Unlock your full potential by mastering the most common Enteroscopy interview questions. This blog offers a deep dive into the critical topics, ensuring you’re not only prepared to answer but to excel. With these insights, you’ll approach your interview with clarity and confidence.
Questions Asked in Enteroscopy Interview
Q 1. Describe the different types of enteroscopy procedures.
Enteroscopy encompasses several techniques to visualize the small bowel, an area traditionally difficult to access with standard endoscopy. The main types are:
- Push Enteroscopy: This uses a long, flexible endoscope, advanced gradually through the small bowel. While simple in concept, its reach is limited, typically only reaching the mid-small bowel.
- Double-Balloon Enteroscopy (DBE): This technique utilizes two balloons on the endoscope – one for propulsion and one for anchoring – allowing for deeper penetration into the small bowel, even reaching the terminal ileum. It’s often the method of choice for lesions identified in the distal small bowel on capsule endoscopy.
- Single-Balloon Enteroscopy (SBE): Similar to DBE, but with a single balloon for advancement and retention. While less effective in deep small bowel intubation than DBE, it is less complex and can be a valuable tool.
- Capsule Endoscopy: This is a non-invasive approach using a small, disposable camera capsule that the patient swallows. Images are wirelessly transmitted as the capsule travels through the GI tract. It’s excellent for visualizing the entire small bowel but lacks the ability for therapeutic interventions.
The choice of technique depends on the clinical indication, the location of the suspected lesion (if known), and the expertise of the endoscopist. For instance, a suspected lesion in the ileum would usually necessitate DBE, while a general small bowel evaluation might start with capsule endoscopy.
Q 2. What are the indications for double-balloon enteroscopy (DBE)?
Double-balloon enteroscopy (DBE) is indicated when other less invasive methods fail to adequately visualize or treat lesions in the small bowel. Specific indications include:
- Obscure gastrointestinal bleeding: When the source of bleeding cannot be identified using upper endoscopy or colonoscopy.
- Iron deficiency anemia of unknown origin: DBE can pinpoint the source of blood loss causing the anemia.
- Small bowel tumors or polyps: For diagnosis and potentially resection of small bowel neoplasms.
- Crohn’s disease: To assess the extent and severity of inflammation in the small bowel.
- Celiac disease: Though less common, DBE can help assess the extent of disease.
- Foreign body retrieval: DBE allows for removal of ingested objects lodged in the small bowel.
- Stricture dilation: For opening narrowed segments of the small bowel.
Essentially, DBE is reserved for situations requiring visualization and/or therapeutic intervention in the small bowel that cannot be achieved by simpler means. It’s a powerful tool but carries higher risk and is not a first-line approach.
Q 3. Explain the contraindications for capsule endoscopy.
Capsule endoscopy, while generally safe, has certain contraindications. These include:
- Significant bowel obstruction: The capsule may become lodged or cause further obstruction.
- Toxic megacolon: The capsule could exacerbate the condition.
- Severe bowel inflammation: Inflammation could delay capsule transit.
- Recent gastrointestinal surgery: The possibility of the capsule becoming trapped in an anastomosis exists.
- History of swallowing problems: The patient may have difficulty swallowing the capsule.
- Pacemaker or other implanted devices: Although rare, potential electromagnetic interference may exist.
- Pregnancy: Although safety has not been fully established, it is generally avoided.
A thorough assessment of the patient’s history and current condition is crucial before performing capsule endoscopy to ensure patient safety. For instance, a patient with a known stricture should not undergo capsule endoscopy, as it could become impacted.
Q 4. How do you manage complications during enteroscopy?
Complications during enteroscopy are relatively rare but can be serious. Management depends on the specific complication, but generally involves:
- Perforation: This is the most serious complication and requires immediate surgical intervention, often laparotomy, to repair the perforation and prevent peritonitis.
- Bleeding: Mild bleeding can be managed with endoscopic hemostasis (e.g., clipping, injection). More severe bleeding may require surgical intervention.
