Interviews are opportunities to demonstrate your expertise, and this guide is here to help you shine. Explore the essential Diagnostic Evaluation interview questions that employers frequently ask, paired with strategies for crafting responses that set you apart from the competition.
Questions Asked in Diagnostic Evaluation Interview
Q 1. Explain the difference between sensitivity and specificity in diagnostic testing.
Sensitivity and specificity are two crucial metrics used to evaluate the performance of a diagnostic test. Think of it like this: you have a test that screens for a disease. Sensitivity refers to the test’s ability to correctly identify individuals who actually have the disease (true positives). A highly sensitive test means very few people with the disease will test negative (false negatives). Specificity, on the other hand, measures the test’s ability to correctly identify individuals who do not have the disease (true negatives). A highly specific test means very few people without the disease will test positive (false positives).
Let’s use a blood test for a particular infection as an example. A highly sensitive test will rarely miss someone who is infected. Conversely, a highly specific test will rarely label someone as infected when they are actually healthy. The ideal diagnostic test would have both high sensitivity and high specificity, but this is not always achievable in practice. Often, there’s a trade-off: increasing sensitivity might decrease specificity and vice versa. The choice between prioritizing sensitivity or specificity depends on the clinical context and the consequences of false positives versus false negatives.
Q 2. Describe the process of evaluating the accuracy of a new diagnostic test.
Evaluating a new diagnostic test involves a rigorous process that typically includes several stages. First, a well-defined study population needs to be recruited, ensuring it represents the target population for the test. This population is then divided into two groups: those with the condition (cases) and those without the condition (controls).
Next, the new diagnostic test is administered to both groups. The results are then compared to a gold standard test – the most accurate existing test for the condition – to determine the number of true positives, true negatives, false positives, and false negatives. Using these values, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) are calculated. These metrics provide a comprehensive assessment of the test’s accuracy. The entire process needs to follow strict quality control measures to avoid bias and ensure reliable results. Finally, these findings are typically peer-reviewed and published to contribute to the body of medical knowledge.
Q 3. How do you interpret a receiver operating characteristic (ROC) curve?
A receiver operating characteristic (ROC) curve is a graphical representation of a diagnostic test’s performance across various threshold settings. The curve plots the true positive rate (sensitivity) against the false positive rate (1-specificity) for all possible thresholds. The area under the curve (AUC) provides a single summary measure of the test’s overall diagnostic accuracy.
An AUC of 1 represents a perfect test, while an AUC of 0.5 indicates a test no better than chance. Generally, an AUC above 0.9 is considered excellent, 0.8 good, 0.7 fair, and below 0.7 poor. The ROC curve helps clinicians visualize the trade-off between sensitivity and specificity. By examining the curve, one can determine the optimal threshold that balances the benefits and risks associated with false positives and false negatives based on the clinical context. For example, a high sensitivity threshold might be preferred for screening tests where missing cases is highly undesirable.
Q 4. What are the limitations of using a single diagnostic test?
Relying on a single diagnostic test can lead to several limitations. No single test is perfect, and they all have inherent limitations in sensitivity and specificity. Using just one test increases the risk of misdiagnosis due to either false positive or false negative results. For instance, a negative test result from a test with low sensitivity could lead to a missed diagnosis, while a positive result from a test with low specificity could result in unnecessary treatment or further investigations.
Furthermore, different tests may have different strengths and weaknesses. Combining multiple tests can provide a more complete and accurate picture. Consider the diagnosis of a heart condition. Electrocardiograms, echocardiograms, blood tests, and even clinical examination may all be needed to arrive at a confident diagnosis. The combination allows for a more comprehensive assessment, reducing the impact of any individual test’s limitations and increasing the overall diagnostic confidence.
Q 5. Discuss the importance of pre-analytical factors in diagnostic testing.
Pre-analytical factors are critical and often overlooked. They encompass all steps taken before the actual testing process, including patient preparation, sample collection, handling, and storage. These factors can significantly impact test results, potentially leading to inaccurate diagnoses. Examples include improper fasting before a blood glucose test (resulting in falsely elevated levels), inadequate sample mixing (leading to uneven concentrations), or incorrect storage temperatures (causing degradation of analytes).
