The right preparation can turn an interview into an opportunity to showcase your expertise. This guide to Contrast sensitivity assessment interview questions is your ultimate resource, providing key insights and tips to help you ace your responses and stand out as a top candidate.
Questions Asked in Contrast sensitivity assessment Interview
Q 1. Explain the concept of contrast sensitivity.
Contrast sensitivity refers to the ability of the visual system to distinguish between objects of varying luminance (brightness) differences. It’s not simply about seeing whether something is there or not (like visual acuity), but about how well we can perceive subtle differences in brightness, which allows us to discern details and textures, even in low light or when objects are partially obscured. Imagine trying to read text on a dimly lit screen – good contrast sensitivity makes this much easier. Poor contrast sensitivity means those subtle brightness differences are harder to discern, making the text blurry and harder to read.
Q 2. Describe the different methods used to assess contrast sensitivity.
Several methods exist for assessing contrast sensitivity. These methods typically involve presenting the patient with stimuli (like stripes or patterns) with varying contrast levels. The patient’s task is to identify the stimuli or determine their orientation. Common methods include:
- Pelli-Robson charts: These use letters or numbers printed with decreasing contrast levels. (Detailed explanation in answer 6).
- Sinusoidal gratings: These are patterns of alternating light and dark bars with varying spatial frequencies and contrast (Detailed explanation in answer 7).
- Computerized visual field analyzers: These sophisticated instruments allow for a more comprehensive assessment of contrast sensitivity across the entire visual field.
- Threshold detection methods: These techniques systematically adjust the contrast level until the patient can just barely detect the stimulus, providing a precise measure of contrast sensitivity.
The choice of method depends on factors like the patient’s age, suspected condition, and available equipment.
Q 3. What are the clinical implications of impaired contrast sensitivity?
Impaired contrast sensitivity has significant clinical implications, impacting daily life in various ways. Patients may experience:
- Difficulty driving at night: Reduced contrast sensitivity makes it harder to distinguish objects, especially in low light conditions.
- Problems reading: Distinguishing letters, especially small ones or those with low contrast, becomes challenging.
- Challenges in navigating crowded environments: Identifying individuals or objects amongst clutter becomes difficult.
- Increased risk of falls: Difficulties in detecting changes in ground level or obstacles can increase fall risk.
- Impaired occupational performance: Many jobs require discerning subtle differences in brightness or texture.
Furthermore, impaired contrast sensitivity can be an early indicator of various eye diseases like cataracts, glaucoma, macular degeneration, and diabetic retinopathy. Early detection and treatment are crucial to preserve visual function.
Q 4. How does contrast sensitivity relate to visual acuity?
While related, visual acuity and contrast sensitivity are distinct aspects of vision. Visual acuity measures the ability to resolve fine detail at high contrast levels (e.g., reading the smallest line on an eye chart). Contrast sensitivity, on the other hand, measures the ability to detect differences in luminance at various levels of contrast. You can have excellent visual acuity but poor contrast sensitivity, or vice versa. For instance, someone might be able to read the smallest letters on an eye chart (high acuity) but struggle to read the same letters if printed with low contrast (poor contrast sensitivity). Think of it like this: visual acuity is about seeing the sharpness of details, while contrast sensitivity is about seeing the details, regardless of their sharpness, even under low lighting conditions.
Q 5. What factors can affect contrast sensitivity?
Many factors can influence contrast sensitivity. These include:
- Age: Contrast sensitivity typically declines with age, particularly after age 50.
- Eye diseases: Conditions like cataracts, glaucoma, macular degeneration, and diabetic retinopathy significantly impact contrast sensitivity.
- Medications: Some medications can affect visual function, impacting contrast sensitivity.
- Neurological conditions: Conditions affecting the visual pathways in the brain can also impair contrast sensitivity.
- Lighting conditions: Low light levels naturally reduce contrast and impact perception.
- Glare: Excessive brightness or glare can reduce contrast sensitivity.
Understanding these factors is crucial for accurate diagnosis and management of impaired contrast sensitivity.
Q 6. Describe the Pelli-Robson chart and its use in assessing contrast sensitivity.
The Pelli-Robson chart is a simple and widely used tool for assessing contrast sensitivity. It consists of a series of rows of three-letter triplets printed in decreasing contrast against a background. Each triplet is printed with progressively lower contrast, starting from high contrast (easily readable) to very low contrast. The patient reads the triplets, and their score reflects the lowest contrast level at which they can correctly identify a specific number of triplets. The test is quick, easy to administer, and provides a reliable measure of contrast sensitivity, particularly useful in a clinical setting for screening purposes. For example, a low score indicates impaired contrast sensitivity.
Q 7. Explain the use of sinusoidal gratings in contrast sensitivity testing.
Sinusoidal gratings are a more sophisticated method used to evaluate contrast sensitivity. These are visual patterns consisting of alternating light and dark bars, with a gradual change in luminance between the bars, creating a smooth sine wave pattern. Key parameters of sinusoidal gratings include:
- Spatial frequency: This refers to the number of cycles (light-dark transitions) per degree of visual angle. Higher spatial frequencies represent finer details.
