The right preparation can turn an interview into an opportunity to showcase your expertise. This guide to Cytology (e.g., FNA, pap smears) interview questions is your ultimate resource, providing key insights and tips to help you ace your responses and stand out as a top candidate.
Questions Asked in Cytology (e.g., FNA, pap smears) Interview
Q 1. Describe the process of performing a Fine Needle Aspiration (FNA).
Fine Needle Aspiration (FNA) is a minimally invasive procedure used to collect cells from a suspicious mass or lesion. Think of it like using a very fine straw to draw out a sample. It’s commonly used for thyroid nodules, lymph nodes, and masses in the breast.
- Sterilization and Preparation: The area is cleaned and sterilized to prevent infection.
- Needle Insertion: A very thin needle, attached to a syringe, is carefully inserted into the lesion under imaging guidance (ultrasound or sometimes CT).
- Aspiration: Gentle suction is applied to the syringe to draw cells into the needle. This might involve multiple passes depending on the lesion’s size and consistency.
- Smear Preparation: The collected cells are then smeared onto glass slides, creating multiple smears to ensure adequate cellularity and to prepare some for different staining techniques.
- Fixation and Staining: The slides are promptly fixed (typically with alcohol) to preserve the cells and subsequently stained (e.g., with Papanicolaou or Diff-Quik stains) to allow visualization under a microscope.
- Microscopic Examination: A pathologist then analyzes the stained slides to determine the nature of the cells and make a diagnosis.
For example, if a patient presents with a palpable thyroid nodule, an FNA would help determine if it’s benign or malignant, avoiding the need for a larger, more invasive surgical biopsy in many cases.
Q 2. What are the key differences between FNA and core needle biopsy?
While both FNA and core needle biopsies are minimally invasive techniques used to obtain tissue samples, they differ significantly in the type and amount of tissue obtained. Think of FNA as sampling a soup – you get a collection of cells, while core needle biopsy is like taking a small cookie cutter from the loaf – you retrieve a cylindrical piece of tissue.
- FNA: Collects individual cells or small cell clusters. It’s quick, simple, and less painful. Ideal for lesions that are predominantly cellular, such as lymph node involvement or thyroid nodules. The diagnostic yield is often lower for solid tumors compared to core needle biopsies.
- Core Needle Biopsy: Extracts a cylindrical core of tissue, providing architectural information and allowing for a more comprehensive histological evaluation. It’s slightly more invasive than FNA, and the analysis includes the tissue structure (architecture) in addition to cellular analysis. This offers a more definitive diagnosis particularly for solid tumors, allowing for the evaluation of things like tissue invasion and necrosis, impossible to assess using FNA.
In practice, the choice between FNA and core needle biopsy depends on factors such as the location and nature of the lesion, the clinical suspicion, and the availability of the necessary equipment and expertise. A highly suspicious breast mass, for example, might warrant a core biopsy for more comprehensive evaluation, whereas an easily accessible superficial lymph node may suffice with FNA.
Q 3. Explain the Bethesda System for reporting cervical cytology results.
The Bethesda System is a standardized reporting system for cervical cytology (Pap smear) results, aiming to improve consistency and reduce variability in interpretation. It categorizes findings into diagnostic categories that guide subsequent management decisions.
The system includes:
- Negative for Intraepithelial Lesion or Malignancy (NILM): This indicates normal or benign cytological findings.
- Atypical Squamous Cells (ASC): Indicates abnormal squamous cells, but not definitive enough for a diagnosis of cancer or precancerous changes. It can be further categorized as ASC-US (Unspecified) or ASC-H (suggestive of high-grade changes).
- Low-Grade Squamous Intraepithelial Lesion (LSIL): Indicates mild dysplasia (abnormal cell growth), usually associated with HPV infection and often regresses spontaneously.
- High-Grade Squamous Intraepithelial Lesion (HSIL): Indicates moderate to severe dysplasia or carcinoma in situ (cancer confined to the surface layers of the cervix). Requires further investigation like colposcopy.
- Squamous Cell Carcinoma (SCC): Indicates invasive squamous cell cancer of the cervix.
- Atypical Glandular Cells (AGC): Suggests abnormal glandular cells (cells of the endocervical glands), requiring further investigation.
- Adenocarcinoma: Indicates invasive cancer arising from the glandular cells of the cervix.
- Other Specified findings: Additional categories exist to address specific findings.
The Bethesda System ensures clear communication between cytotechnologists, pathologists, and clinicians, leading to improved patient care. This structure helps to avoid ambiguous terminology and supports appropriate management strategies, like further investigations, which may involve colposcopy or further biopsies to resolve indeterminate results.
Q 4. How do you differentiate between reactive changes and cancerous cells on a Pap smear?
