Feeling uncertain about what to expect in your upcoming interview? We’ve got you covered! This blog highlights the most important Diagnostic Audiometry interview questions and provides actionable advice to help you stand out as the ideal candidate. Let’s pave the way for your success.
Questions Asked in Diagnostic Audiometry Interview
Q 1. Describe the different types of hearing loss.
Hearing loss is categorized into various types based on the location and severity of the impairment. We broadly classify it as conductive, sensorineural, and mixed, each with its own characteristics and causes.
- Conductive Hearing Loss: This occurs when sound waves are blocked from reaching the inner ear. Think of it like a clogged drain – the sound can’t get through properly.
- Sensorineural Hearing Loss: This involves damage to the inner ear (cochlea) or the auditory nerve, which prevents the transmission of sound signals to the brain. It’s like a damaged phone line – the signal is distorted or lost.
- Mixed Hearing Loss: This is a combination of both conductive and sensorineural hearing loss. The sound is impaired both on its way to the inner ear and in the processing within the inner ear.
- Central Hearing Loss: This is less common and involves damage to the central auditory pathways in the brain that process sound.
The degree of hearing loss in each type can range from mild to profound, affecting an individual’s ability to hear various sounds and speech.
Q 2. Explain the procedure for performing pure-tone audiometry.
Pure-tone audiometry is a fundamental hearing test that measures the threshold of hearing at different frequencies. It helps determine the type, degree, and configuration of hearing loss. Here’s the procedure:
- Patient Preparation: The patient is seated in a sound-treated booth to minimize background noise. They are instructed on the procedure and asked about any relevant medical history.
- Headphone Placement: Headphones are placed over the ears, ensuring a proper seal to prevent sound leakage. We often use both insert earphones and supra-aural headphones depending on patient comfort and test needs.
- Tone Presentation: The audiologist presents pure tones (single frequencies) at various intensities (loudness levels) starting from inaudible levels and gradually increasing.
- Response Indication: The patient responds when they hear the tone by raising a hand, pressing a button, or another agreed-upon signal. We always check to make sure the patient understands before we begin.
- Threshold Determination: The threshold is the lowest intensity at which the patient consistently hears the tone at least 50% of the time. This process is repeated for various frequencies, typically ranging from 250 Hz to 8000 Hz. We test each ear separately.
- Audiogram Plotting: The results are plotted on an audiogram, a graph that displays hearing thresholds for each frequency and ear.
The entire process usually takes around 30-45 minutes, and it’s crucial to maintain a calm and communicative environment to ensure accurate results.
Q 3. What are the different types of hearing tests and when would you use each?
Several hearing tests are used in audiometry, each serving a specific purpose. The choice depends on the patient’s suspected problem and the information needed.
- Pure-tone audiometry: As explained earlier, this is the basic test to assess hearing sensitivity at different frequencies.
- Speech audiometry: This evaluates the ability to understand speech at different loudness levels. Tests include speech reception thresholds (SRT) and speech discrimination scores.
- Immittance testing: This assesses the middle ear function, including the eardrum’s mobility and the middle ear’s pressure. This helps distinguish between conductive and sensorineural hearing losses.
- Otoacoustic emissions (OAEs): These tests measure sounds emitted by the inner ear. They are useful for detecting cochlear dysfunction and are particularly helpful in newborns and young children.
- Auditory brainstem response (ABR): This electrophysiological test assesses the brainstem’s response to auditory stimuli. It’s helpful in diagnosing auditory neuropathy spectrum disorder and other neurological conditions affecting hearing.
- Tympanometry: This measures the mobility of the eardrum and the middle ear structures. It helps diagnose middle ear fluid, and other middle ear pathologies.
The selection of specific tests is often determined by the patient’s age, symptoms, and the audiologist’s clinical judgment. For example, OAEs are often used for newborn hearing screenings, while ABR might be employed when evaluating suspected neurological involvement.
Q 4. How do you interpret an audiogram?
Interpreting an audiogram involves analyzing the plotted data to identify the type, degree, and configuration of hearing loss. The audiogram shows hearing thresholds (in decibels) for different frequencies (in Hertz).
- Thresholds: Lower thresholds indicate better hearing; higher thresholds indicate poorer hearing.
- Shape of the curve: The pattern of the thresholds across frequencies provides insights into the type of hearing loss. For instance, a flat curve across all frequencies suggests a flat hearing loss, while a sloping curve may indicate a high-frequency hearing loss. A peaked curve could suggest noise-induced hearing loss.
- Air conduction (AC) and bone conduction (BC): The audiogram displays both air conduction (how well sound travels through the air to the inner ear) and bone conduction (how well sound travels directly to the inner ear, bypassing the outer and middle ear). Comparing AC and BC helps distinguish between conductive, sensorineural, and mixed hearing losses.
For example, a large air-bone gap (difference between AC and BC thresholds) suggests conductive hearing loss, while similar AC and BC thresholds with elevated values indicate sensorineural hearing loss.
Accurate interpretation necessitates understanding the anatomical and physiological basis of hearing and experience in correlating audiometric findings with clinical findings.
Q 5. Explain the difference between conductive, sensorineural, and mixed hearing loss.
