Cracking a skill-specific interview, like one for Esophageal Manometry, requires understanding the nuances of the role. In this blog, we present the questions you’re most likely to encounter, along with insights into how to answer them effectively. Let’s ensure you’re ready to make a strong impression.
Questions Asked in Esophageal Manometry Interview
Q 1. Explain the principles behind esophageal manometry.
Esophageal manometry is a physiological test that measures the pressure changes within the esophagus as a person swallows. It’s like having a tiny pressure sensor inside the esophagus, recording the strength and coordination of the esophageal muscles as they move food down to the stomach. This helps diagnose various esophageal motility disorders. The principle relies on the use of a catheter with pressure sensors that’s passed into the esophagus. These sensors detect pressure fluctuations and transmit them to a recording device, creating a pressure-versus-time tracing that reflects esophageal function.
Q 2. Describe the different types of esophageal manometry techniques.
There are several types of esophageal manometry, evolving from simple single-channel systems to sophisticated high-resolution manometry (HRM).
- Conventional Manometry: This older technique uses a few pressure sensors, offering a limited view of esophageal pressures. It’s less precise in detecting subtle motility abnormalities.
- High-Resolution Manometry (HRM): This advanced technique uses multiple sensors along a long catheter, providing a detailed, spatial and temporal map of esophageal pressures. HRM gives a much more comprehensive assessment than conventional manometry.
- Impedance Manometry: This combines manometry with impedance measurements. Impedance assesses the movement of liquids and solids through the esophagus, providing information about bolus transit and coordination with esophageal contractions. This adds another layer of diagnostic information.
The choice of technique depends on the specific clinical question and available resources.
Q 3. What are the indications for performing esophageal manometry?
Esophageal manometry is indicated when a patient presents with symptoms suggestive of esophageal motility disorders. These symptoms include:
- Dysphagia: Difficulty swallowing solids or liquids.
- Odynophagia: Painful swallowing.
- Chest pain: Pain in the chest related to swallowing or esophageal motility.
- Heartburn: Though often associated with GERD, manometry can help rule out motility disorders mimicking GERD.
- Regurgitation: The backward flow of stomach contents into the esophagus.
Manometry helps differentiate between functional disorders (like achalasia, diffuse esophageal spasm) and structural disorders (like strictures) that might cause these symptoms.
Q 4. Interpret a high-resolution manometry tracing showing achalasia.
In achalasia, HRM would demonstrate absent or markedly reduced peristalsis (the wave-like contractions that move food down the esophagus) in the distal esophagus. The lower esophageal sphincter (LES), the muscular ring at the bottom of the esophagus, would show elevated resting pressure and incomplete relaxation during swallowing. This is often described as a ‘bird’s beak’ appearance on the pressure tracing due to the sustained high pressure. Imagine a bird’s beak tightly closed preventing food passage. The absence of coordinated peristalsis and the failure of the LES to relax are key diagnostic features in achalasia.
Q 5. Interpret a high-resolution manometry tracing showing diffuse esophageal spasm.
Diffuse esophageal spasm (DES) on HRM shows simultaneous, non-peristaltic contractions throughout the esophageal body. These contractions are often high amplitude and painful, disrupting the normal passage of the bolus. The pressure tracing would show multiple chaotic contractions that lack the organized pattern of normal peristalsis. Imagine the esophagus squeezing irregularly and powerfully, causing pain and difficulty swallowing. The LES pressure may or may not be elevated.
Q 6. Interpret a high-resolution manometry tracing showing nutcracker esophagus.
Nutcracker esophagus is characterized by excessively strong contractions in the distal esophagus during swallowing. HRM would show normal peristalsis, but the amplitude of the contractions is significantly higher than normal (>180 mmHg). These powerful contractions can be painful. Imagine the esophagus squeezing too forcefully, like a nutcracker crushing a nut. The LES pressure is typically normal.
Q 7. What are the limitations of esophageal manometry?
Despite its value, esophageal manometry does have limitations:
- Invasive procedure: It involves passing a catheter, which can cause discomfort to some patients.