Differentiating reactive changes from cancerous cells on a Pap smear requires careful microscopic examination and experience. Reactive changes are cellular alterations triggered by inflammation or infection, while cancerous cells show marked cytological atypia indicating uncontrolled growth.
- Reactive Changes: Often characterized by increased cellularity, nuclear enlargement (but typically within limits), and hyperchromasia (darker staining nuclei), but the overall architecture is usually preserved. Inflammation might be evident from inflammatory cells present in the background.
- Cancerous Cells: Show significant nuclear atypia—increased size and variability in nuclear shape and size, irregular nuclear membranes, increased nuclear-to-cytoplasmic ratio (large nucleus relative to the cell size), and prominent nucleoli (dark-staining structures within the nucleus). Cell architecture is often disrupted. Cells may demonstrate high mitotic activity (cells undergoing division), and the overall cell population is markedly dysplastic.
For example, a Pap smear showing increased squamous cells with enlarged nuclei but no significant architectural disturbance and many inflammatory cells might be considered reactive. However, a smear showing individual cells with markedly enlarged, hyperchromatic and irregular nuclei, high N:C ratio, and loss of architectural cohesion would raise strong suspicion for malignancy.
The interpretation involves assessing several features collectively, not just a single characteristic. Experienced cytotechnologists and pathologists use their knowledge and experience to integrate all these aspects to reach a diagnosis, often relying on established criteria and guidelines.
Q 5. What are the common artifacts encountered in cytology preparations, and how do you address them?
Artifacts in cytology preparations can significantly hamper accurate diagnosis. They are essentially non-biological structures or alterations that mimic or obscure true cytological features.
- Drying artifacts: Cells may appear shrunken or distorted due to air drying before fixation.
- Fixative artifacts: Inadequate fixation can lead to poor cell preservation and structural alterations.
- Staining artifacts: Precipitation of stain or uneven staining can create background clutter and hinder cell examination.
- Contaminating debris: Blood, mucus, or other debris can obscure cellular details.
- Crush artifacts: Overzealous smearing can result in cell damage and distortion.
Addressing these artifacts involves careful specimen handling, proper fixation and staining techniques, and meticulous microscopic examination. Recognising these artifacts is vital as misinterpreting them as abnormal cells can lead to overdiagnosis. For example, an experienced cytotechnologist can differentiate a drying artifact causing nuclear pyknosis (shrinkage) from true nuclear changes in a malignant cell. Quality control measures, including standardised processing and well-trained technicians, are crucial in minimizing artifacts.
Q 6. Describe the different types of cell preservation methods used in cytology.
Cell preservation is crucial in cytology to maintain cellular morphology and prevent degradation, ensuring accurate diagnosis. Various methods are employed to achieve this.
- Alcohol-based fixation: Ethanol or methanol are commonly used. They quickly denature proteins, preserving cell structure. This is the standard for Pap smears and many FNAs.
- Cytospray fixation: This method uses a fine spray of fixative, ensuring rapid and even fixation of the cells, minimizing drying artifacts and improving the quality of cell preservation.
- Saccomanno fixative: A specialized fixative used to preserve the fine details of cells, often used for bronchial washings.
- Air-drying: Although less ideal for preserving fine cellular details compared to alcohol-based fixatives, air drying is used in some rapid staining techniques.
The choice of preservation method depends on the type of specimen, the intended staining technique, and the need for specific preservation of cellular components. For instance, alcohol-based fixation is ideal for standard Papanicolaou staining of cervical smears, preserving nuclear and cytoplasmic details. Whereas cytospray offers advantages for preserving cellular morphology in liquid-based cytology.
Q 7. What are the limitations of FNA in diagnosing certain malignancies?
FNA has limitations in diagnosing certain malignancies, primarily due to its reliance on obtaining a representative sample of cells. It doesn’t provide tissue architecture, which is crucial for some diagnoses.
- Low cellularity: Some lesions may yield insufficient cells for diagnosis.
- Sampling error: The needle may miss areas of malignancy within a larger lesion.
- Necrosis and inflammation: Extensive necrosis or inflammation can obscure malignant cells.
- Difficulties in diagnosing specific subtypes: Distinguishing certain subtypes of malignancies can be challenging based solely on cellular morphology.
- Architectural information loss: The lack of tissue architecture makes assessment of things like invasion, glandular differentiation, and necrosis challenging.
For instance, diagnosing subtle architectural features of certain breast cancers or evaluating the invasiveness of a tumor is difficult with FNA alone. In such cases, a core needle biopsy or surgical excisional biopsy might be necessary for a definitive diagnosis. It is important to remember that FNA is a valuable screening tool, but limitations should be considered, and results interpreted within the clinical context of the patient’s presentation. A negative FNA should not necessarily completely exclude malignancy, and further investigation may be necessary if clinical suspicion remains high.