The key difference lies in the location of the hearing impairment:
- Conductive Hearing Loss: Problem in the outer or middle ear. Sound waves can’t effectively travel to the inner ear. Imagine a partially blocked pipe – water (sound) struggles to flow through.
- Sensorineural Hearing Loss: Problem in the inner ear (cochlea) or auditory nerve. The sound waves reach the inner ear, but the signals aren’t properly processed or transmitted to the brain. This is like a faulty telephone receiver – you can hear the sound, but it’s distorted or unclear.
- Mixed Hearing Loss: Combination of both conductive and sensorineural hearing loss. There are issues in both the outer/middle ear and the inner ear/auditory nerve. Think of a partially blocked pipe with a faulty tap at the other end.
This distinction is crucial for determining appropriate treatment. Conductive loss is often treatable with medical or surgical interventions addressing the outer or middle ear issue, while sensorineural loss often requires management strategies like hearing aids or cochlear implants.
Q 6. What are the common causes of conductive hearing loss?
Conductive hearing loss results from problems interfering with sound wave transmission to the inner ear. Common causes include:
- Earwax buildup (cerumen impaction): Excessive earwax can block the ear canal, preventing sound waves from reaching the eardrum.
- Otitis media (middle ear infection): Fluid buildup in the middle ear caused by infection can impair the vibration of the ossicles (tiny bones in the middle ear).
- Otosclerosis: A bone disorder affecting the ossicles, causing them to stiffen and reduce their ability to vibrate.
- Foreign body in the ear canal: Objects lodged in the ear canal obstruct sound wave transmission.
- Perforated eardrum: A hole in the eardrum can disrupt sound wave transmission to the middle ear.
Many cases of conductive hearing loss are treatable through medical intervention, such as earwax removal, treatment of infection, or surgery.
Q 7. What are the common causes of sensorineural hearing loss?
Sensorineural hearing loss stems from damage to the inner ear (cochlea) or auditory nerve. Causes are diverse and can include:
- Aging (presbycusis): Age-related hearing loss is a common form of sensorineural hearing loss, affecting high frequencies initially.
- Noise-induced hearing loss (NIHL): Prolonged exposure to loud noises, especially in occupational settings, can damage the delicate hair cells in the cochlea.
- Genetic factors: Some forms of hearing loss have a genetic basis, inherited from parents.
- Ototoxic medications: Certain medications, such as some antibiotics and chemotherapy drugs, can be damaging to the inner ear.
- Infections: Viral infections such as measles, mumps, and rubella can damage the inner ear.
- Head trauma: Severe head injuries can damage the inner ear structures or the auditory nerve.
Treatment for sensorineural hearing loss often focuses on managing the condition through hearing aids, cochlear implants, or assistive listening devices. Prevention is crucial, especially regarding noise exposure.
Q 8. Describe the different types of hearing aids and their suitability for various types of hearing loss.
Hearing aids are categorized based on their style and technology. The best fit depends on the individual’s hearing loss type, degree, and lifestyle.
- Behind-the-Ear (BTE): These are the most common type, suitable for all degrees of hearing loss, particularly for those with significant hearing loss or who need powerful amplification. They are durable and easy to maintain. A common example is a BTE aid with a thin tube connecting to an earmold that sits in the ear canal.
- In-the-Ear (ITE): These custom-made devices fit completely inside the outer ear and are suitable for mild to moderately severe hearing loss. They offer better cosmetic appeal than BTEs.
- In-the-Canal (ITC): Smaller than ITEs, these fit deeper into the ear canal and are suitable for mild to moderate hearing loss. They provide more discretion than ITEs but may be less durable.
- Completely-in-Canal (CIC): These are the smallest type, almost invisible, suitable only for mild to moderate hearing loss. They are less powerful than other styles and require more dexterity to handle.
- Invisible-in-Canal (IIC): These are even smaller than CICs and are completely hidden within the ear canal. They are the most discreet option, but also the least powerful and least durable.
Suitability for various hearing losses:
For mild to moderate losses, ITC, CIC, or IIC may be appropriate. For moderate to severe losses, BTE or ITE are typically preferred. The audiologist will consider factors like the shape of the ear canal and the individual’s dexterity when recommending the most suitable style.
Q 9. How do you counsel patients about their hearing loss and treatment options?
Counseling patients involves a sensitive and empathetic approach. It’s crucial to start by acknowledging their feelings and concerns regarding the diagnosis. I explain their hearing loss in simple terms, using analogies to help them understand the impact on their daily life. For example, I might explain that a high-frequency loss is like missing the high notes in a song, making speech understanding difficult in noisy environments.
I explain available treatment options, including hearing aids, assistive listening devices (ALDs) like amplified telephones or TV listeners, and strategies like speechreading. I present the pros and cons of each option, emphasizing that the best choice depends on their individual needs, budget, and lifestyle. Realistic expectations are also crucial. I emphasize that hearing aids won’t restore hearing to normal, but rather improve access to sound and speech. Follow-up appointments are scheduled to address any adjustments needed and to monitor the patient’s progress and satisfaction. Often, I will connect the patient with support groups to address the emotional aspect of dealing with hearing loss.
Q 10. Explain the importance of speech audiometry.
