The right preparation can turn an interview into an opportunity to showcase your expertise. This guide to Corns and Calluses Removal interview questions is your ultimate resource, providing key insights and tips to help you ace your responses and stand out as a top candidate.
Questions Asked in Corns and Calluses Removal Interview
Q 1. Explain the difference between a corn and a callus.
Both corns and calluses are thickened areas of skin caused by friction or pressure, but they differ in their location and shape. A corn is a small, cone-shaped area of thickened skin, typically found on the toes, particularly over bony prominences or between toes. The cone shape is crucial; it’s due to the pressure pushing the hardened skin inwards towards the bone or nerve. A callus, on the other hand, is a larger, flatter area of thickened skin, often found on the soles of the feet, heels, or hands. It develops as a protective response to repeated rubbing or pressure. Think of a callus as a broader, less-pointed response to friction, while a corn is a more concentrated, pointy reaction.
Imagine wearing shoes that are too tight: You might develop a corn on a toe joint, due to the concentrated pressure. However, if you frequently walk barefoot on rough surfaces, you might develop a callus on your heel, due to the widespread friction.
Q 2. Describe the various methods for removing corns and calluses.
Several methods exist for corn and callus removal, ranging from over-the-counter treatments to professional medical procedures.
- Over-the-counter medications: These include salicylic acid plasters or creams, which work by chemically dissolving the thickened skin. Always follow the instructions carefully; overuse can irritate the surrounding skin.
- Pumice stone: Soaking the affected area in warm water softens the skin, making it easier to gently rub away the thickened layer with a pumice stone. This is a more mechanical method and good for calluses.
- Professional removal: Podiatrists or dermatologists can safely remove corns and calluses using various techniques, such as surgical excision (for very stubborn cases), cryotherapy (freezing), or laser treatment. They can also identify and address underlying causes.
- Prescription medications: In some cases, stronger topical medications or oral medications might be prescribed for particularly painful or stubborn cases.
It’s crucial to choose a method appropriate to the severity of the corn or callus. For example, a small, superficial corn might respond well to salicylic acid plasters, while a deep, painful corn might require professional intervention.
Q 3. What are the contraindications for corn and callus removal?
Several contraindications exist for corn and callus removal, particularly regarding self-treatment. Individuals with diabetes, peripheral neuropathy, or poor circulation should avoid self-treating corns and calluses due to the increased risk of infection and complications. These conditions often impair healing and increase the risk of complications such as ulcers or infections. Also, individuals with bleeding disorders or those taking blood-thinning medication should exercise caution and consult a doctor before attempting any removal method. Pregnant women should consult a healthcare professional before using any topical treatments.
Furthermore, if you have a corn or callus that is painful, infected (redness, swelling, pus), or shows signs of unusual changes (like rapid growth or unusual color), seek immediate professional medical advice rather than attempting self-treatment.
Q 4. How do you assess the severity of a corn or callus?
Assessing the severity of a corn or callus involves evaluating several factors:
- Size and depth: Larger and deeper lesions are generally more severe.
- Pain level: Intense pain suggests a more serious condition, potentially involving nerve compression.
- Presence of infection: Signs of infection (redness, swelling, pus, warmth) indicate a need for immediate medical attention.
- Location: Corns on weight-bearing areas (e.g., the heel) can be more problematic.
- Duration: Long-standing lesions may be more difficult to treat.
A podiatrist or dermatologist can conduct a thorough assessment, potentially using diagnostic tools to evaluate the depth and extent of the lesion. They will take into account the patient’s medical history and lifestyle factors to determine the best treatment approach.
Q 5. What are the common complications associated with improper corn and callus removal?
Improper corn and callus removal can lead to several complications:
- Infection: Cutting or scraping the skin can introduce bacteria, leading to infection. This is especially dangerous for individuals with compromised immune systems or circulatory problems.
- Bleeding: Aggressive removal methods can cause bleeding, potentially leading to scarring.
- Deepening of the lesion: Incorrect removal might push the hardened skin deeper into the underlying tissues, making it even more painful and difficult to treat.
- Scarring: Damage to the surrounding skin can result in permanent scarring.
- Nerve damage: Improper removal, especially of a corn, can damage underlying nerves, causing persistent pain or numbness.