Q 8. How do you handle inadequate or unsatisfactory cytology specimens?
Handling inadequate cytology specimens is crucial for patient safety and accurate diagnosis. An inadequate specimen, meaning insufficient cellular material for proper evaluation, results in an inconclusive diagnosis. This isn’t a diagnosis itself; it’s a call for further investigation.
My approach involves a multi-step process: First, I carefully review the clinical history and correlate it with the cytology preparation. Sometimes, a seemingly inadequate sample might suffice if the clinical picture is highly suggestive of a specific diagnosis. Second, if the sample is truly inadequate – lacking cellularity or exhibiting significant artifacts – I would consult with the referring physician. We may discuss the need for a repeat procedure, perhaps with a different technique or using a different site. For instance, a poorly performed fine needle aspiration (FNA) of a thyroid nodule might be repeated using ultrasound guidance. Third, detailed documentation is essential. The cytology report clearly states the reason for inadequacy, suggesting alternative diagnostic steps. This protects both the patient and the healthcare provider from potential misunderstandings and ensures that the patient receives the necessary follow-up care.
Q 9. Explain the significance of cellular morphology in cytological diagnosis.
Cellular morphology—the study of cell shape, size, and internal structures—is the cornerstone of cytological diagnosis. It’s like being a detective, piecing together clues from the microscopic world to identify the culprit – in this case, a disease process. By examining the nucleus (size, shape, chromatin pattern, nucleoli), cytoplasm (amount, color, inclusions), and the overall cell arrangement, we can differentiate between normal and abnormal cells, and even classify the type of abnormality (e.g., reactive, inflammatory, neoplastic).
For example, in a pap smear, the presence of large, hyperchromatic (darkly stained) nuclei with irregular shapes and increased nucleoli in squamous cells strongly suggests malignancy (e.g., cervical cancer). In contrast, benign cells show uniform morphology and normal nuclear-to-cytoplasmic ratios. The interpretation of cellular morphology requires significant training and experience to recognize subtle yet crucial features distinguishing benign from malignant cells.
Q 10. Describe the role of immunocytochemistry in cytology.
Immunocytochemistry (ICC) is a powerful ancillary technique in cytology. It uses antibodies to identify specific proteins within cells, enhancing diagnostic accuracy, especially in challenging cases. Think of it as adding another layer of detail to our microscopic investigation. Antibodies bind to specific target proteins, revealing their presence or absence within cells, which allows us to classify them further.
For instance, in a thyroid FNA, ICC can distinguish between different types of thyroid cancers based on the expression of specific markers such as thyroglobulin (for thyroid follicular cells) and calcitonin (for medullary thyroid cancer). In suspected lymphomas, specific antibodies are used to characterize the lymphoma type. ICC isn’t always necessary, but it’s extremely helpful when the morphology alone is ambiguous or insufficient for a definitive diagnosis.
Q 11. What are the common cytological findings in inflammatory conditions?
Inflammatory conditions show distinct cytological features, primarily reflecting the body’s immune response. The most common findings include an increased number of inflammatory cells, such as neutrophils, lymphocytes, and macrophages.
For example, in acute inflammation, you’ll see a predominance of neutrophils, often exhibiting signs of degeneration. In chronic inflammation, lymphocytes and macrophages are more abundant. Other findings can include reactive mesothelial cells (in serous effusions) and histiocytes (cells involved in tissue repair and cleanup). The background often shows increased cellular debris and inflammatory exudate. It’s crucial to remember that while these inflammatory features are common, they are usually benign; it’s the context and correlation with clinical information that is crucial for proper interpretation. For example, reactive changes in a cervical smear may be associated with infection and thus benign, but similar changes in a lung biopsy could be a reactive phenomenon alongside a malignancy.
Q 12. How do you differentiate between benign and malignant thyroid nodules on FNA?
Differentiating between benign and malignant thyroid nodules on FNA is a key skill in cytopathology. It requires a careful analysis of nuclear features, cellular arrangement, and the presence of any suspicious characteristics.
Benign nodules typically show a uniform population of follicular cells with bland nuclear features (small, round, evenly distributed chromatin). The cells are often arranged in cohesive clusters or microfollicles. In contrast, malignant nodules often exhibit nuclear atypia (enlarged, irregular, hyperchromatic nuclei), increased nuclear-to-cytoplasmic ratios, and an overall disordered cellular arrangement. Features suggestive of malignancy include nuclear pleomorphism (variation in nuclear size and shape), prominent nucleoli, and the presence of psammoma bodies (concentric calcifications). However, some lesions are indeterminate, requiring further investigations like molecular testing or surgical excision for final diagnosis. It’s important to note that the Bethesda System for Reporting Thyroid Cytopathology provides standardized terminology for reporting results and helps reduce ambiguity.
