Cracking a skill-specific interview, like one for Cytology Interpretation, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Cytology Interpretation Interview
Q 1. Describe the Pap smear collection and preparation process.
The Pap smear, or cervical cytology, is a crucial screening test for cervical cancer. The collection process involves using a spatula and a cytobrush to gently collect cells from the transformation zone of the cervix – the area where the squamous epithelium meets the columnar epithelium, a common site for precancerous and cancerous changes. This ensures a representative sample.
After collection, the sample is either directly placed onto a glass slide for conventional Pap staining or into a liquid-based preparation, such as ThinPrep, which allows for better cell dispersion and visualization. In liquid-based preparations, the cells are processed and then transferred to a slide. The slides are then fixed and stained, usually with Papanicolaou (Pap) stain, a multi-chromatic stain which allows for differentiation of different cell types based on their nuclear and cytoplasmic characteristics. This staining process highlights the cellular features crucial for diagnosis.
Q 2. Explain the different types of cellular atypia seen in cervical cytology.
Cellular atypia refers to abnormalities in cell morphology that deviate from the normal pattern. In cervical cytology, several types exist, ranging from benign reactive changes to precancerous and cancerous lesions.
- Reactive changes: These are non-neoplastic changes triggered by inflammation (e.g., infection), radiation, or hormonal influences. Cells may appear enlarged with increased nuclear size, but without significant architectural disruption.
- Atypical squamous cells of undetermined significance (ASCUS): This category represents cells with subtle abnormalities, insufficient to diagnose a specific condition. Further investigation (like HPV testing or colposcopy) is often needed.
- Atypical squamous cells, cannot exclude high-grade squamous intraepithelial lesion (ASC-H): This suggests a higher risk of high-grade precancerous changes. Immediate colposcopy is recommended.
- Low-grade squamous intraepithelial lesion (LSIL): Represents mild dysplasia (abnormal cell growth), often associated with HPV infection. Often regresses spontaneously.
- High-grade squamous intraepithelial lesion (HSIL): Shows moderate to severe dysplasia, indicating a higher risk of progression to cancer. Colposcopy with biopsy is essential.
- Atypical glandular cells (AGC): This refers to abnormal glandular cells, possibly originating from the endocervical or endometrial glands. AGC requires further investigation to rule out endocervical or endometrial cancer.
Q 3. How do you differentiate between reactive changes and dysplasia in a cervical smear?
Differentiating reactive changes from dysplasia requires careful assessment of several cytological features. Reactive changes typically demonstrate inflammation with associated inflammatory cells (e.g., neutrophils). Cells might be enlarged but maintain overall cohesiveness and a relatively normal nuclear-cytoplasmic ratio. Dysplasia, however, shows more significant nuclear atypia, including nuclear enlargement, hyperchromasia (darker staining), increased nuclear-cytoplasmic ratio, and often loss of cell maturation in the squamous epithelium. Architectural abnormalities, such as loss of cell polarity and crowding, are more prominent in dysplastic cells.
A crucial distinction lies in the degree of nuclear abnormality and the overall pattern of cell growth. In reactive changes, nuclear changes are typically mild and uniform, while dysplastic cells show more marked and variable nuclear atypia. Experience and meticulous observation are key to accurate differentiation.
Q 4. What are the Bethesda system classifications for cervical cytology?
The Bethesda System is the standardized reporting system for cervical cytology. It focuses on descriptive terminology, avoiding subjective interpretations. Key classifications include:
- Negative for intraepithelial lesion or malignancy: No abnormal cells detected.
- Atypical squamous cells of undetermined significance (ASCUS): Subtle abnormalities, requiring further investigation.
- Atypical squamous cells, cannot exclude high-grade squamous intraepithelial lesion (ASC-H): Suggests high-grade abnormality requiring colposcopy.
- Low-grade squamous intraepithelial lesion (LSIL): Mild dysplasia.
- High-grade squamous intraepithelial lesion (HSIL): Moderate to severe dysplasia.
- Squamous cell carcinoma: Malignant squamous cells.
- Atypical glandular cells (AGC): Abnormal glandular cells requiring further investigation.
- Endocervical adenocarcinoma: Malignant glandular cells of the endocervix.
- Adenocarcinoma: Malignant glandular cells (often endometrial).
- Other findings (e.g., inflammation, infection): These provide additional clinically relevant information.
Q 5. Explain your approach to interpreting a ThinPrep Pap smear.