- Contrast: This represents the difference in luminance between the light and dark bars, expressed as a percentage.
In testing, the contrast of the grating is gradually reduced until the patient can no longer perceive the pattern. This threshold contrast level is then plotted against spatial frequency, creating a contrast sensitivity function (CSF). The CSF provides a comprehensive profile of the patient’s contrast sensitivity across various spatial frequencies, offering a more detailed and nuanced assessment compared to the Pelli-Robson chart. This is particularly useful in research settings and in diagnosing specific visual impairments.
Q 8. How do you interpret the results of a contrast sensitivity test?
Interpreting contrast sensitivity test results involves understanding the patient’s ability to distinguish between different levels of brightness. The test typically presents a series of striped patterns with varying degrees of contrast and spatial frequency (the number of stripes per degree of visual angle). The results are usually displayed as a graph showing contrast sensitivity (the reciprocal of the contrast threshold) plotted against spatial frequency. A lower contrast sensitivity at various spatial frequencies indicates impaired ability to discern subtle differences in brightness. For example, a score of 1.0 at 6 cycles per degree means the patient could only detect a 1:1 contrast ratio at that spatial frequency. A normal individual would likely score much higher, perhaps 2 or 3. A comprehensive analysis considers the overall shape of the curve, looking for dips that might indicate specific types of visual impairment. Low scores across the board suggest a generalized problem, while specific frequency drops might pinpoint more localized issues.
Imagine trying to read text on a dimly lit screen. A person with good contrast sensitivity can easily differentiate the black letters from the gray background. Someone with reduced contrast sensitivity might struggle, even with significant brightness differences, making reading difficult.
Q 9. What are the common causes of reduced contrast sensitivity?
Reduced contrast sensitivity can stem from various conditions affecting different parts of the visual system. Common causes include:
- Age-related macular degeneration (AMD): Damage to the macula, the central part of the retina, directly impacts contrast sensitivity.
- Cataracts: Clouding of the eye’s lens reduces light transmission and scatters light, leading to decreased contrast perception.
- Glaucoma: Damage to the optic nerve often results in reduced contrast sensitivity, especially at higher spatial frequencies.
- Diabetic retinopathy: Vascular damage in the retina can impair contrast sensitivity.
- Neurological disorders: Conditions affecting the visual pathways in the brain, such as multiple sclerosis, can impair contrast sensitivity.
- Medication side effects: Certain medications can negatively impact visual acuity and contrast sensitivity.
- Uncorrected refractive errors: Nearsightedness, farsightedness, and astigmatism, if left uncorrected, can diminish contrast sensitivity.
It is important to note that these conditions can co-occur, leading to a compounding effect on contrast sensitivity. A thorough eye examination is necessary to identify the underlying cause.
Q 10. How can contrast sensitivity be improved?
Improving contrast sensitivity depends heavily on addressing the underlying cause. Treatment strategies vary depending on the diagnosis:
- Cataract surgery: Replacing a cloudy lens can significantly improve contrast sensitivity.
- Glaucoma management: Early detection and treatment with medications or surgery can help slow disease progression and preserve contrast sensitivity.
- AMD treatment: Treatments like anti-VEGF injections or nutritional supplements might help slow disease progression. Low vision aids like magnifiers and large print materials can improve functional vision.
- Diabetic retinopathy management: Controlling blood sugar levels and managing other risk factors can help prevent further damage and preserve vision.
- Refractive correction: Wearing appropriate glasses or contact lenses can improve visual acuity and contrast sensitivity.
- Low vision rehabilitation: This includes strategies like optimizing lighting, using assistive devices, and adaptive techniques to improve functional vision.
In some cases, even with treatment, some level of contrast sensitivity impairment might remain. In these situations, compensatory strategies and assistive devices play a crucial role in improving daily functioning.
Q 11. Discuss the role of contrast sensitivity in driving safety.
Contrast sensitivity plays a vital role in driving safety. The ability to discern subtle differences in brightness is crucial for detecting pedestrians, other vehicles, and road signs, especially in challenging lighting conditions (e.g., dusk, dawn, or rain). Reduced contrast sensitivity increases the risk of accidents because drivers may not be able to perceive hazards adequately in time to react safely. For instance, a driver might struggle to distinguish a dark-colored pedestrian against a dark background, leading to a collision. Even identifying road markings might be difficult, particularly when contrast is low due to weather or poor lighting. This highlights the importance of regular eye exams, especially for drivers, to assess contrast sensitivity and address any underlying issues.
Q 12. How does contrast sensitivity relate to age-related macular degeneration?
Age-related macular degeneration (AMD) is a major cause of reduced contrast sensitivity. The macula, responsible for central vision and fine detail, is the primary area affected by AMD. As the macula deteriorates, the ability to distinguish between subtle differences in brightness diminishes. This is because the photoreceptor cells responsible for visual acuity and contrast sensitivity are damaged. The severity of contrast sensitivity loss correlates with the severity of AMD. Early-stage AMD might result in mild contrast sensitivity loss, while advanced AMD can lead to significant impairment, affecting daily activities like reading and driving.