- Patient cooperation: The test requires patient cooperation and ability to swallow, making it challenging in certain patient populations (e.g., those with cognitive impairment).
- Interpretation: The interpretation of manometric tracings can be complex and requires expertise and experience. Some subtle abnormalities might be missed.
- Lack of direct visualization: Manometry only provides pressure measurements; it does not directly visualize the esophagus or the movement of the bolus.
Therefore, manometry should be considered within the context of the patient’s clinical presentation, other investigations, and the clinician’s experience.
Q 8. How do you differentiate between esophageal spasm and achalasia using manometry?
Differentiating between esophageal spasm and achalasia using manometry hinges on understanding their distinct patterns of esophageal body contractions and lower esophageal sphincter (LES) relaxation. Esophageal spasm is characterized by simultaneous, non-peristaltic contractions that are often painful. These contractions can be diffuse, involving multiple segments of the esophagus, or localized to a specific area. Achalasia, on the other hand, demonstrates a failure of LES relaxation with aperistalsis or weak peristalsis in the esophageal body. Think of it like this: esophageal spasm is like a chaotic, uncoordinated muscle spasm, whereas achalasia is like a valve that’s stuck shut.
Manometrically, we see:
- Esophageal Spasm: High-amplitude, simultaneous contractions often involving multiple esophageal segments. The LES pressure might be normal or slightly elevated.
- Achalasia: Lack of peristalsis in the esophageal body (or very weak, unorganized peristalsis) and incomplete or absent relaxation of the LES in response to swallowing. LES pressure is significantly elevated. You often see a ‘bird’s beak’ appearance on the pressure profile.
In practice, we analyze the pressure waveforms recorded during swallows to differentiate between these conditions. The presence of painful contractions coupled with normal or slightly elevated LES pressure strongly suggests esophageal spasm, while the combination of aperistalsis and markedly elevated LES pressure points towards achalasia. Clinical presentation also plays a crucial role; patients with achalasia often present with dysphagia (difficulty swallowing) to both solids and liquids, while those with esophageal spasm may experience chest pain and dysphagia more intermittently.
Q 9. Discuss the role of impedance in esophageal manometry.
Esophageal impedance in manometry adds another layer of information by measuring changes in electrical conductivity within the esophageal lumen. While manometry assesses the pressure changes associated with swallowing, impedance measures the changes in the conductivity caused by the movement of fluids, such as saliva, liquid boluses or refluxate. Essentially, it helps identify the location and timing of bolus transit and reflux events.
For example, if we suspect GERD, impedance can provide evidence of reflux episodes even in the absence of detectable pressure changes (silent reflux). This is crucial because the classic symptoms of heartburn don’t always correlate with manometric findings. Impedance and manometry together provide a more comprehensive picture of esophageal function.
In addition, impedance can help differentiate between esophageal clearings (a natural mechanism where the esophagus clears itself of refluxate) and true reflux events. By integrating impedance and pressure data, we gain a far more accurate understanding of the complex interplay between esophageal motility, acid exposure and symptoms.
Q 10. Explain the concept of integrated relaxation pressure.
Integrated relaxation pressure (IRP) is a crucial parameter derived from esophageal manometry that quantifies the degree of lower esophageal sphincter (LES) relaxation during swallowing. It’s not simply about the *lowest* pressure achieved, but rather the *overall* relaxation over a defined time period following a swallow.
To obtain IRP, the manometry system integrates (sums up) the pressure over the duration of LES relaxation after a swallow. A lower IRP indicates better relaxation, which is desirable. A higher IRP suggests poor relaxation, potentially indicating achalasia or other motility disorders. Think of it like this: a sponge completely squeezed is analogous to a fully relaxed LES. If the sponge only partially releases the water, analogous to poor LES relaxation, the IRP will be higher.
IRP helps provide a more nuanced assessment of LES function than just looking at the resting pressure. This is particularly useful in diagnosing and classifying motility disorders like achalasia where the degree of relaxation might be variable and not accurately captured by just looking at the lowest pressure recorded.
Q 11. How is esophageal manometry used in the diagnosis of GERD?
