Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Diagnosis and Management of Common Medical Conditions interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Diagnosis and Management of Common Medical Conditions Interview
Q 1. Describe your approach to diagnosing a patient presenting with chest pain.
Diagnosing chest pain requires a systematic approach prioritizing the identification of life-threatening conditions. It’s crucial to remember that chest pain can stem from a wide range of causes, from relatively benign musculoskeletal issues to life-threatening myocardial infarctions (heart attacks).
- Immediate Assessment: I begin by assessing the patient’s vital signs (heart rate, blood pressure, respiratory rate, oxygen saturation) and performing a focused physical examination, paying close attention to cardiac auscultation (listening to the heart sounds) and lung examination. The character of the pain (location, radiation, quality, onset, duration, associated symptoms) is crucial. Is it sharp, crushing, squeezing? Does it radiate to the arm, jaw, or back? Are there associated symptoms such as shortness of breath, sweating, nausea, or dizziness?
- Electrocardiogram (ECG): An ECG is essential to detect abnormalities in the heart’s electrical activity, such as ST-segment elevation, indicative of an acute myocardial infarction. This is usually done immediately.
- Cardiac Enzymes: Blood tests for cardiac enzymes (troponin) are crucial to detect cardiac muscle damage, a key indicator of a heart attack. This may not show immediately, requiring follow up measurements.
- Further Investigations: Depending on the initial assessment and ECG findings, further investigations may include chest X-ray to rule out pneumothorax (collapsed lung) or other lung conditions, echocardiogram (ultrasound of the heart) to assess cardiac function, or coronary angiography (to visualize coronary arteries and diagnose blockages).
- Differential Diagnosis: The differential diagnosis of chest pain is broad and includes conditions such as pericarditis, esophageal spasm, pulmonary embolism, aortic dissection, musculoskeletal pain, anxiety, and gastroesophageal reflux disease (GERD).
Consider this example: A patient presents with crushing chest pain radiating to the left arm, associated with shortness of breath and sweating. This strongly suggests a myocardial infarction. In contrast, a patient with sharp, localized chest pain worsened by deep breaths might be suggestive of pleurisy or pericarditis. Each scenario requires a different, targeted approach to diagnosis and management.
Q 2. How do you differentiate between viral and bacterial pneumonia?
Differentiating between viral and bacterial pneumonia relies on a combination of clinical findings, chest imaging, and sometimes laboratory tests. However, it’s important to note that differentiating the two is not always straightforward, and treatment is often empiric (based on clinical judgment) early on.
- Clinical Presentation: Viral pneumonia often presents with milder symptoms like gradual onset of cough, low-grade fever, myalgias (muscle aches), and fatigue. Bacterial pneumonia, on the other hand, typically presents with more severe symptoms, including high fever, productive cough (with sputum), chills, and more significant respiratory distress.
- Chest X-ray: This imaging study reveals the extent and pattern of consolidation (areas of fluid in the lungs) and helps to assess the severity of the disease. Bacterial pneumonia is more likely to show patchy or lobar consolidations whereas viral pneumonia can be more diffuse or interstitial. However, imaging alone isn’t definitive.
- Laboratory Tests: Complete blood count (CBC) can show elevated white blood cell count (leukocytosis) which is more pronounced in bacterial pneumonia, though it can also be seen in viral infections. Sputum culture (if obtainable) can identify the causative bacteria in bacterial pneumonia. However, viral tests are usually less helpful in acute management.
- Procalcitonin: This blood test can help differentiate between bacterial and viral infections; elevated levels suggest a higher likelihood of bacterial infection.
For instance, a patient with a high fever, productive cough with rust-colored sputum, and a lobar consolidation on chest X-ray is more suggestive of bacterial pneumonia. Conversely, a patient with a gradual onset of cough, mild fever, and diffuse interstitial changes on chest X-ray is more likely to have viral pneumonia. However, overlapping symptoms can make diagnosis challenging, hence empirical treatment is often a primary strategy.
Q 3. Explain your management strategy for a patient with uncontrolled hypertension.
Managing uncontrolled hypertension involves a multifaceted approach encompassing lifestyle modifications, medication, and regular monitoring. The goal is to reduce cardiovascular risk by achieving and maintaining target blood pressure levels.
- Lifestyle Modifications: This is the cornerstone of hypertension management. I advise patients on adopting a DASH (Dietary Approaches to Stop Hypertension) diet, rich in fruits, vegetables, and low-fat dairy products, while reducing sodium intake. Regular physical activity (at least 150 minutes of moderate-intensity aerobic exercise per week), weight loss if obese, and limiting alcohol consumption are also vital.
- Pharmacological Management: If lifestyle modifications fail to achieve target blood pressure, medication is necessary. The choice of medication depends on factors such as the patient’s age, other medical conditions, and individual response. Common classes include:
- Thiazide diuretics: First-line treatment for most patients.
- ACE inhibitors or ARBs: Particularly beneficial for patients with diabetes or chronic kidney disease.
- Beta-blockers: Often used in patients with coronary artery disease or post-myocardial infarction.
- Calcium channel blockers: Useful in patients with concomitant angina or migraines.
- Monitoring: Regular monitoring of blood pressure, at home and in the clinic, is essential to assess treatment effectiveness and make adjustments as needed. Monitoring for potential side effects of medications is also crucial.
For example, a patient with uncontrolled hypertension despite lifestyle changes might be started on a thiazide diuretic. If blood pressure remains uncontrolled, an ACE inhibitor or ARB might be added. Regular follow-up appointments allow for titration of medications and adjustments based on individual patient responses and potential side effects.
Q 4. What are the key diagnostic criteria for type 2 diabetes mellitus?
The diagnosis of type 2 diabetes mellitus requires the fulfillment of at least one of the following criteria on two separate occasions:
- Fasting Plasma Glucose (FPG): A fasting plasma glucose level of ≥126 mg/dL (7.0 mmol/L).
- Oral Glucose Tolerance Test (OGTT): A 2-hour plasma glucose level ≥200 mg/dL (11.1 mmol/L) during an OGTT.
- HbA1c: A HbA1c level ≥6.5% (48 mmol/mol).
It’s crucial to note that symptoms such as polyuria (increased urination), polydipsia (increased thirst), and polyphagia (increased hunger) might be present but are not mandatory for diagnosis. Additionally, random plasma glucose levels ≥200 mg/dL (11.1 mmol/L) in the presence of classic symptoms are also diagnostic. The tests should be performed correctly to ensure accurate results. Any abnormalities in initial screenings should be followed up with repeat testing.
For example, a patient presenting with symptoms and a fasting plasma glucose of 130 mg/dL on two separate occasions would receive a diagnosis of type 2 diabetes mellitus. Similarly, an HbA1c of 7% would confirm a diagnosis.
Q 5. Outline your approach to managing a patient with acute asthma exacerbation.
Managing an acute asthma exacerbation requires prompt and effective intervention to alleviate symptoms and prevent life-threatening complications. This is a time-sensitive situation.
- Assessment: The initial assessment focuses on the severity of the exacerbation using tools like the Asthma Severity Scale, which assesses respiratory rate, pulse, oxygen saturation, and level of respiratory distress. Vital signs are critical to gauge the emergency nature of the situation.
- Oxygen Therapy: Supplemental oxygen is administered to maintain oxygen saturation above 90%. This is vital to avoid hypoxia (low blood oxygen).
- Bronchodilators: Nebulized short-acting beta-agonists (SABAs) like albuterol are usually administered initially to relieve bronchospasm. Ipratropium bromide can be added for further bronchodilation.
- Systemic Corticosteroids: Oral or intravenous corticosteroids (like prednisone or methylprednisolone) are administered to reduce airway inflammation.
- Monitoring: Continuous monitoring of respiratory rate, pulse oximetry, and clinical status are essential during treatment and after discharge. Additional considerations such as inhaled corticosteroids and long-term control medications are addressed after stabilizing the patient.
- Hospital Admission: Hospital admission is warranted for patients with severe exacerbations who do not respond to initial treatment or exhibit signs of respiratory failure.
For example, a patient with severe wheezing, difficulty breathing, and low oxygen saturation will require immediate administration of oxygen, nebulized albuterol, and systemic corticosteroids. If there is no improvement, or if they have severe respiratory distress, urgent hospitalization might be required for potentially life-saving measures.
Q 6. How would you assess and manage a patient with suspected appendicitis?
Suspected appendicitis requires a careful clinical evaluation and the use of imaging to confirm the diagnosis. The classic presentation is pain starting periumbilically (around the navel) that migrates to the right lower quadrant (RLQ) of the abdomen, associated with nausea, vomiting, and fever. However, presentations can be atypical.
- History and Physical Examination: I obtain a thorough history, focusing on the onset, location, and character of abdominal pain. The physical exam includes palpation (feeling) of the abdomen, looking for tenderness in the RLQ, rebound tenderness (pain when pressure is released), and guarding (muscle spasm). A psoas sign (pain with hip flexion) or obturator sign (pain with hip internal rotation) might be suggestive of appendicitis.
- Laboratory Tests: A complete blood count (CBC) may show leukocytosis (increased white blood cell count), indicating inflammation. This test can give clues but is not definitive.