Speech audiometry is crucial because it assesses how well a person understands speech in various listening conditions. Pure-tone audiometry measures hearing sensitivity, but it doesn’t tell the whole story. Speech audiometry helps determine the impact of a hearing loss on communication and guides treatment decisions. For example, a person might have a mild hearing loss on a pure-tone test, but speech audiometry could reveal significant difficulty understanding speech in noise.
Q 11. What are the different types of speech audiometry tests?
Several speech audiometry tests provide different aspects of speech understanding:
- Speech Reception Threshold (SRT): This measures the lowest intensity at which a person can understand 50% of spoken words (usually spondees – two-syllable words with equal stress on each syllable, e.g., ‘baseball’).
- Word Recognition Score (WRS): This measures the percentage of words a person can correctly identify at a comfortable listening level. This helps determine the clarity of hearing and can pinpoint the frequency region where understanding breaks down.
- Speech in Noise Tests: These assess the ability to understand speech in the presence of background noise, such as the QuickSIN (Quick Speech-in-Noise) test. This is crucial as it reflects real-world listening situations.
The choice of test depends on the patient’s age, communication needs, and the suspected nature of their hearing loss.
Q 12. How do you perform and interpret tympanometry?
Tympanometry is an objective test that assesses the middle ear function by measuring the impedance (resistance to energy flow) of the eardrum and middle ear structures.
Procedure: A small probe is placed in the ear canal. This probe delivers a tone and measures the sound reflected back from the eardrum. The pressure in the ear canal is changed systematically, and the amount of sound reflected is plotted against pressure. This creates a tympanogram, a graph showing the ear’s response to changing pressure.
Interpretation: A normal tympanogram shows a peak at a pressure near atmospheric pressure, indicating a healthy, mobile eardrum and middle ear system. Abnormal patterns can indicate problems such as middle ear fluid (otitis media), eardrum perforation, or ossicular chain dysfunction. For example, a flat tympanogram suggests the presence of fluid in the middle ear.
Q 13. What are the different types of otoacoustic emissions (OAEs) tests?
Otoacoustic emissions (OAEs) are faint sounds produced by the inner ear’s hair cells. Their presence indicates healthy outer hair cell function. There are two main types of OAE tests:
- Transient Evoked Otoacoustic Emissions (TEOAEs): These are elicited by brief clicks or tone pips. They reflect the overall health of the cochlea.
- Distortion Product Otoacoustic Emissions (DPOAEs): These are produced by presenting two pure tones to the ear. They provide more specific information about the functioning of the outer hair cells in certain frequency regions.
Q 14. How do you interpret OAEs results?
The presence of OAEs generally suggests normal outer hair cell function and a healthy cochlea, particularly useful in detecting hearing loss in newborns and infants before behavioral testing is possible. The absence of OAEs, however, is not always conclusive. Factors such as middle ear pathology or sensorineural hearing loss can also suppress OAEs. Therefore, OAE results are always considered in conjunction with other audiological findings, such as pure-tone audiometry and speech audiometry. A detailed clinical picture helps the audiologist accurately interpret the results and diagnose the underlying condition.
Q 15. Explain the purpose of acoustic reflexes testing.
Acoustic reflex testing assesses the stapedius muscle’s involuntary contraction in response to intense sounds. This contraction, mediated by the brainstem, stiffens the ossicular chain in the middle ear, reducing sound transmission. The test helps identify the integrity of the auditory pathway from the middle ear to the brainstem.
Clinically, we use a probe containing a loudspeaker and a sensor to measure the change in impedance (resistance to sound) in the middle ear. A loud sound stimulus is presented, and the presence or absence of a reflex contraction is noted. Absent or asymmetrical reflexes may indicate pathology in the middle ear, inner ear, auditory nerve, or brainstem. For instance, an absent reflex on one side with a normal reflex on the other could suggest a problem like a tumor affecting the brainstem or auditory nerve on the affected side.
Think of it like testing a reflex hammer on your knee – a normal response indicates a healthy pathway. Similarly, a normal acoustic reflex suggests a healthy auditory pathway up to the brainstem.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe the procedure for performing auditory brainstem response (ABR) testing.
Auditory Brainstem Response (ABR) testing is an electrophysiological test that measures the electrical activity in the auditory pathway in response to sound. It’s incredibly useful for identifying auditory neuropathy and other conditions affecting the auditory brainstem.
The procedure involves placing small electrodes on the scalp, usually near the ear and forehead. Click or tone burst stimuli are presented through earphones, and the resulting electrical activity is recorded. The process is painless and usually takes 30-45 minutes. The recorded waveforms represent the electrical activity of different parts of the auditory pathway: cochlea, auditory nerve, brainstem. We analyze wave latencies (time taken for signal to reach different points) and amplitudes to ascertain whether the pathway is functioning properly.
For example, a prolonged wave V latency could suggest a lesion along the auditory pathway, such as demyelination in multiple sclerosis.
Q 17. How do you interpret ABR results?
Interpreting ABR results involves careful analysis of the recorded waveforms, specifically focusing on wave latencies and amplitudes. Normal ABRs show distinct waves with characteristic latencies. Any deviations from these norms can indicate pathology.
We look for:
- Waveform Morphology: Presence, absence, and shape of individual waves (I-V).
