and collaborative problem-solving. We also utilize project management tools to track tasks, deadlines, and individual responsibilities. Open and honest communication among team members is crucial. If a conflict arises between patient needs, we prioritize based on the urgency and severity of the situation, always ensuring patient safety and well-being are paramount. Regular reflection and adjustments to our workflows based on team feedback and workload analysis ensure we are constantly optimizing our processes.
Q 4. Describe your experience using electronic health records (EHRs) to facilitate communication within a collaborative care team.
Electronic health records (EHRs) are indispensable for facilitating communication in collaborative care. Our team uses a system that allows for shared access to patient records, enabling seamless communication between the PCP, behavioral health specialist, and care coordinator. We utilize the EHR for secure messaging, progress note sharing, and the tracking of key metrics such as attendance at appointments and medication adherence. Features such as structured progress notes, standardized templates for assessments and interventions, and embedded decision support tools greatly enhance efficiency and consistency in care. Regular training on EHR functionality is provided to all team members to ensure proficient use and maximize the system’s benefits. For example, using the EHR’s secure messaging, the LCSW can quickly update the PCP on a patient’s progress between appointments, preventing potential delays in care.
Q 5. How do you ensure patient confidentiality and compliance with HIPAA regulations in a collaborative care model?
Maintaining patient confidentiality and adhering to HIPAA regulations are paramount in collaborative care. We rigorously train all team members on HIPAA compliance, emphasizing the importance of protecting patient information. Secure communication channels, such as the EHR’s secure messaging system, are used exclusively for communication related to patient care. Access to patient data is strictly controlled, based on the principle of least privilege – meaning each team member only has access to the information they need to perform their specific role. We conduct regular audits to monitor compliance and address any potential breaches promptly. We also ensure all physical and electronic patient records are secured using appropriate safeguards, complying with all applicable HIPAA standards. Our commitment to patient privacy fosters trust and encourages open communication between patients and our team.
Q 6. Describe your approach to identifying and addressing barriers to care within a collaborative care framework.
Identifying and addressing barriers to care requires a multifaceted approach. We start by actively engaging patients through thorough assessments to understand their individual needs and challenges. These assessments explore practical barriers like transportation, financial constraints, or lack of childcare; social barriers such as stigma or social isolation; and systemic barriers including access to services or insurance coverage. Once identified, we develop collaborative solutions. This may involve connecting patients with transportation assistance, exploring financial aid programs, coordinating childcare services, or advocating for better access to services. Regular team meetings allow us to discuss and strategize around these barriers, often involving referral to community resources or advocacy groups. The focus is on building relationships based on trust and empowering patients to overcome these obstacles.
Q 7. How do you measure the effectiveness of a collaborative care intervention?
Measuring the effectiveness of collaborative care interventions relies on a combination of quantitative and qualitative data. Quantitatively, we track improvements in patient-reported outcomes such as depression and anxiety scores using validated questionnaires (e.g., PHQ-9, GAD-7) at baseline and regular intervals. We also monitor healthcare utilization data, such as hospitalizations and emergency room visits. Qualitatively, we gather patient feedback through surveys and focus groups to understand their experiences and satisfaction with the care received. We also analyze team data to evaluate workflow efficiency and identify areas for improvement. By integrating these different data sources, we gain a comprehensive understanding of the effectiveness of our collaborative care model and make data-driven adjustments to optimize outcomes. A key metric is reduction in depressive symptoms and improvement in functional status.
Q 8. Explain your understanding of the principles of shared decision-making in collaborative care.
Shared decision-making (SDM) in collaborative care is a cornerstone of patient-centered care. It’s not about the clinician deciding for the patient, but rather a partnership where the patient’s values, preferences, and goals are central to the treatment plan. This process involves a conversation where the clinician presents treatment options, explains the risks and benefits of each, and helps the patient understand the implications of their choices. The final decision rests with the patient, empowered by the information provided.
For example, imagine a patient with depression. SDM would involve the clinician explaining different treatment options – medication, therapy, or a combination – outlining the potential side effects and effectiveness of each. The clinician would then actively listen to the patient’s concerns, priorities, and lifestyle to jointly determine the best course of action. This might involve considering the patient’s work schedule, potential medication interactions with other drugs they are taking, or their personal preferences regarding therapy modalities. The aim is a plan that aligns with the patient’s life and preferences, increasing adherence and improving outcomes.
Q 9. How do you communicate effectively with patients, families, and other healthcare professionals in a collaborative care setting?
