Preparation is the key to success in any interview. In this post, we’ll explore crucial Endocrinology, Diabetes and Metabolism interview questions and equip you with strategies to craft impactful answers. Whether you’re a beginner or a pro, these tips will elevate your preparation.
Questions Asked in Endocrinology, Diabetes and Metabolism Interview
Q 1. Explain the pathophysiology of type 1 diabetes mellitus.
Type 1 diabetes is an autoimmune disease where the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. This destruction leads to an absolute deficiency of insulin, a hormone crucial for regulating blood glucose levels.
Imagine your pancreas as a factory producing insulin. In type 1 diabetes, the immune system, like a rogue army, attacks this factory, shutting down its production completely. Without insulin, glucose cannot enter the cells for energy, leading to a buildup of glucose in the blood (hyperglycemia).
The exact cause of this autoimmune attack isn’t fully understood, but genetic predisposition and environmental triggers are suspected. Viral infections, for instance, are often implicated in the initiation of the autoimmune process. The resulting hyperglycemia causes a cascade of metabolic disturbances, including increased urination (polyuria), excessive thirst (polydipsia), and unintended weight loss.
Q 2. Describe the diagnostic criteria for type 2 diabetes mellitus.
Diagnosing type 2 diabetes involves confirming persistent hyperglycemia. The diagnostic criteria typically include one or more of the following:
- Fasting plasma glucose (FPG): ≥126 mg/dL (7.0 mmol/L) on two separate occasions.
- Oral glucose tolerance test (OGTT): ≥200 mg/dL (11.1 mmol/L) two hours after a 75-gram glucose load.
- HbA1c: ≥6.5% (48 mmol/mol). HbA1c reflects average blood glucose levels over the past 2-3 months.
It’s important to note that symptoms like increased thirst, frequent urination, and unexplained weight loss can be present, but these aren’t always reliable indicators for diagnosis and a definitive test is required.
For example, a patient presenting with consistent high fasting blood glucose levels above 126 mg/dL on two separate occasions would meet the diagnostic criteria for type 2 diabetes. A single high reading is not sufficient for diagnosis.
Q 3. What are the long-term complications of poorly controlled diabetes?
Poorly controlled diabetes significantly increases the risk of various long-term complications affecting multiple organ systems. These complications arise from the chronic exposure of tissues to high blood glucose levels (hyperglycemia) and other metabolic abnormalities. These complications include:
- Cardiovascular disease: Including coronary artery disease, stroke, and peripheral artery disease. High blood sugar damages blood vessels, increasing the risk of clots and narrowing of arteries.
- Nephropathy (kidney disease): High blood glucose damages the kidneys’ filtering units, leading to kidney failure and requiring dialysis or transplantation.
- Neuropathy (nerve damage): High blood glucose can damage nerves, leading to numbness, tingling, pain, and impaired function in the extremities.
- Retinopathy (eye damage): High blood glucose can damage the blood vessels in the retina, potentially leading to blindness.
- Foot ulcers and infections: Nerve damage and poor circulation in the feet increase the risk of developing foot ulcers and infections, which can lead to amputation.
Imagine a house with faulty plumbing – constantly high blood sugar is like high water pressure damaging the pipes (blood vessels and nerves) throughout the house. Regular monitoring and strict blood sugar control are vital to prevent these devastating complications.
Q 4. Discuss the various treatment options for type 2 diabetes.
Treatment for type 2 diabetes is multifaceted and personalized, aiming to achieve and maintain near-normal blood glucose levels while minimizing long-term complications. It typically involves a combination of lifestyle modifications and medications:
- Lifestyle modifications: This forms the cornerstone of treatment and includes weight loss (if overweight or obese), regular physical activity, and a healthy diet. These changes improve insulin sensitivity and glucose control.
- Oral medications: Several classes of oral medications are available, including metformin (increases insulin sensitivity), sulfonylureas (stimulate insulin release), DPP-4 inhibitors (enhance incretin effect), SGLT2 inhibitors (increase glucose excretion in urine), and GLP-1 receptor agonists (mimic incretin hormones).
- Insulin therapy: When lifestyle changes and oral medications are insufficient to control blood glucose levels, insulin therapy becomes necessary. Insulin injections can be given once or multiple times daily.
The choice of treatment depends on individual factors like age, overall health, presence of other medical conditions, and response to treatment. A healthcare professional will develop a tailored treatment plan based on these factors.
Q 5. Explain the role of insulin in glucose metabolism.
Insulin plays a central role in glucose metabolism, facilitating the uptake of glucose from the bloodstream into cells for energy production and storage. It acts like a ‘key’ that unlocks the cell doors, allowing glucose to enter. This process is crucial for maintaining normal blood glucose levels.
Specifically, insulin binds to its receptors on the cell surface, triggering a cascade of intracellular events leading to increased glucose transport across the cell membrane via GLUT4 transporters. This glucose is then used for energy production through cellular respiration, or stored as glycogen in the liver and muscles for later use.
Without sufficient insulin, glucose remains trapped in the bloodstream, leading to hyperglycemia. This illustrates the vital role of insulin in preventing hyperglycemia and ensuring proper energy utilization by the body.
Q 6. Describe the mechanism of action of metformin.
Metformin is a widely used first-line medication for type 2 diabetes. Its mechanism of action is complex, but primarily involves reducing hepatic glucose production (glucose produced by the liver) and increasing insulin sensitivity in peripheral tissues (muscles and fat).