While esophageal manometry isn’t the primary diagnostic test for GERD (Gastroesophageal Reflux Disease), it can provide valuable information in specific cases. The role of manometry in GERD diagnosis is primarily to assess esophageal motility, which may be affected in some patients with GERD, particularly those with symptoms that are not well explained by conventional tests like pH monitoring.
Manometry can help rule out other motility disorders that might mimic GERD symptoms (such as achalasia or diffuse esophageal spasm). It may also reveal abnormalities in esophageal clearance mechanisms, potentially suggesting why certain individuals are more susceptible to reflux symptoms. For instance, impaired peristalsis can contribute to reflux by slowing the clearing of refluxate from the esophagus. However, it’s important to note that manometry alone is insufficient to diagnose GERD, and it needs to be used in conjunction with other diagnostic modalities like endoscopy and pH studies.
Q 12. Describe the preparation of a patient for esophageal manometry.
Patient preparation for esophageal manometry is relatively straightforward, but crucial for accurate results. First, a detailed explanation of the procedure and potential discomfort should be given, addressing the patient’s anxiety. The patient should fast for at least 6 hours before the procedure to avoid interfering with the pressure measurements. Medications affecting esophageal motility should be discussed with the physician, some might need temporary cessation while others may require continuation. The patient will be positioned in a seated or semi-recumbent position for the procedure itself.
Patients should be advised to avoid smoking or consuming caffeinated drinks prior to the test, as they can influence esophageal motility. Any dental appliances that might interfere with the placement of the catheter should be removed. In some cases, a local anesthetic may be sprayed in the pharynx and throat to reduce discomfort during the catheter placement.
Q 13. What are the potential complications of esophageal manometry?
Esophageal manometry is generally a safe procedure, but potential complications do exist, though rare. The most common complication is discomfort or gagging during catheter insertion, which can often be mitigated with adequate anesthetic sprays and patient coaching. Rare complications may include esophageal perforation (a hole in the esophagus), bleeding, or infection at the insertion site. The risk of perforation is increased with forceful insertion or in patients with pre-existing esophageal strictures or other pathologies.
To minimize risks, the procedure is always performed by experienced medical professionals. The manometry catheter is carefully advanced under fluoroscopic guidance in some centers. Post-procedure monitoring is standard to identify any unusual symptoms.
Q 14. How do you interpret a manometry study showing ineffective esophageal motility?
Ineffective esophageal motility on manometry indicates that the esophagus isn’t adequately transporting swallowed material toward the stomach. This can manifest in several ways, including decreased or absent peristaltic contractions, reduced amplitude of contractions, or increased propagation time. The interpretation must consider the clinical presentation. For example, a pattern of ineffective esophageal motility coupled with dysphagia and chest pain might suggest diffuse esophageal spasm, while a pattern of aperistalsis and elevated LES pressure strongly indicates achalasia.
The interpretation is not a simple yes/no answer. It involves a careful analysis of the pressure waveforms, considering the presence or absence of peristalsis, the amplitude and regularity of contractions, and the LES pressure. This information is crucial in establishing the most likely diagnosis and planning appropriate management strategies. In some cases, further investigations (such as high-resolution manometry) may be indicated to characterize the abnormality more precisely.
Q 15. Explain the relationship between esophageal manometry and other diagnostic tests.
Esophageal manometry is a key diagnostic tool, but it rarely stands alone. It works best in conjunction with other tests to provide a complete picture of esophageal function. For example, it’s often paired with a barium swallow study (which visually assesses the esophagus’s structure) to correlate motility findings with anatomical abnormalities. If a patient presents with symptoms of GERD (Gastroesophageal Reflux Disease), manometry can help determine the severity of the reflux, while endoscopy might be used to rule out other structural issues like esophageal strictures or Barrett’s esophagus. In cases of dysphagia (difficulty swallowing), manometry complements imaging studies like a CT or MRI scan to differentiate between motility disorders and structural problems. Essentially, manometry focuses on the function of the esophagus, while other tests highlight the structure or presence of other diseases.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you calibrate the equipment for esophageal manometry?