Interpreting a ThinPrep Pap smear involves a systematic approach. I begin with a low-power scan to assess overall cellularity and identify any areas of interest. This provides a general overview of the specimen’s quality and highlights any potential abnormalities. I then proceed to high-power examination, meticulously evaluating individual cells for nuclear and cytoplasmic features such as size, shape, chromatin pattern, and nuclear-cytoplasmic ratio.
The ThinPrep method provides superior cellular dispersion compared to conventional Pap smears, facilitating easier identification of individual cells and improved diagnostic accuracy. The key is to systematically evaluate thousands of cells to identify any atypical cells. The presence of inflammatory cells and the type of inflammatory cells present (neutrophils, lymphocytes, etc.) are also carefully noted, as these findings provide clues to the underlying pathology.
Finally, I correlate cytological findings with the patient’s clinical history and risk factors to arrive at a final diagnosis. For example, a postmenopausal woman presenting with atypical glandular cells would prompt further investigation with more urgency than a young woman with similar findings.
Q 6. Describe the process of evaluating a fine-needle aspiration (FNA) cytology specimen.
Evaluating a fine-needle aspiration (FNA) cytology specimen involves a multi-step process. First, the adequacy of the sample is assessed – ensuring sufficient cellularity and lack of excessive blood or debris. Then, the preparation’s cellular components are examined systematically. I assess cellular features like size, shape, nuclear-to-cytoplasmic ratio, nuclear chromatin pattern, and the presence or absence of nucleoli. The arrangement of cells, whether they are single, in clusters, or in sheets, is important.
In addition, the presence of any background material such as necrosis, inflammation, or hemorrhage is also noted. These features, taken together, provide crucial information about the tissue’s nature (benign, malignant or indeterminate). For example, the presence of single cells with marked nuclear atypia, high nuclear-to-cytoplasmic ratio, and prominent nucleoli in a background of necrosis might be indicative of malignancy. I carefully correlate these cytological features with the clinical history of the patient to reach a final diagnosis.
Q 7. What are the key features of malignant cells in cytology?
Malignant cells in cytology exhibit several key features that distinguish them from benign cells. These features aren’t always present in isolation, and the combination of these features is crucial for diagnosis. Key features include:
- Nuclear pleomorphism: Variation in nuclear size and shape.
- Increased nuclear-to-cytoplasmic ratio: The nucleus occupies a disproportionately large area of the cell.
- Hyperchromasia: Darkly stained, condensed chromatin.
- Prominent nucleoli: Large, dark staining structures within the nucleus.
- Mitotic figures: Visible dividing cells, indicative of rapid cell proliferation.
- Loss of cell polarity and cohesiveness: Cells lack normal organization and adhesion.
- Nuclear molding: Nuclei are deformed due to mutual compression.
- Necrosis: Cell death, often associated with aggressive malignancies.
It’s important to emphasize that the presence of any single characteristic doesn’t necessarily indicate malignancy; it’s the aggregate of cytological features combined with clinical information that allows for an accurate diagnosis.
Q 8. How do you identify and report infectious agents in cytology specimens?
Identifying infectious agents in cytology specimens involves a multi-pronged approach combining microscopic examination with ancillary techniques. Initially, we look for characteristic cytopathic effects – changes in cell morphology indicative of infection. For example, we might see multinucleated giant cells suggestive of viral infections like herpes simplex virus or cytomegalovirus, or intracellular bacteria like Chlamydia trachomatis within the cytoplasm of infected cells.
Beyond morphology, special stains like Gram stain, Giemsa stain, and Periodic acid–Schiff (PAS) stain can help detect and identify bacteria, fungi, and parasites, respectively. For example, a PAS stain is crucial for identifying fungal elements like Candida species. Immunocytochemistry (ICC) is also a powerful tool. Using specific antibodies, we can identify viral antigens or bacterial components within infected cells. Finally, molecular techniques like polymerase chain reaction (PCR) can detect the genetic material of infectious agents even when morphological or staining changes are subtle or absent, increasing sensitivity and specificity significantly. The reporting of infectious agents includes specifying the organism if possible, its location (e.g., intracellular, extracellular), abundance, and the implications for the patient’s condition.
Q 9. Explain the significance of finding atypical glandular cells (AGC) on a Pap smear.
