The thought of an interview can be nerve-wracking, but the right preparation can make all the difference. Explore this comprehensive guide to Diagnosis and Treatment of Acute and Chronic Medical Conditions interview questions and gain the confidence you need to showcase your abilities and secure the role.
Questions Asked in Diagnosis and Treatment of Acute and Chronic Medical Conditions Interview
Q 1. Describe your approach to diagnosing a patient presenting with acute chest pain.
Diagnosing acute chest pain requires a rapid and systematic approach because it can signify life-threatening conditions like a heart attack. My approach begins with immediate assessment of the patient’s vital signs – heart rate, blood pressure, respiratory rate, and oxygen saturation. I’ll then obtain a thorough history, focusing on the characteristics of the pain (location, radiation, quality, severity, duration, associated symptoms like nausea, sweating, shortness of breath).
Simultaneously, I’ll conduct a physical examination, paying close attention to heart sounds (for murmurs or rubs), lung sounds (for crackles or wheezes), and peripheral pulses. Electrocardiogram (ECG) is crucial to detect any abnormalities in heart rhythm or evidence of myocardial ischemia (reduced blood flow to the heart). Blood tests, including cardiac enzymes (troponin), will be ordered to rule out a heart attack. Further investigations, such as a chest X-ray or echocardiogram, may be necessary depending on the initial findings. The entire process is about rapid triage to identify potentially life-threatening situations and initiate appropriate interventions while systematically ruling out other possible causes like pericarditis, pneumothorax, or esophageal spasm. For example, a patient presenting with crushing chest pain radiating to the left arm, associated with shortness of breath and diaphoresis, would immediately raise suspicion of a myocardial infarction, prompting urgent intervention.
Q 2. Explain the differential diagnosis for shortness of breath.
Shortness of breath (dyspnea) has a vast differential diagnosis, meaning many conditions can cause it. It’s crucial to consider the context – is it sudden onset or gradual? Is it related to exertion or position? Are there any other symptoms present?
- Cardiovascular causes: Heart failure, pulmonary embolism (blood clot in the lung), valvular heart disease, arrhythmias.
- Pulmonary causes: Pneumonia, asthma, chronic obstructive pulmonary disease (COPD), pneumothorax (collapsed lung), pulmonary fibrosis.
- Other causes: Anemia, anxiety, obesity, pleural effusion (fluid around the lungs), metabolic acidosis, neurological conditions.
For example, sudden onset dyspnea with pleuritic chest pain (pain worsened by breathing) could suggest a pulmonary embolism. Gradual worsening of dyspnea with chronic cough and wheezing might point towards COPD. Dyspnea exacerbated by exertion in a patient with known heart disease could indicate heart failure. A comprehensive history, physical examination, and appropriate investigations like chest X-ray, ECG, blood tests, and potentially CT pulmonary angiography (for PE), are essential to arrive at an accurate diagnosis.
Q 3. How would you manage a patient with a newly diagnosed type 2 diabetes?
Managing newly diagnosed type 2 diabetes involves a multi-faceted approach focusing on lifestyle modifications and medication. The initial goal is to achieve and maintain glycemic control (blood sugar levels), prevent or delay long-term complications, and improve overall health.
- Lifestyle Changes: This is paramount and includes weight loss (if overweight or obese), regular physical activity (at least 150 minutes of moderate-intensity aerobic activity per week), and a healthy diet (low in saturated and trans fats, refined carbohydrates, and high in fruits, vegetables, and whole grains).
- Medication: Metformin is usually the first-line medication for most patients unless contraindicated. Other medications, such as sulfonylureas, DPP-4 inhibitors, SGLT2 inhibitors, or GLP-1 receptor agonists, may be added based on individual needs and response to treatment. The choice depends on factors like age, other medical conditions, and individual preferences.
- Regular Monitoring: Regular monitoring of blood glucose levels (HbA1c, fasting blood glucose), blood pressure, and lipid profile is crucial to assess treatment effectiveness and make necessary adjustments.
- Education and Support: Providing patients with comprehensive education about diabetes self-management, including diet, exercise, medication, and monitoring, is essential for long-term success. Support groups and regular follow-up appointments with healthcare professionals are vital for adherence to the treatment plan.
For instance, a newly diagnosed 55-year-old overweight patient with a family history of diabetes would likely start with lifestyle modifications and metformin. Regular monitoring and adjustments to the treatment plan based on blood glucose levels and other factors would be necessary to achieve optimal glycemic control and prevent complications.
Q 4. Outline the treatment plan for a patient experiencing an acute asthma exacerbation.
Managing an acute asthma exacerbation is a medical emergency requiring prompt intervention to prevent life-threatening complications. The treatment aims to rapidly relieve symptoms and restore normal lung function.
- Oxygen Therapy: Supplemental oxygen is essential to maintain oxygen saturation levels.
- Bronchodilators: Short-acting beta-agonists (SABAs) like albuterol, delivered via nebulizer or metered-dose inhaler, are the cornerstone of treatment, providing immediate relief of bronchospasm.
- Systemic Corticosteroids: Oral or intravenous corticosteroids (like prednisone or methylprednisolone) are given to reduce inflammation in the airways. This helps prevent further exacerbations.
- Additional Measures: If symptoms do not improve with initial treatment, further interventions might be necessary, including additional bronchodilators such as ipratropium bromide, magnesium sulfate, or even mechanical ventilation in severe cases.