- Infection: Antibiotics are administered to treat infection, and close monitoring of vital signs is crucial.
- Pancreatitis: If the procedure damages the pancreas, supportive care, pain management, and fluid resuscitation are necessary.
- Air embolism: This is rare but serious; it requires immediate treatment to address the embolus.
- Aspiration: If the patient aspirates fluids or vomitus, appropriate respiratory support is provided.
Immediate recognition of the complication, prompt and appropriate management, and continuous monitoring of the patient are vital factors in achieving a positive outcome. Post-procedure monitoring is critical to identify delayed complications.
Q 5. What are the pre-procedural preparations for enteroscopy?
Pre-procedural preparations for enteroscopy aim to ensure patient safety and optimize visualization. These steps often include:
- Bowel preparation: A thorough bowel cleansing is necessary to ensure adequate visualization. This typically involves a bowel prep regimen including clear liquids and laxatives, similar to colonoscopy preparation.
- NPO status: Patients are usually required to fast for a specified period before the procedure to minimize the risk of aspiration.
- Sedation: Enteroscopy is usually performed under conscious sedation or general anesthesia, depending on the procedure and patient preference and tolerance.
- Informed consent: Patients must be fully informed about the procedure, risks, benefits, and alternatives.
- Pre-operative assessments: A complete medical history, physical examination, and appropriate laboratory tests (such as coagulation studies) are usually performed.
- Prophylactic antibiotics: Depending on the indication and risk factors, prophylactic antibiotics might be administered to reduce the risk of infection.
Careful preparation minimizes complications and enhances the success of the procedure. For example, inadequate bowel preparation could obscure visualization, compromising the diagnostic yield.
Q 6. Describe the post-procedural care for enteroscopy patients.
Post-procedural care focuses on monitoring the patient for potential complications and ensuring patient comfort. This includes:
- Monitoring vital signs: Close monitoring of heart rate, blood pressure, respiratory rate, and oxygen saturation is vital, particularly in the initial post-procedure period.
- Assessing for bleeding or perforation: Careful observation for signs and symptoms of perforation (abdominal pain, rigidity) or bleeding (hematochezia, hemodynamic instability) is crucial.
- Pain management: Analgesics are administered to manage post-procedure pain and discomfort.
- Fluid and electrolyte balance: Intravenous fluids may be necessary to restore fluid and electrolyte balance, especially after bowel preparation.
- Diet progression: Patients are usually advanced to a regular diet gradually, often starting with clear liquids.
- Discharge instructions: Patients receive detailed instructions regarding diet, activity level, and potential complications to watch out for.
Thorough post-procedure follow-up is critical for early detection of any complications that may occur beyond the immediate post-procedure period. Regular contact with the patient’s primary care physician or specialist is encouraged.
Q 7. What are the risks associated with enteroscopy?
Enteroscopy, while valuable, carries inherent risks, some more common than others:
- Perforation: A tear in the bowel wall is a serious complication requiring surgery.
- Bleeding: Bleeding can occur at the biopsy site or from other damage to the bowel wall.
- Infection: Infection, ranging from localized to systemic, is a possibility.
- Pancreatitis: Damage to the pancreas during the procedure can cause inflammation.
- Aspiration pneumonia: Aspiration of fluids during sedation is a risk.
- Adverse reactions to sedation: Hypotension, respiratory depression, and allergic reactions can occur.
- Bowel obstruction: While not a direct risk, manipulation can sometimes worsen pre-existing issues.
The risk profile varies significantly based on the type of enteroscopy, the patient’s overall health, and the skill of the endoscopist. These risks are discussed with patients to ensure informed consent and realistic expectations. The benefits of the procedure must always be carefully weighed against these risks.
Q 8. How do you interpret findings from enteroscopy?
