Interviews are more than just a Q&A session—they’re a chance to prove your worth. This blog dives into essential Diagnostic Procedures interview questions and expert tips to help you align your answers with what hiring managers are looking for. Start preparing to shine!
Questions Asked in Diagnostic Procedures Interview
Q 1. Explain the difference between ionizing and non-ionizing radiation in diagnostic imaging.
The key difference between ionizing and non-ionizing radiation lies in their energy levels and their effects on atoms. Ionizing radiation, such as X-rays and gamma rays used in CT scans and nuclear medicine, carries enough energy to remove electrons from atoms, creating ions. This ionization can damage DNA and other cellular components, potentially leading to long-term health risks like cancer. Non-ionizing radiation, like ultrasound, uses lower-energy sound waves. These waves do not ionize atoms; instead, they cause vibrations within tissues, creating images based on the reflections of these sound waves. While generally considered safe, high-intensity ultrasound can potentially cause heating of tissues.
Think of it like this: ionizing radiation is like a powerful hammer that can break things apart, while non-ionizing radiation is more like a gentle tap that causes vibrations. Both can be useful tools in medical imaging, but their potential risks are vastly different and require different safety protocols.
Q 2. Describe the principles of ultrasound imaging.
Ultrasound imaging relies on the principle of sound wave reflection. A transducer emits high-frequency sound waves into the body. These waves travel through different tissues at varying speeds, depending on the tissue’s density. When the sound waves encounter a boundary between two different tissues (e.g., muscle and bone), some of the sound waves are reflected back to the transducer. The transducer then receives these reflected waves, and a computer processes the information to create an image. The time it takes for the sound waves to return, along with the strength of the reflected signal, determines the brightness and location of structures within the image. This allows us to visualize internal organs and structures without using ionizing radiation.
For example, imagine throwing a pebble into a pond. The ripples represent the sound waves. The speed at which the ripples move across the pond would depend on the depth of the water, much like how sound waves travel differently through various tissues. The reflections of these ripples off objects in the pond would give you information on their position and nature, similar to how ultrasound imaging works.
Q 3. What are the safety protocols for patients undergoing CT scans?
Patient safety during CT scans is paramount and involves several protocols. First, we always assess for pregnancy, as radiation exposure to a developing fetus is a significant concern. We utilize effective radiation dose reduction strategies like lowering the kVp (kilovolt peak, which determines the energy of the x-rays) and mAs (milliampere-seconds, which controls the x-ray beam intensity) to minimize radiation exposure while maintaining image quality. Contrast media, if used, are assessed for potential allergies and kidney function. We provide patients with clear instructions on appropriate breathing techniques during the scan to reduce motion artifacts. Post-scan, patients are monitored for any adverse reactions to the contrast media. Furthermore, shielding, when appropriate, is utilized to protect sensitive areas.
Imagine a finely tuned instrument – the CT scanner. We carefully adjust the settings to achieve the optimal image with the least amount of ‘noise’ (radiation). We also carefully monitor the patient, much like a conductor monitoring an orchestra to ensure a flawless performance and minimize any negative impact.
Q 4. How do you ensure proper patient identification and preparation before a diagnostic procedure?
Proper patient identification and preparation are crucial to avoid errors and ensure a smooth, safe procedure. We begin by verifying patient identity using at least two identifiers (e.g., name, date of birth) from the requisition form and comparing them with the patient’s identification bracelet. Next, we explain the procedure clearly, addressing any concerns or questions. Preparation varies based on the procedure. For example, bowel preparation may be necessary for abdominal imaging, while fasting might be required before certain studies. We provide clear instructions and follow-up as needed to ensure patients are well-informed and adequately prepared.
Think of it like meticulously preparing for a surgical operation – every step is crucial to minimize errors and maximize patient safety and the effectiveness of the procedure. Double-checking patient details is like verifying that the patient undergoing surgery is actually the patient listed on the operative notes.
Q 5. Explain the ALARA principle in radiation safety.
ALARA stands for ‘As Low As Reasonably Achievable.’ This principle is fundamental to radiation safety and guides our practices to minimize radiation exposure to patients and staff. It doesn’t mean eliminating all radiation; rather, it means optimizing techniques to reduce exposure to the lowest level possible while still obtaining diagnostic quality images. This involves selecting appropriate imaging modalities, optimizing technical parameters (kVp, mAs in X-ray), using shielding, and employing appropriate radiation protection measures. Balancing image quality with minimizing radiation dose is a constant consideration.