Effective communication in collaborative care requires a multi-faceted approach. With patients, I prioritize active listening, empathy, and clear, jargon-free explanations. I use plain language, check for understanding frequently, and encourage patients to ask questions. With families, I ensure they’re included in conversations as appropriate, respecting patient confidentiality while acknowledging the family’s role in support. Communication with other healthcare professionals relies on clear, concise documentation, regular team meetings, and a collaborative spirit. I utilize secure messaging systems for efficient and confidential communication regarding patient care. For example, if a patient is struggling with medication side effects, I will coordinate with the pharmacist and prescribing physician to adjust the medication or explore alternative options, ensuring all communication is well-documented and shared with the patient.
Q 10. How do you identify patients who would benefit most from collaborative care?
Identifying patients who benefit from collaborative care involves considering several factors. Patients with complex medical and/or behavioral health conditions, those struggling with medication adherence, or those experiencing persistent symptoms despite previous treatment often benefit greatly. Patients who demonstrate a high level of functional impairment and those with unmet social needs can be ideal candidates. A standardized screening tool can help identify patients at risk for poor outcomes and help triage appropriate level of care. For example, a patient with diabetes, anxiety, and difficulty managing their blood sugar might greatly benefit from a collaborative care model, where a behavioral health specialist works closely with the primary care physician to manage both the physical and mental health aspects of their care. This integrated approach improves medication adherence and overall health management.
Q 11. Explain your experience with different models of collaborative care (e.g., PCMH, integrated behavioral health).
I have extensive experience with various collaborative care models. The Patient-Centered Medical Home (PCMH) model emphasizes a team-based approach, providing comprehensive care coordination for patients. In my experience, the PCMH model has improved the patient’s experience and helped reduce hospital readmissions. Integrated behavioral health (IBH) models embed behavioral health professionals directly within primary care settings. This allows for easy access to mental health services and better coordination of care between physical and mental health providers, thereby improving the management of co-occurring disorders. I’ve also worked with models that incorporate community resources, like social workers to address non-medical barriers to care. Each model requires a unique approach to care coordination and communication. The success of any model relies on effective teamwork and shared decision-making.
Q 12. Describe your experience working with diverse populations in a collaborative care setting.
Working with diverse populations requires cultural humility and sensitivity. This involves recognizing the influence of culture, race, ethnicity, language, and socioeconomic status on patients’ health beliefs and behaviors. I prioritize using interpreters when needed, employing culturally appropriate communication styles, and adapting care plans to consider individual cultural preferences. For example, I’ve worked with patients from various cultural backgrounds who have varying beliefs about mental health treatment, so building trust through open communication and respecting diverse perspectives is crucial. Understanding a patient’s cultural context allows for a more effective and patient-centered approach to treatment. This is important to ensure that the care provided is relevant and acceptable to the individual and their community.
Q 13. How do you manage patient transitions of care within a collaborative care model?
Managing patient transitions of care within a collaborative care model requires meticulous planning and clear communication among all team members. I utilize tools like standardized discharge summaries, electronic health record systems, and regular follow-up communication with both patients and the care team involved in the transition. This ensures continuity of care and prevents gaps in service. For example, when a patient is discharged from the hospital, we ensure there’s a coordinated plan for medication reconciliation, follow-up appointments, and continued support from home health or other community resources. This might include specific instructions for the patient’s family members or caregivers, ensuring they understand the plan and can effectively support the patient’s recovery.
Q 14. How do you address ethical dilemmas related to patient care within a collaborative care team?
Ethical dilemmas in collaborative care often arise around issues of confidentiality, patient autonomy, and resource allocation. I approach these situations by actively involving the entire team in discussion, ensuring we are considering all perspectives. We refer to ethical guidelines and relevant policies when addressing complex issues. Open communication, respectful disagreement, and a commitment to the patient’s best interest are essential for navigating these challenges. For instance, if a patient discloses a plan that puts themselves or others at risk, a careful balance between respecting patient confidentiality and ensuring safety requires careful ethical consideration and collaboration among the team members. Ethical decision making in collaborative care requires a structured approach and clear communication within the team.
Q 15. How do you prioritize tasks and manage your workload effectively in a fast-paced healthcare environment?
In the fast-paced world of healthcare, effective prioritization is paramount. I utilize a combination of techniques to manage my workload. Firstly, I employ a prioritization matrix, categorizing tasks based on urgency and importance. This allows me to focus on critical, time-sensitive tasks first, ensuring timely interventions and preventing potential crises. Secondly, I leverage time-blocking techniques, scheduling specific time slots for particular tasks. This prevents task-switching, improves focus, and enhances overall efficiency. Thirdly, I regularly review my to-do list, adjusting priorities as needed based on emerging needs and shifting priorities within the collaborative care team. Finally, I proactively communicate with colleagues, delegating tasks where appropriate to optimize resource allocation. For example, if a patient needs a referral to a specialist urgently, that would naturally take precedence over a less urgent administrative task. This systematic approach keeps me organized and productive, even under pressure.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience developing and implementing care plans for patients with complex medical and behavioral health needs.