Finding atypical glandular cells (AGC) on a Pap smear is a significant finding because it indicates the presence of glandular cells that show abnormalities but don’t clearly fit the criteria for either a benign or a malignant diagnosis. It sits in a grey area. AGC is not a definitive diagnosis itself; it’s a category indicating a need for further investigation to rule out malignancy. The significance lies in the potential for underlying endometrial or endocervical adenocarcinoma. The subtype of AGC (AGC-favor-neg or AGC-favor-pos) influences the recommended follow-up. AGC-favor-negative suggests less likelihood of malignancy, while AGC-favor-positive suggests a higher risk. The follow-up typically involves colposcopy with directed biopsies to definitively characterize the glandular cells and determine whether they are benign, pre-cancerous, or cancerous. Delaying the follow-up for AGC can have serious consequences because early detection of endometrial or endocervical cancer dramatically improves prognosis.
Q 10. Describe the different types of non-gynecologic cytology specimens you have experience with.
My experience encompasses a wide range of non-gynecologic cytology specimens, including fine-needle aspiration (FNA) biopsies from various organs. This includes thyroid FNA, which is vital for evaluating thyroid nodules and differentiating benign from malignant lesions. I’ve extensively worked with body fluid cytology, analyzing specimens such as pleural fluid, peritoneal fluid, cerebrospinal fluid, and pericardial fluid to diagnose conditions like malignancy, infections, and inflammatory processes. Additionally, I’ve reviewed urine cytology samples to detect urinary tract infections, inflammation, and malignancy. I also have experience with non-gastrointestinal specimens like lymph node aspirates for lymphoma or metastasis evaluation. In each case, the approach involves careful microscopic evaluation, correlating cytological features with clinical history and utilizing ancillary tests as needed for accurate diagnosis.
Q 11. How do you handle inadequate or unsatisfactory cytology specimens?
Handling inadequate or unsatisfactory cytology specimens requires a structured approach that ensures patient safety and efficient use of resources. Inadequate specimens are often characterized by insufficient cellular material or obscuring factors that prevent proper evaluation. The first step is to carefully review the specimen for any potential technical issues – issues with sample collection, processing, or preparation. If the inadequacy is due to technical error, a repeat sample may be requested. When this is not possible, we may need to supplement with additional tests, for example a repeat smear. If the initial specimen is deemed truly insufficient to offer even a preliminary diagnosis, this is clearly reported using standardized terminology, e.g., “insufficient for evaluation,” thereby preventing the misinterpretation of a poor specimen, rather than recommending an appropriate course of action. This information ensures the clinician is aware of the limitations and can decide on the next appropriate step.
Q 12. What quality control measures are essential in a cytology laboratory?
Quality control is paramount in a cytology laboratory. We employ several measures to ensure accuracy and reliability. These include rigorous adherence to standardized procedures for specimen collection, processing, and staining. We participate in proficiency testing programs, where we analyze anonymized samples alongside other laboratories to benchmark our performance and identify areas for improvement. Regular calibration and maintenance of equipment, such as microscopes and automated screening systems, are critical. Internal quality control measures consist of running control slides at regular intervals to ensure staining quality and the functioning of our equipment. We meticulously document all steps in the process, adhering to strict chain of custody to guarantee specimen integrity. Finally, regular internal audits and external inspections, done by accrediting bodies, help maintain quality standards and identify areas needing improvement. This all ensures reliable and high-quality cytology results are produced.
Q 13. Describe your experience with using automated screening systems in cytology.
I have extensive experience with automated screening systems in cytology, primarily using image analysis software for Pap smear screening. These systems help in pre-screening samples and identifying areas of interest that require the cytotechnologist’s review. These systems are not designed to replace human interpretation but rather to assist and improve efficiency. The software analyzes cell morphology, identifying potentially abnormal cells that need detailed review by an experienced cytotechnologist. This helps triage samples, ensuring that abnormal cases are prioritized and reviewed promptly, while minimizing the review of normal cases and improving turnaround time for results. However, we must remember that the computer can only detect what it is programmed to look for; therefore, meticulous quality assurance measures are needed to identify cases that require secondary review.
Q 14. How do you interpret immunocytochemistry results in cytology?
Interpreting immunocytochemistry (ICC) results in cytology involves correlating the staining patterns with the morphological features of the cells. ICC uses specific antibodies to detect and localize particular antigens within cells. For example, in a suspected lymphoma, we might use antibodies against CD20 (a B-cell marker) or CD3 (a T-cell marker) to classify the type of lymphoma. The interpretation considers the intensity of staining (strong, weak, absent), the percentage of positive cells, and the staining pattern (membranous, cytoplasmic, nuclear). For example, a strong membranous staining for CD20 on a majority of cells would strongly suggest a B-cell lymphoma. Accurate interpretation requires a deep understanding of the different antigens and their expression patterns in various cell types. It also requires careful consideration of the clinical context, as the ICC findings must be correlated with the patient’s history and other diagnostic data. False-positive and false-negative results are possible; therefore, experienced interpretation is crucial for accurate diagnostic conclusions.