Interpreting enteroscopy findings involves a systematic approach, combining image analysis with clinical context. We assess the mucosa for abnormalities like inflammation, ulcers, polyps, tumors, or vascular lesions. The location, size, morphology, and any associated findings (e.g., bleeding, strictures) are crucial. For example, finding a flat, reddish lesion in the ileum might suggest Crohn’s disease, while a pedunculated polyp in the colon would raise the suspicion of a benign neoplasm. Microscopic examination of biopsies obtained during the procedure is vital for definitive diagnosis.
We meticulously document all findings, including images and video recordings, and correlate these findings with the patient’s symptoms, medical history, and any prior investigations. This integrated approach ensures accurate interpretation and guides appropriate management decisions. A multidisciplinary approach, involving gastroenterologists, pathologists, and surgeons, is often invaluable in complex cases.
Q 9. How do you handle a perforation during an enteroscopy procedure?
A perforation during enteroscopy is a serious complication requiring immediate action. The first step is to withdraw the endoscope immediately, minimizing further trauma. The patient’s vital signs (heart rate, blood pressure, oxygen saturation) are closely monitored. Fluid resuscitation is initiated to combat hypovolemic shock. The decision to manage conservatively with bowel rest, intravenous antibiotics, and close observation versus surgical intervention depends on the severity of the perforation and the patient’s clinical status. Small perforations may sometimes heal spontaneously with conservative management. However, larger or unstable perforations necessitate immediate surgical repair, often requiring laparotomy or laparoscopy to close the defect and address any intra-abdominal contamination.
Q 10. What are the advantages and disadvantages of DBE compared to other enteroscopy techniques?
Double-balloon enteroscopy (DBE) offers the advantage of deeper intestinal intubation compared to single-balloon enteroscopy (SBE) or colonoscopy. This allows visualization and therapeutic interventions in the small bowel, addressing conditions inaccessible by other methods. However, DBE is a more complex and time-consuming procedure, requiring specialized training and equipment. The higher insertion depth also carries a slightly increased risk of complications like perforation, bleeding, and aspiration. SBE, while reaching a shallower depth, is less invasive and suitable for certain indications. Choosing the optimal technique depends on the clinical question, patient factors, and the endoscopist’s expertise. For example, a patient with obscure gastrointestinal bleeding might benefit from DBE if SBE has failed to identify the source. Colonoscopy is limited to the colon and rectum.
- DBE Advantages: Deeper intestinal intubation, better visualization of small bowel.
- DBE Disadvantages: More complex, higher risk of complications, longer procedure time.
- SBE Advantages: Less invasive, faster procedure time.
- SBE Disadvantages: Shallower intubation depth, less reach.
Q 11. Explain the role of bowel preparation in enteroscopy.
Bowel preparation is crucial for successful enteroscopy, ensuring optimal visualization of the intestinal mucosa. Adequate preparation minimizes fecal material, improving image clarity and facilitating the passage of the endoscope. The preparation regimen varies depending on the technique used (DBE, SBE) and the patient’s medical status. It usually involves a combination of oral laxatives and bowel cleansing solutions that are designed to clear the intestinal tract efficiently. Incomplete bowel preparation leads to poor visualization, potentially resulting in missed lesions or inaccurate diagnosis. For example, residual stool can obscure subtle mucosal abnormalities or interfere with the performance of therapeutic interventions during the procedure. Patient compliance and adequate hydration are vital components of effective bowel preparation.
Q 12. Describe the different types of instruments used in enteroscopy.
Enteroscopy utilizes a range of specialized instruments. The core instrument is the enteroscope itself, a long, flexible endoscope with a camera and light source at the distal end. This allows visualization of the intestinal lumen. Different types exist, including single- and double-balloon endoscopes, each designed for specific applications. Accessories such as biopsy forceps, polypectomy snares, argon plasma coagulation probes, and clips are used for therapeutic interventions. These help remove polyps, cauterize bleeding vessels, or close small defects. Additional instruments may include injection needles for submucosal injections (e.g., for lifting lesions prior to biopsy or treatment), specialized catheters for dye injection, and stents for treating strictures. The selection of instruments depends entirely on the specific clinical indication.
Q 13. How do you manage bleeding during enteroscopy?