Developing and implementing care plans for patients with complex needs requires a holistic approach. I begin by conducting thorough assessments, considering the patient’s medical history, behavioral health status, social determinants of health, and personal preferences. This assessment informs the creation of individualized care plans that address both the medical and behavioral health aspects of the patient’s condition. For instance, a patient struggling with depression and diabetes might require integrated care focusing on medication management, therapy sessions, and lifestyle changes through a dietician. The plan details specific, measurable, achievable, relevant, and time-bound (SMART) goals, outlining interventions and monitoring strategies. Regular care team meetings are crucial for reviewing progress, adjusting the plan as needed, and ensuring effective communication. I actively involve the patient and their family in this process to promote adherence and improve outcomes. For example, using technology to provide remote monitoring and communication allows for flexible, personalized support and adjustments to the care plan based on real-time data.
Q 17. How do you use data and analytics to improve the performance of a collaborative care team?
Data and analytics are instrumental in optimizing collaborative care. We routinely collect data on patient outcomes, such as symptom improvement, medication adherence, and hospital readmission rates. This data is then analyzed to identify areas for improvement in our care processes. For example, if we notice a high rate of missed appointments for a particular patient population, we might analyze the scheduling process, transportation barriers, or patient communication methods to address the underlying issues. We use dashboards and reporting tools to visualize this data and track progress toward our goals. This data-driven approach allows us to make evidence-based decisions, refine our strategies, and demonstrate the effectiveness of our collaborative care model to stakeholders. For instance, a statistically significant improvement in patient outcomes, demonstrated through data analysis, strengthens our case for continued funding or program expansion.
Q 18. What are your strengths and weaknesses in a collaborative team setting?
My strengths in a collaborative team setting include excellent communication, active listening, and a proactive approach to problem-solving. I’m comfortable leading discussions, facilitating consensus, and mediating conflicts when they arise. I also strive to create a supportive and inclusive environment where all team members feel valued and heard. A weakness I’ve identified is sometimes being overly focused on detail, which can slow down decision-making processes. I’m actively working on this by learning to delegate tasks effectively and trust my team members’ expertise. This involves consciously prioritizing efficiency alongside accuracy, a skill I’ve developed by using project management tools and focusing on timely communication to keep the team aligned.
Q 19. How do you foster teamwork and collaboration among diverse healthcare professionals?
Fostering teamwork and collaboration requires a multifaceted approach. First, I prioritize open and transparent communication, ensuring everyone has access to relevant information and a platform to voice their opinions. Second, I create opportunities for team building and social interaction, strengthening relationships and fostering mutual respect. Third, I establish clear roles and responsibilities, reducing confusion and promoting accountability. Finally, I encourage a culture of mutual support and respect, emphasizing the importance of each team member’s contribution to the overall success of our efforts. For example, team-building activities, regular team meetings with dedicated time for informal discussions, and celebration of team successes help cultivate a positive and collaborative environment, enhancing team cohesion and effectiveness.
Q 20. Describe a challenging situation you faced in a collaborative care setting and how you resolved it.
In one instance, a patient’s care plan was causing conflict between the physician and the behavioral health specialist. The physician favored a primarily medication-focused approach, while the behavioral health specialist advocated for a stronger emphasis on therapy. To resolve this, I facilitated a structured meeting, ensuring both professionals had ample time to express their perspectives and concerns. I guided them towards a shared understanding of the patient’s needs, emphasizing the benefits of an integrated approach combining both medication and therapy. We collaboratively developed a revised care plan that incorporated elements from both viewpoints, prioritizing the patient’s overall well-being. This experience reinforced the importance of clear communication, active listening, and collaborative problem-solving in resolving conflicts within a collaborative care team.
Q 21. How do you handle conflict within a collaborative care team?
Conflict is inevitable in any team setting, especially when dealing with complex patients and diverse professional perspectives. My approach to conflict resolution involves: 1) Active listening: understanding each party’s perspective without judgment. 2) Identifying the root cause of the conflict: going beyond surface-level disagreements to find the underlying issues. 3) Facilitating open communication: creating a safe space for team members to express their feelings and concerns constructively. 4) Brainstorming solutions collaboratively: working together to develop mutually acceptable solutions. 5) Reaching a consensus: ensuring all parties agree on the chosen course of action. If the conflict persists, I may seek mediation from a neutral third party to facilitate resolution. The key is to approach conflict as an opportunity for growth and improvement, strengthening teamwork rather than undermining it.