Q 13. How does contrast sensitivity relate to glaucoma?
Glaucoma, a condition causing damage to the optic nerve, often leads to a characteristic reduction in contrast sensitivity, especially at higher spatial frequencies. This is because the optic nerve fibers responsible for transmitting visual information are affected. The loss of contrast sensitivity in glaucoma can be subtle in early stages and might not be noticeable until it progresses. As the disease progresses, patients often report difficulty distinguishing details, particularly in low-light conditions. The pattern of contrast sensitivity loss can be helpful in diagnosing and monitoring glaucoma. Regular monitoring of contrast sensitivity, alongside visual field tests, is crucial in managing glaucoma and preventing further vision loss.
Q 14. Explain the difference between spatial frequency and contrast.
Spatial frequency and contrast are two fundamental aspects of visual perception that influence contrast sensitivity. Spatial frequency refers to the number of cycles of a light-dark pattern (like stripes) per degree of visual angle. A higher spatial frequency means more stripes per degree, implying finer detail. Contrast refers to the difference in luminance (brightness) between the light and dark portions of a pattern. High contrast means a large difference in brightness, while low contrast indicates a small difference. Imagine looking at a zebra. The stripes represent spatial frequency; the difference in brightness between the black and white stripes represents contrast. Contrast sensitivity tests use various spatial frequencies and contrasts to assess the ability to detect different patterns, and this information helps determine where along the spatial frequency range any issues lie.
Q 15. What is the significance of the spatial frequency domain in contrast sensitivity testing?
Contrast sensitivity testing doesn’t just measure how well someone can see differences in brightness; it also examines how well they see these differences at various levels of detail. This is where the spatial frequency domain comes in. Spatial frequency refers to the number of cycles of a grating (alternating light and dark bars) per degree of visual angle. Low spatial frequencies represent coarse patterns, like large letters on a sign, while high spatial frequencies represent fine details, like the small print in a book. A contrast sensitivity function (CSF) is a graph that plots contrast sensitivity (the reciprocal of the minimum contrast needed to detect a pattern) against spatial frequency. The shape of this function provides crucial information about the visual system’s ability to process different levels of detail. A peak in the CSF usually occurs at around 4 cycles per degree, representing optimal sensitivity to patterns of that size. Different pathologies affect different parts of the spatial frequency spectrum leading to a characteristic alteration in the CSF. For example, cataracts might predominantly affect high spatial frequencies resulting in difficulty reading small text, while some neurological conditions can affect lower frequencies too, causing issues with navigation.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe the relationship between contrast sensitivity and visual performance in daily activities.
Contrast sensitivity is deeply intertwined with our daily visual experiences. It impacts nearly every aspect of our visual performance. Imagine trying to drive at night – your ability to distinguish a pedestrian from the background depends on your contrast sensitivity. Similarly, reading requires discerning the letters from the page background; poor contrast sensitivity makes this challenging, leading to eye strain and fatigue. Other activities like recognizing faces, navigating crowded environments, or even appreciating the subtle textures in a painting all rely heavily on good contrast sensitivity. Reduced contrast sensitivity means struggling to see in low light conditions (reduced scotopic sensitivity), difficulties identifying objects in cluttered scenes, or mistaking one object for another due to poor differentiation. A practical example: Someone with reduced contrast sensitivity might struggle to see the curb during twilight, increasing their risk of a fall.
Q 17. How do you counsel a patient with reduced contrast sensitivity?
Counseling a patient with reduced contrast sensitivity involves a multi-faceted approach. First, I’d explain the condition in clear, simple terms, emphasizing its impact on daily activities. Then, I’d discuss the potential underlying causes, whether optical (cataracts, refractive errors) or neurological (multiple sclerosis, glaucoma). This is crucial for appropriate management. Recommendations include:
- Optical correction: If refractive error is the culprit, prescribing appropriate glasses or contact lenses can significantly improve contrast sensitivity.
- Medical management: If an underlying condition like cataracts or glaucoma is detected, referring the patient to an ophthalmologist for treatment is necessary.
- Environmental modifications: Suggesting strategies like increasing lighting levels, using high-contrast materials (e.g., black text on white paper), and avoiding glare can enhance visibility.
- Low vision aids: Depending on the severity, I might recommend assistive devices like magnifiers, large print materials, or specialized computer software to support daily tasks.
- Vision therapy: In some cases, vision therapy exercises can be beneficial in improving contrast sensitivity.
- Emotional support: Addressing the patient’s emotional response to reduced vision is crucial. I would provide reassurance and emotional support, help them find appropriate resources, and connect them with support groups if needed.
Q 18. What are the limitations of current contrast sensitivity testing methods?
Current contrast sensitivity testing methods, while valuable, have some limitations. One major limitation is the standardization of testing procedures. Different tests use different stimuli (gratings, sine waves, etc.), and this variability makes comparing results across studies difficult. Another limitation is that many tests assess contrast sensitivity only at a limited range of spatial frequencies, not capturing the entire CSF. Some tests might not adequately account for individual differences in pupil size, attention, and cognitive factors that can affect performance. Additionally, current tests might not be sufficiently sensitive to detect mild contrast sensitivity losses in early stages of certain diseases. For example, certain neurological issues affect contrast sensitivity subtly and may not be fully captured by standard tests. Finally, the testing environment needs to be carefully controlled to minimise effects of ambient light and eliminate other confounding factors.