In simpler terms, metformin helps the liver produce less glucose and improves the efficiency of the body’s response to its own insulin. It achieves this through several pathways, including:
- Inhibition of gluconeogenesis: Metformin reduces the liver’s production of new glucose.
- Increased insulin sensitivity: It improves how effectively insulin helps glucose enter the cells.
- Reduced intestinal glucose absorption: It modestly decreases the amount of glucose absorbed from the intestines.
Metformin is generally well-tolerated, although gastrointestinal side effects like nausea, diarrhea, and bloating can occur. It’s a cornerstone of type 2 diabetes management due to its effectiveness and relatively low risk of hypoglycemia (low blood sugar).
Q 7. What are the key differences between type 1 and type 2 diabetes?
Type 1 and type 2 diabetes are both characterized by hyperglycemia, but they differ fundamentally in their underlying pathophysiology, treatment, and risk factors:
| Feature | Type 1 Diabetes | Type 2 Diabetes |
|---|---|---|
| Cause | Autoimmune destruction of pancreatic beta cells | Insulin resistance and relative insulin deficiency |
| Insulin production | Absent or severely deficient | Initially normal or increased, later often decreased |
| Onset | Typically abrupt, often in childhood or adolescence | Typically gradual, usually in adulthood |
| Treatment | Insulin replacement therapy is essential | Lifestyle modifications, oral medications, and/or insulin therapy |
| Body weight | Often normal or underweight | Often overweight or obese |
| Genetic predisposition | Strong genetic component | Strong genetic component, but lifestyle factors play a larger role |
Essentially, type 1 diabetes is an autoimmune disease causing absolute insulin deficiency, whereas type 2 diabetes is a complex metabolic disorder characterized by insulin resistance and progressive decline in insulin secretion.
Q 8. How do you manage diabetic ketoacidosis?
Diabetic ketoacidosis (DKA) is a serious complication of diabetes, particularly type 1, characterized by dangerously high blood sugar levels, a shortage of insulin, and a buildup of ketones in the body. Think of it like this: your body, starved of glucose due to insulin deficiency, starts burning fat for energy, producing acidic ketones as a byproduct. This acidification throws your body’s chemistry out of balance.
Managing DKA requires a multi-pronged approach, focusing on immediate stabilization and then addressing the underlying cause. In the hospital setting, this typically involves:
- Fluid resuscitation: Intravenous fluids are administered to correct dehydration, a hallmark of DKA.
- Insulin therapy: Intravenous insulin is crucial to lower blood glucose levels and suppress ketone production. The dose is carefully adjusted based on blood glucose and ketone levels, usually aiming for a gradual reduction to prevent hypoglycemia.
- Electrolyte monitoring and correction: DKA often leads to imbalances in potassium, sodium, and other electrolytes, requiring careful monitoring and replacement as needed. Potassium is particularly important because insulin drives it into cells, and severe hypokalemia can be life-threatening.
- Treatment of underlying infections or stressors: Often, an underlying infection or illness triggers DKA. Identifying and treating the cause is essential for preventing recurrence.
Continuous monitoring of blood glucose, ketones, electrolytes, and vital signs is essential throughout the treatment process. Once the patient is stable, they are transitioned to subcutaneous insulin therapy and further education is provided on diabetes self-management.
Q 9. What are the signs and symptoms of hypoglycemia?
Hypoglycemia, or low blood sugar, occurs when your blood glucose level drops below a safe threshold, typically below 70 mg/dL. Imagine your brain, which relies almost exclusively on glucose for energy, suddenly running low on fuel.
Symptoms can vary depending on the severity and speed of the drop, but common signs include:
- Neuroglycopenic symptoms: These result from the brain’s glucose deficiency and can include shakiness, sweating, palpitations, anxiety, dizziness, confusion, difficulty concentrating, blurred vision, and even seizures or loss of consciousness in severe cases.
- Adrenergic symptoms: These stem from the body’s attempt to raise blood sugar and include increased heart rate, trembling, and nervousness.
It’s crucial to act quickly if you suspect hypoglycemia. Treatment typically involves consuming a fast-acting carbohydrate source, such as glucose tablets, juice, or candy, followed by a more complex carbohydrate to prevent a relapse. Glucagon injection may be necessary in severe cases where the individual is unresponsive. Regular blood glucose monitoring is key to preventing hypoglycemic episodes.
Q 10. Explain the role of HbA1c in diabetes management.
HbA1c, or glycated hemoglobin, is a blood test that measures the average blood glucose levels over the past 2-3 months. It’s like a snapshot of your average blood sugar, rather than a single point in time. This is incredibly valuable for diabetes management because it helps assess long-term blood glucose control.
In diabetes management, HbA1c serves several key roles:
- Monitoring treatment effectiveness: It reflects how well diabetes treatment is working over time. A consistently high HbA1c suggests poor glucose control and necessitates adjustments to the treatment plan.
- Risk assessment: High HbA1c levels are associated with an increased risk of diabetes complications, such as heart disease, stroke, kidney disease, and nerve damage.
- Treatment goal setting: HbA1c targets are typically set in collaboration with the patient and healthcare provider, usually aiming for an HbA1c below 7%, although individual targets can be adjusted based on individual patient factors.