It’s essential to prioritize proper techniques and seek professional help when necessary to minimize these risks. Self-treatment should always be approached cautiously and with a clear understanding of the potential consequences.
Q 6. Describe the different types of corns (e.g., hard, soft, seed corns).
Corns are classified into different types based on their location and appearance:
- Hard corns: These are the most common type, appearing as small, hard, and yellowish thickenings of skin. They typically form on the tops or sides of toes, caused by pressure from shoes.
- Soft corns: These are softer, whiter, and usually occur between the toes, often in moist areas. The macerated environment between the toes contributes to their formation.
- Seed corns: These are small, painful corns that often develop on the soles of the feet. They are deeper and more difficult to treat than hard corns.
The type of corn influences the appropriate treatment strategy. For example, a soft corn benefits from keeping the area dry to prevent moisture buildup, whereas a hard corn might respond better to salicylic acid treatments.
Q 7. How do you differentiate between a corn and a wart?
Differentiating between a corn and a wart is crucial, as the treatments differ significantly. Warts are caused by a viral infection (Human Papillomavirus or HPV), while corns and calluses are due to friction or pressure. Key differences include:
- Appearance: Corns and calluses are typically smooth or slightly rough, whereas warts can be rough, bumpy, or cauliflower-like.
- Location: While corns are concentrated on weight-bearing points, warts can appear anywhere on the body.
- Pain: Corns are often painful due to pressure on underlying nerves; warts can be painless or mildly itchy.
- Presence of black dots: Small, black dots (thrombosed capillaries) may be present in warts but are not found in corns.
If you are unsure whether a lesion is a corn or a wart, seek professional medical advice for proper diagnosis and treatment. Incorrect treatment can lead to ineffective treatment or even worsen the condition.
Q 8. What patient education do you provide regarding corn and callus prevention?
Preventing corns and calluses starts with proper foot care. I educate patients on the importance of wearing properly fitting shoes that provide adequate space for the toes and avoid excessive pressure points. We discuss the significance of regularly inspecting their feet for any early signs of thickening or discomfort.
- Proper Footwear: I advise patients to choose shoes made from breathable materials and to avoid high heels or shoes with pointed toes. Think of your shoes like a glove – they should fit comfortably without constricting.
- Regular Foot Care: Daily washing and thorough drying, particularly between the toes, helps prevent moisture buildup that can soften the skin and lead to corn/callus formation. I show them how to gently exfoliate using a pumice stone or foot file on calloused areas, but emphasize avoiding aggressive scrubbing, which can irritate the skin.
- Moisture Balance: I explain the importance of maintaining healthy skin moisture. This means using a moisturizer daily, especially on areas prone to dryness. Overly dry skin is more susceptible to callus formation.
- Padding and Cushioning: For individuals with known pressure points, I recommend using protective padding or cushions inside their shoes to reduce friction and pressure on specific areas.
These preventative measures, coupled with regular professional foot care appointments as needed, are crucial in minimizing the risk of corn and callus development.
Q 9. How do you manage a patient with diabetic foot and corn/callus issues?
Managing a diabetic patient with corns or calluses requires a very cautious approach because of the increased risk of infection and complications. Their reduced sensation (neuropathy) often means they might not feel pain, leading to unnoticed injury and delayed treatment.
- Non-invasive Assessment: I carefully assess the condition of the corn/callus, paying close attention to signs of infection (redness, swelling, warmth, pus, or unusual odor). I avoid any invasive procedures myself and immediately refer patients to a podiatrist, especially if I detect signs of infection or nerve damage.
- Referral and Collaboration: I work closely with the patient’s primary care physician and/or a podiatrist who specializes in diabetic foot care. They are best equipped to manage the diabetic aspects and determine the safest and most effective removal techniques.
- Patient Education: Emphasis is placed on the patient’s regular self-care and foot inspection, including the proper use of prescribed creams or medications, and the importance of immediately reporting any new symptoms or changes in their foot condition.
- Offloading Pressure: This is critical in preventing further damage. The podiatrist may recommend custom-made orthotics or special shoes to redistribute pressure and alleviate the load on the affected areas.
The collaborative approach ensures that the diabetic patient’s overall health and foot care are carefully managed, minimizing the risk of complications.
Q 10. What are the signs and symptoms of infection following corn/callus removal?