Q 22. Describe your experience with telehealth in a collaborative care setting.
My experience with telehealth in collaborative care has been transformative. I’ve utilized telehealth platforms to deliver behavioral health services to patients integrated within primary care settings. This includes conducting initial assessments, providing ongoing therapy sessions, and coordinating care with primary care physicians and other members of the care team. For example, in a recent project, we used video conferencing to deliver Cognitive Behavioral Therapy (CBT) to patients with anxiety disorders. This allowed for increased access to care, particularly for patients in rural areas or with mobility issues. We also utilized secure messaging platforms for asynchronous communication, enhancing communication efficiency and reducing wait times for patient inquiries. The success of this approach was measured by improved patient outcomes, increased patient satisfaction, and cost-effectiveness compared to traditional in-person visits.
Furthermore, I’ve been involved in developing and implementing telehealth protocols to ensure patient privacy and data security, complying with HIPAA regulations. This includes training staff on the secure use of telehealth platforms and implementing appropriate safeguards to protect patient information.
Q 23. How do you ensure the sustainability of a collaborative care program?
Ensuring the sustainability of a collaborative care program requires a multi-pronged approach focusing on financial viability, operational efficiency, and continued quality improvement. Financial sustainability is achieved through securing consistent funding sources, such as grants, contracts with health insurance providers, and demonstrating cost-effectiveness through improved patient outcomes and reduced healthcare utilization. Operational efficiency involves streamlining workflows, optimizing staffing models, and leveraging technology to minimize administrative burden. A key component is the implementation of robust data tracking and analysis systems to monitor key performance indicators (KPIs) such as patient engagement, treatment adherence, and cost savings. For instance, we implemented a data dashboard that tracked patient outcomes and resource allocation, allowing us to identify areas for improvement and to justify continued funding based on demonstrable results. Finally, continuous quality improvement is crucial; regular program evaluation and adaptation based on feedback from patients and providers ensures the long-term effectiveness and relevance of the program.
Q 24. Explain your understanding of evidence-based practices in collaborative care.
Evidence-based practices in collaborative care are interventions and approaches supported by rigorous scientific research demonstrating their effectiveness in improving patient outcomes. This means relying on systematic reviews, meta-analyses, and randomized controlled trials to guide clinical decisions. For example, integrated behavioral health within primary care settings is an evidence-based approach proven to improve the management of chronic conditions like diabetes and hypertension by addressing the impact of behavioral factors on physical health. Specifically, using Cognitive Behavioral Therapy (CBT) for depression and anxiety within a primary care setting is a well-established evidence-based practice. My understanding of these practices includes not only familiarity with the research but also the ability to adapt them to diverse patient populations and clinical contexts. I regularly consult current research to stay abreast of the latest evidence and integrate it into our collaborative care model.
Q 25. How do you address cultural and linguistic barriers to care within a collaborative care model?
Addressing cultural and linguistic barriers is paramount in providing equitable and effective collaborative care. This involves creating a culturally competent team, utilizing culturally appropriate interventions, and ensuring access to language services. We build cultural competency through regular training for all team members on cultural awareness, sensitivity, and effective communication with diverse populations. This training emphasizes understanding the nuances of cultural beliefs and practices that might influence healthcare access and adherence. To address language barriers, we utilize bilingual staff and certified interpreters to ensure effective communication with patients who speak languages other than English. Furthermore, culturally sensitive materials are developed and made available to patients. For example, patient education materials are translated into multiple languages and adapted to reflect cultural norms. Finally, we ensure the availability of culturally appropriate support groups and community resources to enhance patient engagement and support.
Q 26. What are your salary expectations for this role?
My salary expectations for this role are commensurate with my experience, skills, and the market rate for similar positions. I am open to discussing a competitive salary range based on the specific details of the position and the overall compensation package. I’m more interested in a position that offers opportunities for growth, professional development, and a significant contribution to improving patient care.
Q 27. Describe your experience with performance improvement initiatives in collaborative care.
I have extensive experience in performance improvement initiatives within collaborative care. I’ve been involved in projects focusing on enhancing patient access to care, improving care coordination, and optimizing resource allocation. One notable project involved implementing a patient-centered medical home (PCMH) model, which led to significant improvements in patient satisfaction and chronic disease management. We utilized data-driven approaches, such as Plan-Do-Study-Act (PDSA) cycles, to systematically test and refine our interventions. For example, we implemented a new care pathway for patients with diabetes, which incorporated elements of motivational interviewing and telehealth support. Through rigorous monitoring of KPIs, we demonstrated a reduction in A1C levels and improved patient adherence to medication regimens. The success of this initiative involved collaboration with all team members, regular monitoring of process measures, and a focus on continuous quality improvement.
