Cracking a skill-specific interview, like one for Endoscopic Suturing, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Endoscopic Suturing Interview
Q 1. Describe your experience with different endoscopic suturing techniques.
My experience encompasses a wide range of endoscopic suturing techniques, from the simpler interrupted and continuous sutures to more advanced methods like extracorporeal suturing and the use of specialized devices. I’m proficient in using various endoscopic suturing instruments, including linear staplers, endoscopic suturing devices (e.g., Endo-GIA, ProTack), and manual suturing techniques with different needle holders and forceps. For instance, in repairing a colonic perforation, I might utilize a continuous running suture with absorbable material for speed and ease of handling, while a complex esophageal anastomosis might require meticulously placed individual interrupted sutures with non-absorbable material for strength and precision.
- Interrupted sutures: Provide individual stitches offering precise placement and control, ideal for complex repairs.
- Continuous sutures: Faster technique but less precise, suitable for simpler linear repairs.
- Extracorporeal suturing: The tissue is brought outside the body for suturing before being returned to the abdominal cavity. Useful in cases where precise placement or tensioning is crucial.
Q 2. What are the advantages and disadvantages of different suture materials used in endoscopic suturing?
The choice of suture material significantly impacts the outcome of an endoscopic suturing procedure. The ideal material depends on factors such as tissue type, tension requirements, and the desired absorption rate.
- Absorbable sutures (e.g., Vicryl, PDS): These are gradually absorbed by the body, minimizing the need for removal. Advantages include reduced risk of infection and decreased foreign body reaction. However, they might not provide the same strength as non-absorbable sutures, particularly in areas of high tension.
- Non-absorbable sutures (e.g., silk, polypropylene): These retain their strength for a longer period and are ideal for areas requiring strong tensile support, such as anastomoses. They require removal, which carries its own risks. Examples include repairs of large bowel perforations where strength is paramount.
For example, I might use absorbable sutures for closing a small bowel perforation where the tissue heals quickly and strength isn’t a primary concern. Conversely, in a high-tension esophageal anastomosis, I would opt for a non-absorbable suture to ensure the integrity of the repair.
Q 3. Explain your approach to managing bleeding complications during endoscopic suturing.
Managing bleeding during endoscopic suturing is crucial. My approach involves a combination of proactive measures and immediate responses to bleeding episodes. Proactively, this includes careful dissection to minimize tissue trauma, using appropriate hemostatic agents (e.g., surge sponges, coagulation devices), and selecting appropriately sized sutures to avoid excessive tension on the tissue.
If bleeding occurs, I’ll first try to identify the bleeding source using endoscopic visualization. Then, I’ll employ techniques like direct pressure with a sponge, application of clips or cautery, or precise placement of additional sutures to control the bleeding. In more severe cases, surgical intervention might be necessary. For example, if a significant vessel is injured, endoscopic clips or a specialized endoscopic sealant might be needed. I always prioritize minimal tissue trauma and effective hemostasis to prevent complications.
Q 4. How do you select appropriate suture size and type for various endoscopic procedures?
Suture selection is crucial. The size and type of suture depend on the tissue thickness, tension at the surgical site, and the nature of the procedure. Thicker tissues require larger sutures, and areas under high tension need stronger sutures.
For instance, I might use a 3-0 or 4-0 absorbable suture for delicate tissues like the small bowel, while a 2-0 or even larger non-absorbable suture might be necessary for a thick-walled colon. The choice between monofilament (e.g., polypropylene) and braided (e.g., silk) sutures also depends on the specific situation. Monofilament sutures are less likely to harbor bacteria, making them suitable for infected areas, while braided sutures are generally easier to handle.
Q 5. Describe your experience with endoscopic suturing in complex anatomical locations.
I have extensive experience with endoscopic suturing in challenging anatomical locations such as the distal esophagus, the rectosigmoid colon, and the duodenal bulb. These areas present unique challenges due to their proximity to vital structures and often limited visibility. Careful planning, meticulous technique, and the use of specialized instruments are crucial for success in these situations. For example, performing an endoscopic suturing of a duodenal perforation demands precise placement and attention to avoid injury to adjacent pancreatic ducts or blood vessels. I might use a combination of techniques such as clips and sutures to ensure proper hemostasis.