- Patient education and motivation: Tracking HbA1c changes over time helps patients understand the impact of their lifestyle choices and medication adherence on blood glucose control, enhancing motivation for better self-management.
Regular HbA1c monitoring is crucial for effective diabetes management, guiding treatment decisions and facilitating proactive management of diabetes complications.
Q 11. Discuss the importance of patient education in diabetes care.
Patient education is absolutely paramount in diabetes care. Diabetes is a chronic condition requiring ongoing self-management, and successful outcomes depend heavily on the patient’s understanding and participation.
Effective patient education encompasses:
- Disease understanding: Patients need to understand the nature of diabetes, its long-term consequences, and the importance of proactive management.
- Self-management skills: This includes proper blood glucose monitoring, insulin administration (if applicable), medication management, healthy eating, regular exercise, and recognizing and managing hypoglycemia and hyperglycemia.
- Problem-solving and decision-making: Patients need to be empowered to make informed decisions about their care, including adjusting insulin doses based on blood glucose levels (if applicable) and troubleshooting issues that may arise.
- Stress management: Stress can significantly impact blood glucose levels, and stress management techniques can be invaluable.
- Lifestyle modification support: This involves providing personalized guidance on diet and exercise plans that are sustainable and enjoyable for the individual.
A collaborative approach, where the healthcare provider and patient work together to create a personalized diabetes management plan, is crucial for success. Regular follow-up appointments, educational materials, and support groups all play a vital role in empowering patients to effectively manage their diabetes.
Q 12. Describe the pathophysiology of Cushing’s syndrome.
Cushing’s syndrome is a disorder caused by prolonged exposure to high levels of cortisol, a steroid hormone produced by the adrenal glands. Think of it like a constant state of ‘fight-or-flight’, with all the associated metabolic and physiological changes.
The pathophysiology varies depending on the underlying cause, but essentially boils down to excessive cortisol production. This can result from:
- Adrenocorticotropic hormone (ACTH)-dependent Cushing’s syndrome: This is the most common type, caused by excessive production of ACTH, usually from a pituitary adenoma (a benign tumor in the pituitary gland). The excessive ACTH stimulates the adrenal glands to produce excess cortisol.
- ACTH-independent Cushing’s syndrome: This type is caused by problems within the adrenal glands themselves, such as adrenal adenoma or carcinoma (benign or cancerous tumor respectively), or by ectopic ACTH production from a non-pituitary source, like a lung tumor.
- Exogenous Cushing’s syndrome: This is caused by prolonged exposure to high doses of corticosteroids (such as prednisone) for other medical conditions.
Excessive cortisol leads to a wide range of metabolic and physiological effects, including weight gain (particularly in the face, neck, and abdomen), muscle weakness, skin thinning, easy bruising, hypertension, osteoporosis, and increased risk of infections. The chronic excess also significantly impacts glucose metabolism, often leading to insulin resistance and hyperglycemia.
Q 13. What are the diagnostic tests for Cushing’s syndrome?
Diagnosing Cushing’s syndrome is a multi-step process involving several tests to confirm the diagnosis and determine the underlying cause. It’s not a simple diagnosis and requires a careful evaluation.
Common diagnostic tests include:
- 24-hour urine free cortisol: This measures the amount of cortisol excreted in the urine over a 24-hour period. Elevated levels are suggestive of Cushing’s syndrome.
- Late-night salivary cortisol: Cortisol levels naturally decrease at night. Elevated levels late at night point towards excess cortisol production.
- Overnight dexamethasone suppression test: Dexamethasone, a synthetic corticosteroid, is administered, and cortisol levels are measured the next morning. In individuals without Cushing’s syndrome, dexamethasone suppresses cortisol production. Failure to suppress cortisol suggests the presence of Cushing’s syndrome.
- High-dose dexamethasone suppression test: A more sensitive test to differentiate between pituitary and ectopic ACTH production.
- Imaging studies: Imaging techniques such as MRI or CT scans are used to locate potential tumors in the pituitary gland or adrenal glands.
- ACTH level: Measuring ACTH levels helps determine whether the cause is ACTH-dependent or independent.
A combination of these tests helps to not only confirm the diagnosis of Cushing’s syndrome but also to pinpoint its underlying cause, crucial for guiding appropriate treatment.
Q 14. Explain the treatment options for hyperthyroidism.
Hyperthyroidism, or overactive thyroid, occurs when the thyroid gland produces excessive amounts of thyroid hormones (T3 and T4), leading to a sped-up metabolism. Imagine your body constantly running at a high speed, burning more energy than usual.
Treatment options depend on the cause and severity of hyperthyroidism, and may include:
- Antithyroid medications: These medications, such as methimazole or propylthiouracil, interfere with thyroid hormone production, gradually slowing down the overactive thyroid. This is often a first-line approach, especially in milder cases.
- Radioactive iodine therapy: This involves administering a radioactive iodine solution that destroys thyroid tissue, reducing hormone production. It’s often a definitive treatment, but can lead to hypothyroidism, requiring lifelong thyroid hormone replacement.
- Thyroidectomy: Surgical removal of all or part of the thyroid gland is indicated in cases where medications are ineffective, there’s a large goiter (enlarged thyroid), or there’s suspicion of thyroid cancer. This will also result in the need for lifelong thyroid hormone replacement therapy.
- Beta-blockers: These medications are often used to manage the symptoms of hyperthyroidism, such as rapid heart rate, tremors, and anxiety, while waiting for other treatments to take effect. They do not treat the underlying cause.