Q 28. What are your career goals related to collaborative care?
My career goals center on advancing collaborative care models to enhance the quality and accessibility of mental and behavioral healthcare services. I aspire to lead and mentor teams in developing and implementing innovative programs that improve patient outcomes and reduce healthcare disparities. This involves actively participating in research, disseminating best practices, and advocating for policies that support integrated care. Ultimately, I want to make a significant contribution to shaping the future of collaborative care, ensuring that all individuals have access to high-quality, coordinated, and culturally sensitive care.
Key Topics to Learn for Collaborative Care with Medical Professionals Interview
- Understanding the Collaborative Care Model: Explore the principles and philosophies underpinning collaborative care, including shared decision-making and patient-centered approaches.
- Interprofessional Communication & Teamwork: Practice effective communication strategies for interacting with physicians, nurses, social workers, and other healthcare professionals. Consider scenarios requiring conflict resolution and consensus building.
- Patient-Centered Care Planning & Implementation: Develop your understanding of creating and executing individualized care plans that integrate the expertise of various healthcare providers. Focus on patient engagement and shared goals.
- Ethical Considerations in Collaborative Care: Familiarize yourself with ethical dilemmas that may arise in team-based care, including confidentiality, informed consent, and resource allocation.
- Data Management & Documentation in Collaborative Care: Understand the importance of accurate and timely documentation within a collaborative care setting and the use of electronic health records (EHRs).
- Measuring Outcomes and Evaluating Effectiveness: Learn about methods for assessing the effectiveness of collaborative care interventions and using data to drive improvements in patient care.
- Addressing Challenges in Collaborative Care: Prepare to discuss potential barriers to successful collaboration (e.g., communication breakdowns, differing professional perspectives, system limitations) and strategies to overcome them.
- Technology and its role in Collaborative Care: Understand how telehealth, electronic communication tools and other technologies support and enhance collaborative care delivery.
Next Steps
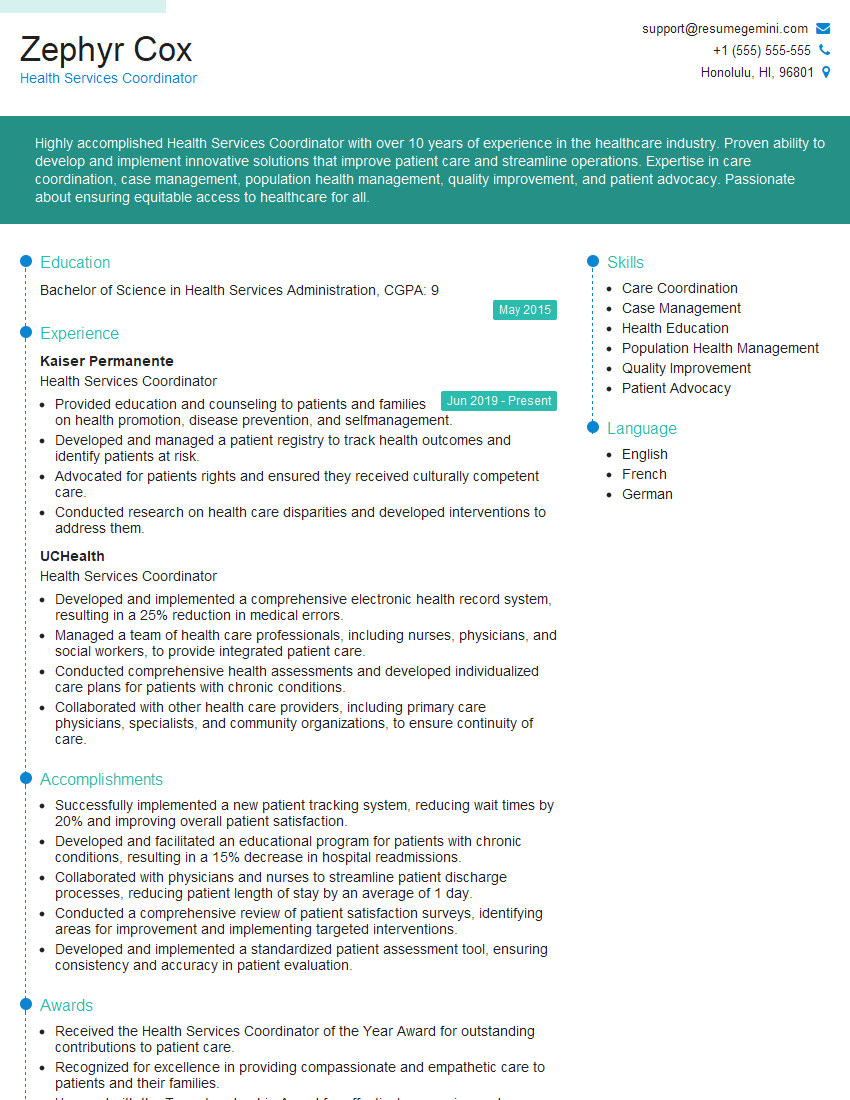