For instance, if we can achieve a good diagnostic image with a lower dose of radiation, we always opt for that lower dose. This is a constant decision-making process, weighing clinical efficacy with the risk associated with radiation exposure.
Q 6. Describe the artifacts commonly seen in ultrasound imaging and their causes.
Ultrasound images can be affected by various artifacts, which are structures or features appearing on the image that do not accurately represent actual anatomy. These can be caused by several factors. For example, acoustic shadowing occurs when sound waves are strongly attenuated by a dense structure (like bone), creating a dark area behind it. Reverberation artifacts appear as multiple parallel lines behind a highly reflective structure, like air in the lungs. Refraction occurs when sound waves bend as they pass from one tissue to another, distorting the image. Acoustic enhancement happens when sound waves are transmitted more easily through a fluid-filled structure, making structures behind it appear brighter than they should. Understanding these artifacts is crucial for accurate image interpretation.
Think of looking at a pond with ripples – the ripples themselves, or how they distort the view of the underwater objects, are like artifacts that can interfere with accurately seeing what’s below.
Q 7. What are the advantages and disadvantages of MRI compared to CT?
MRI (Magnetic Resonance Imaging) and CT (Computed Tomography) are both powerful imaging modalities, but they have distinct advantages and disadvantages. MRI offers superior soft tissue contrast, making it ideal for visualizing the brain, spinal cord, ligaments, and tendons. It uses no ionizing radiation. However, it’s more time-consuming, expensive, and has limitations with patients who have certain metallic implants or claustrophobia. CT, on the other hand, is faster and less expensive, providing excellent bone detail. It’s useful in trauma cases and for detecting internal bleeding. However, it utilizes ionizing radiation, limiting the number of scans a patient can safely undergo.
Imagine choosing between two cars – one is a luxury vehicle (MRI) with superior comfort and features but is expensive and might not be suitable for all terrains. The other is a more rugged, versatile vehicle (CT) that is less expensive but doesn’t offer the same level of comfort and has limitations on long-distance journeys.
Q 8. Explain the role of contrast media in diagnostic imaging.
Contrast media are substances introduced into the body to enhance the visibility of internal structures during diagnostic imaging procedures. They work by altering the density or signal intensity of tissues, making them more easily distinguishable from surrounding structures. This is particularly important for visualizing blood vessels, organs, and other anatomical features that might otherwise be difficult to see on standard imaging.
For example, in a CT scan of the abdomen, an iodine-based contrast agent is often injected intravenously. The iodine atoms absorb X-rays differently than surrounding tissues, resulting in enhanced visualization of blood vessels and organs like the liver, kidneys, and spleen. Similarly, barium sulfate, a non-absorbable contrast agent, is commonly used in fluoroscopy and X-ray examinations to outline the gastrointestinal tract.
Different types of contrast media exist, each with specific properties tailored to different imaging modalities and anatomical areas. Choosing the appropriate contrast agent is crucial for optimal image quality and patient safety, taking into account factors such as patient allergies and renal function.
Q 9. How do you troubleshoot equipment malfunctions during a procedure?
Troubleshooting equipment malfunctions during a procedure requires a systematic approach that prioritizes patient safety and efficient problem-solving. My first step is always to ensure patient safety—moving them to a safe location if necessary. Then, I follow these steps:
- Identify the problem: What exactly isn’t working? Are there any error messages? Is it a software or hardware issue? This often involves carefully observing the equipment’s behavior.
- Check basic connections: Are power cords connected? Are any cables loose or damaged? This seemingly simple check often resolves the issue.
- Consult the equipment manual: Most imaging equipment has comprehensive troubleshooting guides. The manual may provide solutions to common problems or steps for contacting technical support.
- Contact technical support: If the problem persists, contacting the manufacturer’s technical support team is crucial. They possess in-depth knowledge of the equipment and can often provide remote assistance or dispatch an engineer for on-site repair.
- Document the malfunction: Record the nature of the problem, steps taken to troubleshoot it, and the resolution (or lack thereof). This documentation is vital for quality assurance, preventing future incidents, and potentially aiding in warranty claims.