Q 15. How do you handle discrepancies between cytology and histology results?
Discrepancies between cytology and histology results are not uncommon and often highlight the inherent limitations of each technique. Cytology, being a less invasive procedure examining individual cells, can provide a rapid preliminary diagnosis but might miss subtle architectural features. Histology, examining tissue sections, offers a more complete picture of tissue organization and cellular context. When discrepancies arise, I follow a systematic approach:
- Review both reports meticulously: I carefully examine the cytology slides and the histology report, paying close attention to the specific findings and interpretations. I look for possible explanations for the differences, such as sampling error (different areas of the lesion sampled), the nature of the lesion (e.g., a heterogeneous tumor), or limitations of the techniques.
- Correlate clinical information: The patient’s clinical presentation, imaging findings, and other relevant medical history are vital in resolving discrepancies. This broader context often provides clues to reconcile seemingly conflicting results.
- Consult with colleagues: I frequently discuss challenging cases with experienced pathologists and cytopathologists, benefiting from their diverse perspectives and expertise. A multidisciplinary approach enhances diagnostic accuracy.
- Consider additional testing: If the discrepancy remains unresolved, further investigations such as immunohistochemistry (IHC) on the tissue section or repeat cytology may be necessary to clarify the diagnosis.
- Document findings thoroughly: All steps undertaken in resolving the discrepancy, along with the final conclusions, are meticulously documented in the patient’s medical record, ensuring transparency and facilitating future reference.
For example, a cytology report might suggest a benign process while histology reveals a low-grade malignancy. This could be due to the cytology sample being taken from a non-representative area of the lesion, containing only benign cells, whereas the histology section provides a broader view revealing malignant features in other parts of the lesion. Careful correlation with the clinical picture and possible repeat sampling would be necessary to reach a definitive diagnosis.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What is your experience with frozen section cytology?
My experience with frozen section cytology is limited, as it’s not a routinely performed procedure in most cytopathology labs. Frozen section analysis is primarily a histologic technique employed during surgery to provide a rapid intraoperative diagnosis. While cell preparations can be made from frozen sections, the quality is typically inferior to conventionally processed cytology specimens, making cytologic interpretation more challenging. The rapid processing compromises cellular morphology and can introduce artifacts.
However, I am familiar with the principles and understand its potential role in urgent situations where an immediate diagnosis is crucial during a surgical procedure. For instance, if a surgical team needs to quickly determine whether a suspicious lesion is malignant or benign before proceeding with a surgical excision, a frozen section (histologic) would be prepared. The information generated would then guide intraoperative decision-making. While the cytopathology lab may not be directly involved, understanding the context and implications of frozen section results is important for correlating with post-surgical cytology or histology.
Q 17. Explain your understanding of the role of cytology in cancer diagnosis and staging.
Cytology plays a crucial role in both cancer diagnosis and staging. It offers a less invasive way to obtain cells for microscopic examination compared to biopsy. Its importance varies depending on the type of cancer.
- Diagnosis: Cytology is invaluable for detecting malignant cells in various body fluids (e.g., pleural effusions, cerebrospinal fluid) and through fine-needle aspiration (FNA) of suspicious masses. Early detection is key for improved cancer outcomes, and cytology aids in prompt diagnosis in many cases.
- Staging: Once a cancer is diagnosed, cytology can contribute to staging by determining the extent of the disease. For instance, cytologic examination of lymph node aspirates can help determine lymph node involvement (N-stage), a crucial factor in determining the overall stage and prognosis. Cytology can also assess the presence of malignant cells in other body sites, including effusion fluid samples.
Example: In lung cancer, cytologic examination of sputum or bronchoscopic washings can help establish an early diagnosis. Similarly, FNA of a suspicious lung nodule can provide a definitive diagnosis. Then, assessing the presence of malignant cells in pleural fluid obtained by thoracentesis can aid in staging the disease. This information is crucial for tailoring appropriate treatment strategies.
Q 18. What are the limitations of cytology in diagnosing certain conditions?