- Imaging: Ultrasound or CT scan of the abdomen can visualize the appendix and help to confirm the diagnosis of appendicitis. Ultrasound is often the initial imaging choice due to its non-invasiveness and lack of radiation.
Atypical presentations can make diagnosis difficult. For example, an elderly patient may present with vague abdominal pain and low-grade fever without the classic signs. In these cases, imaging is particularly important. If appendicitis is confirmed, surgical appendectomy (removal of the appendix) is usually the treatment of choice. Delaying surgery can lead to complications such as perforation and peritonitis (infection of the abdominal cavity).
Q 7. Describe your approach to a patient presenting with symptoms of a stroke.
Suspected stroke requires immediate attention as prompt treatment can significantly improve outcomes. The key is to quickly recognize the signs and initiate appropriate management.
- Rapid Neurological Assessment: This is the first step, using the FAST (Face drooping, Arm weakness, Speech difficulty, Time to call emergency services) test to quickly identify potential stroke symptoms. A more detailed neurological examination follows.
- Brain Imaging: Non-contrast CT scan is the initial imaging test to rule out intracranial hemorrhage (bleeding in the brain), which contraindicates some thrombolytic therapies. If hemorrhage is excluded, MRI or CT angiography may be needed for further assessment.
- Thrombolytic Therapy: For ischemic stroke (caused by a blood clot), intravenous tissue plasminogen activator (tPA) is the gold standard treatment if given within a specific time window (usually within 3-4.5 hours of symptom onset). The decision to administer tPA is based on several factors including the patient’s clinical presentation, imaging findings, and time since symptom onset.
- Supportive Care: Supportive care includes managing blood pressure, maintaining airway patency, preventing complications such as pneumonia, and providing rehabilitation.
For instance, a patient presenting with sudden onset of right-sided weakness and slurred speech would raise high suspicion for stroke. Immediate brain imaging is crucial to determine the type of stroke. If it’s an ischemic stroke and the time window permits, tPA is administered. Even if tPA isn’t an option, aggressive supportive care to prevent complications and aid neurological recovery is vital.
Q 8. What are the common causes of chronic kidney disease, and how do you manage them?
Chronic kidney disease (CKD) is a gradual loss of kidney function over time. Several factors contribute to its development.
- Diabetes: High blood sugar damages blood vessels in the kidneys, leading to reduced filtration.
- High blood pressure (hypertension): Constantly high blood pressure strains the kidneys, impairing their ability to function effectively.
- Glomerulonephritis: Inflammation of the glomeruli (filtering units in the kidneys), often caused by autoimmune diseases or infections.
- Polycystic kidney disease (PKD): A genetic disorder causing cysts to form in the kidneys, eventually impairing function.
- Obstructions in the urinary tract: Kidney stones or enlarged prostate can block urine flow, damaging the kidneys.
Managing CKD involves a multi-pronged approach focusing on slowing disease progression and managing symptoms. This includes:
- Blood pressure control: Medications like ACE inhibitors, ARBs, and beta-blockers are crucial.
- Blood sugar control (if diabetic): Tight blood sugar management through diet, exercise, and medication (insulin or oral hypoglycemics).
- Dietary modifications: Limiting protein, phosphorus, and potassium intake to reduce the burden on the kidneys.
- Medication management: Treating anemia with erythropoietin, managing electrolyte imbalances, and possibly using phosphate binders.
- Dialysis or kidney transplant: In advanced CKD stages, these life-sustaining treatments become necessary.
For example, a patient with diabetes and hypertension needs strict blood sugar and blood pressure control, along with dietary changes to minimize kidney damage. Regular monitoring of kidney function through blood tests (eGFR, creatinine) and urine tests is essential.
Q 9. How would you manage a patient with a deep vein thrombosis (DVT)?
Deep vein thrombosis (DVT) is a blood clot that forms in a deep vein, usually in the leg. It’s a serious condition because the clot can travel to the lungs (pulmonary embolism), potentially fatal. Management focuses on preventing further clot formation, breaking down existing clots, and preventing future occurrences.
- Anticoagulation: This is the cornerstone of DVT treatment. Heparin (initially, often given intravenously) and warfarin (or newer oral anticoagulants like rivaroxaban or apixaban) are used to prevent further clot formation. The choice of anticoagulant depends on various factors such as patient characteristics and the severity of the DVT.
- Pain and swelling management: Elevation of the affected leg, compression stockings, and pain relievers can alleviate symptoms.
- Thrombolytic therapy: In severe cases, clot-busting drugs (thrombolytics) might be used to dissolve the clot, but they carry a risk of bleeding.
- Inferior vena cava (IVC) filter: In patients at high risk for pulmonary embolism, an IVC filter can be placed to prevent clots from reaching the lungs.
For instance, a young patient with a first-time DVT might be treated with a short course of heparin followed by several months of oral anticoagulation. Regular blood tests are needed to monitor the effectiveness of anticoagulation and adjust the medication dose as needed.
Q 10. Explain your strategy for managing a patient with congestive heart failure.
Congestive heart failure (CHF) is a condition where the heart cannot pump enough blood to meet the body’s needs. Management aims to improve heart function, reduce fluid overload, and alleviate symptoms.
- Lifestyle modifications: Dietary sodium restriction, weight reduction (if overweight or obese), regular exercise (as tolerated), and smoking cessation.
- Medications: Several classes of drugs are used, including:
- Diuretics: To remove excess fluid.
- ACE inhibitors or ARBs: To reduce blood pressure and improve heart function.
- Beta-blockers: To slow the heart rate and reduce workload.
- Digoxin: To improve heart contractility.
- Device therapy: Implantable cardioverter-defibrillators (ICDs) or cardiac resynchronization therapy (CRT) devices may be considered in select patients.
- Fluid management: Careful monitoring of fluid intake and output, and prompt treatment of fluid overload.
Consider a patient with shortness of breath and edema. Initial management would involve diuretics to reduce fluid buildup, along with ACE inhibitors or ARBs to improve cardiac output. Regular monitoring of weight, blood pressure, and heart function is essential. Further interventions may be needed depending on the patient’s response.
Q 11. How do you differentiate between different types of headaches?
Headaches are broadly classified into primary and secondary headaches. Primary headaches, such as migraines and tension-type headaches, are not caused by an underlying medical condition, while secondary headaches result from other problems (e.g., infections, injuries). Differentiating them relies on a detailed history and physical exam.
- Migraine: Typically unilateral, throbbing pain, often accompanied by nausea, vomiting, and sensitivity to light and sound (photophobia and phonophobia). May have an aura (visual or sensory disturbances).
- Tension-type headache: Bilateral, pressing or tightening pain, usually mild or moderate intensity, without nausea or vomiting.
- Cluster headache: Severe, unilateral pain around the eye, often accompanied by tearing, nasal congestion, and Horner’s syndrome.
- Secondary headache: Often associated with other symptoms, such as fever, neck stiffness (meningitis), focal neurological signs (stroke or brain tumor), or recent head trauma.
For instance, a patient with a severe, unilateral headache associated with nausea and vomiting and photophobia is more likely to have a migraine. However, a headache with fever, neck stiffness, and altered mental status warrants immediate investigation for meningitis.
Q 12. What are the risk factors for coronary artery disease, and how do you manage them?
Coronary artery disease (CAD) is the narrowing or blockage of the coronary arteries, which supply blood to the heart. Risk factors are modifiable or non-modifiable.
- Non-modifiable: Age, sex (men are at higher risk), family history of CAD.
- Modifiable: High blood pressure, high cholesterol, smoking, diabetes, obesity, physical inactivity, unhealthy diet.
Management aims to reduce risk factors and prevent further progression.
- Lifestyle changes: Diet rich in fruits, vegetables, and whole grains; regular physical activity; smoking cessation; weight management.
- Medications:
- Statins: To lower cholesterol.
- Antihypertensives: To control blood pressure.
- Antiplatelet agents (aspirin, clopidogrel): To prevent blood clots.
- Diabetes medications: To control blood sugar levels.
- Revascularization procedures: Angioplasty (with or without stenting) or coronary artery bypass grafting (CABG) may be necessary if the arteries are severely blocked.
For example, a patient with high cholesterol, hypertension, and a family history of CAD would benefit from statins to lower cholesterol, antihypertensives to control blood pressure, lifestyle modification, and potentially aspirin to prevent blood clots.
Q 13. How would you assess and manage a patient with suspected meningitis?
Suspected meningitis, an infection of the membranes surrounding the brain and spinal cord, is a medical emergency requiring prompt evaluation and treatment. Assessment involves a thorough history, physical examination, and laboratory investigations.
- History: Fever, headache, neck stiffness (meningismus), altered mental status, rash (e.g., petechiae in meningococcal meningitis).
- Physical examination: Assessing for fever, neck stiffness (resistance to passive flexion of the neck), mental status changes, and rash.
- Laboratory investigations: Lumbar puncture (spinal tap) to obtain cerebrospinal fluid (CSF) for analysis (cell count, glucose, protein, culture for bacteria or viruses), blood cultures, and possibly imaging studies (CT scan or MRI).
Management involves immediate initiation of empiric antibiotic therapy (broad-spectrum antibiotics) based on clinical suspicion, before lab results are available. Further management depends on the causative organism identified through CSF analysis. Supportive measures include fluid resuscitation, antipyretics for fever, and seizure prophylaxis if necessary.