- Monitoring: Continuous monitoring of respiratory rate, oxygen saturation, and clinical status is essential to guide treatment and identify any signs of deterioration.
For example, a patient presenting with severe wheezing, shortness of breath, and decreased oxygen saturation would require immediate administration of oxygen, albuterol via nebulizer, and a course of oral corticosteroids. Frequent monitoring of vital signs and clinical response would be crucial to ensure effectiveness of the treatment and to escalate care if necessary. In severe cases requiring mechanical ventilation, close monitoring in the ICU is essential.
Q 5. What are the key indicators of heart failure, and how would you assess their severity?
Heart failure is a condition where the heart can’t pump enough blood to meet the body’s needs. Key indicators include shortness of breath (especially with exertion or lying down – orthopnea and paroxysmal nocturnal dyspnea), fatigue, edema (swelling in the legs, ankles, and feet), persistent cough, and rapid or irregular heartbeat.
Assessing severity involves evaluating multiple factors:
- Symptoms: The presence and severity of symptoms like shortness of breath, fatigue, and edema are crucial indicators. The New York Heart Association (NYHA) classification is often used to stage the severity based on functional capacity and symptom limitations.
- Physical Examination: Auscultation for heart sounds (e.g., gallops, murmurs), assessing jugular venous pressure (JVP), and checking for edema help gauge the extent of fluid overload and heart function.
- Laboratory Tests: Blood tests, including brain natriuretic peptide (BNP) and N-terminal pro-BNP (NT-proBNP), help assess the severity and prognosis.
- Imaging Studies: Echocardiography provides detailed information about the heart’s structure and function, ejection fraction (amount of blood pumped out with each contraction), and valvular function. Chest X-rays help assess for fluid buildup in the lungs.
For example, a patient with significant shortness of breath at rest (NYHA Class III or IV), elevated BNP levels, low ejection fraction on echocardiogram, and pulmonary edema on chest X-ray would be considered to have severe heart failure.
Q 6. Discuss the management of hypertension in an elderly patient.
Managing hypertension in the elderly requires a careful and individualized approach due to increased risk of adverse events and the presence of comorbidities.
- Lifestyle Modifications: These are fundamental and include a low-sodium diet, weight management, regular physical activity, and limiting alcohol intake. These modifications are often more crucial in elderly patients due to potential for adverse drug interactions and increased sensitivity to medications.
- Medication: Thiazide diuretics are often the first-line choice due to their efficacy and safety profile in older adults. Other classes of drugs, such as ACE inhibitors, ARBs, beta-blockers, and calcium channel blockers, may be used alone or in combination, depending on individual needs and comorbidities (like diabetes, heart failure, or chronic kidney disease). Dosage adjustments are often necessary due to age-related changes in drug metabolism and excretion.
- Regular Monitoring: Close monitoring of blood pressure, kidney function, and electrolyte levels is vital due to increased risk of side effects from medication in older adults. Careful consideration should be given to the potential for drug interactions with other medications the patient is taking.
- Patient Education and Support: Educating elderly patients and their caregivers about their medication regimen, lifestyle changes, and the importance of regular follow-up appointments is key to successful management.
For instance, an 80-year-old patient with hypertension and a history of diabetes might be started on a low dose of a thiazide diuretic, with careful monitoring of blood pressure and kidney function. If blood pressure remains uncontrolled, another medication might be added, but dosage adjustments must consider the patient’s age and the risks of medication side effects.
Q 7. How do you differentiate between bacterial and viral pneumonia?
Differentiating between bacterial and viral pneumonia requires a combination of clinical findings, laboratory tests, and sometimes imaging studies. While symptoms can overlap, some key differences exist.
- Clinical Presentation: Bacterial pneumonia often presents with a more abrupt onset of high fever, chills, productive cough (with purulent sputum – thick, discolored mucus), and pleuritic chest pain. Viral pneumonia tends to have a more gradual onset with less severe symptoms like low-grade fever, non-productive cough, and less severe chest pain.
- Laboratory Tests: Chest X-ray shows characteristic consolidation (area of lung tissue filled with fluid) more often in bacterial pneumonia than viral. Blood tests may show an increased white blood cell count (leukocytosis) suggestive of bacterial infection, though this isn’t always definitive. Sputum culture can help identify the specific bacteria causing the infection in bacterial pneumonia.
- Other Tests: Sometimes more advanced tests like blood cultures or procalcitonin levels are ordered to further distinguish between bacterial and viral origins.
It’s important to note that the clinical presentation can vary, and some cases may be challenging to differentiate. Treatment is often initiated empirically (based on clinical suspicion) and adjusted based on laboratory results and clinical response. For example, a patient with abrupt onset of high fever, productive cough with rusty-colored sputum, and a chest X-ray showing consolidation would strongly suggest bacterial pneumonia, while a patient with a gradual onset of milder symptoms and a chest x-ray showing interstitial changes is more likely to have viral pneumonia. However, definitive diagnosis often requires the combination of clinical presentation, chest imaging, and laboratory testing.
Q 8. Describe your approach to managing a patient with chronic kidney disease.
Managing chronic kidney disease (CKD) is a multifaceted process requiring a collaborative approach between the patient and healthcare team. It centers on slowing disease progression, managing symptoms, and preventing complications. Our approach starts with a thorough assessment of the patient’s kidney function, using measures like glomerular filtration rate (GFR) and albuminuria. We then stage the CKD based on these findings to guide treatment.