Calibrating the esophageal manometry equipment is crucial for accurate pressure readings. This usually involves using a known pressure source, often a calibrated water manometer or an electronic pressure calibrator. The process typically involves connecting the calibration device to the manometry system, and then zeroing the system by adjusting the baseline reading to reflect atmospheric pressure. After zeroing, the system is then exposed to known pressure steps (e.g., 20 mmHg, 40 mmHg, 60 mmHg) to verify linearity and accuracy. The system’s response to these known pressures is recorded, and any deviations from expected values indicate the need for adjustment or system maintenance. A calibration log must be meticulously maintained, documenting dates, calibration results, and any corrective actions taken. Failure to properly calibrate can lead to inaccurate diagnoses and inappropriate treatment decisions.
Q 17. What are the quality control measures you would implement for esophageal manometry?
Rigorous quality control is paramount in esophageal manometry. This includes daily checks of the equipment’s functionality, including verification of pressure transducers and signal integrity. Regular calibration, as described previously, is fundamental. We maintain detailed records of all calibrations, equipment maintenance, and any repairs. Furthermore, we implement proficiency testing using standardized phantoms or simulated manometry tracings to assess the technician’s skill and consistency in data acquisition and interpretation. This ensures that the quality of the data obtained is consistent and reliable across different examinations and examiners. We also regularly review our manometry procedures to make sure we are following the latest guidelines and best practices. Finally, a thorough quality assurance program is followed involving regular review of the data for consistency and adherence to established norms.
Q 18. How do you troubleshoot common problems encountered during esophageal manometry?
Troubleshooting during esophageal manometry often involves systematically checking the entire process. Common problems include poor catheter placement (leading to inaccurate readings), signal artifacts (noise in the pressure tracings), or equipment malfunctions. If poor catheter placement is suspected, we review the fluoroscopic images (if used) and may reposition the catheter. Signal artifacts might be caused by patient movement or electrical interference; we address this by asking the patient to remain still and checking for any external interference. If the equipment malfunctions, a methodical check of the connections, pressure transducer, and recording system is performed. In some cases, a repeat study is necessary. The key is a systematic approach, meticulously checking each component until the problem is identified and resolved. Careful documentation of the issue and any corrective actions is critical.
Q 19. Describe the different types of catheters used in esophageal manometry.
Several catheter types exist, each with its advantages and disadvantages. Solid-state catheters are increasingly popular due to their smaller size, fewer pressure sensors, and resistance to kinking. They often offer high-resolution recordings across multiple sensors, providing detailed pressure profiles. Traditional multi-lumen catheters have been the standard for years, with multiple pressure ports that allow for detailed assessment of the different esophageal segments. These offer an excellent compromise between spatial resolution and ease of placement, but are susceptible to kinking. High-resolution manometry catheters, equipped with numerous sensors, provide the most detailed pressure mapping of the esophagus and are excellent for identifying subtle motility disorders. The choice of catheter depends on the specific clinical question and the expertise of the clinician.
Q 20. What are the normal values for esophageal pressures in different segments?
Normal esophageal pressure values vary depending on the segment being measured and the technique used. Generally, the upper esophageal sphincter (UES) shows a high resting pressure (typically 20-40 mmHg), ensuring that it remains closed except during swallowing. The esophageal body typically exhibits low resting pressure, usually less than 5 mmHg. During peristalsis (the wave-like muscle contractions that propel food down), the body exhibits a pressure increase, which should be coordinated and propagated along its length. The lower esophageal sphincter (LES) usually exhibits a resting pressure ranging from 10-30 mmHg, which helps to prevent reflux. These are just general ranges, and deviations are common. Interpretation always takes into account factors like the patient’s age, symptoms, and the clinical context. The precise values and interpretation should be guided by a thorough understanding of current manometry interpretation standards.
Q 21. How do you explain the results of an esophageal manometry study to a patient?