For instance, if a CT scanner stops mid-scan due to a software error, I’d first check if a power surge occurred, then refer to the troubleshooting manual’s error code, and if all else fails, contact the manufacturer’s tech support. Documenting everything ensures the problem is reported effectively.
Q 10. What are the ethical considerations related to patient confidentiality in diagnostic imaging?
Ethical considerations surrounding patient confidentiality in diagnostic imaging are paramount. Patient information, including images, reports, and any details about their medical history, is strictly protected under laws like HIPAA (in the US) and similar regulations in other countries. Maintaining confidentiality is not just a legal requirement but a fundamental ethical obligation.
This includes:
- Secure storage of images and data: Images and patient data should be stored on secure servers with restricted access, employing strong passwords and encryption to prevent unauthorized access.
- Limited access to information: Only authorized personnel directly involved in the patient’s care should have access to their medical images and reports. Access should be granted based on a “need-to-know” basis.
- Protection of patient privacy during discussions: Conversations about patients should always take place in private settings, avoiding public spaces or overheard discussions.
- Proper disposal of records: When images or reports are no longer needed, they must be disposed of securely, ensuring patient information is not compromised.
A real-world example would be ensuring that only the radiologist, referring physician, and other directly involved healthcare professionals have access to a patient’s MRI scan, and that access logs are maintained and regularly audited.
Q 11. Describe the image acquisition process for a specific modality (e.g., X-ray, CT, MRI).
Let’s describe the image acquisition process for a CT (Computed Tomography) scan. A CT scanner uses X-rays to create cross-sectional images of the body. The process involves several steps:
- Patient positioning: The patient is positioned on the examination table, ensuring correct alignment with the scanner. Immobilization devices may be used if necessary to minimize movement artifacts.
- Scan parameters selection: The radiographer or technologist selects appropriate scan parameters, such as slice thickness, rotation time, and kVp (kilovoltage peak), based on the clinical question and patient characteristics.
- X-ray tube rotation: The X-ray tube and detectors rotate around the patient, acquiring data from multiple angles. The X-rays pass through the body, and the detectors measure the amount of radiation that is transmitted.
- Data acquisition and reconstruction: The acquired data is processed by a computer using sophisticated algorithms to reconstruct cross-sectional images. These images are then displayed for review by the radiologist.
- Image review and post-processing: The radiologist reviews the images to look for abnormalities. Additional post-processing techniques, such as windowing and level adjustments, can be applied to optimize image quality and visibility of specific structures.
Think of it like taking many thin slices of a loaf of bread – each slice is a CT image, and the computer assembles them to show a detailed 3D view of the internal structures.
Q 12. How do you interpret basic imaging findings in your area of expertise?
Interpreting basic imaging findings requires a strong foundation in anatomy, physiology, and pathology, along with experience in recognizing patterns and anomalies. My expertise lies in X-ray interpretation. For example, I look for:
- Fractures: Disruptions in the bone cortex, often accompanied by displacement or angulation.
- Consolidation: Increased density in the lungs, indicating pneumonia or other infiltrative processes.
- Pneumoperitoneum: Free air in the abdominal cavity, which is indicative of a perforation.
- Foreign bodies: Objects that are not supposed to be present within the body, such as ingested items.
- Soft tissue swelling: Increased density in the soft tissues, suggestive of inflammation or injury.
For instance, observing a lucent line across a bone on an X-ray is a classic finding for a fracture. The location and extent of the fracture will aid in diagnosis.
It’s crucial to remember that image interpretation is not an isolated process. The clinical history of the patient, including symptoms and prior medical conditions, plays a vital role in making an accurate diagnosis. I always correlate the imaging findings with the clinical presentation before drawing conclusions.
Q 13. Explain the difference between various types of X-ray examinations.
X-ray examinations vary depending on the anatomical area being imaged and the clinical question being addressed. Here are some key differences:
- Chest X-ray (CXR): A routine examination to evaluate the lungs, heart, and mediastinum. It is useful in detecting pneumonia, pneumothorax, and other pulmonary conditions. Different views are used such as PA (posteroanterior) and lateral projections.
- Abdominal X-ray: Used to assess the abdominal organs, looking for free air, bowel obstructions, or foreign bodies. It’s usually done in an upright and supine position.