Q 6. What are the common challenges you encounter during endoscopic suturing, and how do you address them?
Common challenges include limited visualization, tissue fragility, and the difficulty of manipulating instruments within a confined space. I address these using a combination of approaches. Improving visualization often involves adjusting the endoscopic camera angle, using different endoscopic lenses, or employing advanced imaging techniques. To handle tissue fragility, I use delicate instruments and minimally invasive techniques, taking care to avoid excessive traction. Difficulty with instrument manipulation is overcome through experience, the use of specialized instruments designed for endoscopic suturing, and, in some cases, the assistance of a surgical assistant.
Q 7. Explain the steps involved in performing an endoscopic suturing procedure.
The steps involved in an endoscopic suturing procedure vary based on the specific procedure and anatomical location, but a general framework includes:
- Preparation: This involves bowel preparation (if necessary), appropriate patient positioning, and setting up the endoscopic equipment.
- Endoscopic examination: A thorough endoscopic examination is conducted to assess the extent of the injury or defect.
- Suturing: The chosen suturing technique (interrupted, continuous, etc.) is implemented using the appropriate instruments and suture material.
- Hemostasis: Bleeding is controlled using appropriate methods (e.g., clips, cautery, sutures).
- Final assessment: A final endoscopic examination is performed to ensure complete closure and the absence of bleeding.
- Post-procedure care: This includes monitoring for complications and providing appropriate post-operative instructions to the patient.
For example, in a simple case of a small bowel perforation, the steps might be completed relatively quickly, while a complex esophageal anastomosis would require a more extended and meticulous approach.
Q 8. How do you ensure proper knot security during endoscopic suturing?
Ensuring knot security in endoscopic suturing is paramount to prevent leakage, bleeding, or suture failure. It’s a multi-step process that starts even before the first stitch. We begin by selecting the appropriate suture material and needle type for the tissue involved. For instance, a delicate tissue like the bowel requires a smaller, atraumatic needle and a absorbable suture like PDS or Vicryl. For a thicker tissue, like the stomach wall, we might choose a larger needle and a non-absorbable suture such as polypropylene.
The knot itself is crucial. We typically use a surgical knot, often a square knot or a modified version that provides enhanced security. A square knot is created with two half-hitches, ensuring that each half-hitch is firmly tightened, avoiding any slack. A surgeon will use instruments to pull the knot tightly while carefully avoiding undue tension on the tissues.
Finally, we carefully bury the knot within the tissue layer and check for any loose strands or areas that could lead to slippage. It’s akin to tying a strong, secure knot in a rope – the more carefully you tie it, the more it will hold. Careful attention to detail and experience are essential for consistent knot security.
Q 9. How do you handle suture breakage or knot slippage during a procedure?
Suture breakage or knot slippage during an endoscopic procedure is a serious complication requiring immediate attention. The first step is to assess the situation – where the breakage has occurred and the extent of the problem. If it’s a minor issue, say, a single suture breaking in a non-critical location, we may be able to reinforce the area with additional stitches. This will depend on the location and the nature of the repair that is necessary.
However, if the breakage leads to significant leakage (e.g., a bowel perforation), or a more extensive failure, prompt action is critical. We will switch from a traditional knot-tying technique to a more robust method, such as using a knot pusher which secures the knot extra-luminally for more control and less friction. In some situations, we might need to convert to an open surgical procedure for a more thorough repair.
Prevention is always better than cure. We diligently inspect all equipment and suture material prior to the procedure, maintain appropriate tension on the tissues, and use techniques that minimize tissue trauma and friction to decrease the likelihood of suture breakage.
Q 10. Describe your experience with different types of endoscopic suturing devices.
My experience encompasses a wide range of endoscopic suturing devices, from simple manual needle-passing instruments to advanced robotic systems. I’ve extensively used various types of needle-holders, graspers, and knot-pushers. For instance, I’m proficient with both articulating and non-articulating instruments, choosing the one best suited to the anatomical location and procedure complexity.
I have extensive experience with linear staplers, which are invaluable for creating anastomoses (connections between two structures) – especially when closing off intestinal segments during a colectomy. These staplers provide rapid and efficient closure and minimal trauma to the surrounding tissues, compared to traditional suture techniques.