Q 13. Explain the role of molecular testing in cytological diagnosis.
Molecular testing has revolutionized cytological diagnosis, providing additional information beyond morphological features. Techniques like polymerase chain reaction (PCR) and fluorescence in situ hybridization (FISH) detect specific genetic abnormalities associated with malignancy.
For example, in thyroid FNA, molecular testing can detect mutations in genes such as BRAF and RET, which are commonly associated with papillary thyroid cancer. In non-small cell lung cancer, the identification of specific mutations (e.g., EGFR, ALK) guides therapeutic decisions. Molecular testing is particularly useful in resolving indeterminate cytology results and for guiding management decisions, helping to differentiate between benign and malignant lesions when morphology alone is inconclusive. It helps in risk stratification and can ultimately improve patient outcomes.
Q 14. Describe your experience with quality control and quality assurance in a cytology laboratory.
Quality control (QC) and quality assurance (QA) are paramount in a cytology laboratory to ensure the accuracy and reliability of diagnoses. This involves a multifaceted approach that addresses every step of the process, from specimen collection to reporting.
My experience includes implementing and adhering to stringent QC protocols, encompassing daily checks of equipment (microscopes, staining machines), regular proficiency testing to evaluate the accuracy of our interpretation and ensure competency, and internal quality audits to verify the standardization and consistency of our procedures. We use standardized staining techniques and follow established reporting guidelines like the Bethesda System. Regular review of cases by multiple cytotechnologists and pathologists ensures the quality and accuracy of our interpretations. Moreover, we meticulously track and analyze our results, identifying areas for potential improvement and addressing discrepancies promptly. Continuous improvement is a vital aspect of QA, and regular participation in continuing medical education keeps us updated with the latest advancements and guidelines. This rigorous approach ensures high-quality patient care and minimizes diagnostic errors.
Q 15. What are the safety precautions you take while performing FNA procedures?
Safety is paramount during Fine Needle Aspiration (FNA) procedures. My protocol begins with meticulous hand hygiene and donning appropriate personal protective equipment (PPE), including gloves, gown, and eye protection. The patient’s skin is cleaned with an antiseptic solution. I carefully explain the procedure to the patient, addressing any anxieties and obtaining informed consent. During the procedure itself, I use a small-gauge needle to minimize trauma and bleeding. Constant monitoring of the patient’s vital signs is crucial, particularly in cases involving larger or deeper lesions. After the procedure, the puncture site is dressed with a sterile bandage and the patient is monitored for any adverse reactions or complications like hematoma formation. Proper disposal of needles and other sharps, following established infection control guidelines, is essential. For example, in a thyroid FNA, extra care is taken to avoid puncturing major blood vessels. If unexpected bleeding occurs, pressure is immediately applied to the site, and appropriate intervention like sutures may be needed.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you manage difficult or complex cases in cytology?
Managing complex cytology cases involves a multi-faceted approach. Firstly, I ensure high-quality sample collection and preparation to maximize diagnostic yield. This includes utilizing appropriate fixation techniques and optimal staining methods, such as Papanicolaou stain for Pap smears and Giemsa stain for FNAs. If the initial cytological findings are inconclusive, I carefully correlate the cytological features with the patient’s clinical history, imaging studies (such as ultrasound or CT scans), and other relevant diagnostic information. Consulting with experienced colleagues or specialists, particularly in cases of rare or unusual cytological presentations, is vital. When faced with challenging differential diagnoses, I may order additional tests, such as immunocytochemistry or molecular studies, to refine the diagnosis. For instance, a case of suspicious thyroid nodules might require further testing with immunocytochemistry to distinguish between follicular adenoma and follicular carcinoma. The iterative process of correlation and further investigation allows me to arrive at the most accurate and reliable diagnosis possible.
Q 17. Describe your experience with different types of microscopes used in cytology.
My experience encompasses a range of microscopes commonly used in cytology. I’m proficient with brightfield microscopy for routine cytological examination, utilizing different magnifications to assess cellular morphology and architectural features. I also have significant experience with fluorescence microscopy, which is crucial for immunocytochemical studies, allowing visualization of specific cellular components using fluorescently labeled antibodies. Furthermore, I’m familiar with digital microscopy systems that allow for image capture, storage, and analysis. This aids in better record-keeping, facilitates consultations with other specialists, and even enables remote diagnosis. The transition to digital microscopy has substantially improved efficiency and collaborative possibilities. For example, using a fluorescence microscope with an appropriate antibody panel is crucial for identifying specific types of lymphoma.
Q 18. What is your familiarity with digital imaging and telecytology?