Q 19. Discuss the role of technology in advancing contrast sensitivity assessment.
Technology plays a pivotal role in advancing contrast sensitivity assessment. Digital imaging systems allow for more precise control over stimulus parameters, including spatial frequency, contrast, and luminance. Automated analysis of the test results reduces variability and enhances the accuracy and speed of testing. Adaptive testing techniques can optimize the test duration by focusing on the range of spatial frequencies most relevant to the individual’s performance. Virtual reality (VR) and augmented reality (AR) technologies offer exciting opportunities for creating immersive and engaging contrast sensitivity tests. These can be especially beneficial for assessing functional vision in real-world scenarios. For example, a VR test could simulate driving at night to assess contrast sensitivity in a more ecologically valid context.Furthermore, advancements in image processing techniques can extract more information from the standard testing images offering more in-depth information.
Q 20. Explain the importance of considering patient factors when assessing contrast sensitivity.
Patient factors significantly influence contrast sensitivity assessment. Age is a critical factor, as contrast sensitivity typically declines with age due to changes in the eye’s structure and function. Medical history, including any eye diseases, neurological disorders, or medications, is essential. Cognitive factors like attention and motivation can also affect test performance. It’s crucial to consider the patient’s occupation and daily activities to understand the functional impact of reduced contrast sensitivity. For example, a patient who is a pilot will have different needs and different consequences of poor contrast sensitivity compared to someone who works in an office. The patient’s overall health status, including any physical limitations or cognitive impairments, must also be considered to ensure the test is administered appropriately and the results are interpreted accurately. Finally, understanding a patient’s expectations and concerns can help tailor the explanations and support provided.
Q 21. How do you differentiate between reduced contrast sensitivity due to optical versus neurological issues?
Differentiating between reduced contrast sensitivity due to optical versus neurological issues requires a comprehensive approach. Optical problems, such as cataracts, refractive errors (myopia, hyperopia, astigmatism), or corneal opacities, primarily affect the clarity and transmission of light to the retina. These often lead to a relatively uniform reduction in contrast sensitivity across spatial frequencies. Neurological issues, however, can affect contrast sensitivity in more complex ways. For instance, multiple sclerosis can cause uneven or patchy reductions in contrast sensitivity, often affecting higher spatial frequencies more than lower frequencies. Glaucoma may lead to a more dramatic loss of high-frequency sensitivity. To differentiate, we use a combination of techniques including a thorough ophthalmic examination to assess for any optical abnormalities, visual field testing to check for any visual field defects suggesting neurological damage and detailed assessment of the contrast sensitivity function (CSF) looking for characteristic patterns of impairment. Detailed medical history and neurological examination will help in differentiating between these two categories. In some cases, neuroimaging techniques like MRI may be necessary to confirm neurological involvement. A complete, multi-modal approach enhances the accuracy of diagnosis and appropriate management.
Q 22. What are some common errors in performing contrast sensitivity tests and how can they be avoided?
Common errors in contrast sensitivity testing often stem from improper test administration or environmental factors. These errors can significantly affect the accuracy of the results and lead to misdiagnosis or inappropriate treatment.
Inconsistent testing environment: Variations in room lighting, glare, or background luminance can significantly alter the test outcome. Imagine trying to judge the difference between two shades of gray in a brightly lit room versus a dimly lit one – it’s much harder in the latter. This is why standardized lighting is crucial.
Improper patient instructions: Patients need clear instructions on how to respond and what is expected of them. Ambiguity can lead to inaccurate responses and skewed results. For example, if a patient doesn’t understand the instructions to respond only when they clearly see the grating, false positives or negatives can occur.
Lack of proper calibration and maintenance of equipment: Contrast sensitivity charts and devices need regular calibration to ensure accurate measurements. A malfunctioning device can produce completely unreliable data, similar to using a broken scale to weigh ingredients in a recipe.
Inadequate patient cooperation: Patients with poor attention spans, cognitive impairments, or discomfort may not be able to provide reliable responses. It is essential to establish patient rapport and ensure they are comfortable during the test.
Avoiding these errors requires:
Strict adherence to standardized testing protocols.
Thorough patient instruction and demonstration.
Regular calibration and maintenance of equipment.
Careful selection of test conditions to minimize extraneous variables.
Establishing appropriate patient rapport and addressing any concerns.
Q 23. Describe different types of contrast sensitivity tests and their advantages/disadvantages.
Several types of contrast sensitivity tests are available, each with its own advantages and disadvantages:
Pelli-Robson charts: These charts use sine-wave gratings of varying spatial frequencies and contrasts. They are relatively easy to administer and widely used. However, they are limited in their ability to assess high spatial frequencies.