Explaining manometry results to a patient requires clear, concise communication, avoiding technical jargon. I begin by describing the test’s purpose, and what it aimed to measure. I would then simply explain that the test evaluates how the esophagus moves food towards the stomach. I would avoid overcomplicating things by explaining the specific pressure readings, instead focusing on a general summary of the findings. For example, if the study shows normal esophageal function, I’d explain that the esophagus is working correctly. If there’s an abnormality (e.g., weak contractions, or a poorly functioning LES), I explain this in simple terms, such as, “The muscle contractions were somewhat weaker than normal, which could contribute to some of your symptoms.” I always focus on providing a hopeful outlook, explaining the treatment options available based on the findings. Patient education involves offering support and reassurance, often providing written material to reinforce our conversation.
Q 22. Discuss the role of esophageal manometry in treatment planning.
Esophageal manometry plays a crucial role in treatment planning for various esophageal motility disorders. It provides a detailed assessment of esophageal function, allowing clinicians to accurately diagnose the underlying problem and tailor the most effective treatment strategy. For instance, a patient presenting with dysphagia (difficulty swallowing) might undergo manometry to determine if the cause is due to achalasia (failure of the lower esophageal sphincter to relax), diffuse esophageal spasm (DES), or another motility disorder. The results directly influence the choice between medical management (e.g., medication to relax the sphincter), minimally invasive procedures (e.g., pneumatic dilation), or surgery (e.g., myotomy for achalasia).
For example, if manometry reveals characteristics consistent with achalasia, the physician will consider options like pneumatic dilation or laparoscopic Heller myotomy. Conversely, if the findings point towards a hypertensive lower esophageal sphincter without significant peristalsis, treatment might focus on medication to relax the sphincter. The detailed pressure measurements provided by manometry are invaluable in selecting the most suitable and effective intervention.
Q 23. What are the current advancements in esophageal manometry technology?
Recent advancements in esophageal manometry have significantly improved the accuracy and detail of assessments. High-resolution manometry (HRM) has replaced conventional manometry as the gold standard, offering far greater spatial and temporal resolution. This means we can visualize esophageal contractions with much more precision, identifying subtle patterns that were previously undetectable. Another key advancement is the integration of sophisticated software for data analysis and interpretation. These programs can automatically quantify parameters such as integrated relaxation pressure, peristaltic amplitude, and the presence of abnormalities like premature contractions. Furthermore, the development of more comfortable and easily tolerated catheters makes the procedure more patient-friendly, reducing anxiety and discomfort.
For example, the ability to identify specific patterns within HRM data helps differentiate between various motility disorders with overlapping symptoms. This improved diagnostic accuracy leads to better treatment decisions. Additionally, some newer systems incorporate impedance measurements, allowing simultaneous assessment of esophageal pressure and intraluminal impedance, providing even richer data to improve diagnosis and treatment planning.
Q 24. Compare and contrast high-resolution manometry and conventional manometry.
High-resolution manometry (HRM) and conventional manometry both measure esophageal pressure, but HRM offers significant advantages. Conventional manometry utilizes fewer pressure sensors, resulting in a coarser representation of esophageal contractions. HRM, on the other hand, employs a much higher density of sensors, providing a much more detailed and accurate depiction of pressures along the entire esophageal length. This improved resolution allows for a more precise identification of subtle motility disorders and nuanced patterns of esophageal activity. Think of it like comparing a low-resolution photograph to a high-resolution one; the latter reveals far more detail.
For example, HRM can detect subtle abnormalities like weak peristalsis or non-peristaltic contractions that might be missed by conventional manometry. This improved sensitivity is particularly important in differentiating between various motility disorders, leading to better treatment decisions. While conventional manometry may provide an overall assessment of esophageal function, HRM allows for a more refined and precise diagnosis.
Q 25. Describe your experience with different manometry software packages.
Throughout my career, I’ve had extensive experience with several manometry software packages, including Manoview, Medtronic’s systems, and Sierra Scientific’s systems. Each package has its strengths and weaknesses. For instance, Manoview provides excellent visualization tools and sophisticated analysis algorithms. Medtronic’s systems are known for their user-friendly interface and seamless integration with other clinical data. Sierra Scientific’s systems often feature robust reporting capabilities. The choice of software ultimately depends on the specific needs of the institution and clinician preferences; however, familiarity with a range of packages ensures adaptability to different settings and technological advancements.