To ensure accurate results, strict adherence to standardized protocols is crucial. This includes detailed instructions to patients on sample collection (e.g., timing of blood draw, proper collection containers), meticulous training of healthcare professionals on proper techniques, and use of appropriate sample containers and storage equipment. Failure to control pre-analytical variables can easily introduce errors, leading to potentially incorrect interpretations and treatment decisions. It is, therefore, extremely crucial to ensure high quality and standardized procedures before the analysis begins.
Q 6. How do you handle a discrepancy between different diagnostic tests?
Discrepancies between different diagnostic tests are common. This situation requires a systematic approach. First, one should carefully review the individual test results, noting their sensitivity, specificity, and the circumstances under which they were performed. Are there known limitations or potential interferences associated with a particular test? Also, assessing the patient’s clinical presentation, other relevant symptoms, and medical history is important.
Next, it might be necessary to repeat the discordant tests to rule out analytical errors. Additionally, considering further investigations, such as performing more specific tests or consulting with specialists, might be necessary. For example, if a chest X-ray suggests pneumonia but a blood test for bacterial infection is negative, further investigations like a sputum culture or CT scan could clarify the situation. The ultimate goal is to reconcile the conflicting results and reach the most accurate diagnosis based on the available evidence.
Q 7. Explain the concept of positive and negative predictive values.
Positive and negative predictive values are measures that reflect the probability of a true positive or a true negative based on a positive or negative test result, respectively. Positive predictive value (PPV) represents the probability that a patient with a positive test result actually has the disease. Negative predictive value (NPV) represents the probability that a patient with a negative test result is truly disease-free.
Let’s imagine a scenario with a screening test for a rare disease. Even if the test has high specificity, a positive result might not be as meaningful due to the low prevalence of the disease – the probability of a true positive among all positive results is low. This is the PPV. Conversely, a negative result from a highly sensitive test is more reassuring. In this context, the NPV will be high, indicating that a negative result reliably indicates the absence of the disease. Both PPV and NPV are heavily influenced by the prevalence of the disease in the population being tested.
Q 8. What are the ethical considerations in using diagnostic tests?
Ethical considerations in diagnostic testing are paramount, ensuring patient well-being and rights are prioritized above all else. These considerations encompass several key areas:
- Informed Consent: Patients must fully understand the purpose, benefits, risks, and alternatives to a test before undergoing it. This includes potential side effects, cost implications, and the uncertainty inherent in some tests.
- Confidentiality: Patient data must be protected, adhering to strict privacy regulations like HIPAA (in the US) and GDPR (in Europe). Unauthorized disclosure is a serious breach of ethics and law.
- Beneficence and Non-maleficence: Tests should only be ordered if there’s a clear clinical indication and the potential benefits outweigh the risks of the procedure, including the risk of false positives or negatives leading to unnecessary treatment or delayed diagnosis. We need to minimize harm while maximizing good.
- Justice and Equity: Access to quality diagnostic testing should be fair and equitable, irrespective of socioeconomic status, race, ethnicity, or other demographic factors. Disparities in access can lead to significant health inequities.
- Appropriate Test Utilization: Ordering only necessary tests is crucial. Overtesting exposes patients to unnecessary radiation, costs, and anxiety, while undertesting can delay diagnosis. The cost-effectiveness of tests should always be considered.
For example, imagine a scenario where a patient presents with mild symptoms that could be related to several different conditions. Ethically, we should carefully consider the necessity and benefits of each potential test before ordering any. We might opt for a less invasive and less expensive test first, before resorting to more extensive and costly options.
Q 9. How do you select appropriate diagnostic tests for a specific patient?
Selecting appropriate diagnostic tests is a crucial step in patient care, requiring a systematic approach. It begins with a thorough clinical evaluation, including the patient’s history, physical examination, and presenting symptoms.
Here’s a step-by-step process:
- Define the Clinical Question: What specific information do we need to know to guide treatment? This question drives the selection of tests.
- Consider the Differential Diagnosis: What are the possible conditions based on the clinical presentation? Each potential diagnosis has tests associated with it.
- Evaluate Test Characteristics: For each potential test, consider its sensitivity (ability to correctly identify those with the disease), specificity (ability to correctly identify those without the disease), positive predictive value (probability of having the disease given a positive test), and negative predictive value (probability of not having the disease given a negative test). We also need to consider the test’s cost, invasiveness, and availability.
- Assess Pretest Probability: Based on the patient’s clinical presentation, what is the likelihood of each diagnosis? Tests with higher pretest probabilities are more likely to provide useful information.