A patient presenting with fever, severe headache, and neck stiffness requires immediate hospital admission, initiation of antibiotics (e.g., ceftriaxone and vancomycin), and prompt lumbar puncture. Early diagnosis and treatment are crucial to prevent serious complications like brain damage or death.
Q 14. Describe the diagnostic criteria and management of depression.
Depression is a mood disorder characterized by persistent sadness, loss of interest, and other symptoms. Diagnostic criteria are based on the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
- Symptoms: Depressed mood, loss of interest or pleasure, changes in appetite or weight, sleep disturbances, fatigue, feelings of worthlessness or guilt, difficulty concentrating, recurrent thoughts of death or suicide.
- Duration: Symptoms must be present for at least two weeks.
- Severity: Symptoms must cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
Management involves a combination of approaches:
- Psychotherapy: Cognitive behavioral therapy (CBT) and other forms of psychotherapy help individuals identify and change negative thought patterns and behaviors.
- Medication: Antidepressants (selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), etc.) are often used to alleviate symptoms. The choice of antidepressant depends on the patient’s individual needs and preferences.
- Lifestyle changes: Regular exercise, adequate sleep, healthy diet, and stress management techniques can significantly improve symptoms.
- Hospitalization: May be necessary in cases of severe depression with suicidal ideation or risk of self-harm.
For instance, a patient with persistent sadness, sleep disturbances, and significant weight loss might receive a diagnosis of depression and be offered a course of SSRIs, along with CBT. Regular follow-up appointments are crucial to monitor the patient’s response to treatment and make necessary adjustments.
Q 15. Outline your approach to managing a patient with uncontrolled diabetes with diabetic ketoacidosis.
Managing a patient with diabetic ketoacidosis (DKA), a life-threatening complication of uncontrolled diabetes, requires immediate and aggressive intervention. DKA occurs when the body starts breaking down fat for energy due to a severe lack of insulin, resulting in a buildup of ketones in the blood, causing acidosis (high acidity).
My approach involves the following steps:
- Immediate stabilization: This includes assessing airway, breathing, and circulation (ABCs), initiating intravenous (IV) fluids (usually normal saline) to correct dehydration, and monitoring vital signs closely. Blood glucose and electrolyte levels need immediate assessment.
- Insulin administration: A continuous IV insulin infusion is typically initiated to lower blood glucose levels gradually. The goal is to decrease glucose levels by 50-75 mg/dL per hour, preventing rapid shifts which can be dangerous.
- Electrolyte correction: Potassium levels are crucial. While initially low, they can rapidly shift, potentially leading to dangerous arrhythmias. Potassium replacement is often needed, but only after adequate urine output is established.
- Fluid resuscitation: Intravenous fluid replacement is paramount to correct dehydration, often using normal saline initially, followed by adjustments based on ongoing assessment of fluid status and electrolyte levels.
- Ongoing monitoring: Continuous monitoring of blood glucose, electrolytes (potassium, sodium, chloride, bicarbonate), and vital signs is critical. Hourly blood gas analysis is frequently employed.
- Underlying cause identification: Identifying and treating the underlying cause of DKA is essential, for example, infection, acute illness, or missed insulin doses.
- Transition to subcutaneous insulin: Once the patient’s condition stabilizes, the IV insulin infusion is typically transitioned to subcutaneous insulin injections, with appropriate dosages adjusted based on individual needs.
For example, I recently treated a 60-year-old patient who presented with severe dehydration, rapid breathing, and altered mental status. Her blood glucose was extremely elevated, and ketone levels were significantly high, confirming DKA. Following the protocol outlined above, we were able to stabilize her condition within 24 hours and successfully transition her to subcutaneous insulin therapy.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the common causes of anemia, and how do you investigate and manage them?
Anemia is a condition characterized by a deficiency of red blood cells or hemoglobin in the blood, resulting in reduced oxygen-carrying capacity. Several causes exist, broadly categorized into:
- Nutritional deficiencies: Iron deficiency anemia is the most common, often due to insufficient dietary intake, malabsorption, or chronic blood loss. Vitamin B12 and folate deficiencies can also cause anemia.
- Bone marrow disorders: Conditions like leukemia or aplastic anemia can impair the bone marrow’s ability to produce red blood cells.
- Chronic diseases: Chronic kidney disease, inflammatory diseases, and cancer can cause anemia of chronic disease.
- Hemolytic anemias: These are conditions in which red blood cells are destroyed prematurely, such as sickle cell anemia or autoimmune hemolytic anemia.
- Blood loss: Acute or chronic blood loss, from sources like gastrointestinal bleeding or heavy menstrual bleeding, can lead to anemia.
Investigation includes a complete blood count (CBC) to assess hemoglobin, hematocrit, red blood cell indices, and white blood cell count. Further testing depends on the initial findings. For example, iron studies, vitamin B12 and folate levels, bone marrow biopsy, and stool tests may be necessary.
Management is tailored to the underlying cause. Iron deficiency anemia is typically treated with oral iron supplements. Vitamin B12 or folate deficiencies require appropriate supplementation. Treatment of underlying conditions such as infections or chronic diseases is crucial. Blood transfusions may be necessary in severe cases or during acute blood loss. In hemolytic anemias, specific treatments like corticosteroids or splenectomy might be needed.
Q 17. How would you assess and manage a patient with suspected sepsis?
Sepsis is a life-threatening condition arising from the body’s overwhelming response to an infection. It’s a medical emergency requiring prompt diagnosis and treatment.
Assessment involves a comprehensive evaluation focusing on:
- Symptoms: Fever, chills, rapid heart rate, rapid breathing, low blood pressure, confusion, and altered mental status are common signs.
- Vital signs: Close monitoring of temperature, heart rate, respiratory rate, blood pressure, and oxygen saturation is crucial.
- Laboratory tests: Complete blood count (CBC), blood cultures, inflammatory markers (CRP, procalcitonin), lactate levels, and urine analysis help confirm the presence of infection and assess organ function.
- Source identification: Identifying the source of infection is crucial. This involves a thorough physical examination and potential imaging studies (chest X-ray, CT scan, ultrasound).
Management consists of:
- Rapid administration of intravenous fluids: This is to maintain adequate blood pressure and organ perfusion.
- Broad-spectrum antibiotics: These are initiated promptly based on clinical suspicion, even before definitive culture results are available. Antibiotic selection is often guided by local antibiograms and potential sources of infection.
- Supportive care: This includes oxygen therapy, ventilator support if necessary, and management of organ dysfunction. This also includes close monitoring for organ failure, such as acute kidney injury or disseminated intravascular coagulation.
- Source control: Addressing the source of infection is critical, which may involve surgical drainage of an abscess, removal of an infected catheter, or other interventions.
- Monitoring for complications: Sepsis can lead to various complications, including septic shock, acute respiratory distress syndrome (ARDS), and multiple organ dysfunction syndrome (MODS). Continuous monitoring and aggressive management of these complications are essential.
Consider a case of an elderly patient admitted with altered mental status, fever, and hypotension. Blood cultures revealed Gram-negative bacteria. Prompt fluid resuscitation, broad-spectrum antibiotics, and source control (in this case, treatment of pneumonia) were initiated, leading to a successful outcome.
Q 18. Explain the management of a patient with a urinary tract infection.
A urinary tract infection (UTI) is an infection of the urinary system, most commonly affecting the bladder (cystitis) or the kidneys (pyelonephritis).
Management generally involves:
- Diagnosis: This is typically based on symptoms (dysuria, frequency, urgency, suprapubic pain), urinalysis (showing leukocytes, nitrites, bacteria), and urine culture (to identify the causative organism and its antibiotic susceptibility).
- Antibiotic therapy: This is the cornerstone of treatment. The choice of antibiotic depends on the identified organism and its susceptibility. For uncomplicated UTIs, a short course of antibiotics (e.g., nitrofurantoin, trimethoprim-sulfamethoxazole) is usually sufficient. Complicated UTIs (e.g., pyelonephritis, UTIs in pregnant women, immunocompromised patients) may require longer courses of antibiotics and intravenous administration.
- Symptom relief: Over-the-counter pain relievers like acetaminophen or ibuprofen can help alleviate pain and fever. Increased fluid intake is encouraged to help flush out bacteria.
- Follow-up: A follow-up visit is usually recommended to ensure the infection has resolved. Recurrent UTIs may require further investigation for underlying causes, such as anatomical abnormalities or kidney stones.
For example, a young woman presents with frequent, painful urination and lower abdominal pain. Her urinalysis reveals leukocytes and bacteria. She is prescribed a 3-day course of trimethoprim-sulfamethoxazole, and her symptoms resolve within a few days. Follow-up is not necessary in this uncomplicated case.
Q 19. Describe your approach to a patient presenting with syncope.
Syncope, or fainting, is a sudden, transient loss of consciousness due to decreased blood flow to the brain. Assessing a patient experiencing syncope requires a systematic approach:
- Detailed history: A thorough history is crucial, including the circumstances surrounding the event (e.g., posture, exertion, prodromal symptoms), associated symptoms (e.g., nausea, palpitations, chest pain), and past medical history (e.g., cardiac conditions, neurological disorders).