- Extremity X-rays: Images of the limbs used to detect fractures, dislocations, or other bone abnormalities. The specific views depend on the suspected area of injury.
- Skeletal survey: A comprehensive set of X-rays covering the entire skeleton, usually used in the evaluation of child abuse or metastatic disease.
- Barium studies: These studies use a contrast agent (barium) to visualize the gastrointestinal tract. Examples include barium swallows (esophagus), upper GI series (esophagus, stomach, duodenum), and barium enemas (large intestine). These methods reveal conditions like strictures and tumors.
The choice of examination type is determined by the physician’s clinical suspicions and the information needed to guide management.
Q 14. What quality control measures do you perform to ensure optimal image quality?
Maintaining optimal image quality is essential for accurate diagnosis. We employ several quality control (QC) measures:
- Regular equipment calibration: CT, X-ray, and other imaging equipment requires regular calibration to ensure consistent image quality. This is often performed by biomedical engineers.
- Image quality assurance testing: This involves using standardized phantoms (objects with known characteristics) to assess factors such as image resolution, contrast, and noise. Any deviations from established metrics trigger corrective actions.
- Image review: Regular review of images by experienced personnel helps identify subtle issues and ensures consistency in image acquisition and processing. This is an ongoing quality check performed by radiologists and technologists.
- Maintenance and preventative measures: Regular maintenance, including cleaning and lubrication, is critical to prolong the equipment’s lifespan and prevent breakdowns that may negatively affect image quality. This includes regular cleaning of detectors and X-ray tubes.
- Personnel training: Ensuring that all personnel involved in the imaging process (technologists, radiologists) are properly trained to operate the equipment and follow protocols helps minimize human error.
For instance, if our routine QC tests show a decline in spatial resolution in our CT images, we would investigate the source, which might be due to detector malfunction and then schedule the necessary maintenance/repair. These measures ensure that we consistently deliver high-quality images.
Q 15. How do you maintain proper infection control during diagnostic procedures?
Maintaining proper infection control during diagnostic procedures is paramount to patient safety and preventing healthcare-associated infections (HAIs). It’s a multifaceted process involving strict adherence to established protocols and guidelines.
- Hand Hygiene: This is the cornerstone. We meticulously wash our hands with soap and water or use alcohol-based hand rub before and after each patient interaction, and any time our hands become contaminated. Think of it like a chef washing their hands before preparing a meal – it’s non-negotiable.
- Personal Protective Equipment (PPE): Appropriate PPE, such as gloves, gowns, masks, and eye protection, is used consistently depending on the procedure and the potential for exposure to bodily fluids. For example, during a procedure with a high risk of splashing, we’d wear a gown and eye protection in addition to gloves.
- Sterilization and Disinfection: All equipment that comes into contact with patients must be meticulously sterilized or disinfected according to established protocols. This includes ultrasound probes, endoscopes, and other instruments. We have rigorous cleaning procedures in place and use appropriate disinfectants to prevent contamination.
- Environmental Cleaning: The examination room and surrounding areas are regularly cleaned and disinfected using hospital-grade disinfectants. This includes surfaces, equipment, and floors. We follow a strict schedule to ensure a clean environment.
- Aseptic Techniques: During invasive procedures, we employ strict aseptic techniques to minimize the risk of infection. This involves creating a sterile field and using sterile instruments and supplies.
- Waste Disposal: Medical waste is handled and disposed of appropriately according to established safety regulations. This minimizes risk of exposure and protects both the healthcare workers and the environment.
Regular training and adherence to established infection control protocols are crucial. We also participate in audits and quality control measures to continuously improve our infection control practices.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Describe the role of PACS (Picture Archiving and Communication System) in diagnostic imaging.
PACS, or Picture Archiving and Communication System, is the digital backbone of modern diagnostic imaging. It’s a centralized system that allows for the storage, retrieval, distribution, and display of medical images. Think of it as a highly secure and organized digital library for medical images.
- Image Storage: PACS stores images from various modalities like X-ray, CT, MRI, and ultrasound in a secure, readily accessible format. This eliminates the need for bulky film storage.
- Image Retrieval: Physicians and other healthcare professionals can quickly and easily access images from anywhere within the network, improving diagnostic efficiency. No more searching through filing cabinets.