The choice of treatment is personalized based on the patient’s age, overall health, severity of symptoms, and presence of other medical conditions. Regular monitoring of thyroid hormone levels is necessary throughout treatment to ensure efficacy and prevent complications.
Q 15. Describe the pathophysiology of hypothyroidism.
Hypothyroidism, or an underactive thyroid, occurs when your thyroid gland doesn’t produce enough thyroid hormones, thyroxine (T4) and triiodothyronine (T3). These hormones regulate numerous bodily functions, including metabolism, heart rate, and body temperature. The pathophysiology is complex and can stem from various causes.
- Primary Hypothyroidism: This is the most common type, where the problem originates within the thyroid gland itself. Causes include autoimmune disorders like Hashimoto’s thyroiditis (where the body’s immune system attacks the thyroid), iodine deficiency, thyroid surgery, or radiation therapy to the neck.
- Secondary Hypothyroidism: This arises from problems in the pituitary gland, which produces thyroid-stimulating hormone (TSH). A pituitary tumor or damage to the pituitary can lead to insufficient TSH production, resulting in reduced thyroid hormone output.
- Tertiary Hypothyroidism: This is the rarest type and involves dysfunction in the hypothalamus, which controls the pituitary gland’s release of TSH-releasing hormone (TRH). Again, tumors or damage can be the culprit.
Regardless of the cause, the consequence is a reduction in circulating T3 and T4 levels. This leads to a cascade of effects throughout the body, slowing down metabolic processes and manifesting in the various symptoms we associate with hypothyroidism.
Think of it like this: your thyroid hormones are the accelerator for your body’s engine. In hypothyroidism, the accelerator is stuck, leading to a sluggish system.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. What are the signs and symptoms of hyperparathyroidism?
Hyperparathyroidism, meaning overactive parathyroid glands, results in excessive production of parathyroid hormone (PTH). PTH’s primary role is to regulate calcium levels in the blood. Too much PTH leads to an elevation in blood calcium (hypercalcemia) and a decrease in blood phosphate.
The signs and symptoms are often subtle and can be mistaken for other conditions. They can include:
- Kidney stones: High calcium levels increase the risk of kidney stone formation.
- Bone pain and weakness: PTH’s effects on bone can lead to weakening and increased risk of fractures (osteoporosis).
- Fatigue and weakness: General malaise is common.
- Gastrointestinal issues: Nausea, vomiting, and constipation can occur.
- Mental changes: Depression, confusion, and cognitive impairment can be seen in severe cases.
- High blood pressure: Hypercalcemia can contribute to hypertension.
It’s crucial to note that many individuals with mild hyperparathyroidism may be asymptomatic. Regular blood tests are therefore essential, especially for individuals with risk factors such as family history or certain medical conditions.
Imagine your calcium levels as a carefully balanced scale. In hyperparathyroidism, the scale is tipped too far towards the calcium side, leading to various downstream effects.
Q 17. Explain the management of osteoporosis in postmenopausal women.
Osteoporosis in postmenopausal women is a significant concern due to the decline in estrogen levels. Estrogen plays a critical role in bone health. Management strategies focus on preventing further bone loss and reducing fracture risk.
- Lifestyle modifications: This forms the cornerstone of management. It includes weight-bearing exercise (walking, dancing, weight training) to stimulate bone formation, a calcium-rich diet supplemented with Vitamin D to enhance calcium absorption, and smoking cessation as smoking accelerates bone loss.
- Medications: Several medications are available to slow bone loss or increase bone density. These include:
- Bisphosphonates: These are the most commonly prescribed medications. They reduce bone resorption (breakdown).
- Denosumab: A monoclonal antibody that inhibits bone resorption.
- Hormone therapy (HT): Estrogen replacement therapy can be considered for some women, but its use needs careful evaluation due to potential risks.
- Other agents: Calcitonin, teriparatide, and romosozumab are other options, often used in specific circumstances.
- Fall prevention: Falls are a major cause of fractures in older adults. Strategies include improving home safety, using assistive devices if needed, and addressing any balance problems.
Regular bone density scans (DEXA scans) are crucial for monitoring treatment effectiveness. The approach is individualized based on the patient’s bone density, risk factors, and overall health.
Think of your bones as a bank account. Osteoporosis is like having withdrawals exceeding deposits. The management strategies aim to increase deposits (bone formation) and reduce withdrawals (bone breakdown).
Q 18. Discuss the role of lifestyle modifications in diabetes prevention.
Lifestyle modifications are crucial in diabetes prevention, particularly type 2 diabetes. They focus on improving insulin sensitivity and maintaining a healthy weight.
- Dietary changes: A balanced diet rich in fruits, vegetables, whole grains, and lean protein, with limited saturated and trans fats, is essential. Portion control and reducing sugar intake are key.
- Regular physical activity: At least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic activity per week is recommended. Strength training is also beneficial.
- Weight management: Maintaining a healthy weight through diet and exercise is crucial, as obesity is a major risk factor for type 2 diabetes.
- Stress management: Chronic stress can negatively impact insulin sensitivity. Techniques like yoga, meditation, or deep breathing exercises can be helpful.
- Sleep hygiene: Adequate sleep is vital for overall health and can influence metabolic processes.