- Consider Risk-Benefit Ratio: Weigh the potential benefits of the test against its potential harms, including invasiveness, cost, radiation exposure, and potential psychological impact on the patient.
- Patient Preferences: Patient values and preferences should always be respected, involving them in decision-making whenever possible.
For instance, if a patient presents with chest pain, we might initially order an electrocardiogram (ECG) and cardiac enzyme tests. If these suggest myocardial infarction (heart attack), we might follow up with cardiac catheterization. If the initial tests are negative, other diagnostic avenues may be explored.
Q 10. What are some common sources of error in diagnostic testing?
Errors in diagnostic testing can significantly impact patient care. These errors can arise from various sources:
- Pre-analytical Errors: These occur before the actual testing process. Examples include inadequate patient preparation (e.g., improper fasting), incorrect specimen collection (e.g., hemolyzed blood sample), delayed processing, or incorrect labeling. Poorly maintained equipment and inappropriate transport conditions contribute to inaccuracies.
- Analytical Errors: These are errors during the testing process itself, encompassing instrument malfunction, reagent problems, inadequate calibration, or human error in performing or interpreting the tests. Improper quality control procedures fall under this category.
- Post-analytical Errors: These happen after the testing process, such as data entry errors, incorrect result reporting, or misinterpretation of results by healthcare professionals. This often involves delays in reporting or failure to communicate critical findings.
- Interference from other substances: Certain medications or substances present in the sample can interfere with the test’s accuracy.
For example, a hemolyzed blood sample can lead to falsely elevated potassium levels, whereas improper fasting before a glucose test might result in a false elevation of the glucose level.
Q 11. Describe your experience with quality control procedures in a diagnostic laboratory.
In my experience, quality control (QC) in a diagnostic laboratory is paramount. It’s a multi-faceted process aiming to ensure the accuracy, reliability, and consistency of test results. We employ several strategies:
- Internal Quality Control: This involves regularly running control samples alongside patient samples. These controls have known values, and their results are compared to expected ranges. Any deviation triggers investigation and corrective actions. We use Levey-Jennings charts to visually monitor QC data over time.
- External Quality Assessment (EQA): This entails participating in proficiency testing programs where we analyze blind samples from an external agency and compare our results to those of other laboratories. This helps identify systematic errors and ensures our performance meets established standards.
- Calibration and Maintenance: Analytical instruments require regular calibration and preventative maintenance to ensure accurate measurements. This includes regular checks of equipment and adherence to a scheduled maintenance plan.
- Documentation: Meticulous record-keeping is essential. This includes maintaining logs of QC results, instrument maintenance, and any corrective actions. This audit trail is crucial for traceability and problem-solving.
- Staff Training: Ongoing training for laboratory personnel is vital. This enhances their competence in performing tests, interpreting results, and adhering to QC protocols.
For example, if a control sample repeatedly falls outside the acceptable range, we’d investigate potential causes like reagent degradation, instrument malfunction, or procedural errors. The corrective action might involve replacing reagents, recalibrating the instrument, or retraining personnel.
Q 12. How do you interpret laboratory results and correlate them with clinical findings?
Interpreting laboratory results and correlating them with clinical findings is a critical skill. It’s not simply about reviewing numbers; it’s about understanding their context within the patient’s overall clinical picture.
The process involves:
- Reviewing the Patient’s History and Physical Examination: Understanding the patient’s symptoms, risk factors, and other medical conditions is crucial for interpreting results meaningfully.
- Analyzing the Laboratory Results: This involves comparing the results to reference intervals, considering potential interferences, and assessing the analytical variability of the test.
- Correlation with Clinical Findings: Are the lab results consistent with the patient’s presentation? If not, what are the potential explanations? Does the patient have any other diseases that might confound the interpretation?
- Considering the Test’s Limitations: Every test has its limitations. We must consider the sensitivity, specificity, and predictive values when making inferences.
- Differential Diagnosis: Based on the combined information, we need to develop a differential diagnosis and propose further investigations, if necessary.
Imagine a patient with elevated liver enzymes. Simply stating ‘elevated liver enzymes’ is insufficient. We need to consider the pattern of elevation (e.g., which enzymes are elevated), the patient’s medical history (e.g., alcohol use, medication use), and other clinical findings (e.g., jaundice, abdominal pain). This might point to several possibilities – viral hepatitis, alcoholic liver disease, or medication-induced liver injury. Further tests may be necessary to pinpoint the cause.