Infection following corn or callus removal, even seemingly minor procedures, is a serious concern. Early recognition is key.
- Increased Pain and Tenderness: A significant increase in pain around the affected area beyond the initial discomfort of the procedure. This is more than just a slight ache.
- Redness and Swelling: Noticeable redness spreading beyond the immediate area of treatment and accompanied by swelling or inflammation.
- Warmth to the Touch: The skin around the affected area feels abnormally warm compared to the surrounding skin.
- Pus or Drainage: The presence of pus or any yellowish or greenish discharge from the affected site is a clear sign of infection.
- Fever or Chills: Systemic symptoms like fever or chills suggest a more widespread infection requiring immediate medical attention.
- Unusual Odor: A foul or unpleasant odor emanating from the affected area indicates bacterial growth.
If any of these signs are present, it’s crucial for the patient to seek immediate medical attention to prevent a serious infection.
Q 11. What are the steps you take if a patient experiences bleeding during corn removal?
Bleeding during corn removal is uncommon if proper techniques are used, but it can happen. My immediate actions would be:
- Apply Pressure: I immediately apply direct pressure to the bleeding area using a clean gauze pad or sterile cloth. The pressure should be firm and consistent for at least 5-10 minutes.
- Elevate the Foot: Raising the foot above the heart level can help slow the bleeding by reducing blood flow to the area.
- Assess the Bleeding: I carefully monitor the bleeding. If it’s significant or doesn’t stop after 10 minutes of direct pressure, I’ll refer the patient for further medical evaluation and potential stitches.
- Clean the Wound: Once the bleeding stops, I thoroughly clean the wound with an antiseptic solution to minimize the risk of infection.
- Dressing: I then apply a clean, sterile dressing to protect the area and prevent further contamination.
- Patient Instruction: I will provide the patient with clear instructions on how to monitor the wound and any signs of infection. I’ll schedule a follow-up appointment to check the healing progress.
This structured approach helps to control the bleeding effectively and prevent complications. Prevention through meticulous technique is, of course, the best strategy.
Q 12. Describe your approach to managing a patient with sensitive skin and corns/calluses.
Patients with sensitive skin require a gentler approach to corn and callus removal. Aggressive methods can easily lead to irritation, inflammation, or even skin damage.
- Avoid Harsh Methods: I would avoid using sharp instruments like blades or razors. These can easily cut or damage sensitive skin.
- Gentle Exfoliation: I recommend using a pumice stone or a fine-grade foot file to gently exfoliate the thickened skin, always with light pressure and short sessions to avoid irritation.
- Moisturizing: Regular moisturizing is essential to maintain skin hydration and prevent dryness which aggravates sensitive skin. I would recommend using a fragrance-free, hypoallergenic moisturizer.
- Salicylic Acid (with caution): Low-concentration salicylic acid preparations can be helpful, but it must be used cautiously and under careful supervision to avoid irritation. I may recommend a lower concentration or less frequent application than for patients with less sensitive skin.
- Professional Treatment: In some cases, referring the patient to a podiatrist or dermatologist for professional treatment might be the best option to prevent adverse reactions.
The key is to prioritize gentle and gradual removal methods, always monitoring for any signs of irritation or adverse reactions.
Q 13. Explain how you select the appropriate corn/callus removal technique for each patient.
Selecting the appropriate corn/callus removal technique is based on several factors:
- Severity of the Corn/Callus: For a small, superficial corn, a simple over-the-counter treatment like a pumice stone or salicylic acid patch might suffice. More significant calluses might require professional intervention.
- Patient’s Skin Condition: As discussed, patients with sensitive skin necessitate gentler approaches. Those with diabetic neuropathy require specialized care and referral.
- Patient’s Medical History: Conditions such as diabetes, peripheral artery disease, or compromised immune systems greatly influence the treatment strategy.
- Location of the Corn/Callus: The location affects accessibility and the choice of treatment.
- Patient Preference: While my recommendations guide treatment, patient preferences should always be considered whenever possible. The patient’s comfort and cooperation are vital for successful treatment.
Through a thorough assessment, we can tailor the treatment plan, choosing from options like topical treatments, professional paring, or referral to a podiatrist. This personalized approach ensures safety and efficacy.
Q 14. What are the benefits and limitations of using salicylic acid for corn/callus removal?