- Image Distribution: Images can be shared seamlessly between different departments and healthcare facilities, facilitating consultations and improving patient care. Imagine a cardiologist consulting with a radiologist on a complex case; PACS allows instant image sharing.
- Image Display: Images are displayed on high-resolution monitors, allowing for detailed analysis. Advanced features like image manipulation and measurement tools are often integrated into the system.
- Workflow Optimization: PACS streamlines the workflow by automating many tasks, such as image routing and report generation.
The use of PACS is critical for efficient workflow, optimized storage, and improved collaborative care in diagnostic imaging. It significantly improves patient care by enabling faster access to crucial information.
Q 17. How do you handle situations with difficult or anxious patients?
Handling anxious or difficult patients requires patience, empathy, and effective communication skills. It’s crucial to remember that their anxiety might stem from fear of the unknown, previous negative experiences, or underlying medical conditions.
- Establish Rapport: I begin by introducing myself, explaining the procedure in simple terms, and answering any questions they may have. Building trust is key.
- Active Listening: I pay close attention to their concerns and address them honestly and openly. Sometimes just letting them express their fears can alleviate anxiety.
- Clear and Simple Explanations: I use clear, concise language, avoiding medical jargon. I’ll use analogies or simple comparisons to make complex concepts more understandable.
- Pain Management: For procedures that could cause discomfort, I explain the process and offer appropriate pain relief measures. This can include medication or relaxation techniques.
- Reassurance and Support: I offer reassurance and support throughout the procedure. A calming presence and a supportive attitude can make a huge difference.
- Involving Family Members: In some cases, involving family members or support persons can be helpful, provided the patient is comfortable with this.
If despite these efforts, a patient remains uncooperative, I involve the appropriate medical staff, such as a physician or nurse, to help manage the situation. The patient’s safety and well-being are always the top priority.
Q 18. Explain the process for documenting procedures and findings.
Accurate and complete documentation is essential for legal and medical reasons. It serves as a permanent record of the procedure, findings, and any actions taken.
- Patient Identification: The documentation begins with verifying the patient’s identity using multiple identifiers (name, date of birth, medical record number) to prevent errors.
- Procedure Details: A detailed description of the procedure performed is recorded, including the type of imaging used, the specific areas examined, the technique employed, and any special instructions.
- Findings: All relevant findings are clearly documented, using standardized terminology and avoiding vague descriptions. We may use pre-defined templates or structured reporting formats.
- Images: Images acquired during the procedure are linked to the report electronically via PACS. This provides a complete and readily accessible record.
- Interventions: Any interventions performed during the procedure, such as the administration of contrast media or medication, are carefully documented, including the dosage and route of administration.
- Follow-up recommendations: Any follow-up recommendations made to the referring physician are included in the report.
This detailed documentation ensures continuity of care, facilitates communication between healthcare professionals, and provides a legal record of the diagnostic procedure. It’s crucial for accurate billing and quality assurance as well.
Q 19. How do you ensure patient safety during fluoroscopy procedures?
Fluoroscopy, which uses real-time X-ray imaging, requires special attention to patient safety due to the continuous exposure to radiation. Several measures are implemented to minimize radiation exposure.
- ALARA Principle: We strictly adhere to the ALARA principle – As Low As Reasonably Achievable. This means using the lowest possible radiation dose to achieve diagnostic quality images. We carefully select the appropriate technical factors (kVp, mA, time).
- Lead Shielding: Lead aprons, thyroid shields, and other protective equipment are used to shield the patient from unnecessary radiation exposure. These are crucial, especially for vulnerable areas like the reproductive organs.
- Image Intensifier Settings: The image intensifier’s settings are adjusted to minimize the radiation dose while maintaining image quality. We continuously assess the need for pulsed fluoroscopy versus continuous fluoroscopy.
- Pulse Fluoroscopy: When possible, pulsed fluoroscopy is preferred over continuous fluoroscopy, reducing the radiation dose significantly. It’s like taking pictures instead of a continuous video, reducing exposure time.
- Time Minimization: We minimize the duration of fluoroscopy by efficiently performing the procedure and avoiding unnecessary exposures. Time is the biggest factor for radiation dose.
- Distance Maximization: We maintain appropriate distance from the X-ray beam when possible, reducing the scatter radiation dose.