Key aspects of our management strategy include:
- Blood pressure control: Tight blood pressure control is crucial to slowing CKD progression. We aim for a target blood pressure below 140/90 mmHg, often using a combination of medications like ACE inhibitors, ARBs, or beta-blockers.
- Diabetes management: In patients with diabetes, meticulous blood glucose control is paramount. This often involves insulin therapy, lifestyle modifications, and regular monitoring.
- Dietary adjustments: A diet restricted in protein, phosphorus, potassium, and sodium is often recommended to reduce the burden on the kidneys. We work with registered dieticians to create personalized dietary plans that are both effective and palatable.
- Medication management: We carefully select and monitor medications, minimizing nephrotoxic drugs (those that can damage the kidneys). We also manage anemia with erythropoiesis-stimulating agents and address electrolyte imbalances as needed.
- Regular monitoring: This involves frequent blood tests to monitor kidney function, electrolyte levels, and anemia. We also assess for complications like bone disease, cardiovascular disease, and infections.
- Referral to specialists: Depending on the stage of CKD and the presence of complications, referral to nephrologists, cardiologists, and other specialists may be necessary.
- Patient education and support: Educating the patient about their condition, treatment plan, and lifestyle modifications is essential for successful management. We also connect patients with support groups and resources to help them cope with the challenges of CKD.
For example, a patient with stage 3 CKD and diabetes might require a combination of ACE inhibitors, metformin, a low-protein diet, and regular blood tests to monitor their kidney function and blood glucose levels. We would also discuss the importance of lifestyle changes such as regular exercise and smoking cessation.
Q 9. What are the risk factors for stroke, and how can they be mitigated?
Stroke, a disruption of blood supply to the brain, is a significant cause of disability and death. Several modifiable and non-modifiable risk factors contribute to stroke risk.
Risk Factors:
- Non-Modifiable: Age (risk increases with age), sex (men are slightly more at risk), family history of stroke
- Modifiable: Hypertension (high blood pressure), high cholesterol, diabetes, atrial fibrillation (irregular heartbeat), smoking, obesity, physical inactivity, excessive alcohol consumption, drug abuse (cocaine use is particularly risky).
Mitigation Strategies:
- Blood pressure control: Regular monitoring and medication (if needed) to maintain healthy blood pressure levels.
- Cholesterol management: Dietary changes, exercise, and statin medications (if necessary) to lower cholesterol.
- Diabetes management: Blood glucose control through diet, exercise, and medications.
- Atrial fibrillation management: Medication to thin the blood (anticoagulants) to prevent clot formation.
- Smoking cessation: Counseling and support programs to help quit smoking.
- Weight management: Healthy diet and regular exercise to achieve and maintain a healthy weight.
- Regular exercise: At least 150 minutes of moderate-intensity aerobic activity per week.
- Limited alcohol consumption: Following recommended guidelines for alcohol intake.
- Healthy Diet: A balanced diet rich in fruits, vegetables, and whole grains.
For instance, a patient with hypertension and high cholesterol would benefit from lifestyle modifications such as a low-sodium, low-fat diet, regular exercise, and medication to lower both blood pressure and cholesterol levels. Early detection and management of these risk factors are vital in preventing stroke.
Q 10. Explain the pathophysiology of coronary artery disease.
Coronary artery disease (CAD) is characterized by the buildup of plaque (atherosclerosis) within the coronary arteries, which supply blood to the heart muscle. This plaque consists of cholesterol, fats, calcium, and other substances. Over time, this buildup narrows the arteries, reducing blood flow to the heart.
Pathophysiology:
- Endothelial Dysfunction: The process begins with damage to the endothelium (inner lining) of the arteries. This damage can be caused by various factors, including high blood pressure, high cholesterol, smoking, and diabetes.
- Inflammation: The damaged endothelium triggers an inflammatory response, attracting immune cells to the area. These cells contribute to the formation of plaque.
- Lipid Accumulation: LDL cholesterol (often referred to as “bad” cholesterol) infiltrates the artery wall, contributing significantly to plaque formation.
- Plaque Growth: The plaque continues to grow, leading to thickening and hardening of the artery walls (atherosclerosis).
- Ischemia: As the arteries narrow, blood flow to the heart muscle is reduced (ischemia). This can lead to angina (chest pain) or, in severe cases, a heart attack (myocardial infarction).
- Thrombosis: Plaque can rupture, leading to the formation of a blood clot (thrombosis). This clot can completely block blood flow to a part of the heart, resulting in a heart attack.
In essence, it’s a progressive disease where gradual narrowing of the coronary arteries eventually disrupts blood supply to the heart, leading to various symptoms and potentially life-threatening events. Understanding this pathophysiology allows for targeted prevention and treatment strategies.
Q 11. How would you assess a patient’s cognitive function?
Assessing a patient’s cognitive function involves a multi-faceted approach that takes into account various aspects of mental abilities. There’s no single test; the approach is tailored to the individual’s presentation and suspected cognitive impairments.
Assessment Methods:
- History Taking: A detailed medical history, including information about the patient’s concerns, current medications, and past medical history, is crucial. Gathering information from family members or caregivers can be beneficial.
- Mental Status Examination (MSE): A structured assessment of various cognitive domains, including orientation (time, place, person), attention, memory (short-term and long-term), language, visuospatial skills, and executive functions (planning, problem-solving). Examples of MSE elements include asking the patient to recall three words after a short delay, or to draw a clock.