I have extensive experience with digital imaging in cytology. We use digital microscopes and scanners routinely to create high-resolution images of cytological specimens. These images are integrated into our laboratory information system (LIS), ensuring secure storage and easy access. Digital imaging improves efficiency, facilitates remote consultations, and allows for quantitative image analysis. Telecytology, which involves the remote interpretation of digital cytological images, is increasingly important. This allows for the sharing of expertise across geographical locations, especially beneficial in underserved areas or for rare cases requiring specialized consultation. The use of secure, HIPAA-compliant platforms for image transmission is critical for maintaining patient confidentiality and data integrity. This technology facilitates the efficient exchange of images for second opinions or consultations with specialists.
Q 19. How do you ensure patient confidentiality in cytology practice?
Patient confidentiality is a core value in my practice. We adhere strictly to HIPAA regulations and our institution’s privacy policies. Patient identifiers are carefully managed throughout the entire process, from sample collection and labeling to reporting and storage. All digital images and records are stored securely on password-protected servers with access limited to authorized personnel. We use de-identified data for quality assurance and research purposes. For instance, we might use anonymized data to track diagnostic accuracy or compare different staining techniques. Our commitment to patient privacy extends beyond regulations; it’s an integral aspect of our professional ethics.
Q 20. What are the ethical considerations in reporting cytology results?
Ethical considerations in reporting cytology results are paramount. Accuracy, objectivity, and clarity are essential. The report should be easily understandable to the referring physician, avoiding technical jargon where possible. It’s crucial to avoid over-interpretation and to clearly state the limitations of the test. We always strive to report results in a timely and responsible manner. In cases of critical findings, such as malignancy, I ensure immediate communication with the referring physician. Providing appropriate counseling and support to the patient, while respecting their emotional needs, is also an ethical responsibility, even though it’s usually the role of the patient’s physician.
Q 21. Explain your understanding of the legal implications of cytology reporting.
Legal implications of cytology reporting are significant. Accurate and timely reporting is crucial, as misdiagnosis can have severe consequences for the patient. Maintaining meticulous records, including detailed case notes and images, is vital for legal protection. Adherence to all relevant regulations and guidelines is mandatory. We regularly review and update our procedures to ensure compliance. Malpractice claims can arise from errors in diagnosis or reporting, emphasizing the necessity of precise and well-documented assessments. Maintaining professional liability insurance is crucial. Ultimately, responsible and ethical practice minimizes legal risks and protects both the patient and the cytologist.
Q 22. How do you stay updated with the latest advancements in cytology?
Staying current in the rapidly evolving field of cytology requires a multi-pronged approach. I prioritize continuous professional development through several key strategies.
Professional Organizations: Active membership in organizations like the American Society for Clinical Pathology (ASCP) and the International Academy of Cytology (IAC) provides access to journals, conferences, and webinars featuring the latest research and techniques. For example, I recently attended an IAC webinar on the application of artificial intelligence in cervical cancer screening, which significantly broadened my understanding of emerging technologies.
Peer-Reviewed Journals: I regularly read journals such as Diagnostic Cytopathology and Acta Cytologica to stay abreast of groundbreaking studies and case reports. This allows me to critically evaluate new diagnostic methodologies and their impact on patient care.
Continuing Medical Education (CME): I actively participate in CME courses and workshops focused on advanced cytological techniques, such as liquid-based cytology and fine-needle aspiration (FNA) cytology of challenging sites. Recently, I completed a course on the cytologic features of various salivary gland tumors, which enhanced my diagnostic accuracy in this complex area.
Professional Networks: Engaging with colleagues through conferences and online forums fosters knowledge exchange and allows me to learn from the experiences of others. Discussions with experienced cytotechnologists often provide valuable insights into practical challenges and innovative solutions.
Q 23. Describe your experience working in a team environment in a cytology laboratory.
Teamwork is fundamental to the success of any cytology laboratory. In my previous role, I collaborated closely with cytotechnologists, pathologists, and laboratory assistants within a fast-paced environment. Effective communication was key. For example, we used a daily case review process where we would discuss challenging cases, share insights, and ensure consistent interpretation. We also utilized a collaborative case management system to track specimens and ensure timely turnaround times. This system helped us manage workload efficiently, reducing potential bottlenecks and improving overall efficiency. I believe in fostering a supportive environment where everyone feels comfortable sharing ideas and seeking help. This collaborative approach not only enhanced our diagnostic accuracy but also improved morale and job satisfaction.
Q 24. How do you handle stressful situations in a busy cytology laboratory?