I’m also familiar with newer technologies incorporating advanced imaging and haptic feedback systems which enhances precision and reduces the need for additional instruments which can lead to better patient outcomes.
Q 11. What are the indications and contraindications for endoscopic suturing?
Endoscopic suturing finds its application in a variety of procedures, especially those involving the gastrointestinal tract. Indications include repairing perforations (holes) in the bowel or stomach, closing fistulas (abnormal connections between organs), managing bleeding ulcers, performing anastomoses in cases of bowel resection, and treating various types of injuries or perforations.
However, contraindications exist, too. Severe inflammation, infection, or significant tissue fragility may make endoscopic suturing unsuitable, as it could lead to further complications. Active bleeding can also be a contraindication, unless it can be controlled to a manageable level before suturing is attempted. In situations where a large defect or extensive damage exists, open surgery would be a more appropriate approach.
Each case is carefully evaluated, weighing the benefits and risks of endoscopic suturing before proceeding.
Q 12. How do you assess the success of an endoscopic suturing procedure?
Assessing the success of an endoscopic suturing procedure involves a multi-faceted approach. Immediate post-procedure imaging, such as fluoroscopy or endoscopy, is crucial to visually confirm the integrity of the suture line and ensure there’s no leakage or bleeding. We check for any air or contrast material leak to confirm that the closure is complete and successful.
Beyond the immediate post-operative phase, follow-up endoscopies or imaging studies at regular intervals are necessary to evaluate the healing process. The patient’s clinical status, such as the absence of pain, fever, or signs of infection, also plays a vital role in assessing the overall success of the procedure. Ultimately, the absence of complications and successful healing of the sutured area defines a successful outcome.
Q 13. Describe your experience with post-procedural care related to endoscopic suturing.
Post-procedural care is crucial for a successful outcome after endoscopic suturing. It involves careful monitoring of the patient’s vital signs, pain management, and vigilant observation for signs of complications such as infection, bleeding, or leakage. We may prescribe antibiotics, pain relievers, and sometimes a clear liquid diet initially, gradually progressing to a regular diet as the patient’s condition improves.
Regular follow-up appointments are scheduled for wound assessment and to monitor healing. Patients are educated on recognizing any potential complications and advised on when to seek immediate medical attention. This collaborative approach, combining medical expertise and patient education, is key to successful recovery.
Q 14. How do you maintain sterility and prevent infection during endoscopic suturing procedures?
Maintaining sterility and preventing infection during endoscopic suturing procedures is of paramount importance. We adhere strictly to established protocols for surgical asepsis, beginning with thorough hand hygiene and the use of sterile gloves, gowns, and instruments. The endoscopic equipment is meticulously sterilized using appropriate methods before and after each procedure. The operating room environment is maintained in a sterile condition, and all personnel follow strict sterile techniques.
Prophylactic antibiotics are often administered pre-operatively to reduce the risk of infection, and the choice of antibiotic is tailored to the patient’s individual risk factors and the specific procedure. Post-operatively, careful wound care, diligent monitoring for signs of infection, and prompt administration of antibiotics if an infection is suspected are all essential to minimize the risk of post-procedural infection.
Q 15. Explain your understanding of endoscopic suturing in the context of minimally invasive surgery.
Endoscopic suturing is a revolutionary technique within minimally invasive surgery (MIS). It allows surgeons to perform complex repairs and reconstructions inside the body through small incisions, using specialized instruments and a camera to visualize the surgical field. Instead of large, open incisions, we access the target area through natural orifices or very small incisions, significantly reducing patient trauma, pain, and recovery time. This is particularly beneficial in procedures involving delicate organs like the gastrointestinal tract, lungs, or heart.
For example, in a case of a gastrointestinal perforation, endoscopic suturing allows us to close the perforation directly, avoiding the need for a major laparotomy (open abdominal surgery). This translates to less blood loss, reduced risk of infection, shorter hospital stays, and improved cosmetic outcomes for the patient.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you manage patient discomfort and pain during and after endoscopic suturing procedures?