Q 13. Explain the role of diagnostic imaging in the diagnosis of specific diseases (e.g., cancer, cardiovascular disease).
Diagnostic imaging plays a crucial role in the diagnosis of various diseases, providing visual information about the internal structures and functions of the body.
- Cancer: Imaging modalities like CT, MRI, PET, and ultrasound are essential in detecting tumors, staging cancers (determining their size and spread), guiding biopsies, and monitoring treatment response. For example, a CT scan can reveal the presence and size of a lung tumor, while an MRI can show whether the tumor has invaded nearby tissues. PET scans can help differentiate between cancerous and non-cancerous tissue.
- Cardiovascular Disease: X-ray, echocardiography (ultrasound of the heart), CT angiography, and cardiac MRI are crucial for evaluating heart structures, blood flow, and identifying conditions such as coronary artery disease, heart valve abnormalities, and congenital heart defects. For example, a coronary CT angiogram can visualize blockages in the coronary arteries, while an echocardiogram can assess heart valve function and identify areas of reduced blood flow.
Imaging is not a standalone diagnostic tool; it’s always interpreted in conjunction with clinical findings and other laboratory data.
Q 14. Discuss the advantages and disadvantages of various imaging modalities (e.g., X-ray, CT, MRI, ultrasound).
Different imaging modalities offer unique advantages and disadvantages:
- X-ray:
- Advantages: Widely available, inexpensive, quick, good for detecting fractures and bone abnormalities.
- Disadvantages: Uses ionizing radiation, limited soft tissue contrast.
- CT:
- Advantages: Excellent for visualizing bone and soft tissues, detailed anatomical information.
- Disadvantages: Uses ionizing radiation, higher radiation dose compared to X-ray.
- MRI:
- Advantages: Excellent soft tissue contrast, no ionizing radiation, superior for visualizing brain and spinal cord.
- Disadvantages: Expensive, longer scan times, contraindicated in patients with certain metallic implants.
- Ultrasound:
- Advantages: No ionizing radiation, relatively inexpensive, real-time imaging, portable.
- Disadvantages: Operator-dependent, limited penetration depth, poor visualization of bone and air-filled structures.
The choice of modality depends on the specific clinical question, the area of the body being imaged, and the patient’s clinical status and characteristics. For example, ultrasound is often the first choice for imaging the abdomen and pelvis, while MRI is usually preferred for brain imaging.
Q 15. How do you ensure patient safety during diagnostic procedures?
Patient safety is paramount in diagnostic procedures. It’s a multi-faceted approach that begins before the procedure even starts and continues throughout.
- Pre-procedure checks: This involves verifying patient identification using multiple methods (e.g., name, date of birth, medical record number), confirming the correct procedure is being performed, and assessing the patient’s medical history and allergies to identify potential risks. For example, checking for any contraindications to contrast dye before a CT scan.
- Proper equipment function: Ensuring all equipment is properly calibrated, maintained, and functioning correctly before use. This includes regular quality control checks on analyzers and imaging machines.
- Sterile technique: Adhering to strict sterile techniques during invasive procedures to minimize infection risk. This might involve using sterile gloves, gowns, and instruments and following proper disinfection protocols.
- Monitoring during the procedure: Closely monitoring the patient’s vital signs (heart rate, blood pressure, oxygen saturation) throughout the procedure to detect and respond to any adverse reactions promptly. For instance, monitoring for signs of an allergic reaction during a contrast study.
- Post-procedure care: Providing appropriate post-procedure care instructions and monitoring for any complications. This includes providing aftercare instructions for a biopsy or explaining the potential side effects of a medication given during a procedure.
Ultimately, a culture of safety, through ongoing training and adherence to established protocols, is crucial. Regular safety audits and incident reporting systems help identify areas for improvement and prevent future errors.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe your experience in using diagnostic software and interpreting reports.
I have extensive experience with various diagnostic software applications, including laboratory information systems (LIS), picture archiving and communication systems (PACS), and electronic health records (EHRs). My expertise encompasses data entry, result validation, report generation, and interpretation.
For example, in my previous role, I utilized a LIS system to input patient data, track test results, and generate comprehensive reports. My interpretation skills extend to a wide array of modalities, including blood chemistry, hematology, microbiology, and imaging (X-ray, CT, MRI). I’m proficient in identifying normal ranges and patterns, and detecting anomalies. I understand the importance of correlating test results with clinical information provided by physicians to ensure accurate diagnosis.