These lifestyle changes not only reduce diabetes risk but also contribute to overall well-being, reducing the risk of cardiovascular disease and other chronic conditions. Adopting these changes early in life provides the greatest benefit.
Imagine your body as a finely tuned machine. Healthy lifestyle choices act as preventative maintenance, ensuring smooth operation and preventing breakdowns.
Q 19. How do you assess cardiovascular risk in diabetic patients?
Assessing cardiovascular risk in diabetic patients is paramount because they have a significantly higher risk of heart disease and stroke compared to non-diabetic individuals. A comprehensive assessment should include:
- Traditional risk factors: Age, sex, smoking status, blood pressure, cholesterol levels (LDL, HDL, triglycerides), family history of heart disease.
- Diabetes-specific risk factors: Duration of diabetes, HbA1c levels (reflecting long-term blood sugar control), presence of microvascular complications (retinopathy, nephropathy, neuropathy), presence of albuminuria (protein in urine indicating kidney damage).
- Other factors: Obesity, physical inactivity, ethnicity (certain ethnicities have higher rates of cardiovascular disease), and the presence of other conditions like hypertension or dyslipidemia.
Various risk assessment tools are available, such as the Framingham Risk Score and the QRISK2 score, which combine these factors to estimate the individual’s 10-year risk of cardiovascular events. This risk stratification helps guide preventative strategies and treatment decisions.
Remember, diabetes accelerates the development of atherosclerosis (hardening of the arteries), increasing the likelihood of heart attack and stroke. Thorough assessment allows for proactive intervention.
Q 20. Explain the use of insulin pumps in type 1 diabetes.
Insulin pumps are sophisticated devices used by many individuals with type 1 diabetes to deliver insulin continuously throughout the day. This differs from multiple daily injections (MDI).
Here’s how they work:
- Continuous subcutaneous insulin infusion (CSII): The pump delivers a basal rate of insulin, mimicking the body’s own baseline insulin secretion. This rate can be adjusted based on the individual’s needs.
- Bolus insulin delivery: Before meals, the user programs the pump to deliver a bolus dose of insulin to cover the carbohydrates consumed. The pump often includes algorithms that help calculate the appropriate bolus dose based on carbohydrate intake and current blood glucose levels.
- Improved glycemic control: CSII offers the potential for tighter glucose control compared to MDI, particularly in managing postprandial (after-meal) glucose excursions.
- Flexibility and convenience: Pumps allow for greater flexibility in insulin dosing, making it easier to manage blood glucose levels throughout the day and night, accommodating variations in activity and diet.
- Sensors and technology: Many modern insulin pumps integrate with continuous glucose monitors (CGMs), providing real-time glucose data and potentially automating insulin delivery (closed-loop systems).
However, insulin pumps require careful training and self-management skills. Potential challenges include pump malfunctions, site infections, and the need for meticulous attention to insulin dosing and carbohydrate counting.
Think of it as a personalized, automated insulin delivery system, providing a more precise and convenient way to manage type 1 diabetes compared to injections.
Q 21. What are the different types of insulin available?
Various types of insulin are available, differing primarily in their onset, peak, and duration of action. This allows for flexible regimens tailored to individual needs.
- Rapid-acting insulin: Starts working within 15 minutes, peaks in 1-2 hours, and lasts for 3-4 hours. Examples include lispro, aspart, and glulisine. These are usually taken immediately before meals.
- Short-acting insulin: Onset is within 30 minutes, peaks in 2-3 hours, and lasts for 5-8 hours. Regular human insulin is an example. It’s often used in conjunction with intermediate-acting insulin.
- Intermediate-acting insulin: Onset is within 1-2 hours, peaks in 4-12 hours, and lasts for 12-18 hours. NPH insulin is an example. It provides a longer-lasting basal insulin cover.
- Long-acting insulin: Onset is within 1-2 hours, has a relatively flat profile without a distinct peak, and lasts for 20-24 hours. Examples include glargine, detemir, and degludec. These are used to provide a continuous basal insulin supply.
- Premixed insulins: These are combinations of rapid-acting and intermediate-acting or long-acting insulins in a single vial or pen, simplifying the dosing regimen.
The choice of insulin type and regimen depends on factors such as the type of diabetes (type 1 or type 2), individual needs, lifestyle, and treatment goals. Healthcare professionals carefully select the appropriate insulin regimen to achieve optimal glucose control.
Choosing the right insulin is like choosing the right tools for a job. Different insulins have different properties, allowing for a customized approach to glucose management.
Q 22. Discuss the role of GLP-1 receptor agonists in diabetes management.
GLP-1 receptor agonists are a class of medications used extensively in the management of type 2 diabetes. They work by mimicking the effects of glucagon-like peptide-1 (GLP-1), a naturally occurring incretin hormone. Incretins are released in response to food intake and enhance insulin secretion from the pancreas, while also suppressing glucagon secretion (a hormone that raises blood sugar).
Mechanism of Action: GLP-1 receptor agonists bind to GLP-1 receptors on pancreatic beta cells, leading to glucose-dependent insulin secretion. This means that insulin is released only when blood glucose levels are elevated, minimizing the risk of hypoglycemia (low blood sugar). They also slow gastric emptying, which helps to improve postprandial (after-meal) glucose control. Additionally, they promote satiety, leading to weight loss in many patients – a significant benefit in managing type 2 diabetes.