- Physical examination: A comprehensive physical exam, including cardiovascular, neurological, and orthostatic assessments, helps to identify potential causes.
- Electrocardiogram (ECG): An ECG is essential to evaluate for cardiac arrhythmias, which are a common cause of syncope.
- Other investigations: Further investigations, such as echocardiography, tilt-table testing, or neurological studies, may be needed depending on the clinical suspicion.
Management depends on the identified cause:
- Cardiac causes: Management may involve medications to control arrhythmias, pacemaker implantation, or surgical intervention.
- Neurological causes: Treatment depends on the specific neurological condition.
- Vasovagal syncope: This common type of syncope often requires lifestyle modifications, such as increased fluid intake and avoidance of triggers.
- Orthostatic hypotension: Management includes lifestyle adjustments, medications (e.g., fludrocortisone), or compression stockings.
For example, a young adult presents with recurrent syncope during periods of prolonged standing. His physical exam is unremarkable, but tilt-table testing reveals vasovagal syncope. He is advised on lifestyle modifications, and his symptoms improve significantly.
Q 20. How do you differentiate between different types of skin rashes?
Differentiating between various skin rashes requires careful observation and consideration of several factors:
- Morphology: Describing the rash’s appearance (e.g., macules, papules, vesicles, pustules, plaques) is crucial. Macules are flat, colored spots; papules are raised, solid lesions; vesicles are small, fluid-filled blisters; pustules are pus-filled blisters; plaques are raised, flat-topped lesions.
- Distribution: The location and pattern of the rash (e.g., generalized, localized, linear, annular) provide important clues.
- Associated symptoms: Pruritus (itching), pain, fever, or other systemic symptoms are essential to note.
- Patient history: Information about recent exposures (e.g., plants, allergens), medications, travel history, and pre-existing conditions can aid diagnosis.
For example, a widespread, intensely itchy rash with small, fluid-filled blisters might suggest a viral exanthem, such as chickenpox. A localized, scaly, red patch with well-defined borders might suggest ringworm (tinea corporis). A butterfly-shaped rash across the face might suggest systemic lupus erythematosus. A rash with a target-like appearance might suggest erythema multiforme.
Definitive diagnosis often requires a thorough clinical evaluation and sometimes skin biopsy or other investigations.
Q 21. What are the risk factors for osteoporosis, and how do you manage it?
Osteoporosis is a systemic skeletal disease characterized by low bone mass and microarchitectural deterioration of bone tissue, leading to increased bone fragility and a consequent increase in fracture risk.
Risk factors include:
- Age: Bone density naturally decreases with age, particularly in postmenopausal women.
- Sex: Women are at significantly higher risk, especially after menopause.
- Family history: A family history of osteoporosis increases risk.
- Ethnicity: Caucasians and Asians are at higher risk than African Americans.
- Low body weight: Individuals with low body weight have lower bone mass.
- Lifestyle factors: Lack of physical activity, smoking, excessive alcohol consumption, and inadequate calcium and vitamin D intake contribute to osteoporosis.
- Medical conditions: Certain medical conditions, such as rheumatoid arthritis, hyperthyroidism, and Cushing’s syndrome, increase the risk of osteoporosis.
- Medications: Some medications, like corticosteroids, can increase bone loss.
Management includes:
- Lifestyle modifications: Weight-bearing exercises, adequate calcium and vitamin D intake, smoking cessation, and moderate alcohol consumption.
- Medications: Bisphosphonates, denosumab, teriparatide, and other medications are used to increase bone density and reduce fracture risk.
- Fracture risk assessment: FRAX score or similar tools are used to assess an individual’s 10-year risk of fracture, guiding treatment decisions.
- Regular bone density testing: Dual-energy X-ray absorptiometry (DEXA) scans are used to monitor bone density changes.
For example, a postmenopausal woman with a family history of osteoporosis presents with a recent vertebral fracture. Her DEXA scan reveals osteoporosis. She is started on bisphosphonates, advised on lifestyle modifications, and monitored regularly to assess treatment effectiveness.
Q 22. How do you assess and manage a patient with suspected pulmonary embolism?
Suspected pulmonary embolism (PE) is a serious condition requiring immediate attention. Assessment involves a thorough history focusing on risk factors (e.g., recent surgery, prolonged immobility, cancer, pregnancy), symptoms (e.g., sudden shortness of breath, chest pain, cough, tachycardia), and a physical exam. Crucially, we use clinical prediction rules like the Wells score or Geneva score to stratify risk. Imaging is essential; a CT pulmonary angiography (CTPA) is the gold standard for diagnosis, providing a fast and accurate visualization of the pulmonary arteries. However, if a CTPA is contraindicated (e.g., severe renal impairment), a ventilation-perfusion (V/Q) scan might be used, but it’s less specific. Management depends on risk stratification and diagnosis. Low-risk patients might be managed with serial monitoring and anticoagulation initiation based on clinical judgment. High-risk patients often require immediate anticoagulation with heparin (unfractionated or low molecular weight), followed by long-term anticoagulation with warfarin, direct thrombin inhibitors (e.g., dabigatran), or factor Xa inhibitors (e.g., rivaroxaban). Thrombolytic therapy is considered for patients with massive PE and hemodynamic instability, but carries significant bleeding risks.
For example, a young patient post-surgery presenting with sudden shortness of breath and pleuritic chest pain would trigger immediate investigation with a CTPA. A positive finding would lead to immediate anticoagulation. In contrast, an older patient with risk factors but less pronounced symptoms might benefit from risk stratification scoring before definitive imaging and treatment.
Q 23. Explain your strategy for managing a patient with hyperthyroidism.
Managing hyperthyroidism involves addressing the underlying cause and controlling the hypermetabolic state. The initial assessment includes a thorough history, physical examination (assessing for tachycardia, tremor, goiter), and laboratory tests (TSH, free T4, free T3). Treatment aims to reduce thyroid hormone levels and alleviate symptoms. Antithyroid drugs like methimazole or propylthiouracil are first-line treatment for most patients, blocking thyroid hormone synthesis. Beta-blockers can effectively manage symptoms like tachycardia and tremor, offering immediate relief. In cases of severe thyrotoxicosis (thyroid storm), intravenous fluids, beta-blockers, and corticosteroids are crucial to stabilize the patient. Radioactive iodine therapy is a highly effective option for long-term control, destroying thyroid tissue gradually. Surgery (thyroidectomy) may be necessary for very large goiters, severe hyperthyroidism not responding to other treatments, or suspicion of thyroid cancer.
Imagine a patient with palpitations, weight loss, and nervousness. Elevated free T4 and low TSH confirm hyperthyroidism. We’d initiate methimazole to control thyroid hormone production, add a beta-blocker for symptom relief, and monitor thyroid function regularly. After achieving euthyroidism (normal thyroid hormone levels), we’d discuss long-term management options like radioactive iodine therapy.
Q 24. How would you approach a patient with new onset seizures?
New-onset seizures are a medical emergency requiring immediate attention. Initial management focuses on securing the airway, protecting the patient from injury, and monitoring vital signs. We need to establish the cause of the seizure; a thorough history (including details of the seizure, medications, medical history, and family history) and a neurological examination are crucial. Blood work should include basic metabolic panel, complete blood count, and toxicology screen to rule out metabolic derangements, infections, or drug toxicity. Brain imaging (CT scan or MRI) is crucial to detect structural abnormalities. An EEG can help determine the type of seizure and its origin. Treatment depends on the cause and type of seizure. First-line treatment for many cases is anti-epileptic medication (AED), with choices like levetiracetam, lamotrigine, or valproate depending on the seizure type and patient profile. If the seizure is prolonged (status epilepticus), intravenous benzodiazepines like lorazepam or diazepam are life-saving interventions. Underlying conditions causing the seizures must be treated aggressively.
For instance, a patient experiencing a prolonged seizure would require immediate intravenous benzodiazepines followed by intensive care. A patient with a first-time seizure and normal initial investigations might warrant close monitoring and AED initiation after appropriate imaging.
Q 25. What are the common causes of chronic obstructive pulmonary disease (COPD), and how do you manage them?
Chronic obstructive pulmonary disease (COPD) is primarily caused by long-term exposure to noxious particles or gases, most commonly cigarette smoke. Other risk factors include genetic predisposition (alpha-1 antitrypsin deficiency), occupational exposure, and air pollution. COPD encompasses chronic bronchitis (inflammation of the airways) and emphysema (destruction of alveolar tissue). Management focuses on symptom relief, disease progression slowing, and improving quality of life. This includes smoking cessation, which remains the single most important intervention. Pharmacological treatment consists of bronchodilators (beta-agonists and anticholinergics), often used in combination. Inhaled corticosteroids reduce inflammation and are added for patients with frequent exacerbations or significant symptoms. Long-term oxygen therapy is vital for patients with hypoxemia, improving exercise capacity and survival. Pulmonary rehabilitation is a crucial component, incorporating exercise training, education, and self-management strategies. For severe cases, surgical interventions like lung volume reduction surgery or lung transplantation might be considered.
A patient with a history of smoking and progressive shortness of breath would be assessed for COPD. Spirometry would confirm the diagnosis. Management would involve smoking cessation counseling, bronchodilators, and possibly inhaled corticosteroids, followed by regular follow-up and pulmonary rehabilitation.