I’m comfortable navigating complex software interfaces, troubleshooting technical issues, and ensuring data accuracy and integrity. My proficiency with these systems is critical for efficient workflow and optimal patient care.
Q 17. What are the key performance indicators (KPIs) you monitor in a diagnostic lab?
Key performance indicators (KPIs) in a diagnostic lab are crucial for assessing efficiency, quality, and overall performance. These metrics are regularly monitored and analyzed to identify areas for improvement and ensure optimal service delivery. Some key KPIs include:
- Turnaround Time (TAT): The time taken from sample collection to result reporting. A shorter TAT indicates efficiency and improved patient care.
- Test Accuracy and Precision: Measured through quality control programs and proficiency testing. This reflects the reliability and consistency of the results.
- Error Rate: The number of errors (pre-analytical, analytical, or post-analytical) per test performed. Lower error rates signify improved quality control.
- Equipment Uptime: The percentage of time equipment is operational and available for testing. High uptime is crucial for maintaining productivity.
- Staff Productivity: Metrics assessing the efficiency of lab personnel in performing various tasks.
- Cost per Test: Monitoring this helps optimize resource allocation and cost-effectiveness.
- Patient Satisfaction: Feedback gathered through surveys or other means to assess the overall experience.
Analyzing these KPIs helps identify bottlenecks, implement corrective actions, and continually improve the lab’s performance and efficiency.
Q 18. How do you manage and troubleshoot equipment malfunctions in a diagnostic setting?
Troubleshooting equipment malfunctions involves a systematic approach. My experience encompasses various techniques:
- Initial Assessment: Identifying the specific problem and its symptoms. For instance, an error message displayed on the machine, or an inaccurate result.
- Check Basic Factors: Rule out simple issues like power supply, connections, and reagent levels.
- Consult Manuals and Documentation: Referencing troubleshooting guides and documentation specific to the equipment. This could involve searching for error codes or checking for known issues.
- Perform Basic Maintenance: Carrying out simple maintenance like cleaning sensors, replacing filters, or checking fluid levels.
- Contacting Technical Support: If the issue persists, contacting the equipment manufacturer’s technical support for assistance. This often involves documenting the error and providing detailed information to facilitate effective troubleshooting.
- Preventive Maintenance Scheduling: Adhering to a regular preventive maintenance schedule helps to minimize unexpected breakdowns.
Documentation of all troubleshooting steps is essential for tracking issues, improving maintenance protocols, and ensuring regulatory compliance.
Q 19. Describe a situation where you had to troubleshoot a diagnostic test result.
In one instance, a patient’s blood glucose level was unexpectedly high, despite the patient reporting normal dietary habits and no history of diabetes. Initially, I suspected a sample handling error. I reviewed the pre-analytical process, including the time of sample collection, the type of tube used, and the transportation conditions. I also checked the analyzer calibration and quality control data to rule out instrument malfunction.
Upon finding no errors, I investigated the possibility of an interfering substance. Further investigation revealed the patient had recently started taking a steroid medication, which could elevate blood glucose levels. Consulting with the physician, we were able to confirm this was the cause and adjust treatment accordingly. This highlighted the critical importance of considering factors beyond laboratory analysis when evaluating test results and the necessity of strong physician-laboratory communication.
Q 20. How do you stay current with advancements in diagnostic technology and techniques?
Staying current in the rapidly evolving field of diagnostic technology requires a multifaceted approach:
- Professional Organizations: Active membership in professional organizations like the American Association for Clinical Chemistry (AACC) provides access to conferences, journals, and continuing education opportunities.
- Continuing Medical Education (CME): Participating in CME courses and workshops helps to stay abreast of the latest advancements in diagnostic techniques and technologies.
- Scientific Journals: Regularly reading peer-reviewed journals and scientific publications is essential to stay updated on research findings and new developments.
- Industry Conferences and Webinars: Attending conferences and webinars provides opportunities to network with peers, learn about new products, and gain insight into emerging technologies.
- Online Resources: Utilizing reputable online resources and databases provides access to vast amounts of information on diagnostic testing.
Continuous learning is not just about technological updates; it’s also about refining analytical skills and staying informed about best practices and regulatory changes.