Cytology, while a powerful diagnostic tool, has limitations:
- Sampling error: Cytology examines a small sample of cells, and the sample may not be representative of the entire lesion. This can lead to false-negative results, where malignant cells are missed.
- Limited architectural information: Unlike histology, cytology provides limited information about the overall tissue architecture and arrangement of cells. This can make it difficult to differentiate between certain types of lesions, especially those with overlapping cytologic features.
- Difficulty in differentiating subtle cellular changes: Cytology might not always be able to distinguish between reactive and neoplastic changes, leading to diagnostic uncertainties.
- Cellular degeneration: Cell degradation during sample handling or processing can compromise the quality of the specimen and make interpretation more challenging.
Example: Distinguishing between a reactive lymph node and a low-grade lymphoma can sometimes be challenging using cytology alone. The subtle cellular features might overlap, requiring additional testing such as immunohistochemistry or even a biopsy for definitive diagnosis.
Q 19. Describe a challenging case you encountered and how you approached it.
One challenging case involved a fine-needle aspiration (FNA) of a thyroid nodule. The cytology showed a heterogeneous population of cells, with some features suggestive of malignancy (nuclear atypia, increased nuclear-to-cytoplasmic ratio) but also features of benign follicular cells. The initial interpretation was ‘indeterminate’, a frustrating diagnosis given the clinical need for a definitive diagnosis to guide treatment.
My approach involved a multi-step strategy:
- Careful re-evaluation of the slides: I meticulously reviewed the slides several times, focusing on subtle cytologic features that might indicate malignancy.
- Correlation with clinical and imaging data: The patient’s history, ultrasound findings (size, echogenicity of the nodule), and thyroid stimulating hormone (TSH) levels were reviewed carefully. The nodule’s size and ultrasound features suggested a higher risk of malignancy.
- Consultation with colleagues: I discussed the case with a colleague, a highly experienced cytopathologist, to benefit from an additional perspective.
- Recommendation for further testing: Based on the combined data, it was recommended that the patient undergo a thyroid biopsy for definitive diagnosis, which revealed follicular thyroid carcinoma. This highlighted the importance of an integrated approach and emphasized that cytology’s limitations in some cases necessitate additional testing.
Q 20. How do you maintain patient confidentiality in the context of cytology reporting?
Maintaining patient confidentiality in cytology reporting is paramount. I strictly adhere to HIPAA regulations and institutional policies regarding the handling of protected health information (PHI).
- Secure storage of specimens and reports: Cytology slides and reports are stored in secure, password-protected electronic systems, accessible only to authorized personnel.
- Use of anonymized identifiers: When presenting cases for educational or research purposes, patient identifiers are removed to ensure confidentiality.
- Restricted access to reports: Only authorized healthcare providers involved in the patient’s care have access to the cytology reports. The information is never disclosed to unauthorized individuals or entities.
- Secure communication: All communication concerning cytology results uses secure messaging channels to avoid potential breaches of confidentiality.
Any violation of patient confidentiality would be considered a serious breach of ethical guidelines and could have severe legal implications. Strict adherence to established protocols is essential.
Q 21. What are your strategies for staying updated on the latest advancements in cytology?
Staying updated in the rapidly evolving field of cytology requires a multi-pronged approach:
- Continuing medical education (CME): I actively participate in CME activities, including workshops, conferences, and online courses, to keep abreast of new diagnostic techniques, technologies, and research findings.
- Professional organizations: Membership in professional organizations, such as the American Society of Cytopathology (ASC), provides access to educational resources, publications, and networking opportunities.
- Peer-reviewed journals: I regularly read peer-reviewed journals specializing in cytology and pathology, staying informed about the latest research advancements and clinical guidelines.
- Collaboration with colleagues: Discussions with colleagues and participation in case reviews provide valuable learning experiences and insights.
- Participation in quality assurance programs: Active involvement in quality assurance programs ensures consistent adherence to best practices and helps identify areas for improvement.
By utilizing these strategies, I ensure that my knowledge and skills remain current and that I can provide the highest quality of care to my patients.
Q 22. Describe your proficiency with different types of microscopes used in cytology.