The ability to interpret data from different software packages accurately is crucial for consistency and reliability in diagnoses and treatment planning. I have consistently strived to maintain proficiency in all the systems encountered in my practice.
Q 26. How do you ensure the safety and comfort of the patient during the procedure?
Patient safety and comfort are paramount during esophageal manometry. Before the procedure, I thoroughly explain the procedure to the patient, answering all their questions and addressing any concerns. This ensures informed consent and helps reduce patient anxiety. The procedure itself involves passing a thin, flexible catheter through the nose and into the esophagus. Using topical anesthetic nasal spray and adequate lubrication significantly minimizes discomfort. Throughout the procedure, I maintain open communication with the patient, monitoring their response closely and stopping if significant discomfort arises. Post-procedure, I provide clear instructions on managing any potential side effects (like sore throat) and advise on dietary modifications for optimal recovery.
For example, I always adjust the procedure based on the patient’s individual response. If a patient reports discomfort, I will immediately adjust the catheter placement or briefly pause the test. My aim is to ensure the patient feels as safe and comfortable as possible during the entire process.
Q 27. Explain how esophageal manometry helps to determine the need for surgery.
Esophageal manometry plays a critical role in determining the need for surgery in various esophageal motility disorders. For example, in achalasia, HRM often shows a characteristic absence of peristalsis and incomplete relaxation of the lower esophageal sphincter (LES). The severity of these findings, particularly the degree of LES hypertension, often guides surgical decision-making. Patients with significant symptoms and pressure abnormalities unresponsive to medical management are often considered candidates for surgical myotomy. Similarly, in severe cases of diffuse esophageal spasm (DES) where medical therapy fails, manometry findings might support the consideration of surgical intervention, although this is less common than in achalasia.
Therefore, manometry results are not the sole determinant but a critical component in the overall assessment that ultimately decides whether surgical intervention is necessary. Other factors such as symptom severity, patient preference, and the presence of other medical conditions are also carefully considered before making a recommendation for surgery.
Q 28. Discuss the ethical considerations related to the use of esophageal manometry.
Ethical considerations in using esophageal manometry center around informed consent, patient safety, and the responsible interpretation and communication of results. Patients must be fully informed about the procedure’s purpose, risks, and benefits before consenting. Maintaining patient confidentiality is essential, and results should only be shared with authorized medical personnel involved in their care. Accurate interpretation of manometric data is critical to avoid misdiagnosis and unnecessary interventions. Clinicians must be proficient in interpreting the results and understand the limitations of the test.
For instance, a crucial ethical consideration is avoiding unnecessary or invasive procedures based on poorly interpreted manometric data. Openly discussing uncertainties and limitations of the test with patients fosters trust and ensures that treatment decisions are made ethically and collaboratively. The ethical use of manometry requires a thorough understanding of the test’s limitations and a commitment to responsible clinical practice.
Key Topics to Learn for Esophageal Manometry Interview
- Basic Principles of Esophageal Motility: Understand the physiological mechanisms behind esophageal peristalsis, including the roles of the upper and lower esophageal sphincters.
- Esophageal Manometry Techniques: Become proficient in the different manometry techniques (e.g., high-resolution manometry, impedance planimetry) and their clinical applications. Understand the limitations of each technique.
- Interpreting Manometric Data: Master the skills needed to interpret pressure waveforms, identify characteristic patterns of various esophageal motility disorders (e.g., achalasia, diffuse esophageal spasm), and differentiate normal from abnormal findings.
- Clinical Applications of Esophageal Manometry: Familiarize yourself with the use of esophageal manometry in diagnosing and managing various esophageal diseases, including dysphagia, reflux, and motility disorders.
- Correlation with other Diagnostic Tests: Understand how esophageal manometry findings correlate with other diagnostic tests such as endoscopy, pH monitoring, and imaging studies.