- Neuropsychological Testing: More formal tests administered by trained professionals to evaluate specific cognitive functions in greater detail. These tests are often used to differentiate between different types of cognitive impairment.
- Imaging Studies: Brain imaging techniques such as MRI or CT scans can detect structural abnormalities in the brain that might be contributing to cognitive impairment.
- Laboratory Tests: Blood tests can help rule out medical conditions that can mimic cognitive impairment, such as thyroid disorders or vitamin deficiencies.
For example, a patient presenting with memory problems might undergo an MSE, followed by specific memory tests if indicated. If the MSE reveals significant impairment, neuropsychological testing may be warranted to obtain a more comprehensive profile of their cognitive strengths and weaknesses. Blood tests and brain imaging would help rule out other causes.
Q 12. What are the common causes of chronic abdominal pain, and how do you investigate them?
Chronic abdominal pain is a common complaint with a wide range of potential causes. A thorough investigation is necessary to determine the underlying etiology.
Common Causes:
- Gastrointestinal Disorders: Irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), peptic ulcer disease, celiac disease, gastroparesis
- Gynecological Conditions: Endometriosis, pelvic inflammatory disease (PID), fibroids
- Urological Conditions: Kidney stones, urinary tract infections (UTIs), interstitial cystitis
- Musculoskeletal Conditions: Muscle strains, hernias, back problems
- Other Causes: Food intolerances, abdominal adhesions (scar tissue), anxiety, depression
Investigation:
The investigation is tailored to the individual patient’s presentation and history but often involves:
- Detailed History: Characterizing the pain (location, onset, duration, aggravating/relieving factors), associated symptoms (nausea, vomiting, diarrhea, constipation, fever, weight loss), menstrual history (for women), bowel habits.
- Physical Examination: Palpating the abdomen to assess for tenderness, masses, or rigidity.
- Laboratory Tests: Blood tests (complete blood count, inflammatory markers, liver function tests), stool tests (occult blood, parasites).
- Imaging Studies: Abdominal X-ray, ultrasound, CT scan, MRI, depending on the suspected diagnosis.
- Endoscopy: Upper endoscopy (esophagus, stomach, duodenum), colonoscopy (large intestine), if gastrointestinal causes are suspected.
For example, a patient with persistent right lower quadrant pain, fever, and vomiting might undergo an abdominal ultrasound or CT scan to investigate appendicitis. A patient with chronic diarrhea and weight loss might require a colonoscopy to rule out inflammatory bowel disease.
Q 13. Discuss the management of a patient with a severe allergic reaction.
Management of a severe allergic reaction (anaphylaxis) is a medical emergency requiring immediate intervention. Anaphylaxis is a life-threatening, systemic reaction that can rapidly progress and lead to death if not treated promptly.
Management:
- Immediate Action: The first priority is to ensure the patient’s airway is patent. If the patient is having difficulty breathing, assist with breathing (e.g., positioning, oxygen) or intubate if necessary.
- Epinephrine Administration: Epinephrine is the cornerstone of anaphylaxis treatment. It is administered intramuscularly (usually into the thigh) to reverse the effects of histamine release. Repeat doses may be required.
- Supportive Care: This includes monitoring vital signs, managing airway and breathing, administering intravenous fluids, and providing oxygen.
- Additional Medications: Depending on the patient’s symptoms, additional medications may be necessary, such as antihistamines (diphenhydramine) to counteract further histamine effects and corticosteroids (e.g., methylprednisolone) to reduce inflammation.
- Monitoring and Observation: Patients experiencing anaphylaxis require close monitoring in a hospital setting for several hours, even after initial symptom improvement, as a biphasic reaction (a recurrence of symptoms) can occur.
Imagine a patient who experiences sudden swelling of the tongue and throat, difficulty breathing, and a drop in blood pressure after an insect sting. Immediate intramuscular epinephrine is administered, followed by supportive care and transfer to the emergency department. The patient will receive close monitoring for potential recurrence of symptoms. This emphasizes the importance of prompt recognition and treatment to prevent a potentially fatal outcome.
Q 14. Explain the importance of patient education in managing chronic conditions.
Patient education plays a vital role in managing chronic conditions. It empowers patients to actively participate in their care, improving adherence to treatment plans and leading to better health outcomes. Without understanding their condition, patients are less likely to follow prescribed medication regimens, lifestyle changes, or regular monitoring schedules.
Importance of Patient Education:
- Improved Adherence: When patients understand their condition and treatment plan, they are more likely to adhere to medication regimens, follow dietary recommendations, and make necessary lifestyle changes.
- Enhanced Self-Management: Patient education enables self-monitoring and early detection of complications, allowing for prompt intervention. For example, a patient with diabetes learning how to monitor their blood glucose can take timely action to prevent complications.
- Improved Quality of Life: Understanding the disease process and available treatment options empowers patients, reducing fear and anxiety associated with chronic illness and leading to improved quality of life.
- Reduced Hospitalizations and Emergency Room Visits: By actively managing their condition and promptly addressing potential problems, patients can significantly reduce the need for hospitalizations and emergency department visits.
- Cost-Effectiveness: Improved self-management and adherence to treatment plans translate into long-term cost savings for both the patient and the healthcare system.
For instance, a patient with hypertension learns the importance of regular blood pressure monitoring, dietary sodium restriction, and adherence to their medication. This knowledge empowers them to actively participate in their care, improving their chances of successful blood pressure management and reducing their risk of stroke or heart attack. Patient education strategies include individual consultations, group sessions, educational materials, and the use of technology (e.g., mobile apps).