Managing bleeding during enteroscopy requires a prompt and systematic approach. The first step is to identify the bleeding source using careful visualization. Once located, several methods are available to control the bleeding. These include: direct hemostasis using clips, endoscopic injection of sclerosing agents or epinephrine, argon plasma coagulation, or even snare polypectomy, depending on the source and severity of the bleeding. If bleeding cannot be controlled endoscopically, or if the source is inaccessible, further intervention like surgical consultation may be necessary. Post-procedure monitoring, including observation for recurrent bleeding, is vital. For example, a visibly bleeding angiodysplasia in the small bowel can often be successfully treated with argon plasma coagulation, while a large ulcer requiring haemostasis may necessitate clip application or surgical intervention.
Q 14. What are the indications for single-balloon enteroscopy (SBE)?
Single-balloon enteroscopy (SBE) is indicated for evaluating and treating lesions in the proximal small bowel that are inaccessible by conventional colonoscopy. Specific indications include: obscure gastrointestinal bleeding (where the source hasn’t been found with other methods), recurrent abdominal pain suggestive of small bowel disease (e.g., Crohn’s disease), suspected small bowel tumors, and the need for polypectomy or other therapeutic interventions in the proximal small bowel. SBE is often used as a less invasive, initial approach before considering the more extensive DBE. For example, in a patient with recurrent unexplained anaemia, SBE can help in visualizing the small bowel and investigating the presence of possible sources of slow bleed. It has limitations as it cannot reach the same depth as DBE.
Q 15. What are the differences between SBE and DBE?
Single-balloon enteroscopy (SBE) and double-balloon enteroscopy (DBE) are both techniques used to visualize the small bowel, but they differ in their mechanism and capabilities. SBE uses a single balloon to advance the endoscope, limiting its reach and maneuverability, particularly in the distal ileum. Think of it like a single-stage rocket – it can get you some distance but has limitations. DBE, on the other hand, uses two balloons – one for propulsion and another for anchoring – allowing for more precise control and deeper insertion. It’s like a two-stage rocket: more power, further reach. This means DBE can reach further into the small bowel than SBE, improving diagnostic yield for lesions located in more distal areas.
- SBE: Simpler technique, less expensive equipment, shorter procedure time, but limited reach and maneuverability.
- DBE: Increased reach and maneuverability, improved visualization of the distal ileum and cecum, but more complex technique, longer procedure time, and higher potential for complications.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. Explain the role of sedation in enteroscopy.
Sedation plays a crucial role in enteroscopy, ensuring patient comfort and tolerance during the procedure, which can be lengthy and sometimes uncomfortable. We typically use conscious sedation, aiming for a level of relaxation where the patient is comfortable but still able to respond to verbal commands. This helps reduce anxiety, pain, and the need for higher doses of analgesics, ultimately making the procedure safer and more efficient. The specific sedative agents and their dosages are carefully tailored to the individual patient’s needs, age, and medical history, always considering potential interactions with other medications.
For example, a combination of midazolam (a benzodiazepine for sedation) and fentanyl (an opioid for pain relief) is commonly used. The goal is not to render the patient unconscious but to create a state of comfortable relaxation that allows for the procedure to be completed safely and effectively.
Q 17. How do you monitor a patient’s vital signs during enteroscopy?
Continuous and meticulous monitoring of vital signs is essential throughout the enteroscopy procedure to ensure patient safety. We typically monitor heart rate, blood pressure, respiratory rate, oxygen saturation (SpO2), and ECG continuously. This is often done using multi-parameter patient monitors, which provide a real-time graphical display of these vital signs. Any significant deviation from baseline readings necessitates immediate attention and potentially adjustments to the sedation level or the procedure itself. For example, a sudden drop in blood pressure might require slowing or stopping the procedure, administering fluids, or adjusting the patient’s position.
Regular pulse oximetry measurements and capnography (monitoring CO2 levels) are crucial for detecting respiratory depression, a potential complication associated with sedation. A dedicated nurse or technician is always present to assist with monitoring and responding to any changes.