Salicylic acid is a common keratolytic agent used to soften and remove thickened skin in corns and calluses.
- Benefits: It’s readily available over-the-counter, relatively inexpensive, and effective in softening the thickened skin, making it easier to remove. It works by breaking down the bonds between the dead skin cells.
- Limitations: Salicylic acid can cause skin irritation, redness, or burning in sensitive individuals. It shouldn’t be used on open wounds or infected areas. Incorrect or prolonged use can cause skin damage. It’s vital to follow the instructions carefully and not exceed the recommended concentration or application frequency. Also, individuals with diabetes or peripheral artery disease should use it with extreme caution and under medical supervision due to increased risk of complications.
Salicylic acid can be a valuable tool when used appropriately, but its limitations require careful consideration and responsible application. I always stress the importance of patient education and monitoring to avoid potential adverse effects.
Q 15. Discuss the use of surgical methods for corn/callus removal.
Surgical methods for corn and callus removal are rarely necessary and are typically reserved for very difficult or stubborn cases that haven’t responded to conservative treatments. These procedures are usually performed by podiatrists or dermatologists.
One common surgical technique involves the use of a scalpel to excise (cut out) the corn or callus. This is usually done under local anesthesia to minimize discomfort. Another method may involve the use of a laser to ablate (remove) the thickened skin. Post-operative care involves keeping the area clean and dry and applying prescribed topical medications to aid healing.
Important Note: Self-surgical removal is strongly discouraged as it carries a high risk of infection and improper healing, leading to potentially serious complications.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are your safety protocols when removing corns and calluses?
Safety is paramount when removing corns and calluses. My protocols include:
- Thorough assessment: I always begin with a careful examination of the affected area to determine the size, depth, and location of the corn or callus, and to check for any signs of infection.
- Proper sterilization: All instruments are sterilized using an autoclave before each use to prevent the spread of infection.
- Local anesthesia (when necessary): For more invasive procedures, local anesthesia is administered to ensure the patient’s comfort and minimize pain.
- Aseptic technique: I maintain a sterile field throughout the procedure to reduce the risk of infection.
- Patient education: Patients are thoroughly instructed on post-operative care and the signs of infection (increased pain, redness, swelling, pus).
- Appropriate referrals: If I encounter a situation beyond my expertise (e.g., suspected infection, underlying medical condition), I immediately refer the patient to a specialist like a podiatrist or dermatologist.
Q 17. How do you document the corn/callus removal procedure?
Documentation is crucial for legal and medical reasons. My documentation includes:
- Patient demographics: Name, date of birth, contact information.
- Detailed description of the lesion: Size, location, type (corn, callus), presence of infection or other complications.
- Procedure performed: Specific technique used (e.g., shaving, chemical peeling).
- Anesthesia used (if any): Type and amount.
- Post-operative instructions: Detailed home care instructions provided to the patient.
- Follow-up appointments: Scheduled date(s) for monitoring healing.
- Photographs (optional but recommended): Before and after images to track progress.
All this information is recorded in the patient’s chart, following HIPAA guidelines and maintaining patient confidentiality.
Q 18. What are the signs of an underlying medical condition that might cause corns and calluses?
Persistent or unusually painful corns and calluses can sometimes indicate an underlying medical condition. These include:
- Diabetes: Diabetics have reduced sensation in their feet, making them more susceptible to unnoticed injuries that can lead to serious complications.
- Peripheral neuropathy: Nerve damage affecting the extremities can cause numbness and reduced sensation, increasing the risk of developing corns and calluses without awareness.
- Arthritis: Joint deformities from arthritis can alter weight distribution, leading to increased pressure on certain areas and thus corn/callus formation.
- Psoriasis: This skin condition can sometimes lead to thickened, scaly areas that resemble corns or calluses.
- Certain types of fungal infections: These can mimic the appearance of a corn or callus.
If I suspect an underlying condition, I always refer the patient to a physician or appropriate specialist for further evaluation and management.
Q 19. How do you handle a patient with a recurring corn or callus?
Recurring corns or calluses suggest an underlying cause that needs to be addressed. My approach involves:
- Identifying the root cause: This may involve assessing the patient’s footwear, gait (walking style), and any potential medical conditions. Poorly fitting shoes are a common culprit!