Regular safety checks of equipment and staff training on radiation safety protocols are essential for ensuring patient safety during fluoroscopy procedures.
Q 20. What are the limitations of your specific area of diagnostic expertise?
My specific area of expertise is in diagnostic ultrasound. While highly effective, it does have limitations.
- Operator Dependence: The quality of the ultrasound image is heavily reliant on the skill and experience of the sonographer. A less experienced sonographer might miss subtle findings.
- Image Quality: Image quality can be affected by factors such as patient habitus (body size and composition), bowel gas, and the presence of overlying structures. Obesity, for example, can significantly reduce image penetration.
- Limited Penetration: Ultrasound has limited penetration depth compared to other modalities like CT or MRI. It’s less effective for visualizing deep-seated structures.
- Bone Attenuation: Bone significantly attenuates ultrasound waves, making it difficult to visualize structures beyond bone. It’s challenging to get a clear image through the ribs, for instance.
- Air Interference: Air-filled structures like lungs significantly interfere with ultrasound waves, making it unsuitable for imaging these areas.
These limitations are important to consider when ordering and interpreting ultrasound examinations. Often, other imaging modalities are necessary for a complete evaluation. It’s crucial to select the most appropriate imaging technique for each clinical situation.
Q 21. Describe a time you had to troubleshoot a complex technical issue.
During a routine ultrasound examination, our machine suddenly displayed a critical error message indicating a problem with the transducer. The patient was mid-examination, and I couldn’t acquire any further images.
- Assessment: I immediately assessed the situation and checked the transducer connections. It was securely connected, ruling out simple connection issues.
- Troubleshooting Steps: I followed the machine’s troubleshooting guide step-by-step. This involved checking power supply, internal diagnostics, and running self-tests.
- Collaboration: As the problem persisted, I contacted our biomedical engineering department for assistance. They remotely accessed the machine’s diagnostics to run more in-depth tests.
- Temporary Solution: While waiting for the engineer, I used a backup transducer to complete the examination, ensuring the patient was not significantly delayed.
- Resolution: The biomedical engineer identified a faulty internal component within the transducer. The component was repaired, and the machine was back online within a few hours.
This incident highlighted the importance of having backup equipment, comprehensive troubleshooting guides, and readily available technical support. The successful resolution ensured minimal disruption to patient care.
Q 22. How do you stay updated on the latest advancements in diagnostic imaging technology?
Staying current in the rapidly evolving field of diagnostic imaging requires a multi-pronged approach. I prioritize continuous professional development through several key strategies. Firstly, I actively participate in professional organizations like the American College of Radiology (ACR) and the Society of Diagnostic Medical Sonography (SDMS), attending conferences and webinars to learn about the latest technological breakthroughs and clinical applications. These events often feature presentations by leading experts and offer opportunities for networking and knowledge exchange. Secondly, I subscribe to leading peer-reviewed journals such as Radiology, Radiographics, and AJR American Journal of Roentgenology, regularly reviewing articles on new imaging modalities, techniques, and research findings. Thirdly, I actively engage in online continuing medical education (CME) courses and modules offered by reputable platforms, ensuring I’m up-to-date on best practices and safety protocols. Finally, I maintain a professional network with colleagues in the field, participating in regular discussions and case reviews to share experiences and insights on the latest advancements.
Q 23. Describe your experience with different types of imaging equipment.
My experience encompasses a broad range of diagnostic imaging equipment, including conventional radiography (X-ray), fluoroscopy, computed tomography (CT), magnetic resonance imaging (MRI), ultrasound, and nuclear medicine modalities such as PET/CT. For instance, I’ve extensively used CT scanners to diagnose various trauma injuries, from fractures to internal bleeding, utilizing advanced reconstruction techniques to create detailed 3D models. With MRI, I’ve worked extensively with various sequences, such as T1-weighted and T2-weighted imaging, to effectively differentiate different tissue types and identify pathologies in the brain, spine, and musculoskeletal system. My experience with ultrasound includes both abdominal and obstetrical applications, performing examinations, and interpreting results for various clinical scenarios. In nuclear medicine, I’ve worked with PET/CT scans for cancer staging and treatment monitoring. This broad experience enables me to select the most appropriate imaging modality for each clinical situation, maximizing diagnostic accuracy and minimizing patient exposure to radiation.