Q 18. How do you maintain asepsis during enteroscopy?
Maintaining asepsis during enteroscopy is paramount to prevent infections. We adhere to strict sterile techniques throughout the procedure. This begins with thorough hand hygiene and the use of sterile gloves, gowns, drapes, and instruments. The endoscope itself is meticulously cleaned and disinfected according to manufacturer’s instructions before and after each use, following a high-level disinfection protocol. The insertion site is prepared using an antiseptic solution, and we maintain a sterile field around the area. Appropriate barrier precautions are used to prevent contamination. Post-procedure, meticulous cleaning and reprocessing of the equipment according to guidelines is strictly followed to prevent cross-contamination.
For example, we use high-level disinfectants like glutaraldehyde or peracetic acid to eliminate potential pathogens from the endoscope. Strict adherence to these protocols minimizes the risk of healthcare-associated infections and ensures patient safety.
Q 19. Explain the concept of advanced enteroscopy techniques.
Advanced enteroscopy techniques encompass a range of sophisticated methods that extend the reach and capabilities of traditional enteroscopy. These techniques often involve specialized endoscopes and equipment, allowing for the exploration of areas previously inaccessible. Examples include:
- Deep enteroscopy: This utilizes advanced techniques and specialized endoscopes to reach segments of the small bowel previously unreachable by conventional methods, facilitating diagnosis and treatment of lesions in distal locations.
- Capsule endoscopy: A small, disposable camera is swallowed by the patient; images are transmitted wirelessly to a recording device, allowing for visualization of the small bowel without the need for invasive endoscopy. It is useful for identifying causes of obscure gastrointestinal bleeding.
- Endoscopic mucosal resection (EMR): This involves using endoscopes to remove abnormal tissue, such as polyps or early stage tumors, from the small bowel.
- Endoscopic submucosal dissection (ESD): This technique allows for more extensive resection of lesions compared to EMR. It is used when larger or deeper lesions are present.
These techniques significantly enhance the diagnostic and therapeutic options available for small bowel disorders.
Q 20. Describe your experience with various enteroscopy equipment.
Throughout my career, I’ve gained extensive experience with a variety of enteroscopy equipment from different manufacturers. This includes both SBE and DBE systems, with varying features and functionalities. I’m proficient in using endoscopes with different insertion diameters, working lengths and video imaging systems. I am also familiar with ancillary devices, such as biopsy forceps, polypectomy snares and injection needles required for both diagnostic and therapeutic procedures. I’ve worked with both standard and high-definition endoscopes, appreciating the improved visualization afforded by the latter. Furthermore, I’m experienced in using both traditional and more advanced equipment for procedural enhancement, like specialized balloon inflation systems and accessory channels. This broad experience allows me to adapt to different technological settings and choose the best equipment for each individual case.
Q 21. How do you troubleshoot common technical issues during enteroscopy?
Troubleshooting technical issues during enteroscopy is a critical aspect of the procedure. Common problems include balloon inflation failures, difficulties in advancing the endoscope, and issues with the video imaging system. My approach involves a systematic and methodical assessment of the problem.
- Balloon Inflation: If the balloon fails to inflate, I first check the inflation tubing for kinks or blockages. I then verify the functionality of the inflation pump and check the balloon itself for any damage. If necessary, I switch to a backup inflation system.
- Endoscope Advancement: Difficulty advancing the endoscope might be due to loops or angulation of the bowel, or an obstruction. Gentle manipulation, changing the insertion angle, or using appropriate irrigation techniques can usually resolve this. In some cases, it may require switching to a smaller diameter scope or alternative techniques.
- Video System: Problems with the video display involve checking the connections, the camera settings, and the light source. If the issue persists, I’d switch to a backup camera or system.
A thorough understanding of the equipment, the principles of enteroscopy, and a calm, methodical approach are essential for efficiently handling these technical challenges and ensuring patient safety.
Q 22. What is your experience with reporting enteroscopy findings?