- Modifying risk factors: I counsel patients on wearing properly fitting shoes, using appropriate padding or inserts, and adjusting their activities to reduce pressure on affected areas.
- Long-term management strategies: This might include regular professional removal of the corn or callus combined with home care measures like using emollients or keratolytics (medications that soften and remove dead skin) as prescribed.
- Consideration of custom orthotics: In certain cases, custom-made orthotics can redistribute pressure and prevent recurrence.
The goal is to break the cycle of corn/callus formation by addressing the underlying cause and empowering the patient to take preventative measures.
Q 20. Describe your experience with different types of corn/callus removal tools.
I have experience with a variety of corn and callus removal tools, each with its own advantages and disadvantages:
- Scalpels: Used for surgical excision of deeply embedded or large lesions. Requires precision and sterile technique.
- Curettes: Small, spoon-shaped instruments used to scrape away thickened skin. Good for smaller lesions.
- Surgical scissors: Used to trim away thickened skin carefully.
- Pumice stones: For home use; effective in removing superficial layers of thickened skin. Should be used gently to avoid injury.
- Salicylic acid-based preparations: These are keratolytics; they chemically dissolve dead skin. They come in various forms (patches, liquids) and are often used in conjunction with other methods.
Choosing the appropriate tool depends on the size, depth, and location of the corn or callus, as well as the patient’s overall health and preferences. Safety and proper technique are always prioritized.
Q 21. How do you counsel a patient about home care after corn/callus removal?
Post-operative counseling is critical for successful healing and prevention of recurrence. I provide patients with:
- Instructions on wound care: Keeping the area clean and dry, applying any prescribed topical medications.
- Footwear advice: Wearing comfortable, properly fitting shoes to minimize pressure on the affected area. Avoiding high heels and tight-fitting shoes is important.
- Home care instructions: This might include using emollients to moisturize the skin, avoiding harsh scrubbing, and inspecting the area daily for signs of infection.
- Follow-up appointments: Scheduling follow-up appointments to monitor healing progress and address any concerns.
- Early warning signs of complications: Educating the patient about signs of infection (redness, swelling, pain, pus) and instructing them to seek immediate medical attention if they develop.
Providing clear, concise, and personalized home care instructions empowers patients to actively participate in their healing process and helps prevent complications.
Q 22. What are the legal and ethical considerations when removing corns and calluses?
Legal and ethical considerations in corn and callus removal center around patient safety, informed consent, and proper scope of practice. Legally, I must adhere to all relevant state and national regulations governing healthcare professionals, ensuring I’m properly licensed and practicing within the boundaries of my professional qualifications. Ethically, I’m bound by principles of beneficence (acting in the patient’s best interest), non-maleficence (avoiding harm), autonomy (respecting patient decisions), and justice (providing equitable care). This means obtaining explicit, informed consent before any procedure, fully explaining the process, potential risks (infection, bleeding, scarring), and alternative treatments. I must also maintain confidentiality and accurately document all procedures and patient interactions.
For example, I would never attempt to treat a corn or callus that shows signs of infection or displays characteristics suggesting a more serious underlying condition. I would always refer such cases to a podiatrist or physician for appropriate management. Similarly, I must accurately represent my skills and qualifications and avoid making claims I cannot substantiate.
Q 23. How do you deal with a patient who is experiencing pain during the procedure?
Patient comfort is paramount. If a patient experiences pain during a corn or callus removal procedure, I immediately stop and assess the situation. The cause of the pain might be the technique, the depth of removal, or an underlying sensitivity. I might adjust my technique, using a less aggressive approach, taking more frequent breaks, or applying a topical anesthetic like a lidocaine cream prior to resuming. Open communication is key – I explain what I’m doing and why, encourage the patient to express their discomfort, and reassure them that we’ll work together to manage the pain. If the pain persists or is severe, I stop the procedure and refer the patient to a podiatrist or medical doctor for further assessment and potentially more advanced pain management techniques.
For instance, I might use a smaller, sharper instrument to make smaller, more precise cuts, reducing the chance of causing unnecessary pain or trauma. I might also switch to a different technique altogether if the initial method isn’t working well.
Q 24. Describe a challenging case involving corn/callus removal and how you handled it.