Managing patient discomfort is paramount in endoscopic suturing. We use a multi-modal approach. This starts with pre-operative counseling and education to set realistic expectations. Then, appropriate anesthesia techniques, including sedation and analgesia, are chosen to ensure the patient remains comfortable during the procedure. Post-operatively, pain management strategies focus on a combination of analgesics, often tailored to the individual patient’s needs. Regular pain assessments, close monitoring for complications like bleeding or infection that could exacerbate pain, and promptly addressing any issues are crucial. We frequently utilize non-opioid pain management strategies, like NSAIDS and regional anesthesia, to minimize side effects.
For instance, a patient undergoing an endoscopic suturing for a colonic perforation might receive a combination of intravenous analgesics during the procedure and then transition to oral pain medication post-procedure, supplemented by regular follow-up appointments to assess pain levels and adjust the medication plan accordingly.
Q 17. Describe your experience with the use of endoscopic ultrasound (EUS) in conjunction with suturing.
Endoscopic ultrasound (EUS) is an invaluable tool when combined with endoscopic suturing. EUS provides high-resolution images of the tissues in the area, allowing for precise localization of lesions or perforations. This accurate visualization is especially crucial in complex cases where the anatomy is distorted or the location of the target tissue is challenging to identify using standard endoscopy. EUS guidance ensures the placement of sutures is accurate and minimizes the risk of unintended damage to surrounding structures.
For example, in a patient with a difficult-to-reach perforation, EUS can pinpoint its exact location, guiding the insertion of the suturing device and allowing for precise repair. In situations involving deep lesions or those hidden behind other structures, EUS allows for safe and effective suturing, improving surgical outcomes.
Q 18. What are the potential complications associated with endoscopic suturing?
Although endoscopic suturing is generally safe, potential complications can occur. These include perforation (a hole in the organ), bleeding, infection, suture failure (the sutures not holding), and adverse reactions to anesthesia. Other less frequent but serious complications can include injury to adjacent structures, such as blood vessels or nerves. The occurrence of these complications is significantly reduced through meticulous technique, thorough pre-procedural planning, and careful post-operative monitoring.
For instance, bleeding can be managed with immediate endoscopic hemostasis techniques or, if severe, potentially requiring a surgical intervention. Infection is mitigated by rigorous aseptic techniques and the use of prophylactic antibiotics where appropriate.
Q 19. How do you prevent perforation during endoscopic suturing?
Preventing perforation during endoscopic suturing is a top priority. This is achieved through a combination of meticulous technique, utilizing appropriate instruments, and careful tissue handling. Precise visualization via high-quality endoscopy and EUS, when necessary, is paramount. We always use the smallest possible needle and suture size appropriate for the tissue strength. Understanding the tissue characteristics and potential fragility is also important. Slow, deliberate suturing avoids unnecessary trauma to the tissue. The use of appropriately sized instruments minimizes the risk of accidental perforation.
For instance, in suturing a friable (easily torn) tissue, we might use smaller needles and absorbable sutures that minimise inflammation and promote tissue healing, minimizing the chance of perforation.
Q 20. Explain the importance of proper tissue handling during endoscopic suturing.
Proper tissue handling is fundamental to successful endoscopic suturing. Gentle manipulation of the tissues avoids unnecessary trauma and minimizes the risk of perforation and bleeding. Using appropriate grasping forceps and avoiding excessive traction are key. Adequate exposure of the surgical field is vital for precision and careful assessment of the tissue planes. We need to be mindful of the tissue’s fragility and avoid causing unnecessary tears or disruptions during the procedure.
For example, when closing a perforation in a hollow organ, we must ensure that the tissue edges are properly approximated before placing the sutures to prevent leakage and ensure effective repair. Gentle handling reduces tissue damage, promotes faster healing, and ultimately minimizes complications.
Q 21. Describe your experience with using different endoscopic visualization systems.
My experience encompasses various endoscopic visualization systems, from standard white-light endoscopes to advanced high-definition endoscopes and narrow-band imaging (NBI) systems. High-definition endoscopes offer superior image quality, enabling better visualization of delicate structures and facilitating more precise suturing. NBI systems enhance the visualization of vascular patterns in the tissue, improving the identification of abnormal areas and potentially reducing complications. Each system has its advantages and limitations, and the choice depends on the specific clinical scenario.
For example, in a complex procedure involving bleeding, NBI can provide a detailed view of the vessels to aid in controlling the bleeding before and during suturing. The selection of the visualization system is often discussed with the surgical team to determine the optimal approach.