Reporting enteroscopy findings requires meticulous detail and precision. My reports always follow a standardized format, ensuring consistency and clarity. This typically includes a comprehensive description of the procedure itself – the type of enteroscopy performed (e.g., double-balloon enteroscopy, capsule endoscopy), the extent of the bowel visualized, and the overall duration. More importantly, the report details any abnormalities found, such as polyps, ulcers, tumors, or inflammatory changes. I use precise anatomical location descriptions (e.g., specifying the distance from the ileocecal valve), and I always include the size, shape, and appearance of any lesions. I incorporate high-quality images (endoscopic photographs and videos) to support my findings and provide visual context. Finally, I conclude with a concise summary of my interpretations and recommendations for further management, which may involve biopsy results, follow-up procedures, or referral to other specialists. For example, a finding of a 1cm sessile polyp in the ileum would necessitate a detailed description of its appearance, alongside a recommendation for polypectomy and histopathological examination. This standardized approach ensures that referring physicians and other healthcare professionals have all the information they need to make informed decisions regarding patient care.
Q 23. How do you maintain patient safety during enteroscopy?
Patient safety is paramount in enteroscopy. My approach prioritizes meticulous preparation, careful technique, and constant monitoring throughout the procedure. Pre-procedure, this includes a thorough review of the patient’s medical history, including allergies, medications, and any potential bleeding risks. We also ensure adequate bowel preparation to optimize visualization. During the procedure, continuous monitoring of vital signs (heart rate, blood pressure, oxygen saturation) is crucial. I pay close attention to potential complications, such as perforation, bleeding, or hemodynamic instability. We utilize sedation appropriately and monitor the patient’s respiratory status closely. Proper equipment function is checked before and during the procedure. The use of suction and irrigation to maintain clear visualization are critical, and any unusual findings are immediately addressed. Post-procedure, we monitor for any complications and provide clear instructions for post-procedure care, emphasizing signs and symptoms to watch out for, such as abdominal pain, fever, or bleeding. For example, if a patient develops signs of perforation, immediate intervention is necessary, possibly requiring surgical repair. A proactive and multi-faceted approach to patient safety is absolutely critical in minimizing risks and ensuring optimal patient outcomes.
Q 24. Describe a challenging case you encountered during enteroscopy and how you resolved it.
One challenging case involved a patient with recurrent gastrointestinal bleeding, where both colonoscopy and upper endoscopy were unrevealing. Suspecting a small bowel source, we proceeded with double-balloon enteroscopy. The patient had significant angulation and adhesions within the small bowel, making navigation extremely difficult. Repeated attempts to advance the scope were unsuccessful. We needed to carefully balance the need to thoroughly examine the small bowel with the risk of perforation. To resolve this, we employed various techniques, including slow and gentle advancement of the scope, strategic use of water insufflation to create space, and occasional pauses to allow for patient comfort and recovery. We also utilized fluoroscopy to confirm scope position and aid in navigation. Eventually, we identified a small angiodysplasia (abnormal blood vessel) in the distal jejunum as the source of bleeding. This was successfully treated with argon plasma coagulation. This case highlights the importance of careful navigation, patience, and skillful use of ancillary technologies in complex enteroscopy cases. The outcome underscored the value of persistence and a meticulous approach to avoid complications.
Q 25. What are the latest advancements in enteroscopy technology?
Recent advancements in enteroscopy technology are significantly improving diagnostic capabilities and patient outcomes. High-definition endoscopes with enhanced image quality provide clearer visualization of the small bowel mucosa. Improvements in scope design, such as increased flexibility and maneuverability of the double-balloon enteroscopy scopes, have broadened the reach of the procedure. The development of full-spectrum endoscopy (allowing simultaneous visualization in white light and narrow-band imaging) improves the detection of subtle lesions. Moreover, advancements in chromoendoscopy (using dyes to highlight lesions) are further enhancing detection rates. Capsule endoscopy, a less invasive technique, continues to evolve, with improvements in image resolution and battery life. Integration of advanced imaging techniques like confocal laser endomicroscopy (CLE) allows for real-time microscopic visualization of the bowel wall, aiding in the diagnosis of inflammatory conditions or early-stage cancers. These technologies enable more accurate diagnoses, better targeting of lesions, and improved treatment outcomes. For instance, the ability to perform real-time tissue diagnosis via CLE during the enteroscopy procedure, reduces the need for additional procedures, improves the diagnostic yield, and lessens patient discomfort.