I once encountered a patient with a very thick, deeply embedded callus on their heel that was resistant to conventional treatments. Multiple sessions of meticulous shaving and softening with salicylic acid yielded minimal results. The patient had a history of diabetes, which complicated the situation because even minor cuts could lead to serious complications. This meant extra caution was necessary. My approach involved a combination of strategies. First, I used a urea-based cream for a more effective softening over a longer period, in addition to the salicylic acid. Then, I used a specialized micromotor with a diamond burr, ensuring meticulous control to avoid excessive pressure or depth. I worked in small increments and frequently checked the patient’s comfort level. This very gradual approach ultimately allowed me to remove the callus effectively without causing any damage or pain. After each session, I applied an antimicrobial dressing and advised the patient on proper foot care, focusing on hydration and pressure relief.
Q 25. What are the latest advancements in corn and callus removal techniques?
Recent advancements focus on improving patient comfort and minimizing risk. These include: more effective topical medications that offer better keratolytic action (breaking down hard skin) with less irritation; improved micromotor tools with finer burrs for more precise and less traumatic removal; the use of laser treatments in specific cases, which can precisely target and ablate hyperkeratotic tissue; and development of advanced dressings that enhance healing and reduce infection risk. Research is also ongoing into non-invasive techniques that can effectively treat corns and calluses without the need for physical removal. For example, some research explores the use of ultrasound energy to break down thickened skin. While still experimental, such advancements promise a less invasive and more comfortable patient experience.
Q 26. How do you stay updated on best practices for corn and callus removal?
Staying updated is crucial in this field. I actively participate in continuing education courses and workshops offered by professional organizations like the American Podiatric Medical Association (APMA). I regularly read peer-reviewed journals focusing on podiatry and dermatology, searching for research on new techniques, treatments, and best practices. I also attend conferences and workshops where I can network with other professionals and learn about innovative approaches to corn and callus removal. Keeping abreast of changes in regulations and guidelines is also part of my ongoing professional development. This continuous learning ensures that I provide patients with the safest and most effective care available.
Q 27. What is your approach to managing patient expectations regarding corn/callus treatment?
Managing patient expectations begins with a thorough initial consultation. I explain the nature of corns and calluses, the treatment options, the likely number of sessions needed, and the potential outcomes. I also emphasize that complete removal might not be possible in all cases, especially for deep-seated or recurring problems. I provide realistic timeframes for healing and recovery, explaining that the process often involves multiple appointments. Honest and clear communication helps prevent misunderstandings and unrealistic expectations. For example, I might say something like, “While we can significantly improve your comfort and reduce the size of the callus, it’s unlikely that it will disappear completely in one session.” This upfront transparency establishes trust and builds a strong therapeutic relationship.
Q 28. How would you handle a complaint from a patient regarding corn/callus removal?
Handling patient complaints involves a calm, empathetic, and professional approach. I would first actively listen to the patient’s concerns without interruption, making sure I fully understand their perspective. Then, I would review the patient’s records and the treatment plan to identify any potential areas where things might have gone wrong or expectations weren’t met. I would apologize if appropriate, even if I don’t believe a mistake was made, because acknowledging their feelings is important. Depending on the nature of the complaint, I might offer an alternative treatment plan, a follow-up appointment, or possibly a partial or full refund. If the issue is complex or I’m unable to resolve it, I might involve a supervisor or seek guidance from professional organizations. Maintaining open communication and documenting all interactions is crucial to resolving complaints effectively and maintaining a positive professional reputation.
Key Topics to Learn for Corns and Calluses Removal Interview
- Anatomy and Physiology of Skin: Understanding the structure of skin, including the epidermis, dermis, and subcutaneous tissue, is crucial for diagnosing and treating corn and callus formations.
- Differentiation of Corns and Calluses: Learn to distinguish between hard corns, soft corns, and calluses based on their location, appearance, and underlying causes. This includes understanding the role of pressure and friction.
- Non-Surgical Treatment Methods: Master the techniques and applications of various non-surgical treatments, including salicylic acid plasters, keratolytics, pumice stones, and other topical treatments. Understand their limitations and potential side effects.
- Surgical Excision Techniques (if applicable): If the role involves surgical procedures, thoroughly understand the appropriate techniques, safety precautions, and post-operative care for corn and callus removal.