- Wave Latencies: Absolute latencies (time taken for each wave to appear) and interpeak latencies (time between waves). Significant delays might indicate a problem in transmission speed in the pathway.
- Wave Amplitudes: Reduced amplitude could suggest decreased neural activity, for instance, caused by auditory neuropathy.
- Symmetry: Comparing the responses from both ears. Asymmetry suggests unilateral pathology.
The interpretation is not solely based on numbers but involves integrating the ABR findings with the patient’s clinical history and other test results. For example, a child with normal hearing thresholds but an abnormal ABR might have auditory neuropathy, where the hearing nerve cannot effectively send signals to the brain.
Q 18. What are the common challenges in performing pediatric audiometry?
Pediatric audiometry presents unique challenges due to children’s limited cooperation, varying developmental levels, and communication skills. Some common challenges include:
- Maintaining Attention: Keeping young children focused during testing can be difficult. They may become distracted easily.
- Behavioral Responses: It can be hard to differentiate between true hearing loss and a child’s unwillingness to respond to the stimulus.
- Communication Barriers: Accurate interpretation of responses is challenging with non-verbal children.
- Middle Ear Infections: Frequent middle ear infections common in young children can affect test results.
We need to use age-appropriate techniques, including play audiometry, visual reinforcement audiometry, and conditioned play audiometry. Sometimes, sedation is required for accurate assessment.
Q 19. How do you adapt your testing approach for different age groups?
Adapting testing approaches for different age groups requires a flexible strategy. We utilize different techniques depending on the child’s developmental stage and communication skills.
- Infants (0-6 months): Primarily use ABR and otoacoustic emissions (OAEs) – objective tests that don’t rely on the child’s cooperation.
- Toddlers (6 months – 3 years): Conditioned play audiometry, where the child is rewarded for responding to sounds, often with toys or verbal praise, is crucial.
- Preschoolers (3-5 years): Play audiometry can still be employed; however, conventional behavioral tests might also be possible with good cooperation.
- School-aged children (5+ years): Standard adult audiometric procedures can be used, although it is crucial to engage them and provide clear, age-appropriate instructions.
This flexible approach ensures we get the most reliable results and adapt to the child’s individual needs.
Q 20. Explain the role of assistive listening devices.
Assistive listening devices (ALDs) are tools that help individuals with hearing loss overcome environmental barriers to communication. They enhance signal-to-noise ratio and improve speech audibility.
Examples include:
- Hearing aids: Amplify sound to compensate for hearing loss.
- FM systems: Transmit the speaker’s voice directly to the listener’s hearing aid or a receiver.
- Loop systems: Use magnetic loops to transmit sound directly to hearing aids with a telecoil feature.
- Personal amplification devices: Portable devices that amplify sounds from various sources.
ALDs are critical in improving communication in various settings, such as classrooms, workplaces, and social gatherings. They significantly enhance quality of life for people with hearing impairments.
Q 21. Describe your experience with different audiometric equipment.
Throughout my career, I’ve had extensive experience with a wide range of audiometric equipment from various manufacturers. My expertise covers both traditional and modern devices. I’m proficient in using audiometers for pure-tone audiometry, speech audiometry, and immittance testing. This includes equipment for performing ABR and OAEs, as well as specialized equipment for pediatric audiometry. I’m also familiar with different software packages used for data analysis and report generation. I stay current with technological advancements and regularly attend professional development sessions on new equipment and methodologies to ensure that I am delivering the best possible patient care using the most advanced and appropriate technology.
For instance, my experience includes working with various brands of audiometers, including [mention specific brands if comfortable], with a deep understanding of their calibration procedures and troubleshooting. This allows me to provide high-quality, reliable results to patients and ensure our equipment always operates at peak performance.
Q 22. How do you maintain and troubleshoot audiometric equipment?
Maintaining and troubleshooting audiometric equipment is crucial for accurate and reliable test results. It involves a multi-faceted approach encompassing daily checks, preventative maintenance, and systematic troubleshooting.
- Daily Checks: Before each patient session, I perform a series of checks. This includes verifying the calibration of the audiometer using a known-good acoustic calibrator, ensuring proper functionality of the earphones and inserts, and checking the integrity of the sound-booth’s acoustic seal. Any inconsistencies are immediately addressed.
- Preventative Maintenance: Regular preventative maintenance is key. This involves periodic servicing by qualified technicians, cleaning of equipment components (e.g., earphones, transducers), and replacement of worn parts as recommended by the manufacturer. Detailed records are kept for every maintenance activity.
- Troubleshooting: When problems arise, a systematic approach is essential. For instance, if a pure-tone audiometry test yields inconsistent results, I would first check the calibration, then examine the earphones for damage or proper placement in the patient’s ears. I’d also consider the patient’s cooperation and potential external noise interference. If the problem persists, I’d consult the manufacturer’s troubleshooting guide or seek assistance from a qualified technician.
Think of it like maintaining a finely tuned instrument – regular care ensures accurate readings and prevents costly repairs down the line. Ignoring these steps can lead to inaccurate diagnoses and compromised patient care.
Q 23. What are the ethical considerations in diagnostic audiometry?
Ethical considerations in diagnostic audiometry are paramount. They center on ensuring patient well-being, providing informed consent, maintaining confidentiality, and upholding professional standards.