Vistech Contrast Sensitivity charts: These charts also utilize sine-wave gratings but offer a broader range of spatial frequencies and contrasts, providing a more comprehensive assessment. They are more sensitive to detecting subtle deficits than Pelli-Robson charts, but are more complex and time-consuming to administer.
Computerized contrast sensitivity tests: These tests utilize computer-generated stimuli and can offer more precise control over parameters such as spatial frequency, contrast, and orientation. They’re highly flexible but require specialized equipment. They can also assess contrast sensitivity dynamically, mimicking real-world situations.
Simultaneous Threshold Method: This involves presenting various gratings to the patient at once, which is more efficient than presenting them individually. This method also addresses attention-related issues encountered when testing with individual presentations. But it requires careful patient instruction and might require advanced instrumentation.
The choice of test depends on the specific clinical needs and the available resources. For example, Pelli-Robson charts might suffice for a quick screening test, while Vistech charts or computerized tests are more suitable for detailed assessments.
Q 24. How do you determine the reliability of contrast sensitivity measurements?
Reliability of contrast sensitivity measurements is determined through several methods:
Test-retest reliability: This involves administering the same test to the same individual on different occasions. High test-retest reliability indicates that the measurements are stable over time, similar to weighing yourself on a scale multiple times in a short period – the results should be consistent.
Inter-rater reliability: This assesses the consistency of measurements obtained by different examiners using the same test. If multiple examiners administer the same test and obtain similar results, inter-rater reliability is high, reflecting consistent methodology.
Intra-rater reliability: This measures the consistency of measurements taken by the same examiner on different occasions. It’s similar to test-retest but focuses on the examiner’s consistency – are they administering the test and interpreting results consistently?
Statistical analysis: Statistical measures such as the coefficient of variation or intraclass correlation coefficient can quantify the reliability of the measurements. This will help establish the consistency of the data obtained.
Factors affecting reliability include patient cooperation, proper test administration, and equipment calibration. Minimizing these sources of error is critical in ensuring reliable measurements.
Q 25. Discuss the use of contrast sensitivity testing in the diagnosis of various ocular diseases.
Contrast sensitivity testing plays a crucial role in diagnosing various ocular diseases because many conditions affect the ability to distinguish between different shades of gray or luminance. Low contrast sensitivity is frequently seen in conditions affecting:
Cataracts: Cataracts cause light scattering, reducing contrast sensitivity.
Glaucoma: Damage to the optic nerve can lead to a loss of contrast sensitivity, particularly at higher spatial frequencies.
Macular degeneration: This condition affects the central part of the retina, resulting in reduced contrast sensitivity, especially in the central visual field.
Diabetic retinopathy: This condition can cause damage to the blood vessels in the retina, leading to decreased contrast sensitivity and blurred vision.
Multiple sclerosis: The demyelination of nerve fibers in the optic nerve can impact contrast sensitivity.
Contrast sensitivity tests are valuable not only for diagnosis but also for monitoring disease progression and assessing the effectiveness of treatment. For example, if a patient with cataracts undergoes cataract surgery, changes in their contrast sensitivity can be tracked to evaluate the success of the procedure.
Q 26. How is contrast sensitivity testing relevant to low vision rehabilitation?
Contrast sensitivity testing is highly relevant to low vision rehabilitation because it helps identify the specific visual challenges experienced by individuals with low vision. By understanding the nature and extent of contrast sensitivity loss, clinicians can tailor rehabilitation strategies to improve functional vision.
Interventions may include:
Optical devices: Magnifiers, telescopes, or specialized lenses can improve contrast sensitivity by increasing the luminance or reducing glare.
Non-optical strategies: Techniques such as improving lighting, using high-contrast materials, increasing font size, and employing assistive technology can compensate for reduced contrast sensitivity.
Visual training exercises: Specific exercises can help improve contrast sensitivity, particularly in individuals with certain conditions such as macular degeneration.
For example, a patient with macular degeneration might benefit from using a magnifier with an increased luminance to aid in reading, or they might participate in visual training focused on enhancing contrast perception.
Q 27. Explain the impact of lighting conditions on contrast sensitivity measurements.
Lighting conditions significantly impact contrast sensitivity measurements. The relationship isn’t simply linear; it’s more complex. Too much or too little light can negatively impact results.
Low-light conditions: In low light, the pupil dilates to allow more light to enter the eye, but this can also increase scattering and decrease contrast. Imagine trying to read in a dark room. The lower contrast between ink and paper makes reading more difficult.
High-light conditions: High-intensity light can cause glare, which can also reduce contrast. Think about trying to read a sign on a sunny day; the sun’s glare washes out the contrast on the sign.
Glare: Glare is a major factor, regardless of overall light level. Glare comes from direct sources (sun) or reflections (glossy surfaces). Glare decreases contrast perception dramatically.
Therefore, standardized lighting conditions are critical for accurate and reliable measurements. The testing environment should be carefully controlled to minimize glare and maintain a consistent luminance level throughout the test. Different lighting conditions can cause significant discrepancies in test results, emphasizing the importance of maintaining a standardized environment for consistency.
Q 28. Describe the role of adaptive optics in improving contrast sensitivity testing.