Q 26. What continuing education have you undertaken related to enteroscopy?
I actively participate in continuing medical education (CME) to stay current with advancements in enteroscopy. I regularly attend national and international gastroenterology conferences, focusing on sessions dedicated to advanced endoscopic techniques and new technologies. I participate in workshops and hands-on training programs to enhance my technical skills. I also consistently review peer-reviewed journal articles and textbooks on enteroscopy to remain abreast of the latest research and best practices. I am a member of several professional organizations, including the American Society for Gastrointestinal Endoscopy (ASGE), where I regularly access updates on guidelines and recommendations. For example, I recently completed a CME course on advanced polypectomy techniques in the small bowel, which directly improved my skills and patient care in handling difficult cases involving polyp removal.
Q 27. Explain your understanding of the ethical considerations in enteroscopy.
Ethical considerations in enteroscopy are central to my practice. Informed consent is paramount. Patients must understand the procedure, including its benefits, risks, and alternative options. This conversation must be tailored to the individual’s understanding and requires patience and clear communication. Maintaining patient confidentiality is also critical, adhering strictly to HIPAA regulations and data protection guidelines. The procedure should always be medically justified, with the potential benefits outweighing the risks. Appropriate sedation and pain management are essential to ensure patient comfort and minimize distress. Transparency in reporting findings and recommendations is essential. I always strive to act in the best interest of the patient, promoting autonomy and respecting their wishes. For instance, if a patient refuses a particular aspect of the procedure, their decision must be honored, and alternative management strategies must be explored together.
Q 28. How do you handle difficult conversations with patients regarding enteroscopy risks?
Handling difficult conversations about enteroscopy risks requires empathy, patience, and clear communication. I begin by acknowledging the patient’s concerns and validating their anxieties. I explain the risks in a straightforward, understandable manner, avoiding medical jargon whenever possible. I use analogies to help explain complex concepts, comparing the risks to everyday events they might readily grasp. I emphasize that while risks exist, they are relatively low and that I take every precaution to minimize them. I actively listen to their questions and address their concerns honestly and directly. Providing written information alongside the verbal explanation can aid in comprehension and retention. I always make sure the patient feels comfortable asking questions and expressing their doubts. For example, if a patient is worried about perforation, I might explain it like a ‘small puncture,’ and detail the rarity of its occurrence and the measures in place to prevent it. Open and honest communication is key to building trust and allowing the patient to make an informed decision.
Key Topics to Learn for Enteroscopy Interview
- Enteroscopy Techniques: Deep understanding of different enteroscopy techniques (e.g., double-balloon enteroscopy, single-balloon enteroscopy, push enteroscopy), their indications, contraindications, and relative advantages/disadvantages.
- Image Interpretation and Diagnosis: Proficiency in interpreting enteroscopic images to identify pathologies such as tumors, inflammation, and bleeding sources. Practice analyzing case studies to hone diagnostic skills.
- Procedural Complications and Management: Thorough knowledge of potential complications (e.g., perforation, bleeding, infection) and established protocols for their prevention and management. Be prepared to discuss risk mitigation strategies.
- Patient Selection and Preparation: Understanding the criteria for patient selection, bowel preparation techniques, and pre-procedural assessments to ensure patient safety and procedural success.
- Advanced Enteroscopic Techniques: Familiarity with advanced techniques such as endoscopic mucosal resection (EMR), endoscopic submucosal dissection (ESD), and chromoendoscopy, if applicable to your experience level.