Q 15. How do you approach a patient with symptoms suggestive of depression?
Approaching a patient with symptoms suggestive of depression requires a multifaceted approach emphasizing empathy, thorough assessment, and collaborative care. I begin by establishing a safe and trusting environment, using open-ended questions to understand the patient’s experiences, thoughts, and feelings. This includes inquiring about their mood, sleep patterns, appetite changes, energy levels, concentration, and any suicidal ideation. It’s crucial to listen actively and validate their feelings without judgment.
A comprehensive assessment involves evaluating the duration and severity of symptoms, exploring potential contributing factors (e.g., life stressors, medical conditions, substance use), and ruling out other medical conditions that can mimic depression. This might involve blood work, physical examination, and possibly referral to other specialists.
Based on the assessment, I’d develop a personalized treatment plan that may involve psychotherapy (e.g., cognitive behavioral therapy, interpersonal therapy), medication (antidepressants), or a combination of both. Regular monitoring is essential to assess treatment response, adjust medications as needed, and provide ongoing support. Close collaboration with the patient, their family (with the patient’s consent), and other healthcare professionals ensures optimal care and improves adherence to the treatment plan. For example, if a patient presents with persistent sadness, fatigue, and loss of interest in activities, and screens positive for depression on validated scales, I would discuss treatment options, including therapy and potentially antidepressants like SSRIs or SNRIs, explaining the potential benefits and side effects in detail.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience with interpreting electrocardiograms (ECGs).
Interpreting electrocardiograms (ECGs) is a crucial skill for any physician. My experience encompasses years of analyzing ECGs in various clinical settings, from routine check-ups to emergency situations. I’m proficient in identifying normal sinus rhythm, various arrhythmias (e.g., atrial fibrillation, ventricular tachycardia), conduction abnormalities (e.g., bundle branch blocks, heart blocks), and ischemic changes (e.g., ST-segment elevation myocardial infarction, ST-segment depression).
My interpretation process begins with a systematic review of the ECG tracing, focusing on the rate, rhythm, axis, and intervals. I look for characteristic features of different arrhythmias and ischemic patterns. For example, a rapid, irregularly irregular rhythm with absent P waves strongly suggests atrial fibrillation. ST-segment elevation in multiple leads would be indicative of a STEMI (ST-elevation myocardial infarction), requiring immediate intervention. It’s not merely about identifying abnormalities; understanding the clinical context is vital. The patient’s symptoms, medical history, and other clinical findings help me determine the significance of ECG findings and guide my treatment decisions. I always cross-reference ECG results with other diagnostic information to arrive at a comprehensive diagnosis.
I regularly utilize ECG interpretation software and resources to enhance accuracy and efficiency, but ultimately, clinical judgment and experience are paramount. Misinterpretation can have serious consequences, so I always prioritize thoroughness and attention to detail.
Q 17. How would you manage a patient with uncontrolled bleeding?
Managing uncontrolled bleeding is a critical emergency situation requiring immediate action. The first step is to assess the severity and source of bleeding. This involves identifying the location of the bleeding (e.g., external, internal), the rate of blood loss, and the patient’s vital signs (e.g., blood pressure, heart rate, respiratory rate).
Simultaneously, I’d initiate basic life support measures, including applying direct pressure to the bleeding site, elevating the injured extremity if possible, and maintaining the patient’s airway, breathing, and circulation (ABCs). For severe external bleeding, I might use tourniquets as a last resort, carefully documenting their application time and location. For internal bleeding, I would focus on fluid resuscitation (IV fluids) to maintain blood pressure and prepare for potential blood transfusions.
Depending on the suspected source and severity, I would order relevant investigations (e.g., blood tests, imaging studies) and potentially initiate advanced interventions, such as surgery or angiographic procedures. Throughout the process, close monitoring of vital signs and the patient’s overall condition is essential. Patient monitoring and prompt intervention are critical in determining successful management of uncontrolled bleeding.
Q 18. Describe your approach to wound care.
Wound care is a crucial aspect of patient management, encompassing assessment, cleaning, closure, and ongoing monitoring to promote healing and prevent complications. My approach begins with a thorough assessment of the wound, noting its size, depth, location, and the presence of any foreign bodies, signs of infection (e.g., redness, swelling, pus), or significant bleeding.
Cleaning the wound involves gentle irrigation with sterile saline solution to remove debris and contaminants. I would then assess the need for wound closure, which depends on the wound’s characteristics and the patient’s overall health. Options include sutures, staples, or wound adhesives. Simple wounds that are clean and superficial may be left open to heal by secondary intention.
Following closure, I’d apply appropriate dressings to protect the wound, absorb drainage, and maintain a moist environment conducive to healing. Pain management is also important, utilizing analgesics as needed. Regular follow-up visits are crucial to monitor wound healing, assess for complications (e.g., infection, dehiscence), and adjust the treatment plan if necessary. Patient education about wound care (e.g., hygiene, dressing changes) is an integral part of my approach. For example, a deep laceration requiring sutures would be cleaned meticulously, sutured, and covered with a sterile dressing. The patient would receive instructions on wound care and follow-up appointments to monitor for any signs of infection.
Q 19. What are the common side effects of commonly prescribed medications for diabetes?