- Informed Consent: Patients must fully understand the purpose, procedures, and potential risks and benefits of any audiological test before proceeding. This includes explaining the results in a clear and understandable way, even if the results are difficult to convey.
- Confidentiality: Patient information is highly sensitive. I strictly adhere to confidentiality protocols, ensuring all patient data is protected from unauthorized access or disclosure. This is particularly critical given the sensitive nature of hearing loss and its potential impact on a person’s quality of life.
- Competence: I only perform tests within my scope of competence. Referring complex cases to specialists, if necessary, is an ethical imperative. This ensures patients receive the best possible care.
- Objectivity: Maintaining objectivity is crucial. Personal biases should never influence test interpretation or recommendations. This prevents inaccurate diagnoses and treatment plans.
- Accurate Reporting: Test results must be accurately documented and reported. Honest and transparent communication with patients and referring physicians is essential.
Ethical practice builds trust with patients and contributes to a positive professional reputation.
Q 24. How do you ensure patient confidentiality and HIPAA compliance?
Ensuring patient confidentiality and HIPAA compliance is an absolute necessity. My practice adheres strictly to all HIPAA regulations.
- Data Security: Patient information is stored securely using encrypted electronic health records (EHRs) and password-protected computer systems. Physical files are kept in locked cabinets in a secure location.
- Access Control: Access to patient data is strictly limited to authorized personnel on a need-to-know basis. Each individual has unique login credentials, and access is monitored.
- Patient Authorization: Patient authorization is obtained before releasing any information to third parties, except where legally required (e.g., reporting to a referring physician).
- HIPAA Training: I regularly undergo HIPAA compliance training to stay up-to-date on the latest regulations and best practices. This ensures that our office consistently meets or exceeds the legal requirements for protecting sensitive patient information.
- Data Breach Protocol: We have a comprehensive data breach protocol in place that outlines steps to be taken in the event of a security incident. This ensures prompt identification, containment, and remediation of potential breaches.
Maintaining patient privacy is not just a legal obligation; it’s a fundamental ethical responsibility. A breach of confidentiality can have severe consequences for both the patient and the healthcare provider.
Q 25. Describe a situation where you had to troubleshoot a difficult audiometric test.
I once encountered a patient who exhibited inconsistent results during speech audiometry. She consistently scored significantly better on phonetically balanced sentence tests compared to monosyllabic word recognition tests. This discrepancy suggested a possible central auditory processing disorder rather than simply a peripheral hearing loss.
To troubleshoot this, I first re-administered the tests, paying close attention to patient comfort and minimizing background noise. I then employed different testing modalities, such as dichotic listening tests and speech-in-noise testing. These alternative tests helped isolate the potential for central processing deficits.
The results confirmed a central auditory processing disorder contributing to her speech perception difficulties. This case highlighted the importance of a thorough assessment using a range of tests and the need to consider central auditory processing when interpreting speech audiometry results. The patient was then referred to a specialist for further evaluation and therapy.
Q 26. How do you stay current with the latest advancements in diagnostic audiometry?
Staying current with advancements in diagnostic audiometry is crucial for providing optimal patient care. I employ several strategies to achieve this.
- Professional Organizations: Active membership in professional organizations like the American Academy of Audiology (AAA) provides access to journals, continuing education courses, and conferences featuring cutting-edge research and clinical practices. I regularly attend conferences and webinars.
- Peer-Reviewed Journals: I subscribe to and regularly read peer-reviewed journals focusing on audiology and related fields. This allows me to stay abreast of the latest research findings and clinical studies.
- Continuing Education: I participate in continuing education courses and workshops to update my knowledge and skills on new technologies, diagnostic techniques, and treatment approaches. Maintaining my professional certifications keeps me current and up-to-date.
- Online Resources: I utilize reputable online resources and databases to access research articles, clinical guidelines, and information on new equipment and software.
Continuous learning is essential for maintaining a high level of expertise in this rapidly evolving field.
Q 27. Explain your understanding of the relationship between audiology and other medical specialties.
Audiology has strong interdisciplinary relationships with various medical specialties. Understanding these connections is vital for comprehensive patient care.
- Otolaryngology (ENT): Close collaboration with ENT specialists is essential, as many hearing problems are related to ear diseases and require medical intervention. We frequently work together to diagnose and manage conditions such as otitis media, cholesteatoma, and Meniere’s disease.
- Neurology: Audiologists often work with neurologists to assess and manage auditory neuropathies and central auditory processing disorders which can be linked to neurological conditions.
- Pediatrics: In pediatric audiology, collaboration with pediatricians is crucial for early identification and management of hearing loss in infants and children. Early detection is paramount for optimal development.
- Geriatric Medicine: Age-related hearing loss (presbycusis) is very common. We frequently collaborate with geriatricians to ensure that our elderly patients receive appropriate hearing aids and support services.
- Speech-Language Pathology: Speech-language pathologists and audiologists work closely together when managing communication difficulties related to hearing impairment.
Effective interprofessional collaboration improves the quality of patient care by providing holistic assessment and management strategies.
Q 28. Describe your experience with electronic health records (EHRs) in audiology.
My experience with electronic health records (EHRs) in audiology has been overwhelmingly positive. EHR systems have significantly improved efficiency and streamlined workflows within our practice.