My proficiency with microscopes in cytology extends across various types, each optimized for specific applications. I’m highly experienced with brightfield microscopy, the cornerstone of cytology, which uses transmitted light to visualize stained specimens. This allows for detailed examination of cellular morphology, including nuclear-to-cytoplasmic ratio, chromatin pattern, and the presence of any cytoplasmic inclusions. I’m also proficient with fluorescence microscopy, crucial for immunocytochemistry (ICC) where fluorescently labeled antibodies bind to specific cellular components, enhancing diagnostic sensitivity. For example, using fluorescence microscopy with a specific antibody can highlight the presence of cytokeratins in epithelial cells, helping distinguish them from other cell types. Finally, I have experience with digital microscopy, which allows for image capture, storage, and analysis, crucial for telecytology and quality control. Digital imaging allows for easier sharing of images for consultation and for standardized measurement of cellular features.
Q 23. Explain your understanding of the legal and ethical considerations in cytology.
Legal and ethical considerations in cytology are paramount. Patient confidentiality, as dictated by HIPAA (Health Insurance Portability and Accountability Act) in the US, is strictly adhered to. All patient information is treated with the utmost privacy. Accurate and timely reporting is critical, as delayed or inaccurate results can have significant implications for patient care. Maintaining the chain of custody for samples is essential to ensure the integrity of the results and avoid legal challenges. Furthermore, I understand the implications of my interpretations, recognizing that my findings directly influence diagnostic and treatment decisions. Maintaining objectivity and adhering to established guidelines are critical in preventing bias. For example, I would never offer an opinion outside my area of expertise, instead always ensuring proper consultation with a pathologist when necessary.
Q 24. How do you manage workload effectively in a high-volume cytology laboratory?
Managing workload in a high-volume cytology lab requires a systematic approach. Prioritization is key; we use a combination of standardized workflows, automation where applicable (e.g., automated slide stainers, cell-block processors), and efficient case management software to streamline the process. I prioritize urgent cases, such as those with strong clinical suspicion of malignancy, ensuring timely turnaround times. Teamwork is crucial; we maintain open communication, delegating tasks appropriately and supporting each other during peak times. Regular quality control checks, including internal audits and proficiency testing, ensure consistent performance and accuracy despite the high volume.
Think of it like conducting an orchestra; each musician (cytotechnologist) has their role, but a conductor (lab manager) is essential to ensure harmony and efficiency.
Q 25. Describe your experience with data analysis and reporting in cytology.
Data analysis and reporting are integral to cytology. I regularly participate in compiling data on laboratory performance, including turnaround times, error rates, and diagnostic accuracy. This information helps in identifying areas for improvement and in tracking trends in disease prevalence and characteristics. I’m proficient in using Laboratory Information Systems (LIS) for data entry and retrieval. We utilize statistical analysis to track our accuracy rates, allowing for continuous quality improvement. For example, if we identify a specific diagnostic category with a higher-than-average error rate, we can implement targeted training or refine our diagnostic criteria for that area. Reporting is concise, clear, and tailored to the specific needs of clinicians – highlighting key findings and their clinical significance. The use of standardized reporting templates further improves communication and reduces ambiguity.
Q 26. How do you collaborate effectively with other healthcare professionals, such as pathologists and clinicians?
Effective collaboration with pathologists and clinicians is essential. Open and clear communication is paramount. I participate in multidisciplinary team meetings, presenting my findings and discussing cases with pathologists and clinicians. This collaborative approach leads to better diagnostic accuracy and patient care. For instance, if I observe atypical cells in a Pap smear, I’ll clearly communicate my observations to the pathologist, including detailed descriptions and illustrative images. The pathologist will then review the case and make the final diagnosis. Conversely, feedback from pathologists on our interpretations helps us refine our skills and improve accuracy. Maintaining a respectful and professional demeanor in all communications is key.
Q 27. What is your approach to continuous professional development in cytology?
Continuous professional development is a priority. I actively participate in continuing medical education (CME) courses, workshops, and conferences focused on advancements in cytology techniques and diagnostic criteria. I regularly review peer-reviewed journals and textbooks to stay updated on the latest research findings and guidelines. I also participate in internal training programs and mentorship opportunities within my department, sharing my knowledge with colleagues and learning from their expertise. This continuous learning ensures that I stay abreast of the evolving landscape of cytology and maintain high standards of diagnostic accuracy.
Q 28. How do you ensure accuracy and precision in your cytology interpretation?
Ensuring accuracy and precision is a cornerstone of my practice. I employ a meticulous and systematic approach to slide examination, following standardized protocols and using quality control measures throughout the process. This includes careful preparation and staining of specimens, systematic scanning of slides under the microscope, and meticulous documentation of findings. I utilize quality control measures, including internal proficiency testing and participation in external quality assurance programs to track our performance and identify areas needing improvement. Regular calibration and maintenance of equipment are also essential to ensure the reliability of our results. Double-checking findings and consulting with colleagues when uncertainties arise are integral parts of the process. Accuracy, above all, is never compromised. It’s like building a house – each step, from laying the foundation to the final touches, requires precision to create a strong and reliable structure.