- Practical Problem-Solving: Practice analyzing hypothetical manometric tracings and formulating appropriate diagnostic and therapeutic recommendations. Consider scenarios involving atypical presentations or challenging interpretations.
- Emerging Technologies and Future Directions: Stay updated on the latest advancements in esophageal manometry technology and its evolving role in clinical practice.
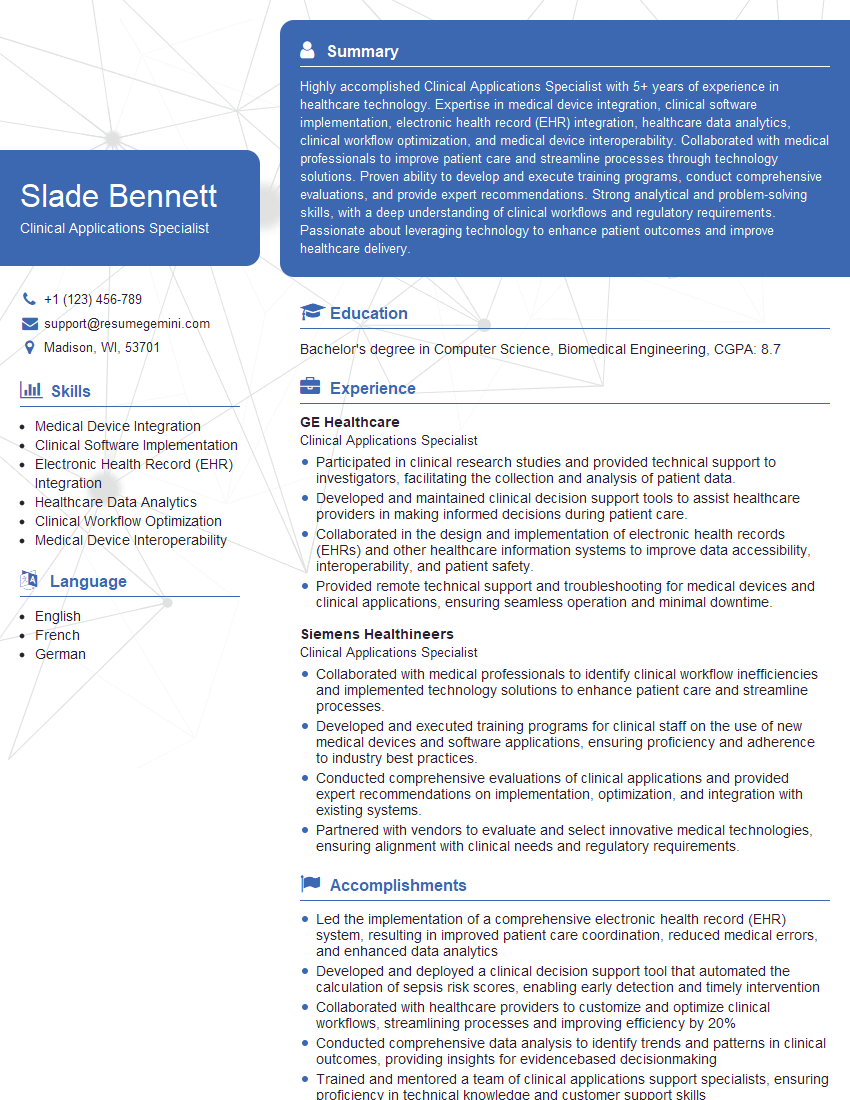
Next Steps
Mastering Esophageal Manometry opens doors to exciting career opportunities in gastroenterology and related fields. A strong understanding of this crucial diagnostic tool significantly enhances your value as a healthcare professional. To maximize your job prospects, creating an ATS-friendly resume is essential. ResumeGemini can help you craft a compelling resume that highlights your skills and experience effectively, increasing your chances of landing your dream job. We offer examples of resumes tailored to Esophageal Manometry to help guide you. Take the next step towards a successful career – build your best resume with ResumeGemini today!
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
To the interviewgemini.com Webmaster.
Very helpful and content specific questions to help prepare me for my interview!
Thank you
To the interviewgemini.com Webmaster.
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.