Q 24. How do you work effectively as part of a healthcare team?
Effective teamwork is paramount in healthcare. I believe in fostering open communication, active listening, and mutual respect among all team members. My approach involves proactively sharing relevant information, participating in collaborative discussions, and valuing diverse perspectives. For instance, in a recent case involving a patient with complex abdominal pain, I collaborated closely with the radiologist, gastroenterologist, and surgeon. I provided detailed imaging reports, highlighting relevant findings, and actively participated in multidisciplinary rounds to facilitate a comprehensive diagnosis and treatment plan. Clear and timely communication, especially when critical findings are involved, ensures efficient patient care and avoids delays in treatment. I believe in a supportive team environment where everyone feels comfortable voicing concerns and offering suggestions, ultimately leading to optimal patient outcomes.
Q 25. Explain your understanding of radiation protection regulations.
My understanding of radiation protection regulations is comprehensive and firmly rooted in adherence to ALARA (As Low As Reasonably Achievable) principles. I am proficient in applying safety protocols for both patients and personnel, including the use of appropriate shielding, optimized imaging parameters, and adherence to radiation safety guidelines established by organizations such as the Nuclear Regulatory Commission (NRC) and the International Commission on Radiological Protection (ICRP). This includes understanding and correctly applying radiation dose limits, performing quality control checks on equipment, and employing techniques like image optimization to minimize radiation exposure while maintaining image quality. Furthermore, I am trained to properly document radiation exposure and conduct regular safety audits to ensure continuous compliance with all relevant regulations. I would actively participate in radiation safety training programs, staying updated on any changes or new recommendations. A recent example involved optimizing a CT protocol to reduce radiation dose by 20% without compromising diagnostic image quality, a direct application of ALARA principles.
Q 26. Describe your experience with image post-processing and analysis.
Image post-processing and analysis is an integral part of my workflow, significantly enhancing diagnostic accuracy. I am proficient in using various software packages, including PACS (Picture Archiving and Communication Systems) and advanced image processing tools. My skills include windowing and leveling for optimal image visualization, utilizing various image enhancement techniques to improve visibility of subtle details, and employing advanced reconstruction algorithms, such as MIP (Maximum Intensity Projection) and MPR (Multiplanar Reconstruction), to better interpret complex anatomical structures. For example, in evaluating chest CT scans, I often use MPR to create coronal and sagittal views, allowing for better visualization of lung lesions and their relationship to surrounding structures. This detailed analysis, coupled with my clinical experience, helps improve diagnostic confidence and ultimately leads to better patient care.
Q 27. How do you handle situations where images are suboptimal or unclear?
When confronted with suboptimal or unclear images, a systematic approach is crucial. First, I carefully review the technical parameters of the examination, identifying potential issues such as motion artifacts, inadequate exposure, or incorrect positioning. Second, I communicate with the technologist to ascertain whether any technical problems occurred during the acquisition. Third, I explore alternative imaging techniques or additional views to gain supplementary information. For example, if a chest X-ray is unclear due to patient motion, I might request a repeat examination while implementing strategies to minimize motion. If the issue remains, I might suggest a higher-resolution CT scan for more detailed visualization. Finally, if all attempts to improve image quality fail, I consult with senior colleagues or specialists for a second opinion and to determine the best course of action for patient management. The goal is always to obtain the clearest possible image while balancing diagnostic needs and patient safety.
Key Topics to Learn for Diagnostic Procedures Interview
- Imaging Techniques: Understanding the principles, applications, and limitations of various imaging modalities such as X-ray, CT, MRI, Ultrasound, and Fluoroscopy. Consider the strengths and weaknesses of each in diagnosing different pathologies.
- Laboratory Diagnostics: Mastering the interpretation of blood tests (hematology, chemistry, coagulation), urinalysis, microbiology cultures, and other laboratory results. Practice analyzing abnormal results and correlating them with clinical presentations.
- Electrodiagnostic Studies: Familiarize yourself with the principles and applications of EEG, ECG, EMG, and nerve conduction studies. Be prepared to discuss the interpretation of waveforms and their diagnostic significance.
- Pathophysiology and Disease Processes: Develop a strong understanding of the underlying pathophysiology of common diseases and how diagnostic procedures are used to confirm or rule out diagnoses. Practice connecting the dots between clinical symptoms and diagnostic findings.