High-volume cytology laboratories can be incredibly demanding. To handle stress effectively, I employ several strategies. Firstly, I prioritize organization and time management. I develop and adhere to a structured workflow to ensure efficient processing of specimens. Secondly, I maintain a calm and focused demeanor, even under pressure. I believe that a methodical approach combined with clear communication with my colleagues helps to diffuse tense situations. For instance, during periods of high workload, I’ve found that proactive communication regarding anticipated delays to pathologists helps maintain transparency and avoids misunderstandings. Finally, recognizing the importance of self-care, I maintain a healthy work-life balance to avoid burnout. This includes regular exercise, sufficient sleep, and time spent on activities outside of work.
Q 25. Describe a challenging case you have encountered and how you resolved it.
One challenging case involved a fine-needle aspiration (FNA) of a thyroid nodule. The cytology showed a predominantly follicular pattern with some areas suggestive of malignancy. The initial interpretation was indeterminate. This presented a diagnostic dilemma, as indeterminate cytology often necessitates surgical intervention. To resolve this, I collaborated closely with the pathologist. We reviewed the slides meticulously, focusing on subtle nuclear features and cellular arrangements. We also consulted additional literature and discussed the case with other experienced colleagues. Ultimately, after extensive evaluation and correlation with clinical information, including ultrasound imaging, we reached a consensus that the cytological features leaned slightly towards a benign diagnosis, leading to more conservative management with close clinical follow-up. The patient avoided unnecessary surgery, and further imaging later confirmed the benign nature of the nodule. This experience reinforced the importance of thorough evaluation, collaboration, and the integration of clinical data into cytological interpretation.
Q 26. What are your strengths and weaknesses as a cytotechnologist?
My strengths lie in my meticulous attention to detail, strong analytical skills, and ability to work effectively both independently and as part of a team. I’m a quick learner and adept at adapting to new technologies and techniques. For example, I readily embraced the transition to liquid-based cytology and quickly became proficient in the interpretation of these preparations. A weakness I’m actively working on is delegation. While I enjoy taking ownership of tasks, I recognize the importance of effectively delegating responsibilities to optimize workflow efficiency within the team.
Q 27. Where do you see yourself in 5 years in the field of cytology?
In five years, I envision myself as a highly skilled and experienced cytotechnologist, contributing significantly to the advancement of the field. I aim to enhance my expertise in advanced cytological techniques, potentially specializing in a particular area such as gastrointestinal cytology or body fluid cytology. I also aspire to take on more leadership responsibilities, mentoring junior cytotechnologists and contributing to the development of new protocols and quality improvement initiatives within the laboratory. Further, I plan to pursue opportunities for professional development, possibly through further education or advanced certifications.
Q 28. Why are you interested in this particular cytology position?
I’m particularly interested in this cytology position because of [Laboratory Name]’s reputation for excellence and its commitment to innovation. I’ve been consistently impressed by [Laboratory Name]’s pioneering work in [mention specific area of laboratory’s expertise], and I’m eager to contribute my skills and experience to such a forward-thinking organization. The opportunity to collaborate with experienced cytotechnologists and pathologists within a supportive environment is incredibly appealing, and I believe that my skills and work ethic align perfectly with the values and goals of [Laboratory Name].
Key Topics to Learn for Cytology (e.g., FNA, pap smears) Interview
- Specimen Collection & Handling: Understanding proper techniques for FNA and Pap smear collection, including patient preparation, specimen adequacy, and preventing artifacts.
- Microscopic Examination & Interpretation: Mastering the identification of normal and abnormal cellular features in both FNA and Pap smears, including recognizing benign, precancerous, and cancerous changes.
- Cellular Morphology & Differential Diagnosis: Developing expertise in differentiating various cell types and recognizing subtle morphological clues to arrive at an accurate diagnosis. This includes understanding the limitations of cytology and knowing when to request additional testing.
- Quality Assurance & Quality Control: Familiarity with laboratory protocols, proficiency testing, and understanding the importance of maintaining quality standards in cytology practice.
- Reporting & Communication: Crafting clear, concise, and informative cytology reports that effectively communicate findings to clinicians. Understanding the implications of different diagnostic categories and their impact on patient management.
- Common Cytologic Diagnoses: Deep understanding of the cytological presentation of common conditions such as cervical dysplasia, endometrial hyperplasia, thyroid nodules, and breast lesions.
- Ancillary Techniques: Knowledge of immunocytochemistry, flow cytometry, and molecular techniques used in cytology for diagnostic confirmation and subtyping.
- Ethical & Legal Considerations: Understanding patient confidentiality, proper handling of sensitive results, and adherence to professional guidelines.