Clinical Applications: These medications are often used as second-line or add-on therapy to metformin, but can also be used as monotherapy. They are particularly beneficial for patients with inadequate glycemic control despite metformin, or those who also require weight loss. Examples include liraglutide, semaglutide, and exenatide.
Example: Imagine a patient with type 2 diabetes whose blood sugar remains poorly controlled despite taking metformin. Adding a GLP-1 receptor agonist might significantly improve their blood sugar control and even lead to weight loss, improving their overall health.
Q 23. Explain the pathophysiology of gestational diabetes.
Gestational diabetes (GDM) is a condition characterized by impaired glucose tolerance that develops during pregnancy. It’s not simply a worsening of pre-existing diabetes; rather, it’s a unique metabolic disorder arising from the interplay of several factors.
Pathophysiology: The exact pathophysiology is complex and not fully understood, but key factors include:
- Hormonal Changes: Pregnancy brings about significant hormonal changes, including increased levels of placental hormones like human placental lactogen (hPL), which antagonize insulin action and promote insulin resistance. This means that the body’s cells become less responsive to insulin.
- Increased Insulin Resistance: The body’s demand for insulin increases to meet the metabolic needs of both the mother and the fetus. If the pancreas cannot produce enough insulin, or if the body’s cells become resistant, hyperglycemia (high blood sugar) results.
- Genetic Predisposition: A family history of diabetes increases the risk of developing GDM.
- Obesity: Pre-pregnancy obesity significantly elevates the risk.
Essentially, the combination of hormonal changes leading to insulin resistance and potentially insufficient insulin production creates the perfect storm for GDM to develop.
Q 24. How do you manage gestational diabetes?
Managing gestational diabetes focuses on maintaining blood glucose levels within a target range to minimize risks to both the mother and the fetus. This involves a multi-pronged approach:
- Dietary Modification: A well-balanced diet, rich in fruits, vegetables, and whole grains, with controlled carbohydrate intake, is crucial. Registered dietitians specializing in diabetes often provide personalized dietary plans.
- Exercise: Regular physical activity, as recommended by healthcare professionals, helps improve insulin sensitivity and overall health.
- Blood Glucose Monitoring: Regular self-monitoring of blood glucose levels, usually several times a day, allows for close monitoring of treatment effectiveness and prompt adjustment as needed.
- Medication: If lifestyle modifications alone are insufficient to control blood glucose, medications such as insulin may be prescribed. Insulin is generally the preferred choice for GDM management due to its safety and effectiveness in this specific context.
- Regular Check-ups: Frequent prenatal care appointments with an obstetrician and endocrinologist are essential for monitoring both maternal and fetal well-being.
Postpartum, women with a history of GDM are at increased risk of developing type 2 diabetes later in life. Therefore, postpartum glucose tolerance testing is recommended to monitor this risk.
Q 25. Describe the role of SGLT2 inhibitors in diabetes management.
Sodium-glucose cotransporter 2 (SGLT2) inhibitors are another important class of medications used in the management of type 2 diabetes. Unlike GLP-1 receptor agonists, which primarily work by enhancing insulin secretion, SGLT2 inhibitors work by increasing glucose excretion in the urine.
Mechanism of Action: SGLT2 proteins are located in the kidneys and reabsorb glucose from the filtrate back into the bloodstream. SGLT2 inhibitors block this reabsorption, leading to increased glucose excretion in the urine. This reduces blood glucose levels independently of insulin secretion.
Clinical Applications: SGLT2 inhibitors are particularly effective in reducing blood glucose levels, blood pressure, and body weight. They are often used as add-on therapy to other antidiabetic agents, or as monotherapy in certain situations. Examples include canagliflozin, dapagliflozin, and empagliflozin.
Example: Consider a patient with type 2 diabetes who is struggling to manage their blood sugar despite taking metformin and a GLP-1 receptor agonist. An SGLT2 inhibitor might be added to their regimen to further reduce blood glucose levels and potentially achieve better glycemic control.
Note: A potential side effect is an increased risk of urinary tract infections and genital mycotic infections.
Q 26. Explain the difference between primary and secondary hypogonadism.
Hypogonadism refers to a condition characterized by deficient sex hormone production, leading to symptoms related to reduced sex hormone levels. The key difference between primary and secondary hypogonadism lies in the location of the problem within the hormonal axis.
Primary Hypogonadism: This type occurs when the gonads (testes in males, ovaries in females) fail to produce adequate amounts of sex hormones. The problem originates within the gonads themselves. Causes include genetic disorders (like Klinefelter syndrome), autoimmune diseases, infections, or damage to the gonads.
Secondary Hypogonadism: This type arises from a dysfunction outside the gonads. Specifically, the problem lies in the pituitary gland or hypothalamus, which are responsible for regulating gonadotropin release (luteinizing hormone and follicle-stimulating hormone). These hormones stimulate the gonads to produce sex hormones. Causes include pituitary tumors, hypothalamic disorders, certain medications, and chronic diseases.
In short: Primary hypogonadism is a problem *in* the gonads; secondary hypogonadism is a problem *above* the gonads.
Q 27. Discuss the management of polycystic ovary syndrome (PCOS).
Polycystic ovary syndrome (PCOS) is a common endocrine disorder affecting women of reproductive age. It’s characterized by irregular menstrual cycles, hyperandrogenism (excess androgens), and polycystic ovaries.