Q 21. What are the legal and regulatory requirements related to diagnostic testing?
Diagnostic testing is subject to a complex web of legal and regulatory requirements designed to ensure accuracy, patient safety, and ethical practice. These regulations vary by jurisdiction but generally include:
- Clinical Laboratory Improvement Amendments (CLIA): In the United States, CLIA regulations govern the quality and accuracy of laboratory testing. This includes requirements for personnel qualifications, proficiency testing, and quality control measures.
- Health Insurance Portability and Accountability Act (HIPAA): HIPAA regulations in the U.S. mandate the protection of patient health information, including diagnostic test results. Maintaining patient confidentiality is paramount.
- College of American Pathologists (CAP) Accreditation: Many labs seek CAP accreditation, a voluntary process demonstrating adherence to high standards of quality and performance.
- International Organization for Standardization (ISO) Standards: ISO 15189 provides internationally recognized standards for medical laboratories, covering aspects like quality management and competence.
- Data Privacy Regulations: Depending on the location, various regulations govern the handling and storage of patient data, including data security and compliance with privacy laws like GDPR (in Europe).
- Licensure and Certification: Personnel performing diagnostic tests typically require relevant licenses or certifications, demonstrating their competency and qualifications.
Understanding and adhering to these regulations is critical for ensuring legal compliance and maintaining high standards of patient care.
Q 22. How do you explain complex diagnostic results to patients and their families?
Explaining complex diagnostic results requires empathy, clear communication, and a tailored approach. I begin by assessing the patient’s and family’s understanding of medical terminology and their preferred learning style. I avoid overwhelming them with technical jargon, instead using simple language and analogies to illustrate complex concepts. For instance, if explaining a complex cardiac report, I might use a simple analogy of the heart as a pump, explaining blockages or irregularities in terms of reduced flow or inefficient pumping.
I break down the results into manageable chunks, focusing on the key findings and their implications for treatment and prognosis. I encourage questions and actively listen to their concerns, addressing them with patience and honesty. I always ensure they understand the next steps, who to contact if they have further questions, and what to expect in terms of follow-up care. Visual aids, like diagrams or charts, can be particularly helpful, making abstract concepts more concrete and easier to understand.
For example, I recently explained a complicated genetic test result to a family. Instead of just presenting the technical data, I used a family tree to show the inheritance pattern and highlighted the specific gene mutations involved in a way they could easily grasp. We then discussed the potential implications for their children, emphasizing both the risks and the available options for managing the condition.
Q 23. Describe your experience with different types of diagnostic specimens.
My experience encompasses a wide range of diagnostic specimens, including blood (serum, plasma, whole blood), urine, tissue biopsies, cerebrospinal fluid (CSF), and various bodily fluids. I’m proficient in handling and processing each type according to established laboratory protocols, ensuring specimen integrity and avoiding contamination. This involves understanding the appropriate collection methods, storage conditions, and transportation requirements for each specimen type.
For example, the handling of CSF requires meticulous attention to prevent bacterial contamination, while tissue biopsies necessitate careful preservation to maintain cellular morphology for accurate pathological analysis. I’m familiar with various preservation techniques, including formalin fixation and freezing, depending on the intended analyses.
My experience also includes working with less common specimens, such as stool samples for microbiological testing and sputum samples for cytological and microbiological analysis. Understanding the unique challenges associated with each specimen type is crucial for ensuring reliable and accurate results.
Q 24. What are the potential risks and benefits of different diagnostic procedures?
Every diagnostic procedure carries inherent risks and benefits, and it’s crucial to weigh them carefully. For instance, a coronary angiogram, while offering a highly detailed view of coronary arteries, carries the risk of bleeding, allergic reactions to contrast dye, and damage to blood vessels. However, the benefits of early detection and treatment of coronary artery disease far outweigh these risks in many cases.
Similarly, a biopsy, while crucial for definitive diagnosis of many diseases, can cause pain, bleeding, infection, and in rare cases, nerve damage. However, the potential benefits of early cancer detection and targeted treatment justify the risks in appropriate clinical settings.
I always ensure patients are fully informed of both the potential benefits and risks of any procedure before they consent. This includes discussing alternative diagnostic methods, their associated risks and benefits, and the implications of delaying or forgoing the procedure. This shared decision-making approach empowers patients to make informed choices that align with their individual circumstances and values.
Q 25. How do you ensure the confidentiality of patient diagnostic information?