Key Topics to Learn for Cytology Interpretation Interview
- Cellular Morphology: Mastering the identification and differentiation of normal and abnormal cells, including their size, shape, nuclear-to-cytoplasmic ratio, and chromatin patterns. Practical application: Accurate interpretation of Pap smears and fine-needle aspirations.
- Specimen Adequacy and Quality Control: Understanding the criteria for evaluating specimen adequacy and the importance of quality control procedures to ensure reliable results. Practical application: Identifying artifacts and limitations in cytology preparations and making informed judgments about diagnostic confidence.
- Inflammatory and Reactive Processes: Differentiating between reactive changes and true neoplastic processes. Practical application: Recognizing inflammatory conditions and distinguishing them from precancerous and cancerous lesions.
- Benign and Malignant Lesions: Distinguishing benign from malignant cells based on cytomorphological features. Practical application: Accurately identifying and classifying neoplastic lesions, including low-grade squamous intraepithelial lesions (LSIL), high-grade squamous intraepithelial lesions (HSIL), and invasive squamous cell carcinoma.
- Diagnostic Reporting: Understanding the principles of clear, concise, and accurate diagnostic reporting in cytology. Practical application: Communicating cytological findings effectively to clinicians, incorporating appropriate terminology and ensuring clarity to support patient care.