Q 22. How do you adapt your suturing technique to different patient anatomies and pathologies?
Adapting my suturing technique to different patient anatomies and pathologies is crucial for successful endoscopic surgery. It’s like tailoring a suit – a one-size-fits-all approach simply won’t work. I consider several key factors:
- Anatomical Variations: The location and size of the target tissue differ significantly between patients. For instance, a hiatal hernia repair in a thin patient will require a different approach than one in an obese patient. I adjust the instrument selection, suture type, and knot-tying technique to accommodate these variations. For example, using longer instruments for deeper locations or smaller needles for delicate tissues.
- Pathological Conditions: The presence of inflammation, scarring, or fragility of tissue requires careful consideration. In cases of severe inflammation, I might opt for a slower, more gentle approach, using absorbable sutures that minimize tissue reaction. If the tissue is fragile, I might choose a less traumatic needle or employ a running suture technique instead of individual stitches.
- Endoscopic Platform: The type of endoscope and its capabilities influence my technique. Flexible endoscopes offer more maneuverability in complex anatomies, while rigid endoscopes provide better stability for precise suturing. I adapt my approach based on the specific endoscope’s limitations and capabilities.
Ultimately, adapting my technique involves a combination of pre-operative planning (reviewing imaging, anticipating challenges), intra-operative assessment (visualizing the tissue and its characteristics), and dexterity to adjust my approach in real-time.
Q 23. How do you stay updated on the latest advancements in endoscopic suturing techniques and technology?
Staying updated in this rapidly evolving field is paramount. I employ a multi-pronged approach:
- Professional Societies: Active membership in organizations like the American Society for Gastrointestinal Endoscopy (ASGE) and participation in their conferences and workshops provide exposure to the latest research, techniques, and technologies.
- Peer-Reviewed Journals: I regularly read journals like Gastrointestinal Endoscopy and Endoscopy to stay abreast of new studies and clinical trials.
- Online Resources and Courses: Many online platforms offer continuing medical education (CME) courses and webinars on advanced endoscopic suturing techniques. These often feature live demonstrations and expert opinions.
- Mentorship and Collaboration: I actively seek out mentorship from experienced colleagues and collaborate with other surgeons, exchanging experiences and insights.
- Hands-on Training: Whenever possible, I participate in advanced training courses and workshops that provide hands-on experience with new instruments and technologies. This is crucial to developing proficiency and confidence.
This continuous learning process ensures that I’m always at the forefront of advancements in endoscopic suturing and can offer my patients the best possible care.
Q 24. Describe your experience with teaching or mentoring others in endoscopic suturing.
Teaching and mentoring have always been an important part of my practice. I’ve mentored several junior surgeons and fellows, focusing on a practical, hands-on approach.
- Structured Training Programs: I design and implement training programs that combine didactic sessions with supervised practical training on models and, ultimately, observation during actual procedures.
- Individualized Mentoring: I provide personalized feedback and guidance to each trainee, identifying their strengths and weaknesses and tailoring instruction accordingly. I often use video recordings of procedures to review technique and identify areas for improvement.
- Case-Based Learning: I use real-world case studies to illustrate different suturing techniques and strategies for managing complications. This helps trainees learn how to apply theoretical knowledge to practical situations.
- Open Communication and Feedback: Creating a safe learning environment where trainees feel comfortable asking questions and seeking feedback is crucial for effective mentorship.
Watching trainees develop their skills and achieve mastery is immensely rewarding. It’s a testament to the power of collaborative learning and a positive contribution to the field.
Q 25. How do you maintain a safe and efficient workflow during endoscopic suturing procedures?
Maintaining a safe and efficient workflow during endoscopic suturing is a delicate balance of preparation, precision, and teamwork.
- Pre-operative Planning: Thoroughly reviewing the patient’s medical history, imaging studies, and understanding the specific pathology are crucial. This allows for careful planning of the procedure, selection of appropriate instruments, and anticipating potential challenges.
- Instrument Organization: Ensuring all necessary instruments are readily available and organized prevents delays and enhances efficiency. This includes having backup instruments prepared for potential difficulties.
- Aseptic Technique: Strict adherence to sterile techniques is paramount to minimize the risk of infection. This includes meticulous hand hygiene, gowning, gloving, and proper draping.