- Patient Assessment and Consultation: Learn effective communication skills to gather patient history, assess their condition, and provide appropriate recommendations for treatment. This includes identifying contraindications for certain treatments.
- Hygiene and Infection Control: Understand and practice strict hygiene protocols to prevent infections during treatment procedures and ensure patient safety.
- Post-Treatment Care and Patient Education: Learn how to advise patients on proper foot care, including the use of padding, moisturizers, and appropriate footwear to prevent recurrence.
- Ethical Considerations and Professional Conduct: Understand and uphold ethical guidelines and professional standards in the practice of corns and calluses removal.
- Troubleshooting Common Complications: Be prepared to discuss and address potential complications like infection, bleeding, or inadequate removal of the corn or callus.
Next Steps
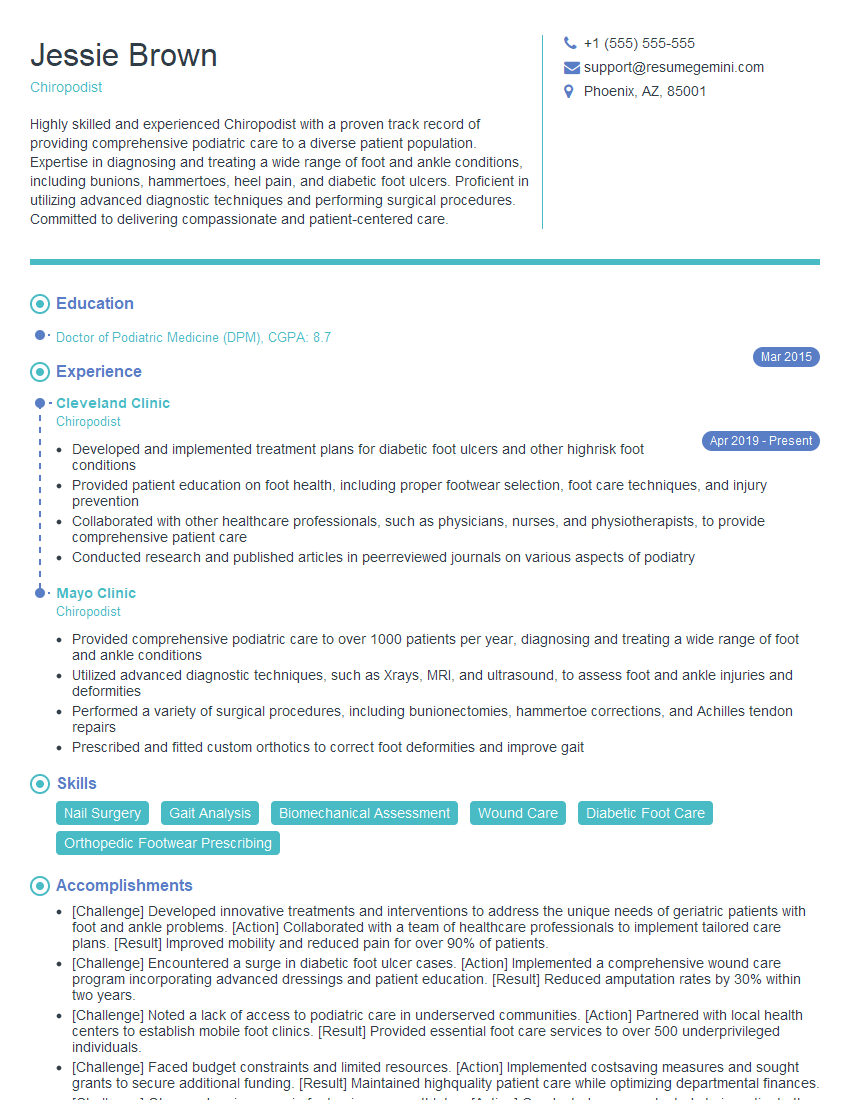
Mastering the art of corns and calluses removal opens doors to a fulfilling and rewarding career in podiatry or related fields. To maximize your job prospects, invest time in creating a compelling and ATS-friendly resume that highlights your skills and experience. ResumeGemini is a trusted resource to help you build a professional resume that stands out. Examples of resumes tailored to the Corns and Calluses Removal field are available to guide your efforts, ensuring your qualifications shine through to potential employers.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.