Commonly prescribed medications for diabetes, such as insulin and oral hypoglycemics, can have several side effects. Insulin, while highly effective, can cause hypoglycemia (low blood sugar), characterized by symptoms like shakiness, sweating, confusion, and even loss of consciousness. Weight gain is another potential side effect.
Oral hypoglycemics, like metformin, can lead to gastrointestinal side effects such as nausea, diarrhea, and abdominal discomfort. Metformin can also rarely cause lactic acidosis, a serious complication. Sulfonylureas, another class of oral hypoglycemics, can increase the risk of hypoglycemia and weight gain. Thiazolidinediones can cause fluid retention and potentially exacerbate heart failure.
It’s important to note that the occurrence and severity of side effects vary among individuals and depend on several factors, including the specific medication, dose, and individual patient characteristics. Regular monitoring of blood sugar levels and patient education are essential to minimize these risks and promptly address any side effects that occur.
Q 20. Discuss the principles of infection control.
Infection control principles aim to prevent the transmission of infectious agents and protect both patients and healthcare workers. These principles revolve around several key elements:
- Hand hygiene: Frequent and thorough handwashing with soap and water or the use of alcohol-based hand rubs is crucial to eliminate microorganisms.
- Personal protective equipment (PPE): Using appropriate PPE (e.g., gloves, gowns, masks, eye protection) when interacting with potentially infectious patients or materials is essential to prevent contamination.
- Environmental cleaning and disinfection: Regularly cleaning and disinfecting surfaces and equipment reduces the microbial load and prevents the spread of infection.
- Sterilization and disinfection of medical instruments: Proper sterilization techniques are vital to eliminate all microorganisms from medical equipment.
- Waste management: Safe disposal of infectious waste prevents environmental contamination and protects healthcare workers.
- Respiratory hygiene/cough etiquette: Covering coughs and sneezes, and proper disposal of tissues, helps to prevent the airborne spread of infectious agents.
- Isolation precautions: Isolating patients with known or suspected infections helps to contain the spread of the infection to other patients and healthcare workers.
Adherence to these principles significantly reduces the risk of healthcare-associated infections (HAIs) and ensures a safe environment for patients and healthcare professionals.
Q 21. How do you communicate with patients and their families about difficult diagnoses?
Communicating difficult diagnoses to patients and their families requires sensitivity, empathy, and skillful communication. I begin by creating a private and comfortable setting, allowing ample time for the conversation. I use plain language, avoiding medical jargon, and ensure the patient and family understand the information. I start by acknowledging the emotional impact of the diagnosis.
I present the information in a clear and concise manner, focusing on the key points and addressing any questions or concerns. I actively listen to their responses, validating their feelings, and providing emotional support. I offer realistic hope and discuss available treatment options, outlining potential benefits and challenges.
I involve the patient in decision-making, respecting their autonomy and preferences. I collaborate with other healthcare professionals (e.g., social workers, chaplains) to provide comprehensive support and resource coordination. Following the initial discussion, I provide written materials summarizing the diagnosis and treatment plan. Regular follow-up appointments provide opportunities for ongoing communication and support. For instance, delivering a cancer diagnosis involves carefully explaining the type and stage, offering appropriate treatment options while acknowledging the emotional impact. A multidisciplinary approach including oncology, social work, and palliative care support is crucial.
Q 22. Explain your understanding of evidence-based medicine.
Evidence-based medicine (EBM) is the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients. It’s not simply about following the latest fad, but about integrating the best available research with clinical expertise and patient values.
This involves a systematic approach: formulating a clinical question (often using the PICO framework – Patient, Intervention, Comparison, Outcome), searching for relevant research (including randomized controlled trials, cohort studies, and meta-analyses), critically appraising the quality and validity of the evidence, and applying the findings to the specific patient context. Patient preferences and values are paramount, as EBM aims to find the best treatment for that individual patient, not just a statistically significant result.
For example, consider a patient with hypertension. EBM would guide me to consult clinical practice guidelines, review the evidence on various antihypertensive medications (e.g., ACE inhibitors, beta-blockers, calcium channel blockers), and consider the patient’s individual characteristics (age, comorbidities, other medications) to select the most appropriate and effective treatment, taking into account any potential side effects and the patient’s preferences.
Q 23. How do you stay updated on the latest advancements in medical treatment?
Staying updated in medicine requires a multifaceted approach. I regularly read peer-reviewed journals like the New England Journal of Medicine, The Lancet, and JAMA. I also attend conferences and workshops, participate in continuing medical education (CME) courses, and actively engage with online medical resources, including reputable websites and professional societies.
Furthermore, I subscribe to several medical newsletters and podcasts that curate the latest research and clinical guidelines. I actively participate in journal clubs with colleagues to discuss new findings and critically analyze research methodologies. This collaborative approach not only keeps me abreast of advancements but also fosters critical thinking and improves my clinical decision-making skills. Staying current isn’t just about reading articles; it’s a continuous process of learning, discussion, and reflection.
Q 24. Describe a time you had to make a critical decision under pressure.
During my residency, I encountered a patient presenting with sudden onset chest pain and shortness of breath. The initial ECG was inconclusive, but her clinical picture strongly suggested a pulmonary embolism (PE). Given the life-threatening nature of PE, immediate action was crucial. The pressure was immense, as a delay in diagnosis could have fatal consequences.