Q 26. Describe your approach to managing a patient with a gastrointestinal bleed.
Managing a gastrointestinal (GI) bleed requires a rapid assessment to determine the source and severity of bleeding. This starts with stabilizing the patient, including intravenous fluids to maintain blood pressure and oxygen supplementation. A thorough history (including medications, recent illnesses, and travel) and physical examination are crucial. Laboratory investigations include complete blood count (to assess hemoglobin and hematocrit), blood type and crossmatch, clotting studies, and liver function tests. Endoscopy (upper endoscopy or colonoscopy) is the gold standard for identifying the source of bleeding, guiding further treatment. Angiography may be necessary for high-risk bleeds not controlled by endoscopy. Treatment strategies depend on the location and cause of the bleed. This could include endoscopic techniques to stop bleeding (e.g., injection of epinephrine, thermal coagulation), medications to reduce acid production (e.g., proton pump inhibitors), or surgery.
For example, a patient presenting with hematemesis (vomiting blood) would undergo immediate stabilization and then upper endoscopy to identify the source of bleeding, perhaps a peptic ulcer. Based on the endoscopic findings, appropriate treatment, including endoscopic hemostasis or medical management, would be initiated.
Q 27. How do you assess and manage a patient with suspected heart failure?
Suspected heart failure requires a comprehensive assessment, beginning with a detailed history (including symptoms like shortness of breath, fatigue, edema) and physical examination (checking for jugular venous distension, edema, lung sounds). Essential investigations include blood tests (assessing renal function, electrolytes, and biomarkers like BNP or NT-proBNP), electrocardiogram (ECG), and chest X-ray. Echocardiogram is the gold standard for assessing cardiac structure and function, providing