Next Steps
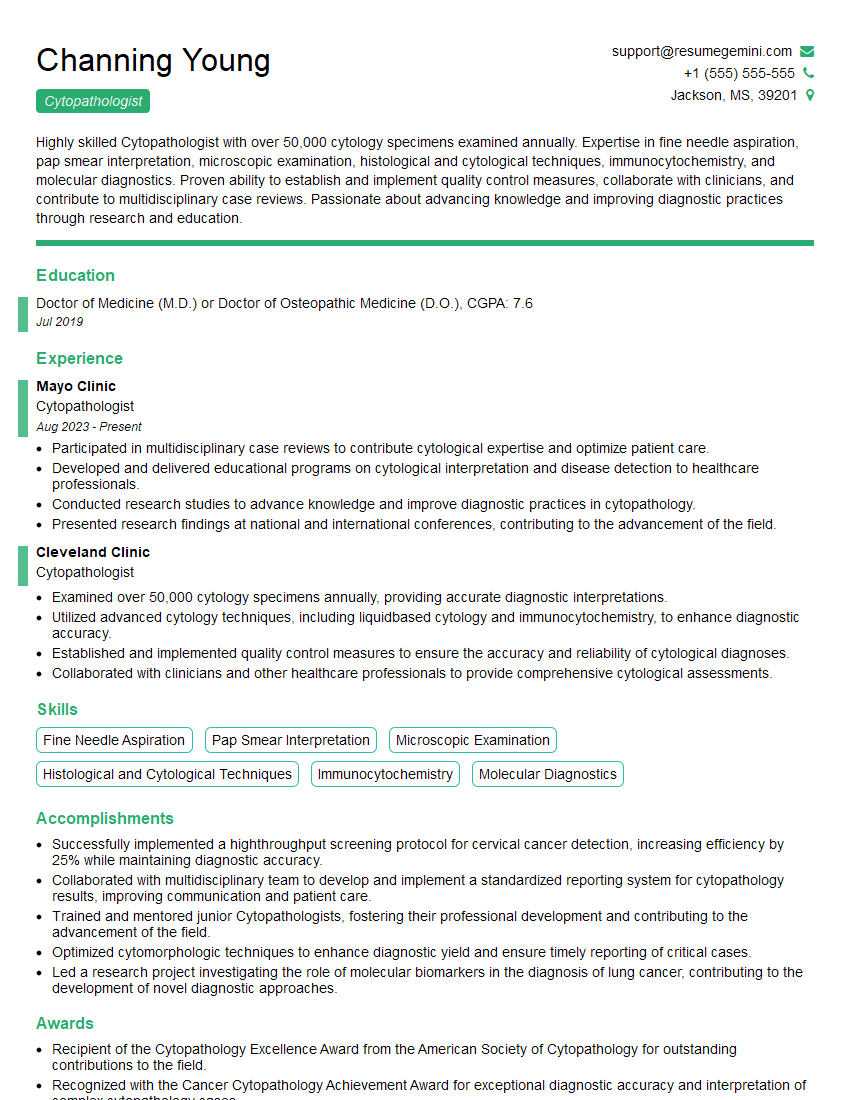
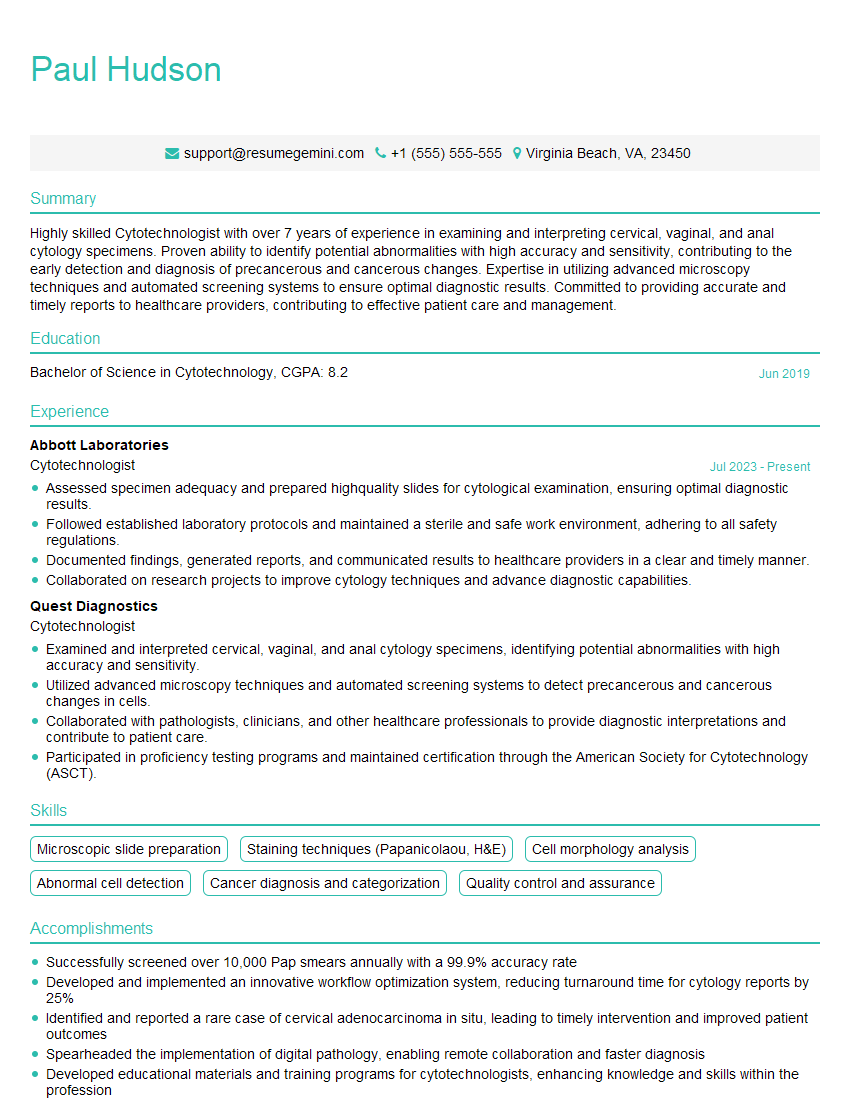
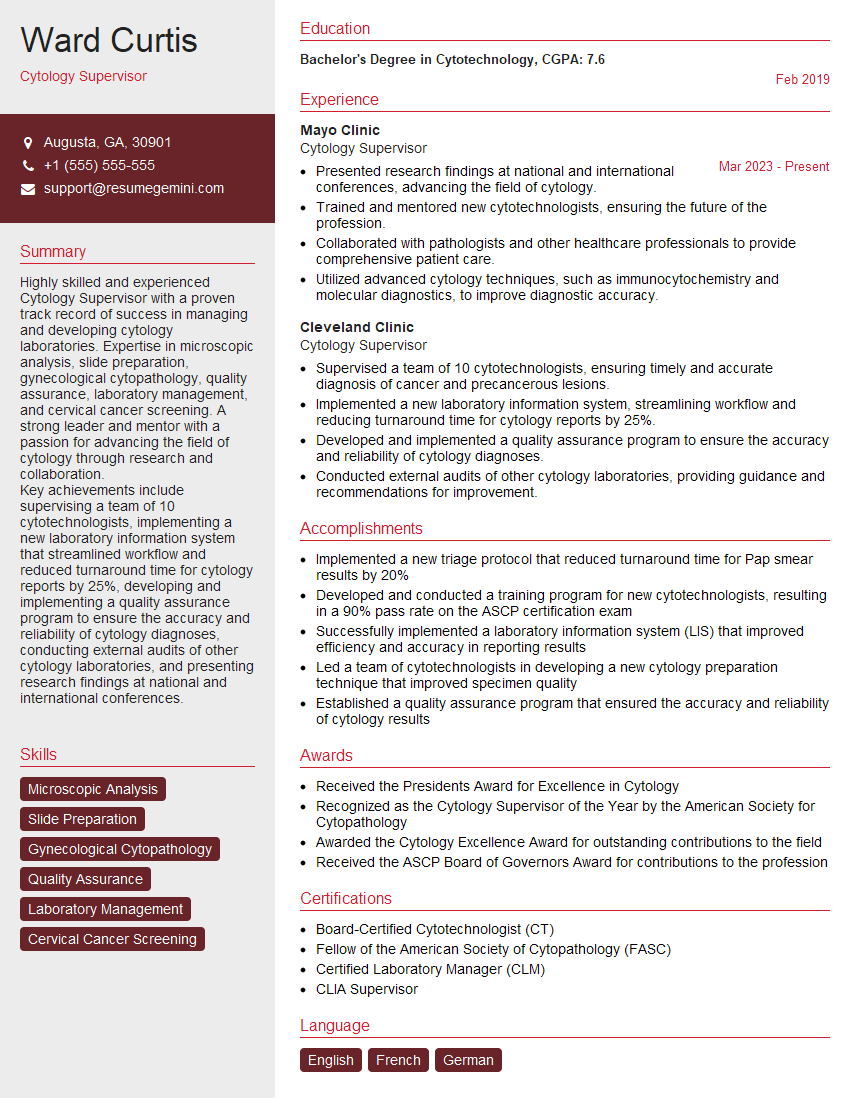
Mastering cytology, particularly FNA and Pap smear interpretation, is crucial for career advancement in pathology and related fields. It demonstrates a high level of expertise and opens doors to specialized roles and increased responsibility. To significantly boost your job prospects, crafting an ATS-friendly resume is vital. ResumeGemini is a trusted resource that can help you build a professional and effective resume that highlights your skills and experience. Examples of resumes tailored specifically to Cytology, including expertise in FNA and Pap smears, are available to help you present your qualifications in the best possible light.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.