- Teamwork and Communication: Effective communication with the surgical team, including nurses, assistants, and anesthesiologists, is crucial. A clear understanding of roles and responsibilities, combined with open communication regarding progress and any unexpected events, ensures smooth workflow and patient safety.
- Time Management: Efficient time management is essential. Careful planning and execution minimize the procedure’s duration, thus reducing the risk of complications associated with prolonged surgery.
By meticulously addressing these aspects, we ensure patient safety and procedural efficiency.
Q 26. What are your preferred methods for documenting endoscopic suturing procedures?
Documentation of endoscopic suturing procedures requires comprehensive and detailed records to facilitate communication, ensure quality control, and meet legal requirements.
- Operative Report: A detailed operative report outlines the indication for the procedure, the technique employed, any complications encountered, and the outcome. It should include specifics such as suture type and number used.
- Imaging Documentation: Before and after images (endoscopic images and potentially other imaging modalities like CT or MRI) provide a visual record of the procedure and its outcome.
- Video Recording: Video recording of the procedure is often beneficial for educational purposes, quality assurance, and potential future review if complications arise. This offers a complete record of the surgical process.
- Electronic Medical Record (EMR): Integrating all documentation into the patient’s EMR ensures easy access to the information by relevant healthcare professionals. This is crucial for continuity of care and efficient communication.
The comprehensive nature of this documentation protects both the patient and the surgical team by allowing for thorough review and analysis.
Q 27. How do you manage unexpected complications during an endoscopic suturing procedure?
Managing unexpected complications during endoscopic suturing requires a calm, systematic approach.
- Immediate Assessment: Quickly assess the nature and severity of the complication. This might involve bleeding, perforation, or inadvertent damage to adjacent structures.
- Appropriate Intervention: Based on the assessment, implement the necessary corrective measures. This could involve controlling bleeding with clips or coagulation, repairing a perforation, or addressing any other damage.
- Teamwork and Consultation: Involve the surgical team, possibly seeking consultation from a senior colleague or specialist depending on the nature and severity of the complication. Open communication is key here.
- Documentation: Meticulously document the complication, the interventions undertaken, and the final outcome. This ensures transparency and facilitates learning from the experience.
- Post-operative Management: Close monitoring of the patient’s post-operative course is vital to detect and manage any late-onset complications.
A structured approach, combined with effective teamwork and communication, is crucial in mitigating the effects of unexpected complications.
Q 28. Describe a challenging endoscopic suturing case and how you successfully managed it.
One particularly challenging case involved a patient with a large, complex Zenker’s diverticulum and significant inflammation. The diverticulum was adhered to surrounding structures, making dissection difficult and increasing the risk of perforation.
My strategy involved a meticulous, step-by-step approach:
- Careful Dissection: I used a combination of blunt and sharp dissection to separate the diverticulum from the surrounding tissues, minimizing trauma.
- Precise Suturing: I employed a layered closure technique, using absorbable sutures to minimize tissue reaction and ensure secure closure.
- Strategic Instrument Selection: I chose instruments that would provide optimal precision and maneuverability in the confined space, minimizing tissue trauma.
- Frequent Assessment: Throughout the procedure, I regularly assessed the tissue integrity and ensured that the suturing was secure and not causing undue tension.
By combining meticulous technique with careful planning and real-time adaptation, we successfully closed the diverticulum without any complications. The patient made a full recovery, highlighting the importance of careful surgical planning and flexible intraoperative decision-making.
Key Topics to Learn for Endoscopic Suturing Interview
- Instrument Selection and Handling: Understanding the nuances of different endoscopic suturing instruments, their appropriate applications, and proper handling techniques for optimal precision and efficiency.
- Knot Tying Techniques: Mastering various knot-tying methods (e.g., intracorporeal, extracorporeal) suitable for endoscopic surgery, including their advantages and limitations in different surgical scenarios.
- Suture Materials: Knowledge of different suture materials (absorbable vs. non-absorbable), their properties, and selection criteria based on the specific surgical procedure and tissue type.
- Surgical Anatomy and Tissue Handling: Deep understanding of relevant anatomy and delicate tissue handling techniques to minimize trauma and achieve precise suturing.