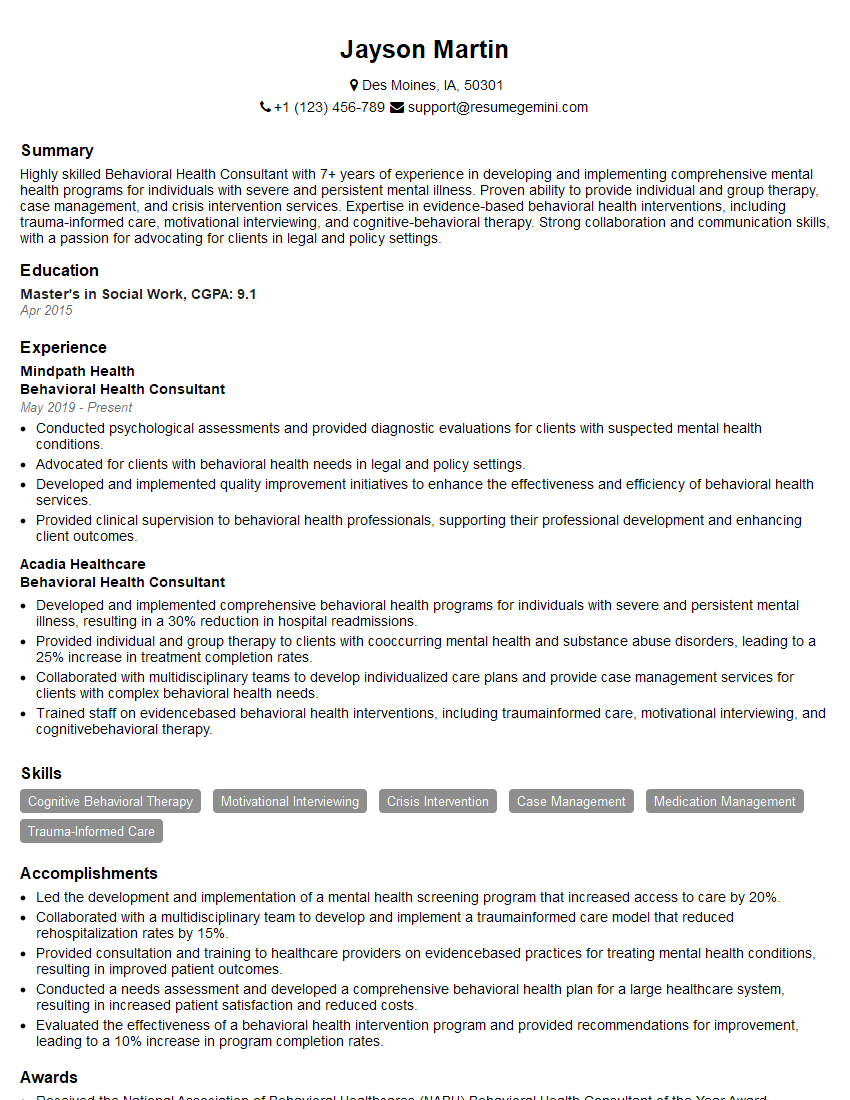
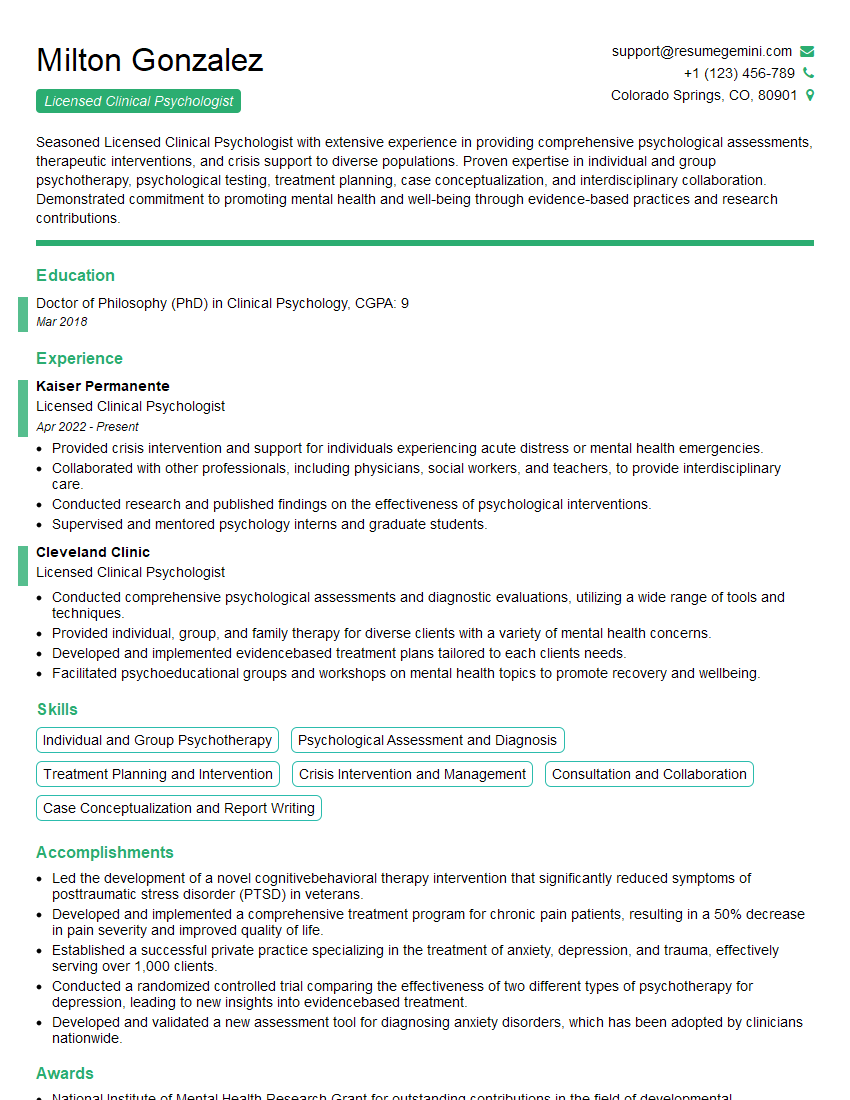
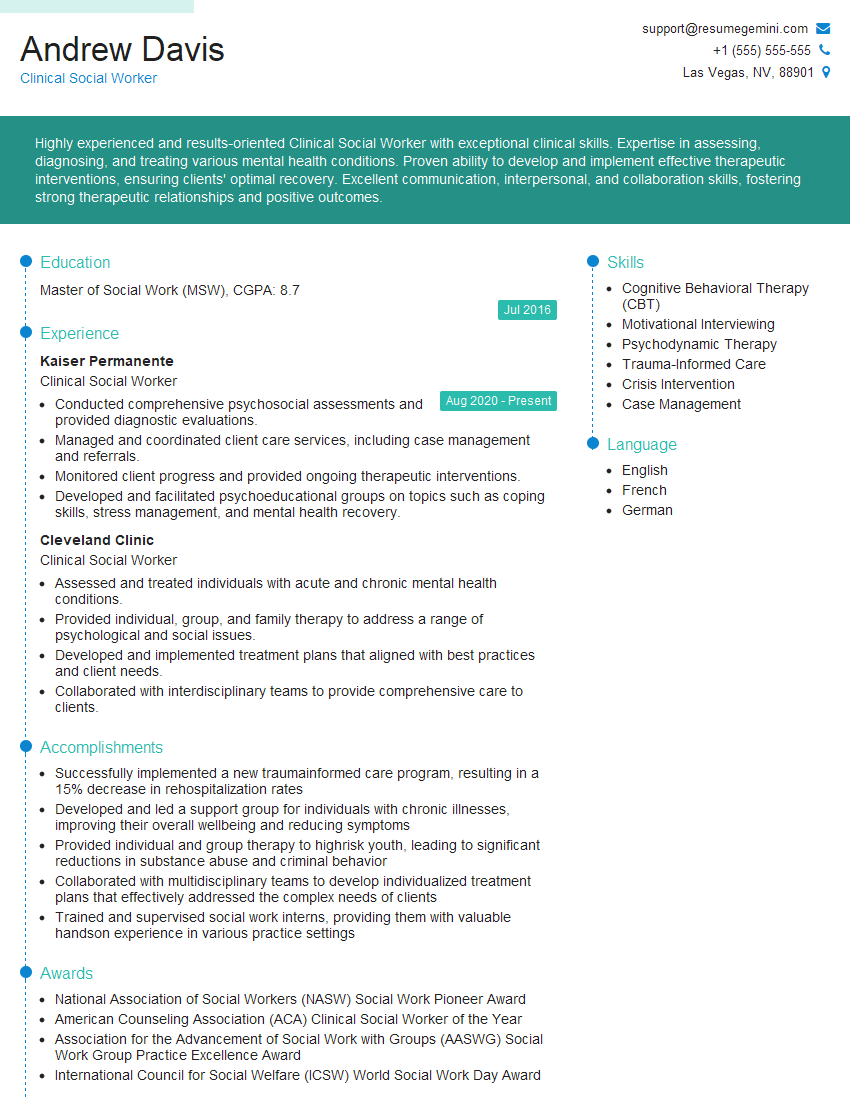
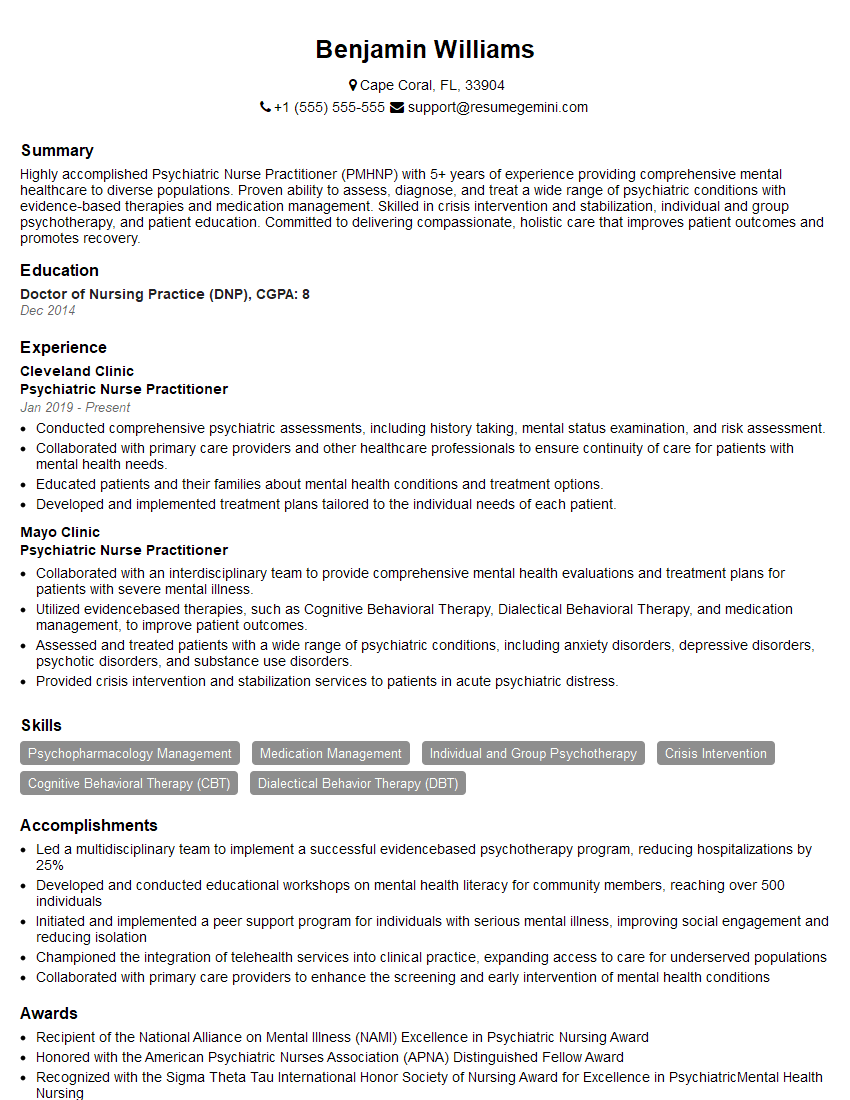
Mastering collaborative care principles is crucial for advancing your career in healthcare. It demonstrates your commitment to patient-centered care and your ability to thrive in a team-based environment, opening doors to diverse and rewarding opportunities. To significantly increase your chances of securing your dream role, a well-crafted, ATS-friendly resume is essential. ResumeGemini is a trusted resource to help you build a professional and impactful resume that highlights your skills and experience effectively. We offer examples of resumes tailored specifically to Collaborative Care with Medical Professionals to guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.