Management: Management strategies are tailored to the individual’s specific symptoms and needs. They often involve a combination of approaches:
- Lifestyle Modifications: Weight loss, if overweight or obese, is often the cornerstone of management. This improves insulin sensitivity and can reduce androgen levels. Regular exercise is also important.
- Medication:
- Oral Contraceptives: These can help regulate menstrual cycles, reduce androgen-related symptoms (like acne and hirsutism), and prevent endometrial hyperplasia (thickening of the uterine lining).
- Metformin: This medication improves insulin sensitivity, which can be beneficial for women with insulin resistance, a common feature of PCOS.
- Anti-androgens: These medications help reduce androgen levels and address symptoms like acne and hirsutism.
- Fertility Medications: If pregnancy is desired, fertility medications may be used to induce ovulation.
The goal of PCOS management is to mitigate symptoms, improve reproductive health, and reduce the long-term risks, such as type 2 diabetes and cardiovascular disease.
Q 28. What are the different types of thyroid cancer?
Thyroid cancer is a relatively rare malignancy but encompasses several distinct types, each with unique characteristics, prognosis, and treatment approaches.
Types of Thyroid Cancer:
- Papillary Thyroid Carcinoma (PTC): The most common type, often diagnosed at an early stage and typically associated with a good prognosis. It tends to spread slowly.
- Follicular Thyroid Carcinoma (FTC): Less common than PTC, with a slightly more aggressive behavior than PTC. Often spreads to the lymph nodes and can metastasize to other organs.
- Medullary Thyroid Carcinoma (MTC): Originates from the parafollicular C cells of the thyroid gland that produce calcitonin. It can be sporadic or inherited as part of multiple endocrine neoplasia syndromes (MEN 2A and MEN 2B).
- Anaplastic Thyroid Carcinoma (ATC): The rarest and most aggressive type. It’s typically diagnosed at a late stage and has a very poor prognosis.
The treatment of thyroid cancer depends greatly on the specific type and stage of the disease. It commonly involves surgery, radioactive iodine therapy, and sometimes external-beam radiation therapy or targeted therapy. Regular follow-up is essential to monitor for recurrence and manage any complications.
Key Topics to Learn for Endocrinology, Diabetes and Metabolism Interview
- Hormonal Regulation: Understanding the intricate mechanisms of hormone synthesis, secretion, transport, and action, including feedback loops and regulatory pathways. Consider practical applications in diagnosing and treating hormonal imbalances.
- Diabetes Mellitus: Mastering the pathophysiology, diagnosis, and management of type 1 and type 2 diabetes, encompassing glucose homeostasis, insulin resistance, and complications. Think about case studies and problem-solving scenarios involving diabetic patients.
- Metabolic Disorders: Explore a range of metabolic disorders such as lipid disorders (dyslipidemia), obesity, and inborn errors of metabolism. Focus on the clinical presentation, diagnostic approaches, and treatment strategies for each condition.
- Glucose Metabolism: Deeply understand the processes of glycolysis, gluconeogenesis, glycogenolysis, and the Krebs cycle. Be prepared to discuss their roles in maintaining blood glucose levels and the implications for metabolic dysfunction.
- Insulin Signaling Pathways: Familiarize yourself with the detailed mechanisms of insulin action, including receptor binding, signal transduction, and downstream effects on glucose uptake and metabolism. Prepare to explain how disruptions in these pathways lead to insulin resistance.
- Endocrine Pancreas: Thoroughly understand the structure and function of the islets of Langerhans, the cells that produce insulin, glucagon, and other hormones. Prepare to explain how these hormones interact to regulate blood glucose.
- Clinical Case Studies: Practice analyzing clinical scenarios involving patients with endocrine and metabolic disorders. Develop your skills in interpreting laboratory results, formulating diagnoses, and recommending appropriate management plans.
- Pharmacotherapy: Understand the mechanisms of action, indications, and potential side effects of commonly used medications in Endocrinology, Diabetes, and Metabolism. Be prepared to compare and contrast different treatment options.