I quickly initiated appropriate supportive care (oxygen, monitoring), while simultaneously ordering a D-dimer test and a CT pulmonary angiography (CTPA) – the most definitive diagnostic test for PE. I had to weigh the potential risks and benefits of these tests, considering the time constraints and the patient’s clinical stability. The CTPA confirmed the PE, and prompt treatment with anticoagulation saved her life. This experience reinforced the importance of rapid assessment, decisive action, and a thorough understanding of critical care management in life-threatening situations.
Q 25. Describe your experience with interdisciplinary teamwork.
Interdisciplinary teamwork is fundamental to effective patient care. I’ve consistently collaborated with nurses, pharmacists, physiotherapists, social workers, and other specialists. For instance, in managing a patient with complex diabetes, I worked closely with a registered dietician to develop an individualized meal plan, with a diabetes educator to improve self-management skills, and with a physical therapist to improve mobility and exercise adherence. This collaborative approach ensures holistic care, addresses multiple needs simultaneously, and improves patient outcomes.
Effective teamwork requires clear communication, mutual respect, and a shared understanding of goals. I value the perspectives of other healthcare professionals and actively solicit their input in patient management. Open communication and a willingness to listen to different viewpoints are vital for achieving optimal patient outcomes.
Q 26. How do you handle difficult patients or family members?
Handling difficult patients or family members requires empathy, patience, and effective communication skills. I always start by actively listening to their concerns, validating their feelings, and ensuring they feel heard. I strive to understand their perspective, even if I don’t necessarily agree with it. I use clear and straightforward language, avoiding medical jargon whenever possible, to ensure transparency and understanding.
If communication remains challenging, I involve other members of the healthcare team, such as a social worker or a psychologist, to help mediate or provide additional support. Sometimes, setting clear boundaries and expectations is necessary, while maintaining a compassionate and respectful approach. The goal is always to de-escalate the situation, build rapport, and ensure that the patient’s medical needs are addressed effectively, while respecting the concerns of their family.
Q 27. Describe your experience with electronic health records (EHRs).
My experience with electronic health records (EHRs) is extensive. I utilize EHR systems daily for patient documentation, ordering tests, accessing medical history, and communicating with other healthcare providers. I’m proficient in using various EHR functionalities, including documenting progress notes, managing medication lists, and reviewing lab results. EHRs have significantly improved efficiency and streamlined workflows. They enable better coordination of care and ensure information is readily available to all involved in the patient’s care.
However, I also recognize the limitations. The time spent on documentation can sometimes detract from direct patient interaction. Furthermore, ensuring data accuracy and security is crucial. It’s important to use EHR systems efficiently and effectively, prioritizing patient care while recognizing both the benefits and drawbacks of this technology. Example of EHR entry: Progress Note - Patient presented with acute exacerbation of COPD. Oxygen saturation 88% on room air. Administered nebulized albuterol and ipratropium. Ordered chest x-ray.
Key Topics to Learn for Diagnosis and Treatment of Acute and Chronic Medical Conditions Interview
- Acute Condition Management: Understanding the rapid assessment and stabilization of patients presenting with acute conditions like myocardial infarction, stroke, or sepsis. This includes practical application of diagnostic tools and immediate treatment protocols.
- Chronic Disease Management: Developing comprehensive treatment plans for long-term conditions such as diabetes, hypertension, and asthma. This involves exploring patient education, medication management, and lifestyle modifications.
- Differential Diagnosis: Mastering the art of distinguishing between various conditions presenting with similar symptoms. Practice applying clinical reasoning and diagnostic algorithms to arrive at accurate diagnoses.
- Pharmacotherapeutics: Gaining a thorough understanding of drug mechanisms of action, indications, contraindications, adverse effects, and drug interactions relevant to acute and chronic conditions.
- Evidence-Based Medicine: Critically evaluating medical literature and applying research findings to clinical practice. This includes understanding the hierarchy of evidence and interpreting clinical trial data.
- Patient Communication & Collaboration: Practicing effective communication techniques for explaining diagnoses, treatment plans, and managing patient expectations. Understanding the importance of teamwork and collaboration within the healthcare setting.
- Ethical Considerations: Recognizing ethical dilemmas and applying ethical principles in the diagnosis and treatment of patients, including informed consent and end-of-life care.
- Health Maintenance and Preventative Care: Understanding strategies for preventing acute and chronic conditions, including risk factor modification and screening recommendations.