- Common Cytologic Diagnoses: Developing familiarity with the common diagnoses encountered in various body sites, such as the cervix, respiratory tract, and urinary tract. Practical application: Applying knowledge of specific cytological features to reach accurate diagnoses in different clinical contexts.
- Ancillary Techniques: Understanding the role and interpretation of ancillary techniques used in cytology, such as immunocytochemistry and molecular diagnostics. Practical application: Integrating ancillary test results to improve diagnostic accuracy and refine treatment strategies.
Next Steps
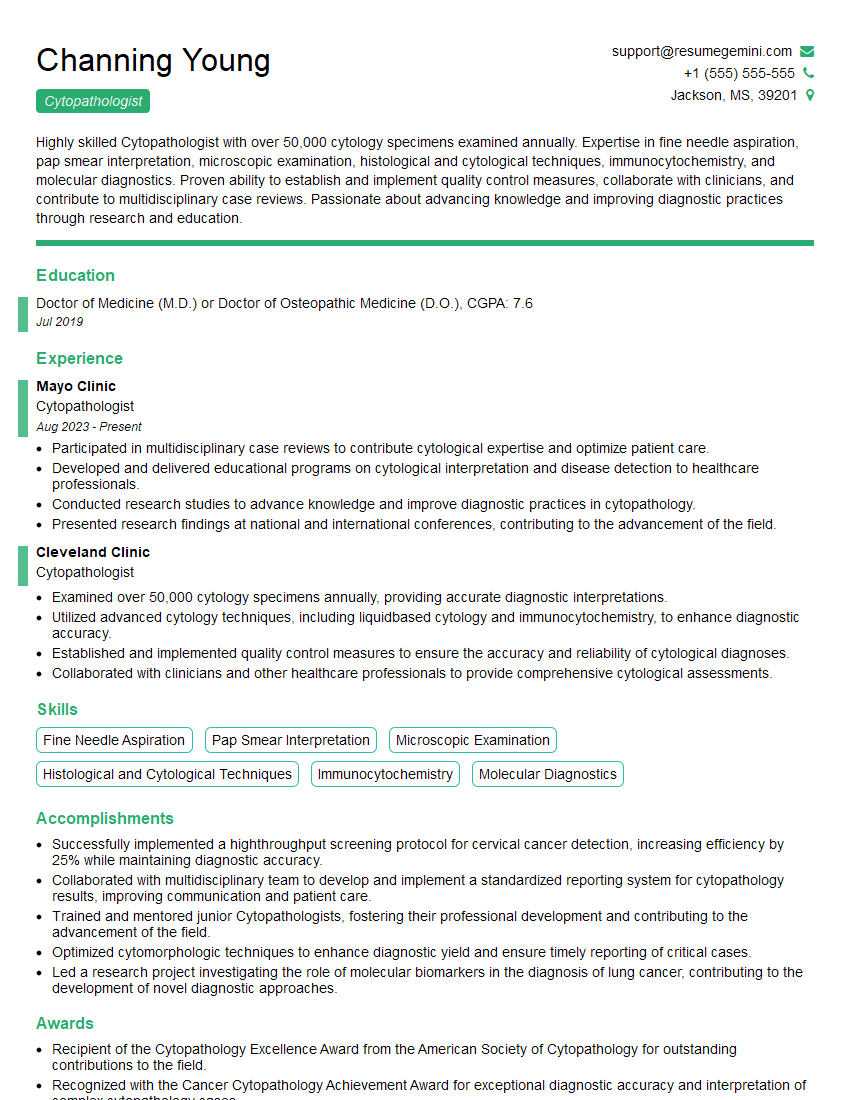
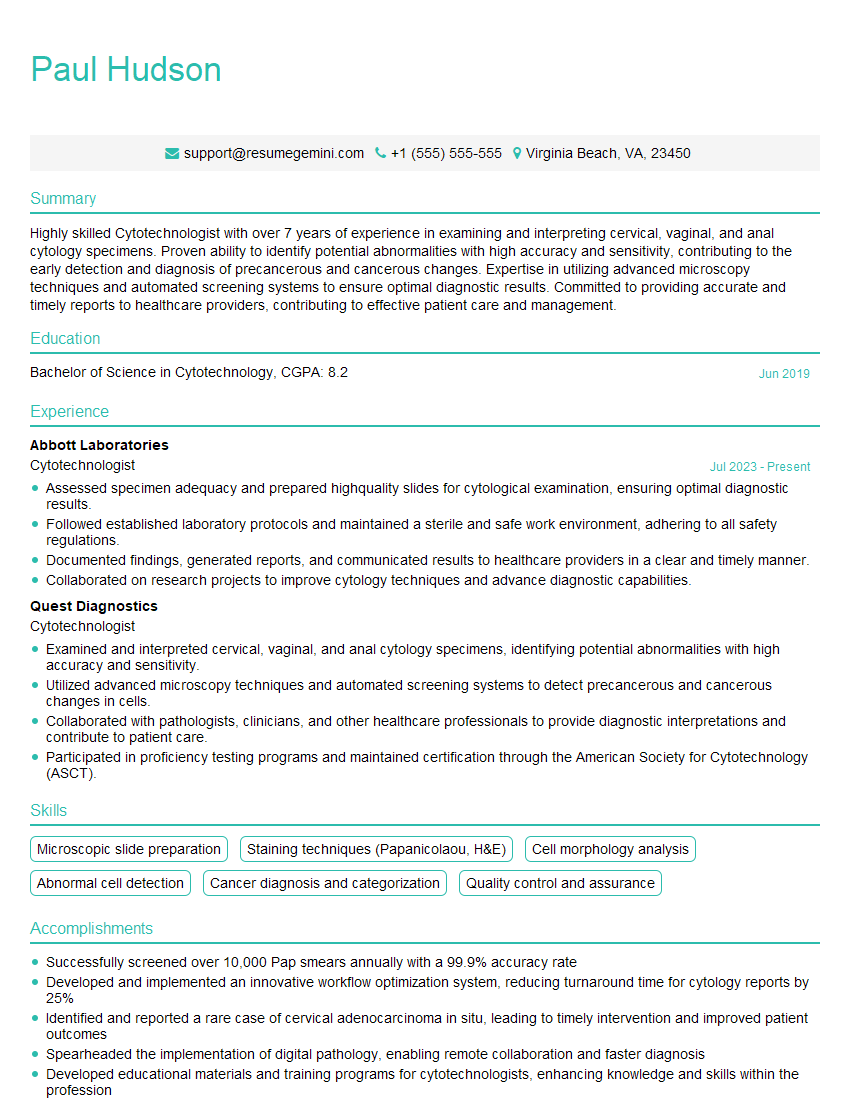
Mastering Cytology Interpretation is crucial for career advancement in the field of pathology and related healthcare disciplines. It opens doors to specialized roles with increased responsibility and earning potential. To maximize your job prospects, creating an ATS-friendly resume is essential. ResumeGemini is a trusted resource that can help you build a professional resume tailored to highlight your skills and experience in Cytology Interpretation. Examples of resumes specifically designed for Cytology Interpretation professionals are available to guide your resume creation. Invest the time in crafting a strong resume; it’s your first impression on potential employers.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.