- Anesthesia and Sedation: Knowledge of the role of anesthesia and sedation in enteroscopy procedures and potential interactions.
- Post-Procedural Care: Understanding post-procedural monitoring, recovery protocols, and potential complications that may arise post-procedure.
- Ethical and Legal Considerations: Familiarity with relevant ethical guidelines and legal considerations related to enteroscopy procedures.
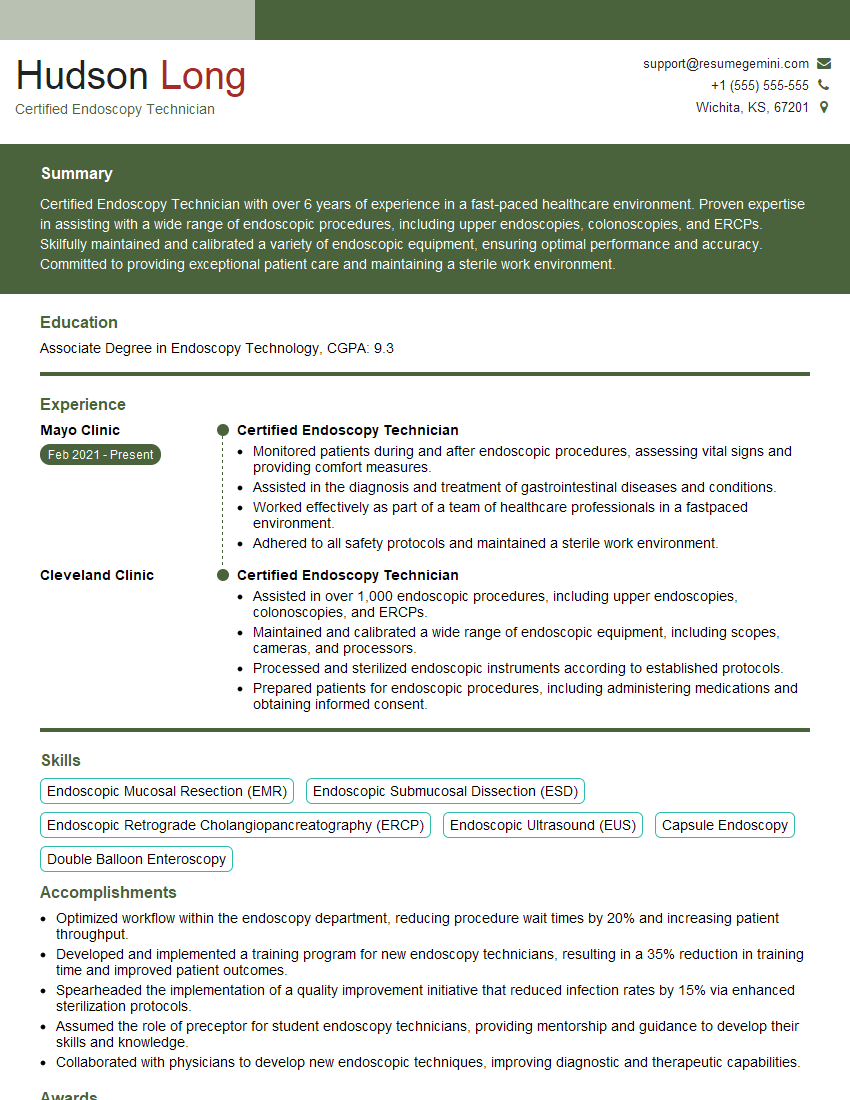
Next Steps
Mastering Enteroscopy opens doors to exciting career opportunities and allows you to make a significant impact on patient care. To maximize your job prospects, it’s crucial to present yourself effectively. Creating an ATS-friendly resume is key to getting your application noticed by recruiters and hiring managers. We strongly recommend using ResumeGemini to build a professional and impactful resume that highlights your skills and experience in Enteroscopy. ResumeGemini provides examples of resumes tailored to the Enteroscopy field, helping you craft a compelling document that showcases your qualifications effectively.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.