crucial information about ejection fraction and valvular function. Management involves optimizing cardiac output and reducing preload and afterload. This includes lifestyle modifications (diet, exercise, weight reduction), medication (diuretics to reduce fluid overload, ACE inhibitors/ARBs to reduce afterload, beta-blockers to reduce heart rate and contractility, and aldosterone antagonists to reduce sodium and water retention). Cardiac resynchronization therapy (CRT) or implantable cardioverter-defibrillators (ICDs) may be considered in specific cases. In severe cases, mechanical circulatory support (e.g., ventricular assist devices) or heart transplantation might be necessary.
For example, a patient presenting with shortness of breath, edema, and reduced ejection fraction on echocardiogram would be diagnosed with heart failure. Management would involve diuretics to manage fluid overload, ACE inhibitors to reduce afterload, beta-blockers to control heart rate, and lifestyle modifications.
Q 28. Explain your strategy for managing a patient with a wound infection.
Managing a wound infection requires a systematic approach. Initial assessment includes evaluating the wound’s appearance (e.g., erythema, swelling, purulent drainage), assessing the patient’s overall condition (fever, leukocytosis), and obtaining a wound culture to identify the causative organism. Treatment depends on the severity of infection. For localized infections, cleaning the wound and applying appropriate topical antibiotics might suffice. More serious infections may require systemic antibiotics, chosen based on the culture results or clinical suspicion. Debridement (surgical removal of infected tissue) may be necessary for extensive infections. Pain management is important. Close monitoring of the patient’s response to treatment and regular wound assessment are crucial. In some cases, surgical drainage may be needed to remove pus and reduce pressure.