- Quality Assurance and Control: Understand the importance of quality control in diagnostic procedures, including safety protocols, equipment maintenance, and regulatory compliance. Be ready to discuss best practices and troubleshooting techniques.
- Ethical and Legal Considerations: Be aware of ethical implications surrounding patient privacy, informed consent, and the appropriate use of diagnostic procedures. Understand relevant legal frameworks and regulations.
- Problem-Solving and Critical Thinking: Practice analyzing complex cases, interpreting ambiguous results, and formulating differential diagnoses. Develop your ability to synthesize information from multiple sources to reach accurate conclusions.
Next Steps
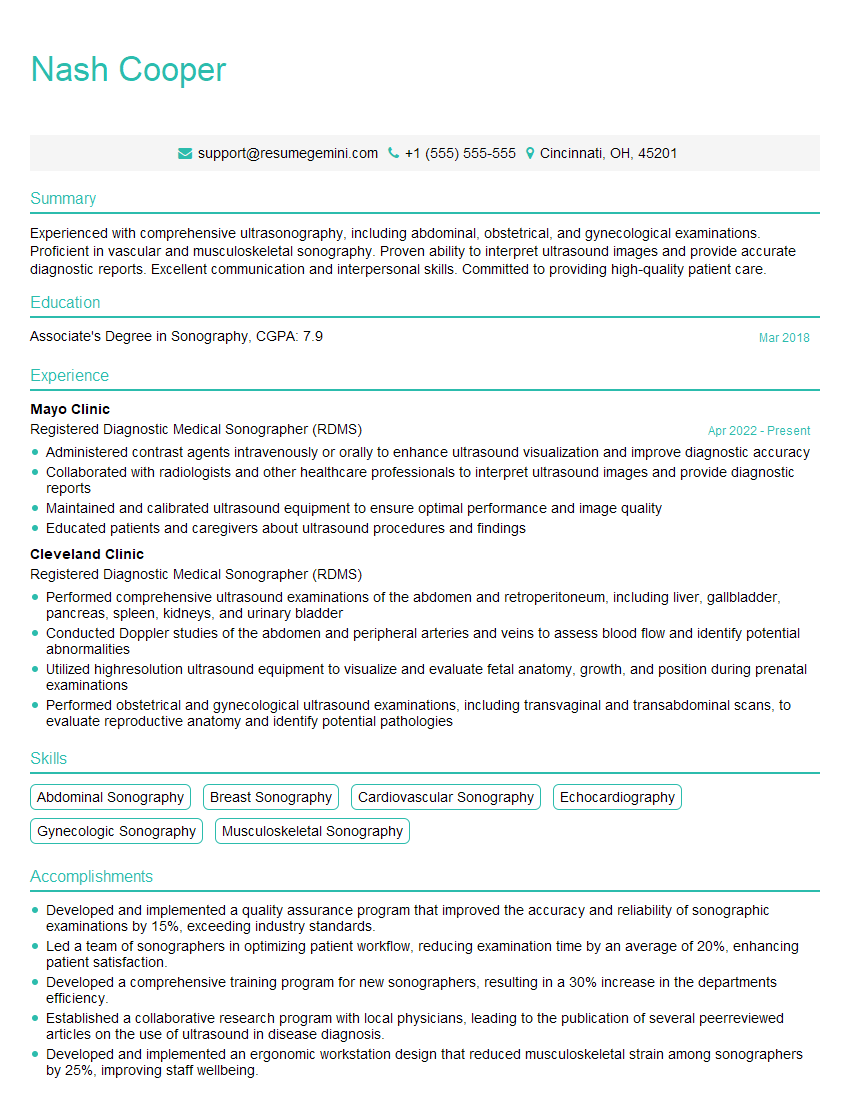
Mastering Diagnostic Procedures is crucial for advancing your career in healthcare. A strong understanding of these techniques will make you a highly valuable asset to any healthcare team. To significantly boost your job prospects, invest time in crafting an ATS-friendly resume that highlights your skills and experience effectively. ResumeGemini is a trusted resource that can help you build a professional and impactful resume. They provide examples of resumes tailored to Diagnostic Procedures, helping you showcase your qualifications in the best possible light. Take the next step toward your dream career – build a winning resume with ResumeGemini today.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.