Confidentiality is paramount in diagnostic evaluation. I strictly adhere to HIPAA regulations and institutional policies regarding the protection of patient health information. All patient data, whether electronic or paper-based, is handled according to these regulations. Access to patient information is restricted to authorized personnel on a need-to-know basis.
Electronic health records (EHRs) are secured with strong passwords and encryption. Paper records are stored in locked cabinets in secure areas. I never disclose patient information to unauthorized individuals, and I always ensure that all conversations about patients are conducted in private settings or through secure communication channels.
I regularly undergo training on data privacy and security protocols to stay abreast of evolving regulations and best practices. Additionally, I promptly report any suspected breaches of confidentiality to the appropriate authorities.
Q 26. Describe your experience with different types of diagnostic equipment.
My experience with diagnostic equipment is extensive, spanning various modalities. I’m proficient in operating and maintaining equipment such as hematology analyzers, chemistry analyzers, coagulation analyzers, microscopes (including fluorescence and confocal microscopy), and imaging systems such as ultrasound machines and X-ray machines (though direct operation of the latter is typically the purview of radiologic technologists, my expertise lies in interpreting the resultant images).
I understand the principles of operation for each device, including calibration, quality control procedures, and troubleshooting common malfunctions. I’m adept at interpreting the results generated by this equipment and using those results to contribute to accurate diagnoses. For example, I’m proficient in identifying artifacts and technical issues that can affect the accuracy of laboratory test results. This knowledge is crucial for ensuring the quality and reliability of the diagnostic information we provide.
I also stay updated on new technologies and advancements in diagnostic equipment. Keeping abreast of developments allows for improved efficiency and the use of cutting-edge tools for more accurate and timely diagnosis.
Q 27. How do you prioritize tasks and manage workload in a fast-paced diagnostic setting?
Prioritizing tasks and managing workload in a fast-paced diagnostic setting requires effective time management and organizational skills. I use a combination of strategies to ensure efficient workflow and timely delivery of results. This includes prioritizing tasks based on urgency and clinical importance, using a combination of ‘urgent and important’, ‘important but not urgent’, ‘urgent but not important’ and ‘neither urgent nor important’ matrix.
I utilize electronic task management systems to track deadlines, delegate tasks when appropriate, and manage my schedule effectively. I communicate proactively with colleagues and clinicians, ensuring clear expectations and timely updates on the progress of diagnostic testing. I also regularly review my workflow to identify bottlenecks and areas for improvement.
For instance, I might prioritize STAT (statim, meaning immediately) requests over routine tests, ensuring that critical results are available to clinicians as quickly as possible. In addition, I frequently batch similar tests together to optimize workflow and minimize turnaround times.
Q 28. Explain your approach to continuous improvement in diagnostic evaluation practices.
Continuous improvement is essential for maintaining high standards of diagnostic evaluation. My approach involves several key strategies. Firstly, I actively participate in continuing medical education (CME) activities to stay updated on new technologies, diagnostic techniques, and best practices. This includes attending conferences, workshops, and online courses, and reading peer-reviewed journals.
Secondly, I regularly review my own performance and identify areas for improvement. I actively seek feedback from colleagues and clinicians to refine my skills and enhance efficiency. I use quality control charts and data analysis to monitor the accuracy and precision of laboratory tests. I also participate in audits and quality improvement initiatives, contributing to the development and implementation of new protocols and procedures.
Finally, I embrace a culture of learning and sharing knowledge within my team. By collaborating with colleagues and sharing best practices, we can collectively improve the quality of diagnostic services we provide. For example, we recently implemented a new protocol for handling specimens, resulting in a significant reduction in turnaround time and errors.
Key Topics to Learn for Diagnostic Evaluation Interview
- Test Selection & Interpretation: Understanding the principles behind choosing appropriate diagnostic tests based on patient presentation, and accurately interpreting results considering sensitivity, specificity, and predictive values.
- Differential Diagnosis: Developing a structured approach to differentiating between various possible diagnoses based on clinical findings and test results. This includes prioritizing likely diagnoses and ruling out critical conditions.
- Clinical Reasoning & Problem-Solving: Applying critical thinking skills to analyze complex patient cases, identify patterns, and form evidence-based conclusions. Practice utilizing case studies to improve this skill.
- Ethical Considerations: Understanding the ethical implications of diagnostic testing, including informed consent, patient confidentiality, and the responsible use of resources.