- Improved Efficiency: EHRs allow for quick access to patient history, test results, and treatment plans. This eliminates the need for searching through paper files, saving valuable time and improving efficiency.
- Enhanced Communication: EHRs facilitate seamless communication with referring physicians and other healthcare providers. Secure messaging and shared data exchange enhance coordination of care.
- Data Analysis & Research: EHRs allow for easier data analysis and research, providing valuable insights into patient populations and treatment outcomes. This data can be used to improve practice efficiency and patient care.
- Improved Documentation: EHRs provide a structured format for documentation, reducing the risk of errors and ensuring comprehensive records. The ability to easily generate reports and summaries is extremely beneficial.
- Patient Portal: Many EHRs include patient portals that allow patients to access their medical records and communicate securely with providers, empowering patients with their health information.
However, a successful EHR implementation requires proper training and ongoing support. Overcoming the initial learning curve and adapting to new workflows are necessary for maximizing the benefits of EHR systems.
Key Topics to Learn for Diagnostic Audiometry Interview
- Pure-Tone Audiometry: Understanding the principles, procedures, and interpretation of air and bone conduction thresholds. Practical application: Diagnosing conductive, sensorineural, and mixed hearing losses.
- Speech Audiometry: Mastering speech reception thresholds (SRT), speech discrimination scores (SDS), and their clinical significance. Practical application: Assessing the impact of hearing loss on speech understanding.
- Immittance Testing: Thorough knowledge of tympanometry, acoustic reflexes, and their interpretation in identifying middle ear pathology. Practical application: Differentiating between conductive and sensorineural hearing loss.
- Otoacoustic Emissions (OAEs): Understanding the principles and clinical applications of OAEs in identifying cochlear dysfunction. Practical application: Early detection of hearing loss in infants and screening for auditory pathology.
- Auditory Brainstem Response (ABR): Knowledge of ABR principles, recording techniques, and interpretation for diagnosing auditory neuropathy and retrocochlear pathology. Practical application: Assessing the integrity of the auditory pathway.
- Hearing Loss Classification and Management: Familiarity with different types of hearing loss, their causes, and appropriate management strategies. Practical application: Developing individualized rehabilitation plans.
- Patient Communication and Counseling: Effective strategies for communicating complex audiological information to patients and their families. Practical application: Building rapport and ensuring patient understanding.