For example, a patient with a deep wound showing signs of infection (redness, swelling, pus) would undergo wound debridement, receive systemic antibiotics (based on culture results, if available), and require close monitoring for improvement.
Key Topics to Learn for Diagnosis and Management of Common Medical Conditions Interview
- History Taking and Physical Examination: Mastering the art of obtaining a comprehensive patient history and performing a thorough physical exam to identify key clues pointing towards a diagnosis. This includes understanding the importance of open-ended questions and active listening.
- Differential Diagnosis: Develop the ability to systematically formulate a differential diagnosis, considering various possibilities based on presented symptoms and findings. Practice prioritizing diagnoses based on likelihood and urgency.
- Common Respiratory Conditions: Gain a strong understanding of the diagnosis and management of conditions like pneumonia, asthma, COPD, and influenza. This includes recognizing diagnostic criteria, interpreting relevant investigations (e.g., chest X-ray, spirometry), and outlining appropriate treatment strategies.
- Cardiovascular Conditions: Become proficient in diagnosing and managing common cardiovascular issues such as hypertension, angina, heart failure, and arrhythmias. This includes understanding risk factors, interpreting ECGs, and applying evidence-based management guidelines.
- Gastrointestinal Conditions: Develop expertise in the diagnosis and management of conditions like gastroesophageal reflux disease (GERD), peptic ulcer disease, inflammatory bowel disease, and irritable bowel syndrome. Familiarize yourself with relevant investigations and treatment approaches.
- Diabetes Mellitus: Understand the different types of diabetes, diagnostic criteria, complications, and management strategies, including both pharmacological and lifestyle interventions.