- Communication & Collaboration: Mastering effective communication with patients, physicians, and other healthcare professionals to clearly convey information and collaborate on patient care plans.
- Data Analysis & Statistical Concepts: Familiarity with basic statistical concepts relevant to diagnostic test performance, including measures of central tendency and variability. Understanding how to interpret and analyze data from diagnostic tests.
- Specific Diagnostic Modalities (Depending on Role): Deepen your understanding of specific diagnostic modalities relevant to your target role, such as imaging techniques (X-ray, CT, MRI, Ultrasound), laboratory tests, or other specialized diagnostic tools.
- Limitations of Diagnostic Tests: Critically assessing the limitations of different diagnostic tests and the potential for false positives and false negatives. Understanding how these limitations impact clinical decision-making.
Next Steps
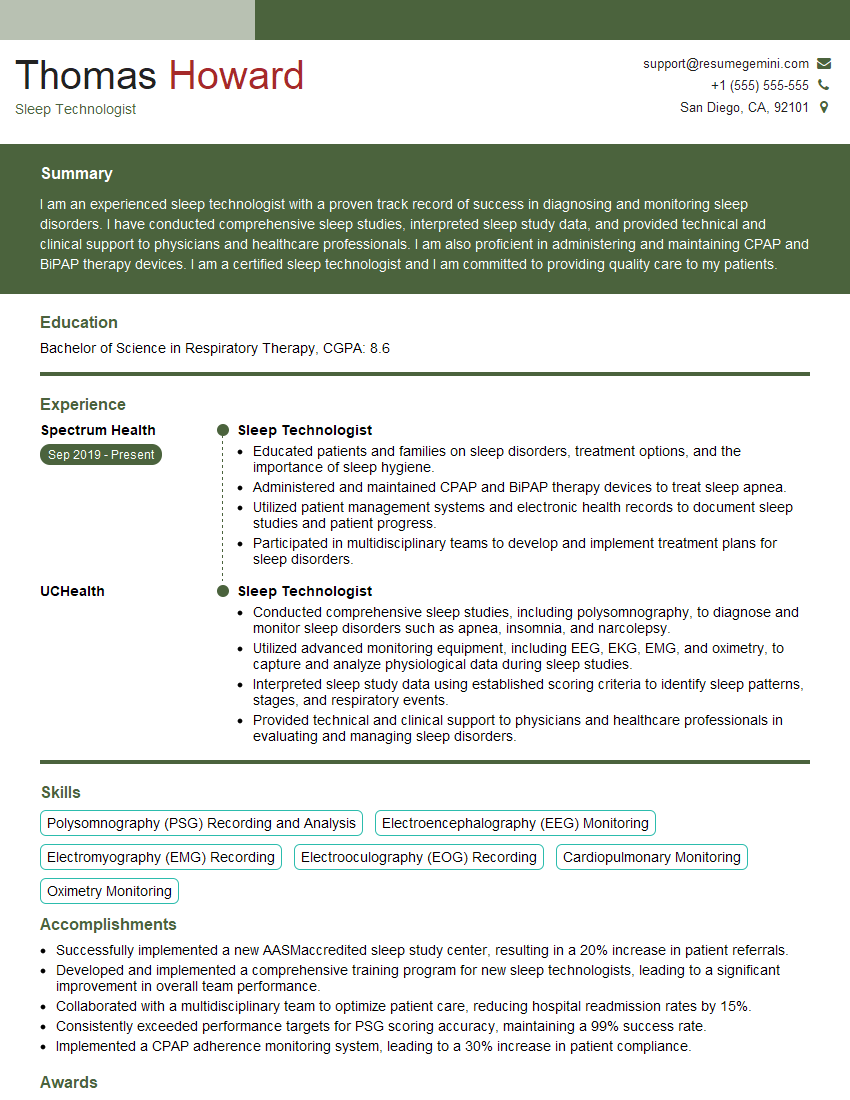
Mastering diagnostic evaluation is crucial for career advancement in healthcare, opening doors to more specialized roles and increased responsibilities. A strong resume is key to showcasing your skills and experience to potential employers. To maximize your job prospects, create an ATS-friendly resume that highlights your key competencies and achievements. ResumeGemini is a trusted resource to help you build a professional and impactful resume. Examples of resumes tailored specifically to Diagnostic Evaluation roles are available to guide you.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.