Next Steps
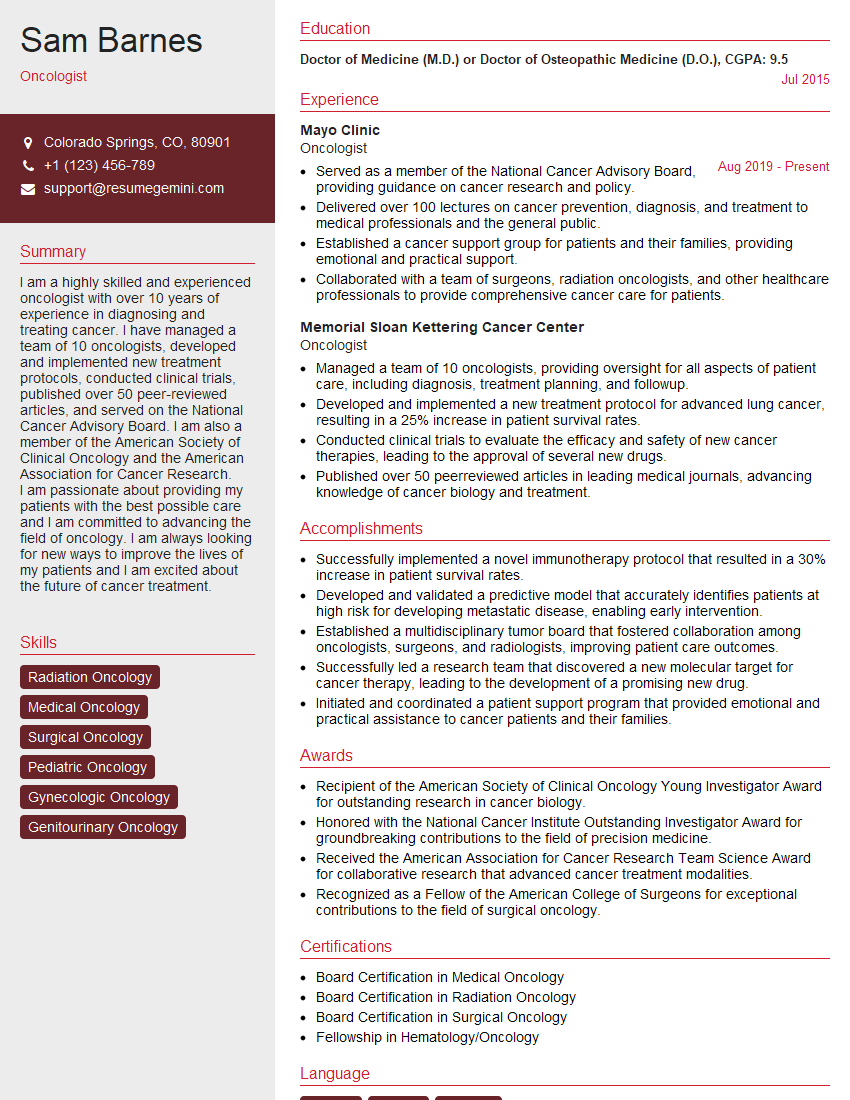
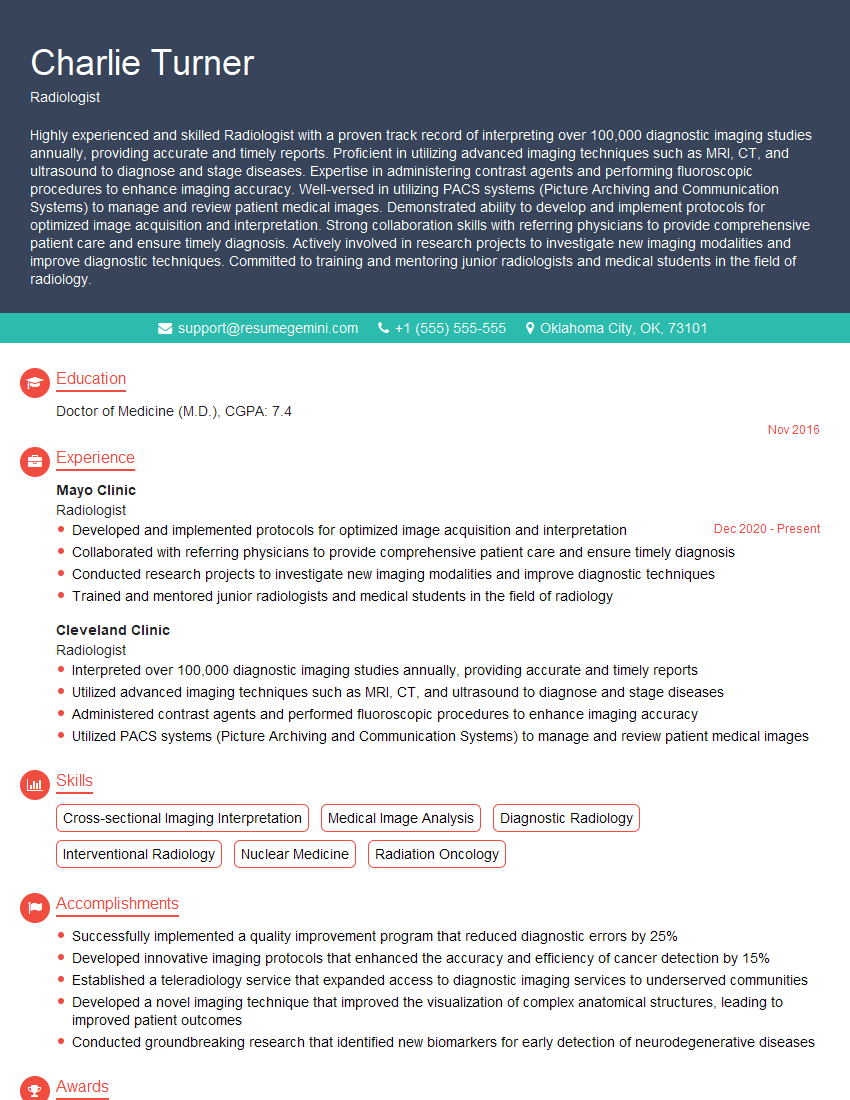
Mastering the diagnosis and treatment of acute and chronic medical conditions is crucial for career advancement in healthcare. A strong foundation in these areas demonstrates your competence and readiness for challenging roles. To significantly improve your job prospects, it’s essential to craft an ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource that can help you build a professional and impactful resume, ensuring your application stands out. Examples of resumes tailored to Diagnosis and Treatment of Acute and Chronic Medical Conditions are available to guide you through this process. Take the next step towards a successful career today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.