Adaptive optics (AO) represent a significant advancement in ophthalmic technology, including contrast sensitivity testing. AO systems use deformable mirrors to correct for aberrations in the eye’s optical system. These aberrations, which distort the image on the retina, can significantly affect contrast sensitivity, resulting in blurred vision and reduced perception.
By correcting for these aberrations in real time, AO systems can improve the clarity of the retinal image, enhancing contrast sensitivity and revealing details that might otherwise be obscured. This means we can get a much clearer picture of a patient’s true contrast sensitivity, free from the interference of eye aberrations.
Using AO, researchers can precisely measure the impact of ocular aberrations on contrast sensitivity. This technology is particularly useful in studying the effects of aging, diseases, and surgical interventions on the optical quality of the eye.
While AO is currently more prevalent in research settings than in routine clinical practice, its potential to improve the accuracy and sensitivity of contrast sensitivity testing is undeniable, offering the opportunity for more precise diagnoses and more targeted interventions.
Key Topics to Learn for Contrast Sensitivity Assessment Interview
- Fundamentals of Contrast Sensitivity: Understand the definition, importance, and measurement techniques of contrast sensitivity. Explore the underlying physiological mechanisms involved in visual perception and how they relate to contrast sensitivity.
- Clinical Applications: Discuss the role of contrast sensitivity testing in diagnosing and managing various ophthalmic conditions. Consider applications in areas like low vision rehabilitation and driver’s license assessments.
- Different Testing Methods: Become familiar with various contrast sensitivity tests (e.g., Pelli-Robson chart, sine-wave gratings) and their strengths and limitations. Understand how to interpret the results of these tests.
- Factors Affecting Contrast Sensitivity: Explore the influence of age, optical quality (e.g., cataracts, refractive errors), and neurological conditions on contrast sensitivity. Be prepared to discuss how these factors impact test interpretation.
- Interpreting Test Results and Reporting: Practice analyzing and interpreting contrast sensitivity data, understanding normal versus abnormal findings and how to communicate these effectively in a professional report.