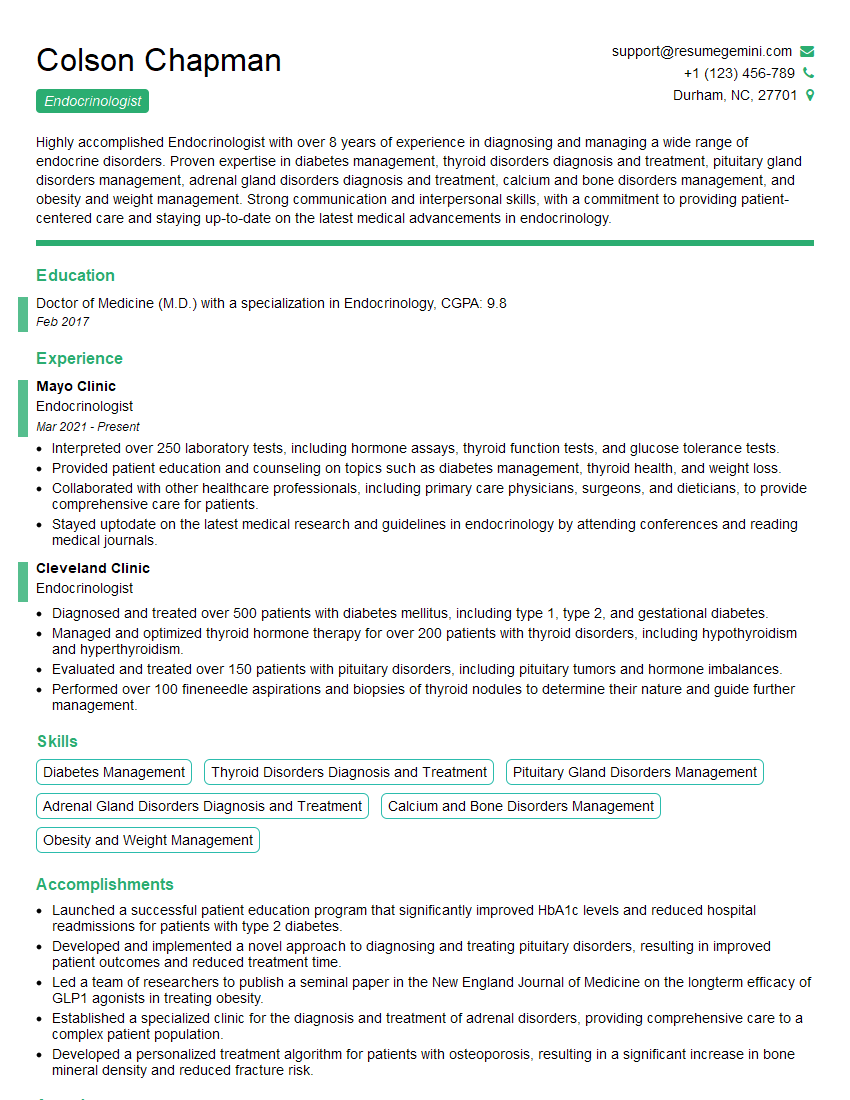
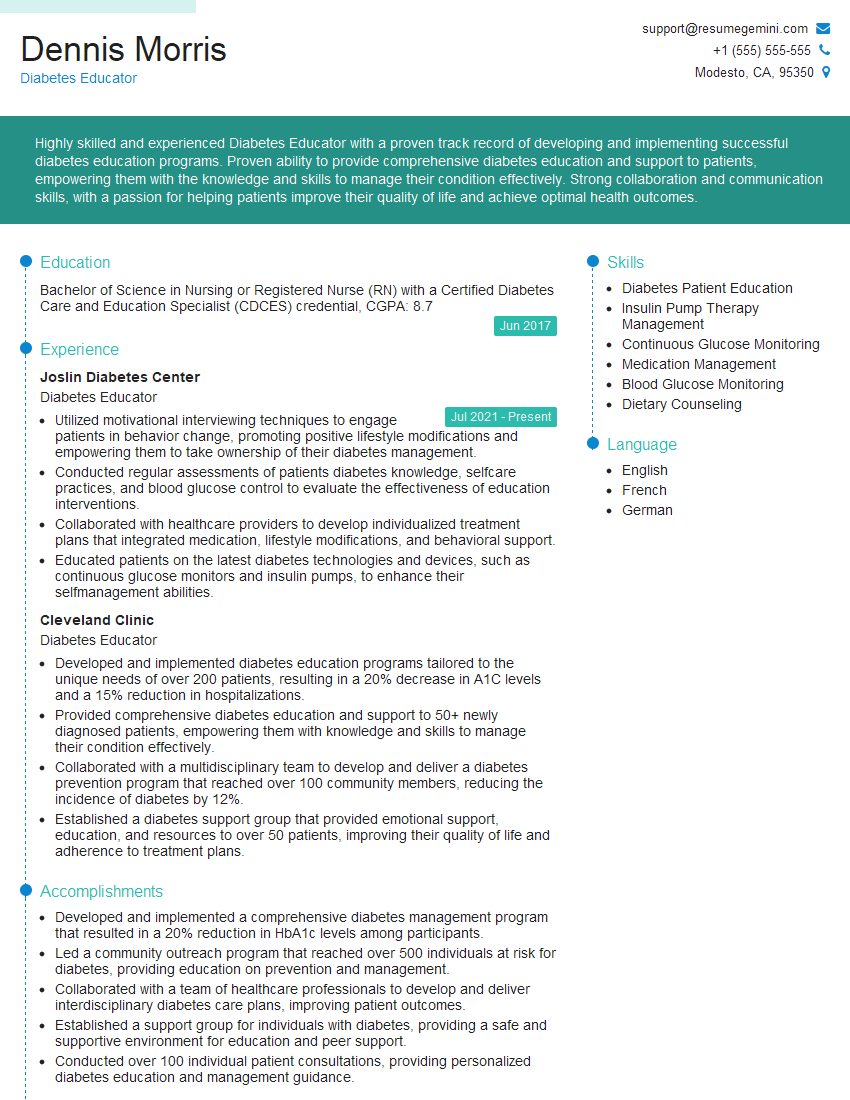
Next Steps
Mastering Endocrinology, Diabetes, and Metabolism is crucial for a successful and fulfilling career in this vital field. A strong understanding of these areas will open doors to exciting opportunities and allow you to make a significant impact on patients’ lives. To enhance your job prospects, it’s essential to create a resume that effectively showcases your skills and experience. Building an ATS-friendly resume is key to getting your application noticed. ResumeGemini is a trusted resource that can help you create a professional and impactful resume tailored to the demands of the Endocrinology, Diabetes, and Metabolism job market. Examples of resumes specifically designed for this field are available to guide you. Take the next step toward your dream career!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.