- Approaches and Techniques: Familiarity with various endoscopic suturing techniques (e.g., running, interrupted, purse-string sutures) and their application in diverse surgical settings.
- Troubleshooting and Complications: Recognizing potential complications (e.g., knot slippage, suture breakage, tissue injury) and developing strategies for effective troubleshooting and management.
- Safety and Sterility: Adherence to strict sterile techniques and safety protocols to prevent infections and ensure patient safety.
- Practical Application: Discuss your experience (or simulated experience through training) applying these techniques in various procedures (e.g., gastrointestinal, urological, gynecological surgeries).
- Emerging Technologies: Awareness of advancements in endoscopic suturing, such as robotic-assisted surgery and novel suture materials.
Next Steps
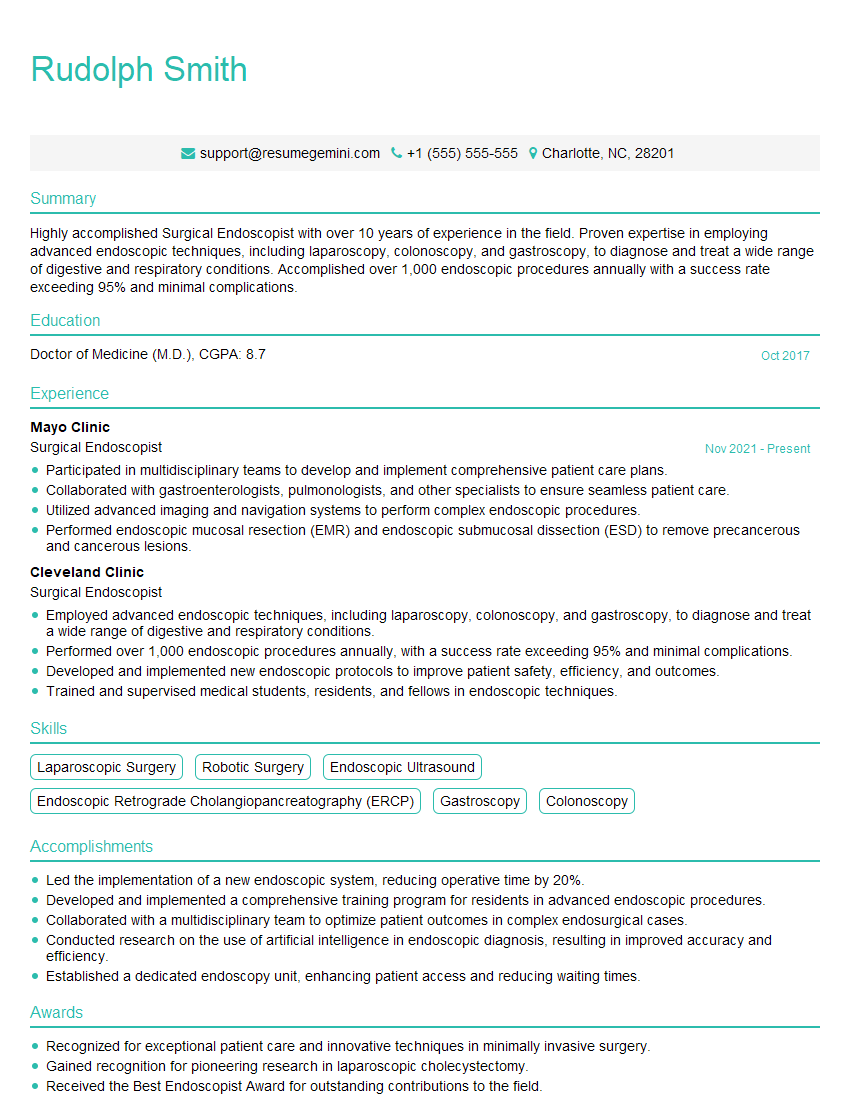
Mastering endoscopic suturing is crucial for career advancement in minimally invasive surgery, opening doors to specialized roles and increased earning potential. A strong resume is key to showcasing your skills and experience to potential employers. To increase your chances of getting noticed by Applicant Tracking Systems (ATS) and recruiters, invest in creating an ATS-friendly resume. ResumeGemini is a trusted resource to help you build a professional and impactful resume. Examples of resumes tailored to Endoscopic Suturing are available to guide you through the process.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.