- Equipment Operation and Maintenance: Understanding the functionality and maintenance of audiometric equipment. Practical application: Troubleshooting common equipment issues and ensuring accurate test results.
- Ethical Considerations in Audiology: Awareness of ethical guidelines and professional responsibilities in audiological practice. Practical application: Making sound clinical judgments while adhering to ethical standards.
Next Steps
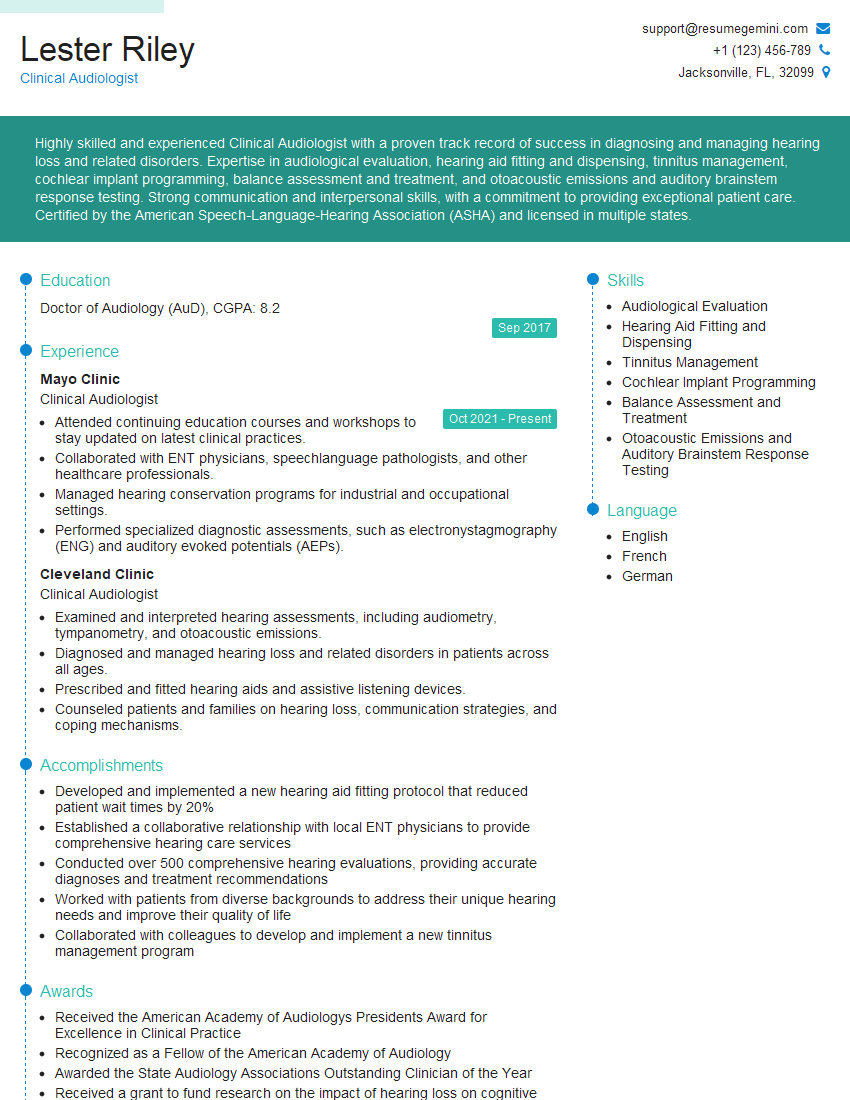
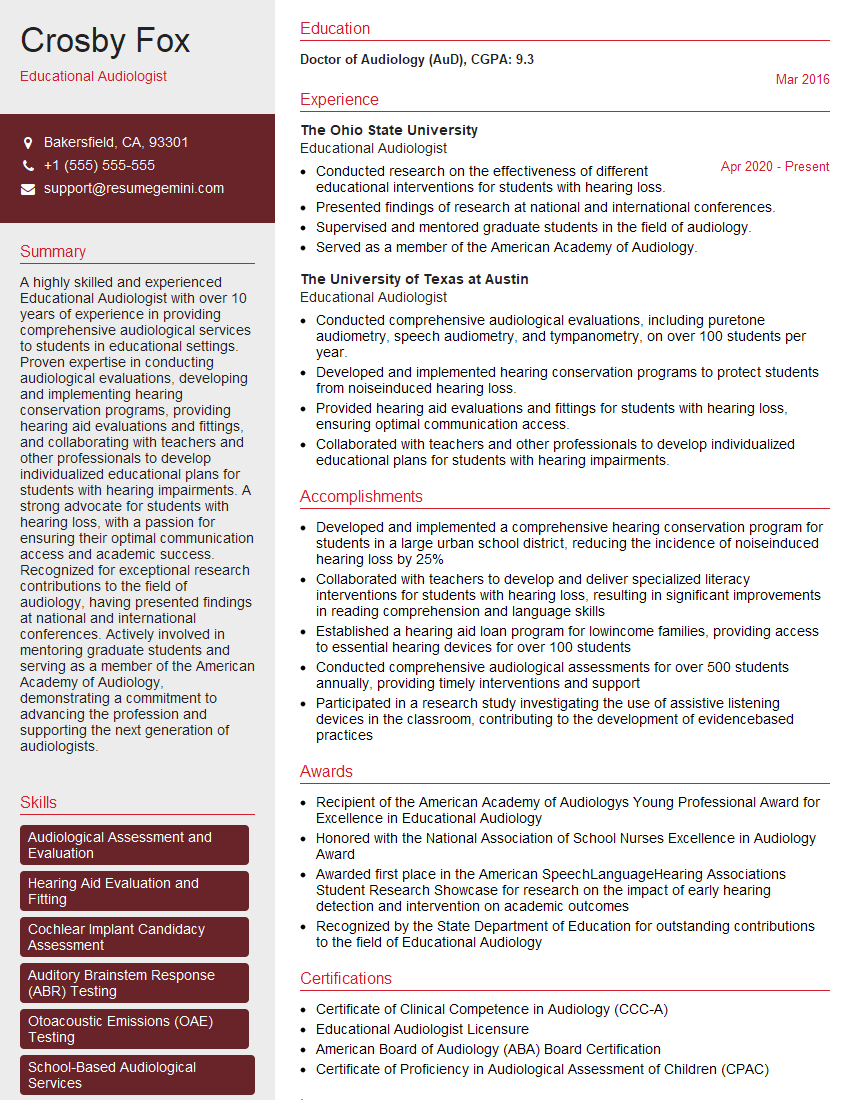
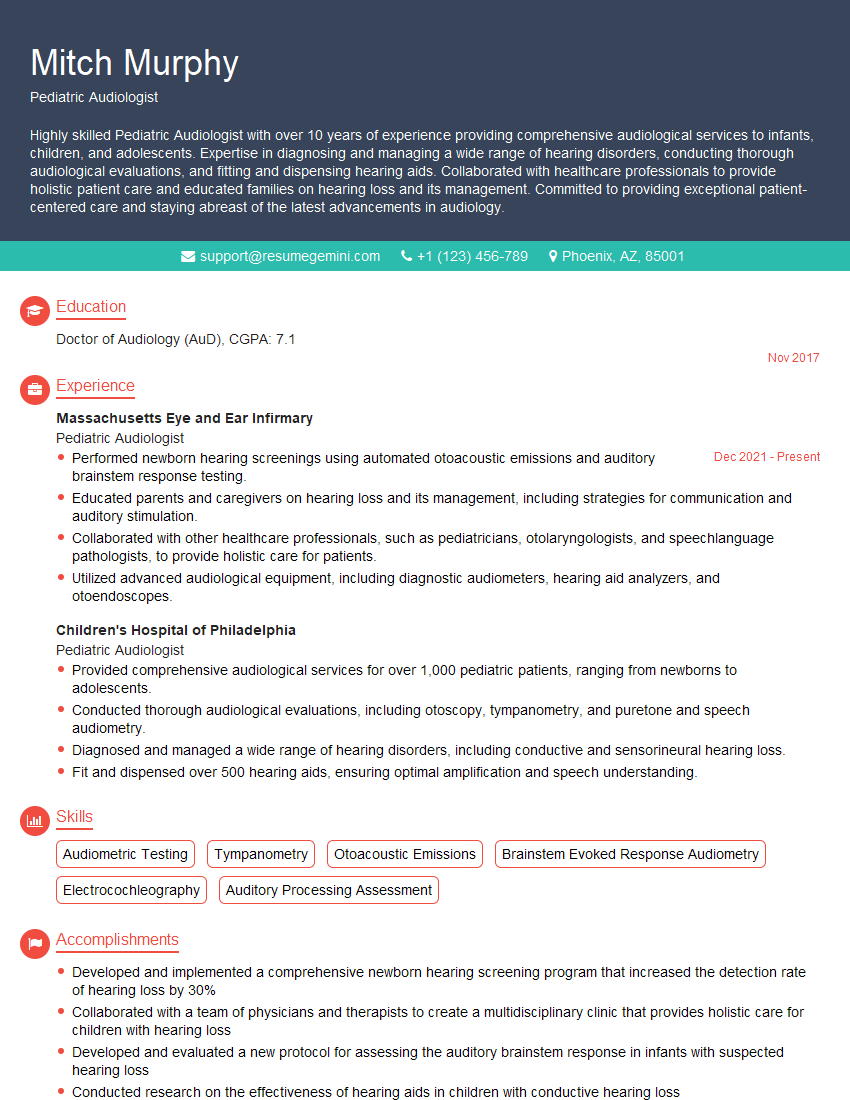
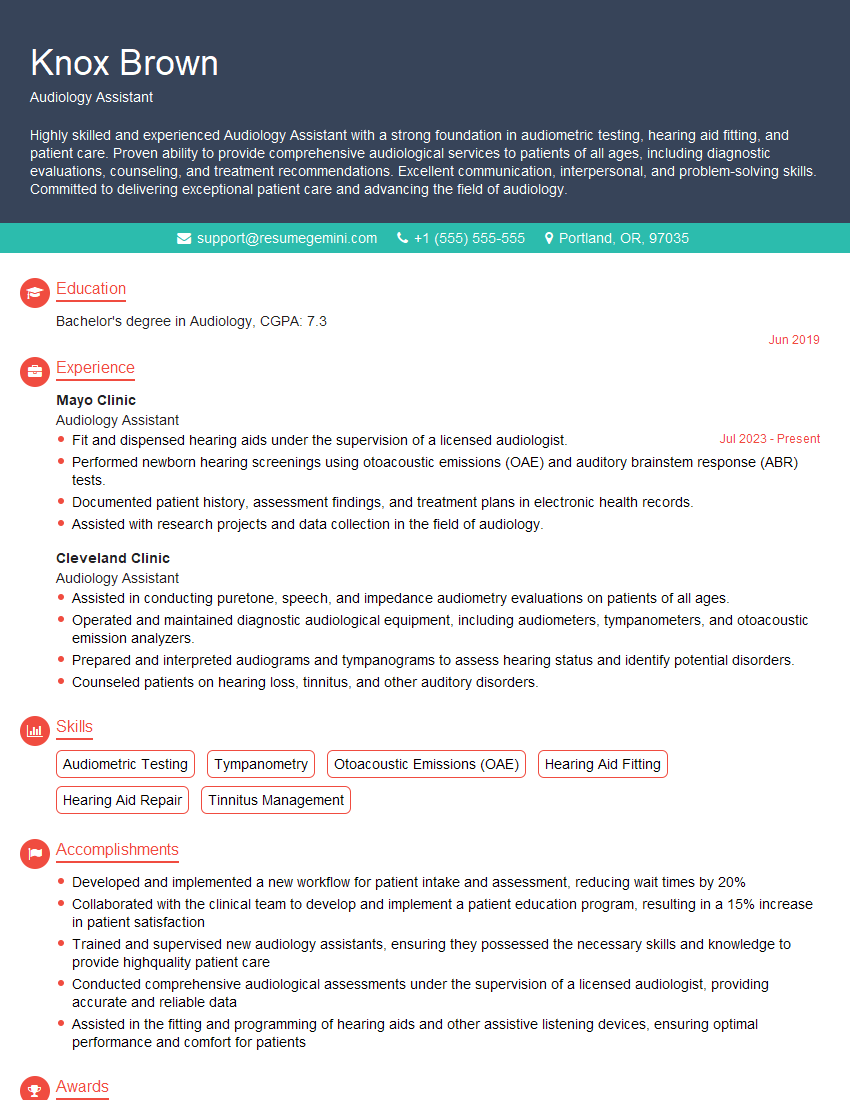
Mastering Diagnostic Audiometry is crucial for a successful and rewarding career in audiology, opening doors to diverse opportunities and professional growth. A strong resume is your key to unlocking these opportunities. Creating an ATS-friendly resume is essential for getting your application noticed by potential employers. To elevate your resume and significantly increase your chances of landing your dream job, we strongly recommend using ResumeGemini. ResumeGemini provides a user-friendly platform and offers examples of resumes tailored specifically to Diagnostic Audiometry professionals, helping you present your skills and experience in the best possible light.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.