- Troubleshooting and Problem-Solving: Develop your ability to identify potential sources of error during testing and suggest solutions. This includes understanding patient factors and equipment limitations.
- Technological Advancements: Stay updated on the latest technologies and methodologies used in contrast sensitivity assessment, demonstrating your commitment to professional development.
Next Steps
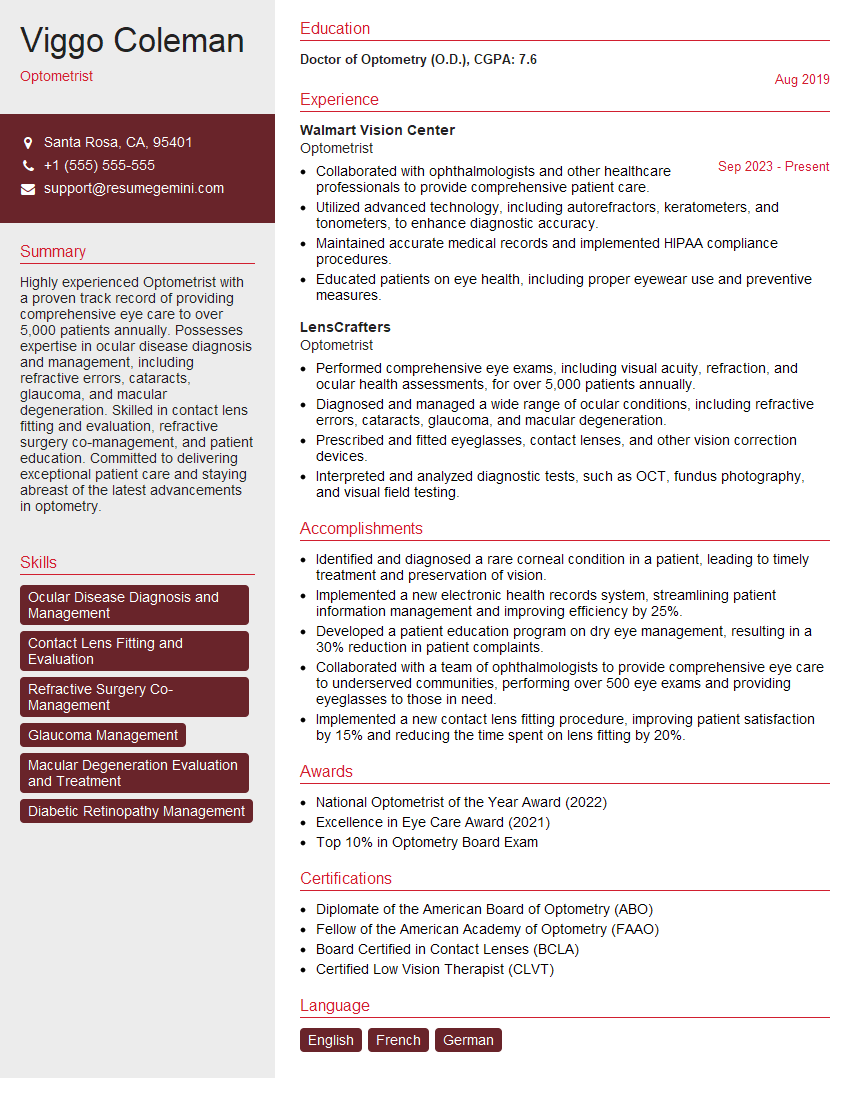
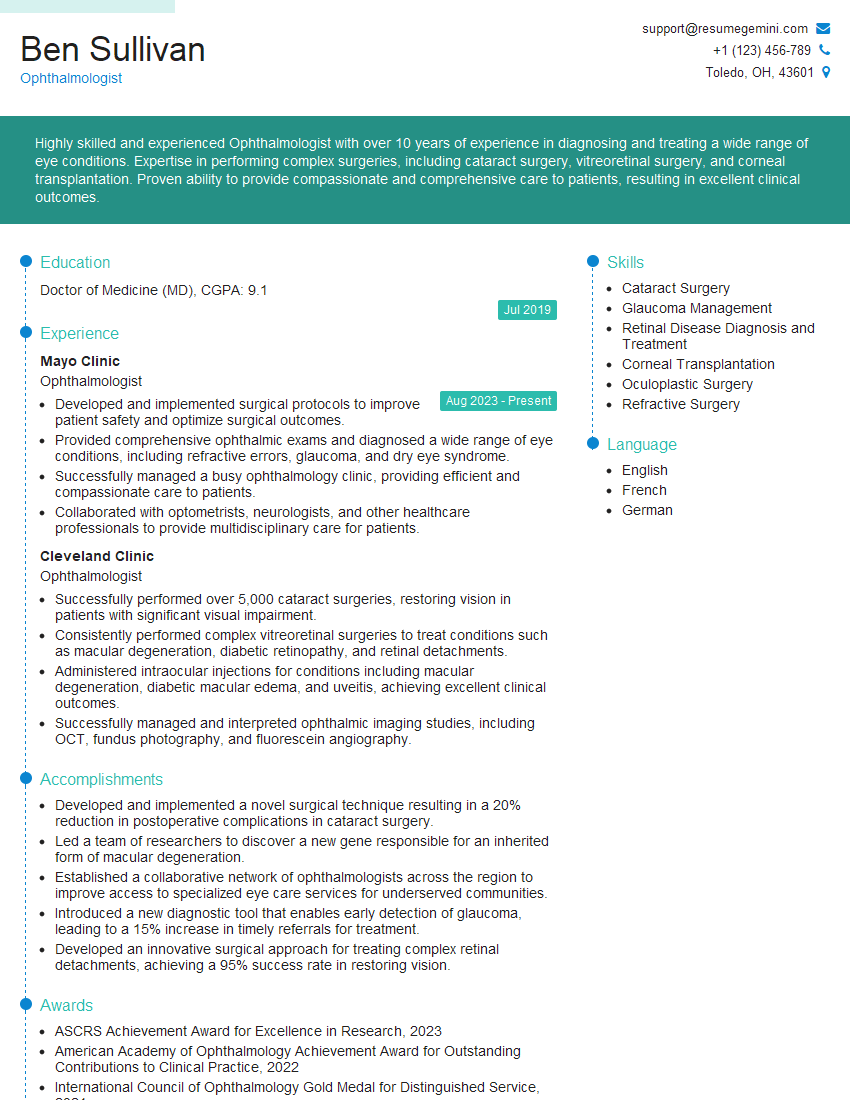
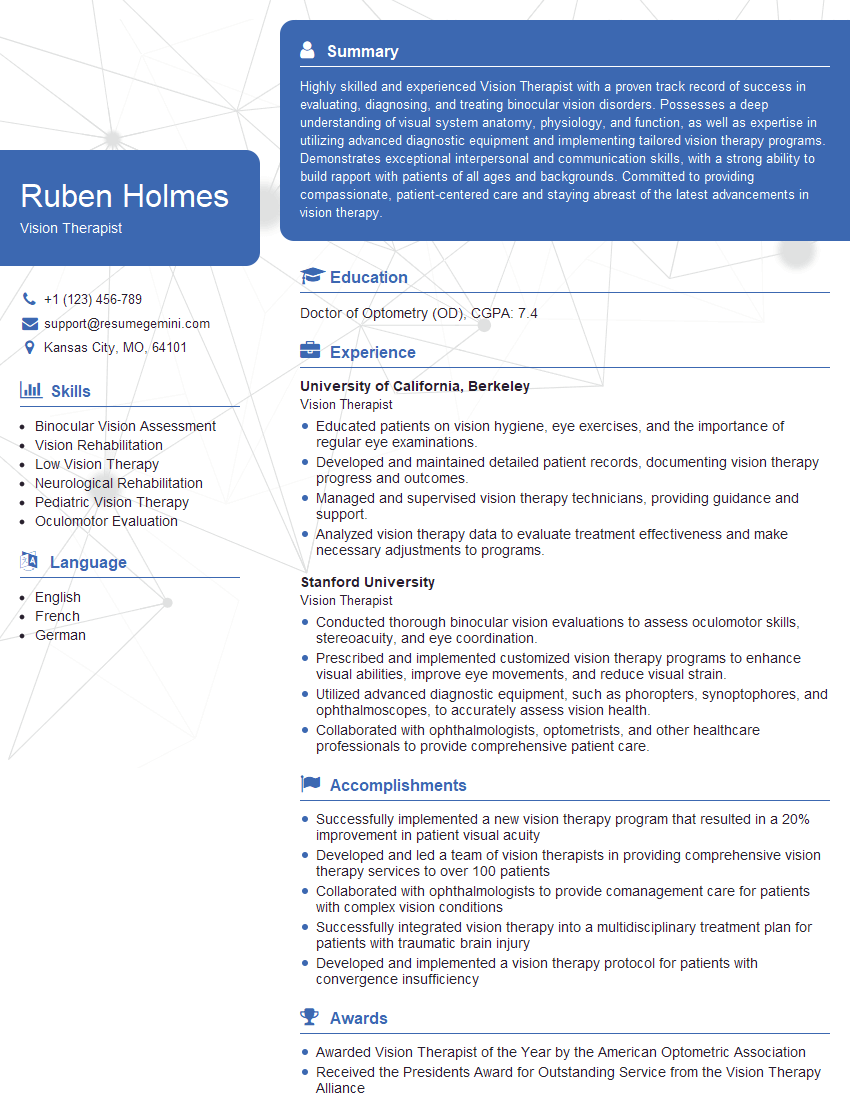
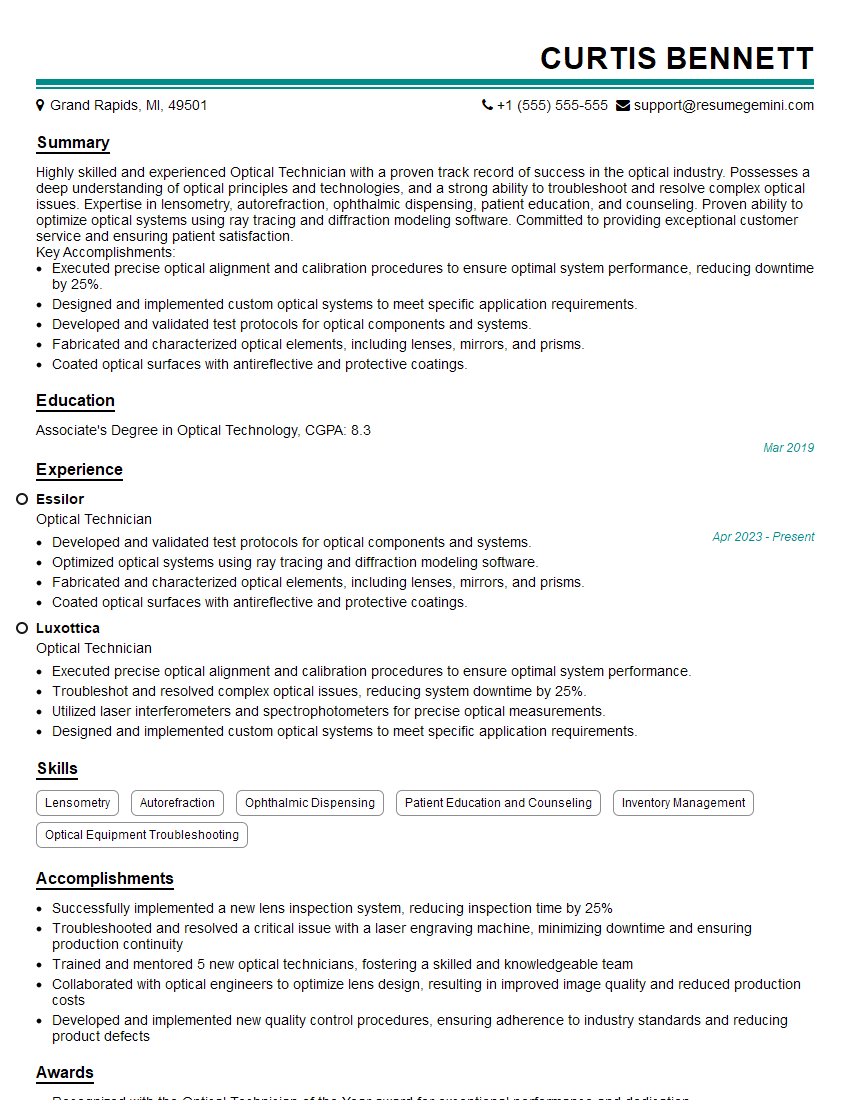
Mastering contrast sensitivity assessment opens doors to exciting career opportunities in ophthalmology, optometry, and related fields. A strong understanding of this crucial diagnostic tool is highly valued by employers. To maximize your job prospects, create an ATS-friendly resume that effectively highlights your skills and experience. ResumeGemini is a trusted resource to help you build a professional and impactful resume. We provide examples of resumes tailored to contrast sensitivity assessment roles to guide you through the process. Invest time in crafting a compelling resume—it’s your first impression on potential employers.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.