- Infectious Diseases: Familiarize yourself with common infectious diseases, their transmission, diagnostic tests, and treatment protocols. This includes understanding antibiotic stewardship and the importance of infection control.
- Interpreting Laboratory Results: Develop skills in interpreting common laboratory tests relevant to diagnosing and managing these conditions. Understand the limitations and potential biases of laboratory data.
- Clinical Reasoning and Problem-Solving: Practice applying your knowledge to solve complex clinical scenarios. Focus on developing a structured approach to problem-solving, using evidence-based medicine principles.
- Ethical and Legal Considerations: Understand the ethical and legal implications of medical decision-making in the context of diagnosis and management.
Next Steps
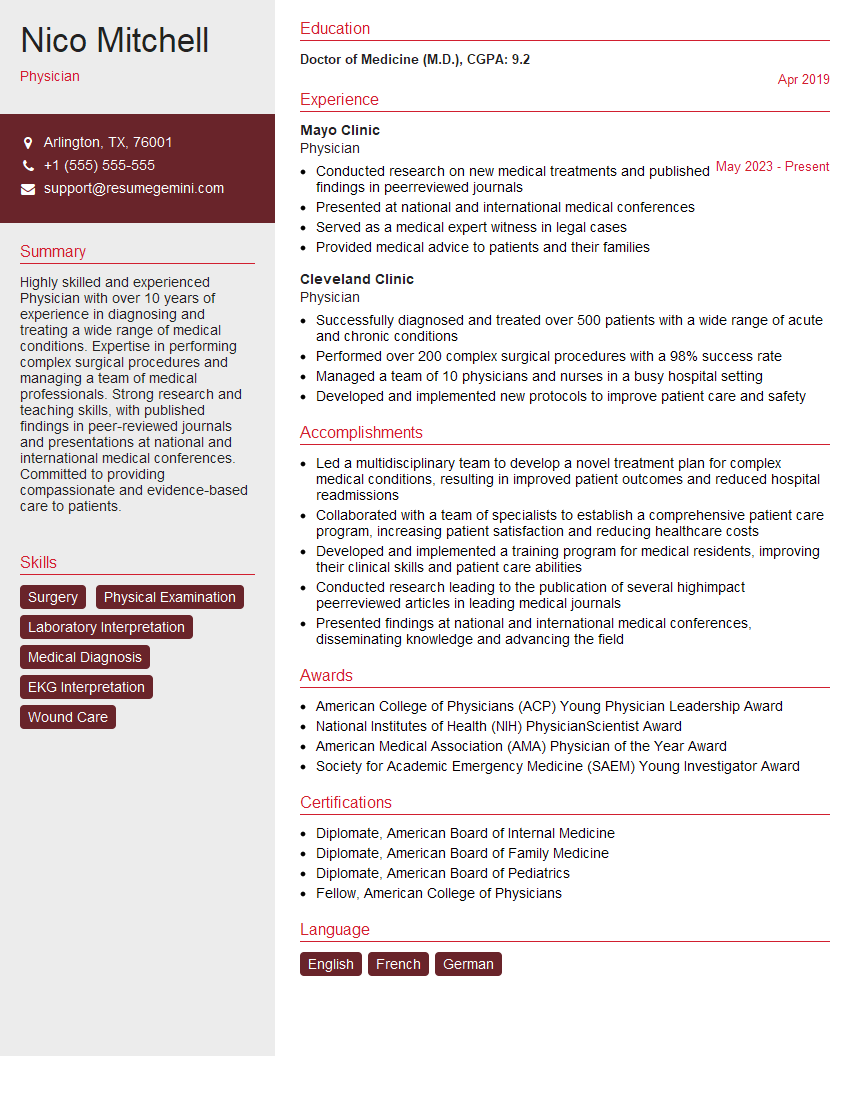
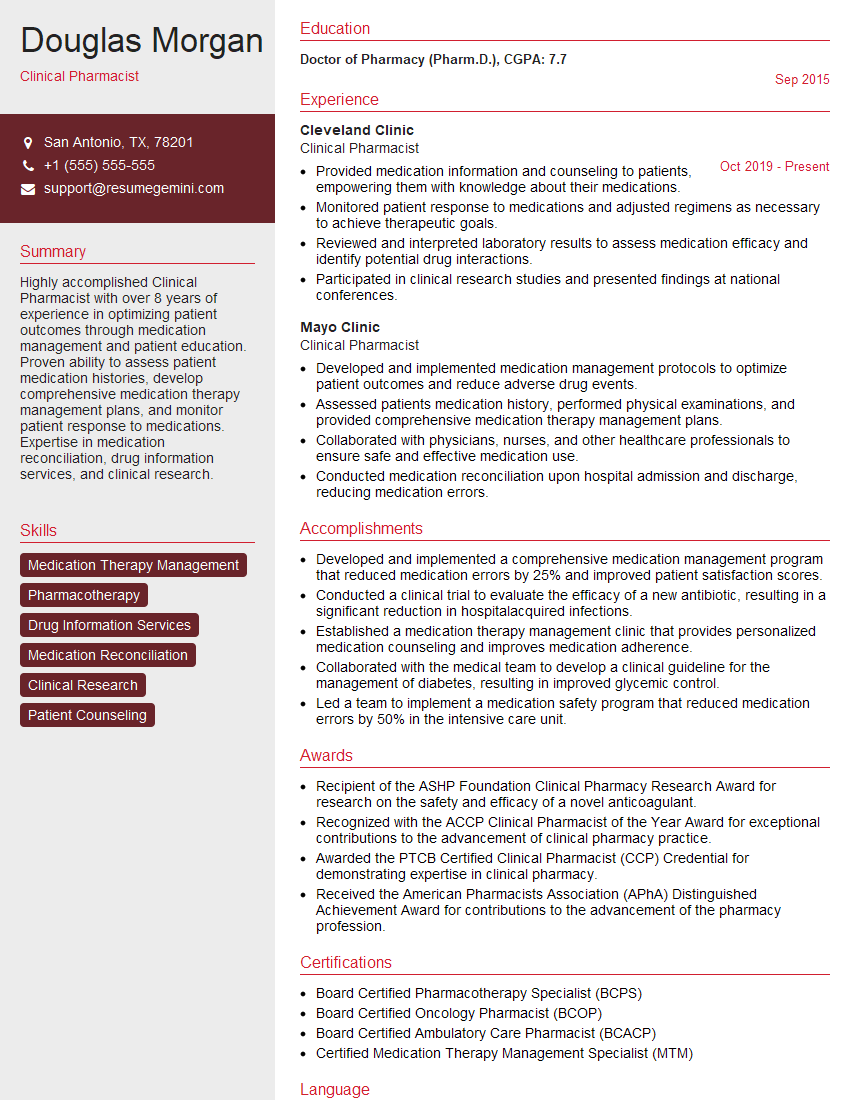
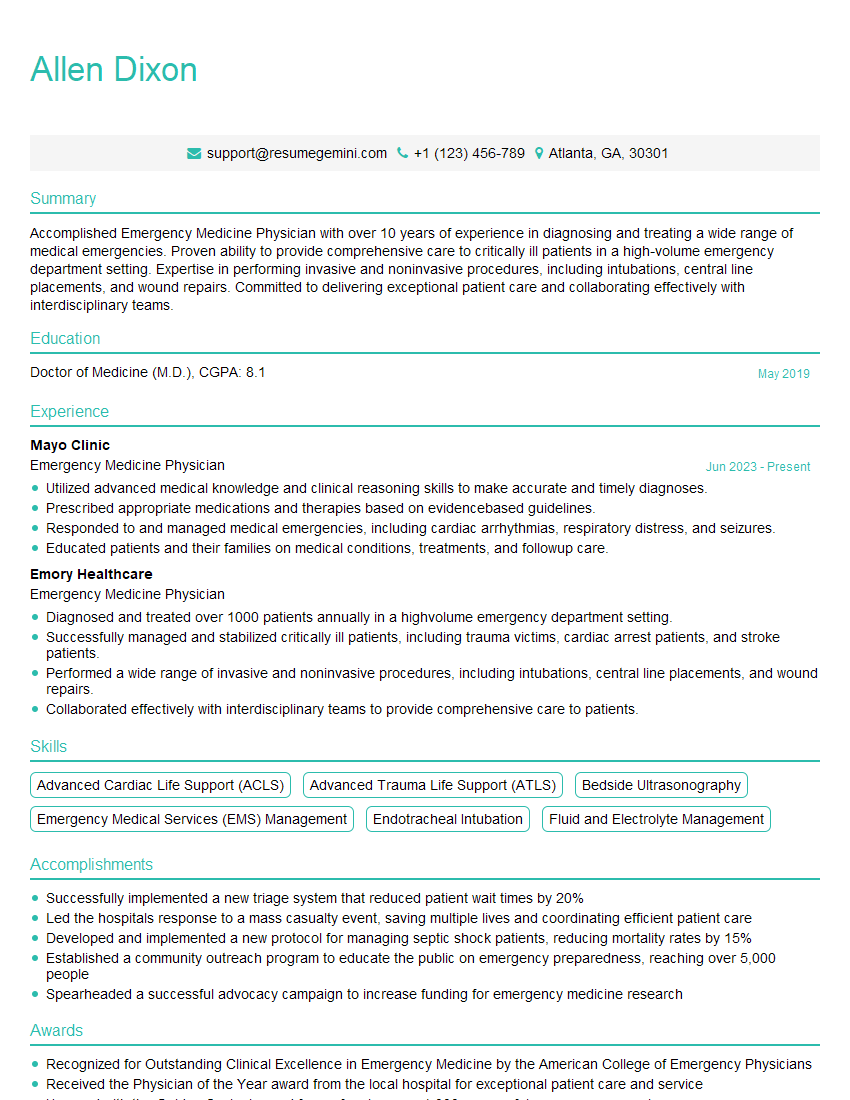
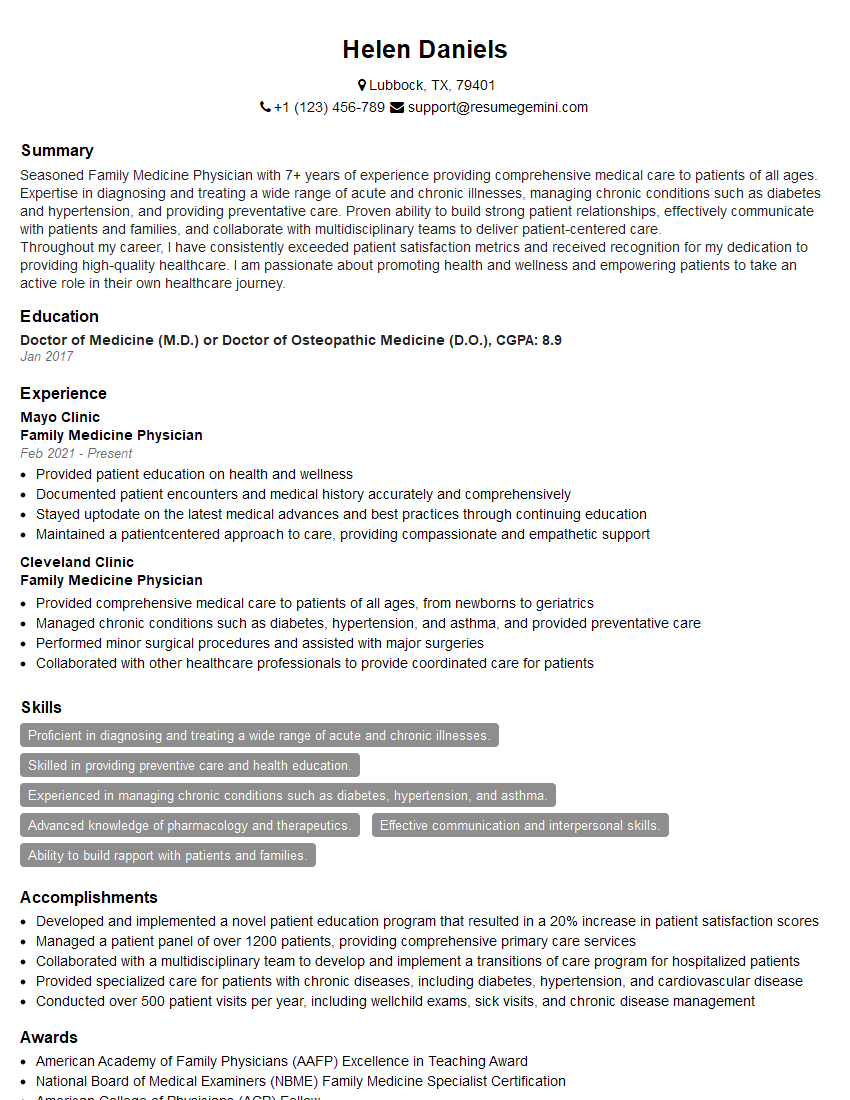
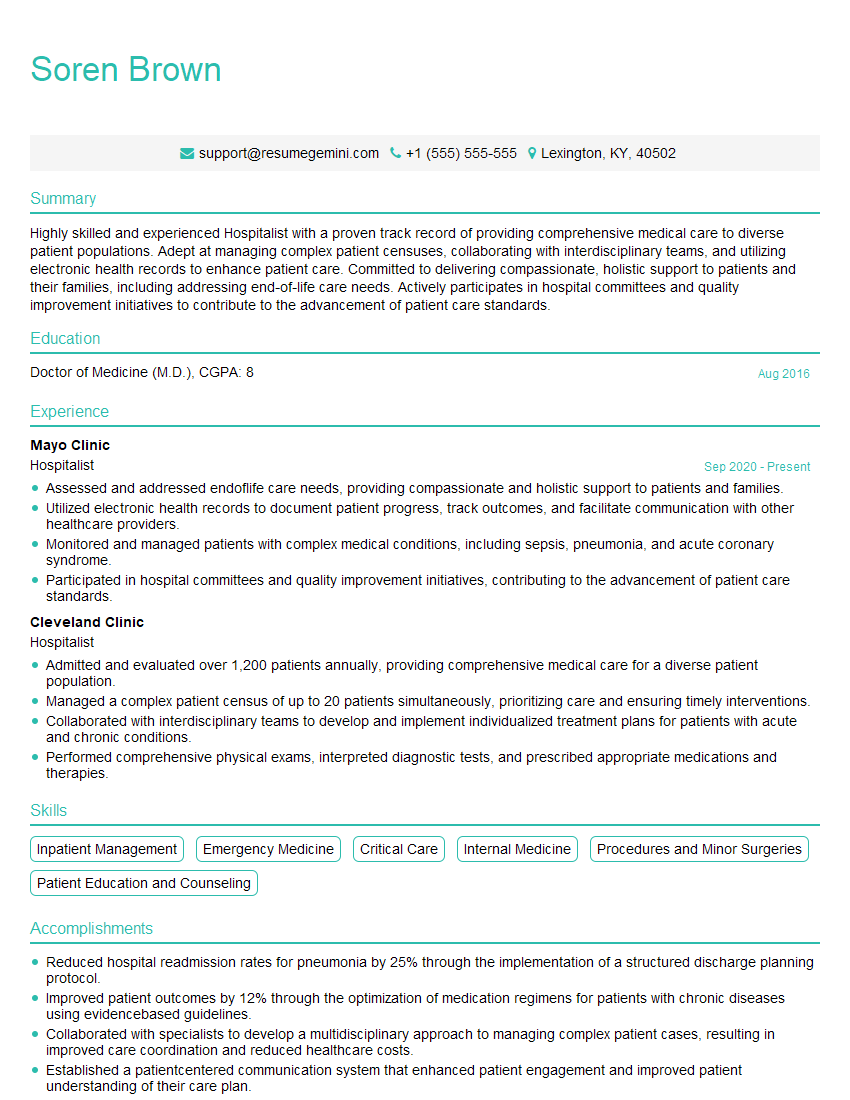
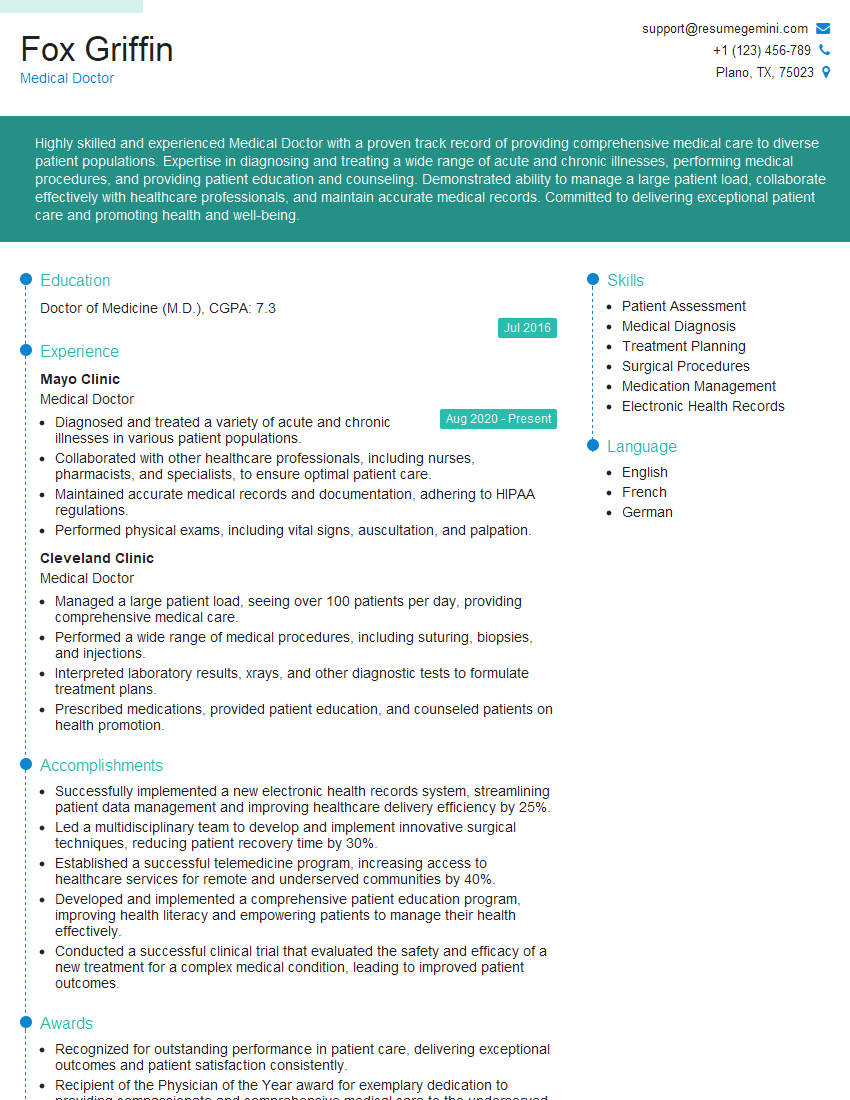
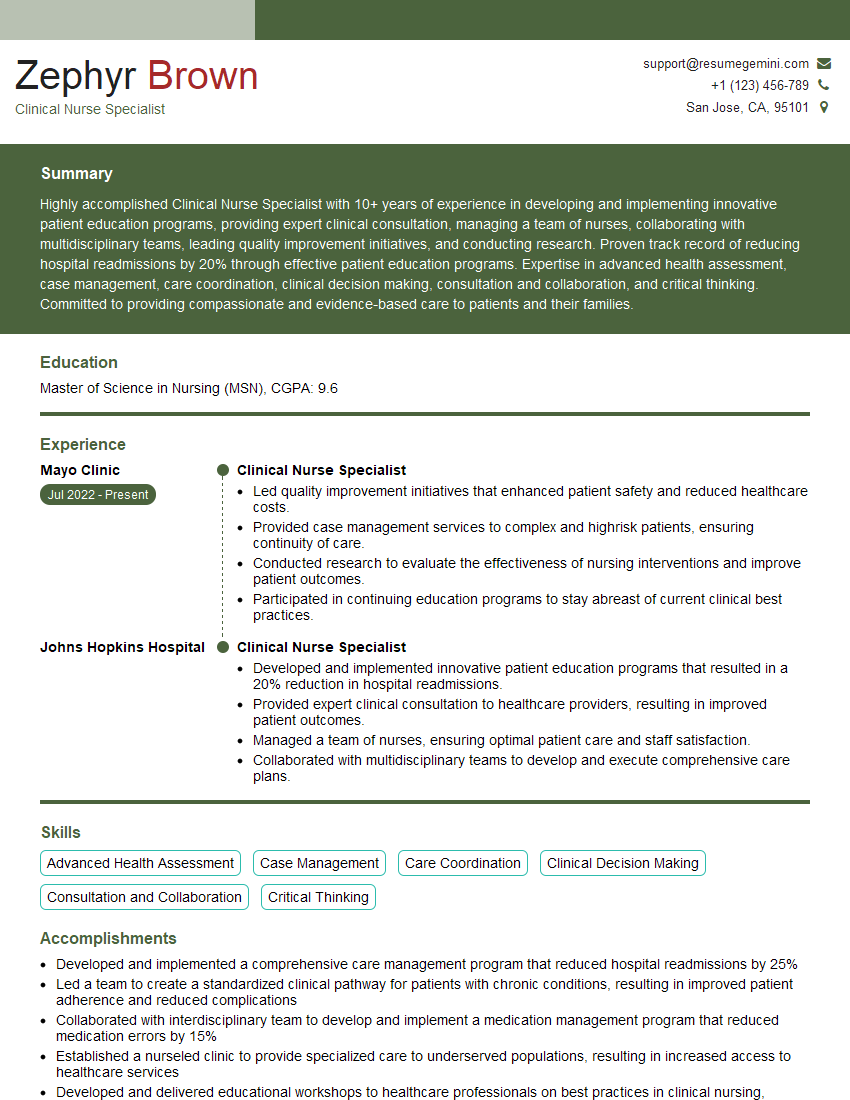
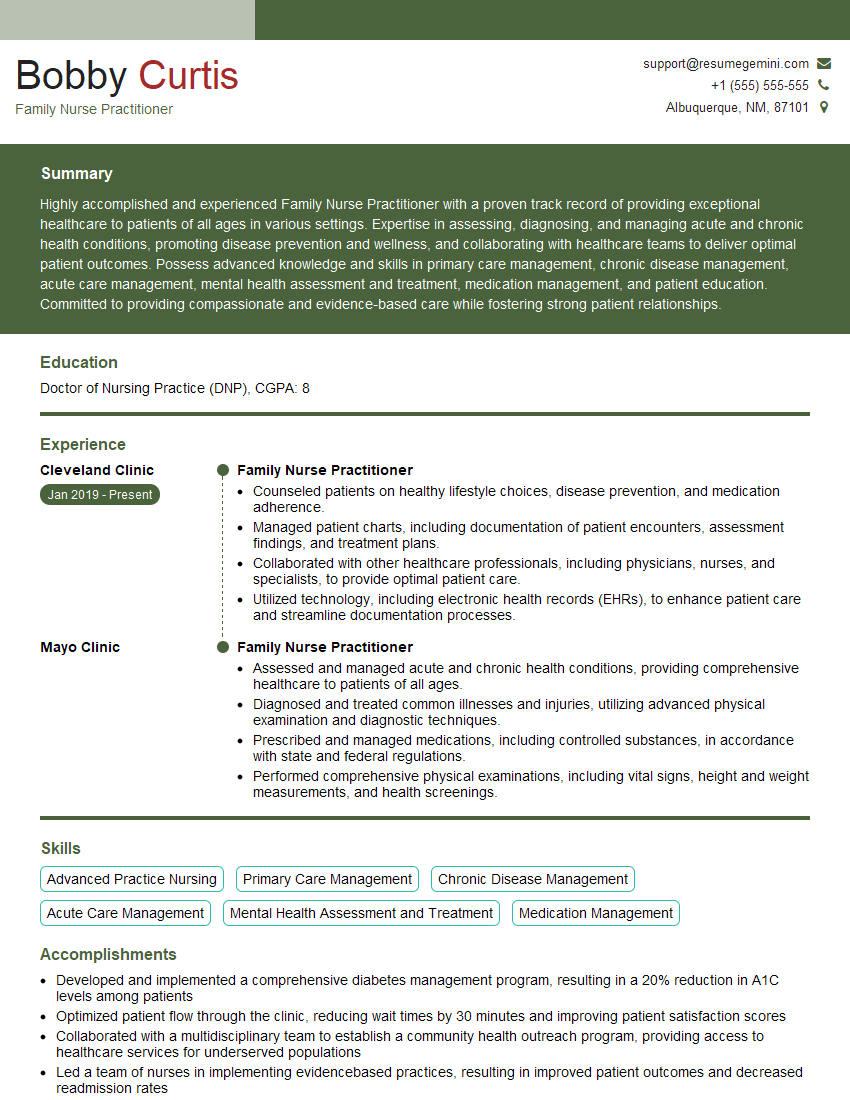
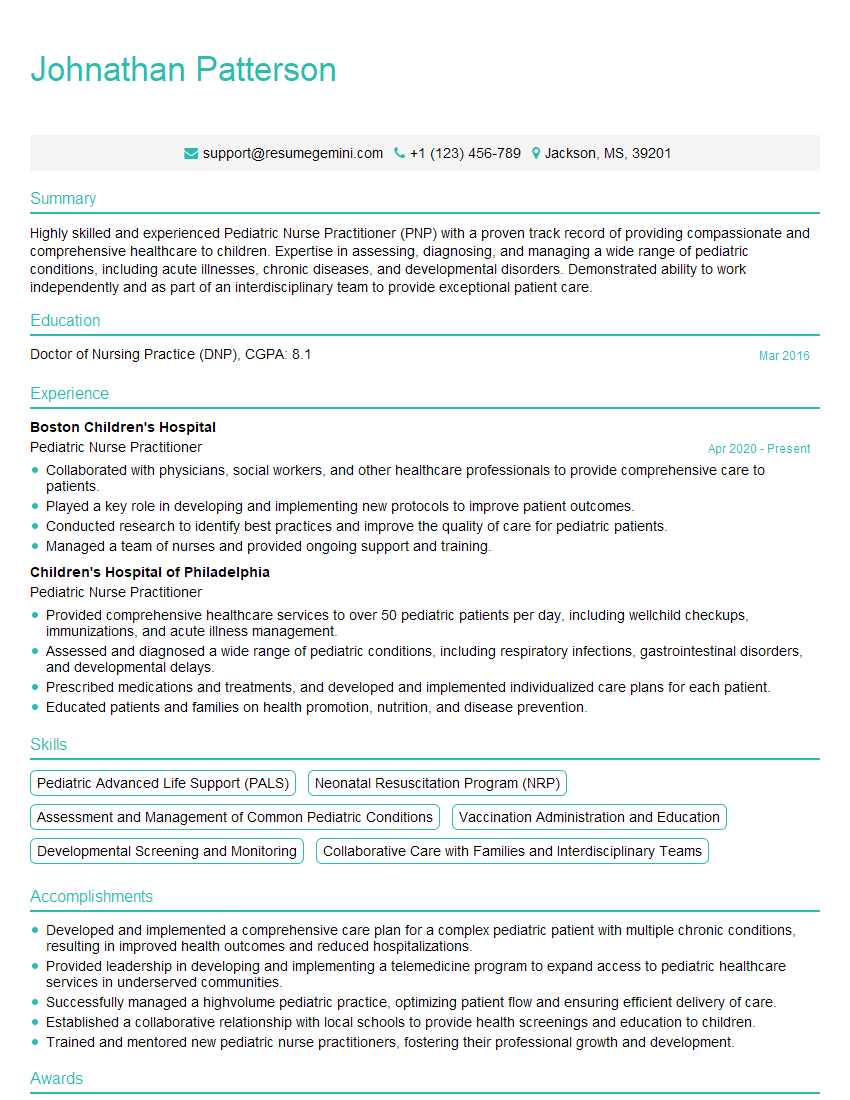
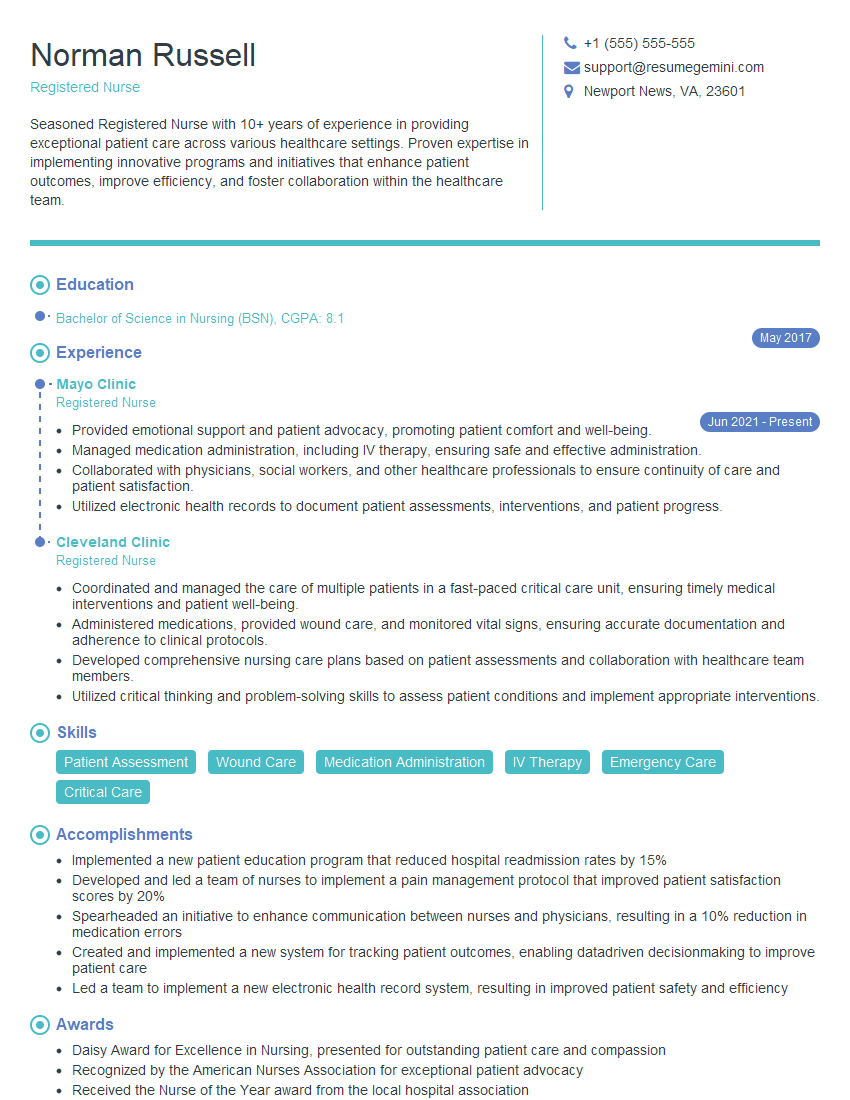
Mastering the diagnosis and management of common medical conditions is crucial for career advancement and demonstrates a strong foundation in clinical practice. A well-crafted, ATS-friendly resume is key to showcasing your skills and experience effectively to potential employers. To maximize your job prospects, consider using ResumeGemini to build a professional and impactful resume. ResumeGemini provides valuable resources and examples of resumes tailored to the Diagnosis and Management of Common Medical Conditions field, helping you stand out from the competition. Invest time in creating a resume that highlights your expertise and resonates with hiring managers. This will significantly improve your chances of securing your desired role.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.