Every successful interview starts with knowing what to expect. In this blog, we’ll take you through the top Exercise Assessment and Evaluation interview questions, breaking them down with expert tips to help you deliver impactful answers. Step into your next interview fully prepared and ready to succeed.
Questions Asked in Exercise Assessment and Evaluation Interview
Q 1. Describe the different methods for assessing body composition.
Assessing body composition involves determining the proportion of fat mass to fat-free mass (muscle, bone, water, etc.) in the body. Several methods exist, each with its own strengths and limitations.
- Anthropometry: This involves using simple measurements like height, weight, and circumferences (waist, hip, etc.) to estimate body composition. It’s inexpensive and easy to perform but less precise than other methods. For example, calculating Body Mass Index (BMI) falls under this category. However, BMI doesn’t differentiate between muscle mass and fat mass, leading to potential inaccuracies.
- Skinfold Calipers: This technique measures subcutaneous fat (fat just below the skin) at multiple sites using calipers. The measurements are then used in prediction equations to estimate total body fat percentage. While more accurate than BMI, it requires trained personnel and the accuracy depends on the skill of the technician and the chosen equation.
- Bioelectrical Impedance Analysis (BIA): BIA uses a small electrical current passed through the body to estimate body composition. Fat tissue resists the current more than lean tissue, allowing for an estimation of body fat percentage. It’s convenient and relatively inexpensive, but factors like hydration level can significantly affect the accuracy of the results. For example, being dehydrated can lead to an overestimation of body fat.
- Hydrostatic Weighing (Underwater Weighing): This ‘gold standard’ method measures body density by comparing weight on land to weight underwater. It’s highly accurate but requires specialized equipment and is not readily accessible to most people.
- Air Displacement Plethysmography (Bod Pod): This method uses air displacement to determine body volume and subsequently body density, similar to hydrostatic weighing, but is generally considered more comfortable for the subject. It also offers a high degree of accuracy.
- Dual-Energy X-ray Absorptiometry (DEXA): DEXA is a very accurate method that uses low-dose X-rays to measure bone mineral density, fat mass, and lean mass. It’s considered the gold standard for body composition assessment, although it’s expensive and requires specialized equipment.
The choice of method depends on factors like cost, availability of equipment, required accuracy, and the individual’s characteristics.
Q 2. Explain the principles of VO2 max testing and its clinical significance.
VO2 max testing measures the maximum amount of oxygen your body can utilize during intense exercise. It’s a crucial indicator of cardiorespiratory fitness.
Principles: The test involves progressively increasing the intensity of exercise (e.g., on a treadmill or cycle ergometer) while continuously monitoring oxygen uptake (VO2), carbon dioxide production (VCO2), and breathing frequency. The VO2 max is reached when oxygen uptake plateaus despite increasing exercise intensity. This represents the body’s maximum capacity for oxygen consumption.
Clinical Significance: VO2 max is a strong predictor of cardiovascular health and mortality risk. A lower VO2 max is associated with increased risk of cardiovascular disease, while higher VO2 max indicates better cardiovascular fitness and improved prognosis after a cardiac event. It helps clinicians assess the effectiveness of cardiac rehabilitation programs, monitor disease progression, and guide exercise prescription.
For example, a patient recovering from a heart attack might undergo VO2 max testing to determine a safe and effective exercise intensity for their rehabilitation plan. Monitoring changes in VO2 max over time can track their progress and guide adjustments in the program.
Q 3. How do you interpret a graded exercise test (GXT)?
Interpreting a Graded Exercise Test (GXT) involves analyzing the physiological responses throughout the test to assess cardiovascular fitness and identify any abnormalities.
The interpretation includes analyzing the:
- Heart rate response: The expected increase in heart rate with increasing exercise intensity is assessed. An abnormal response might indicate underlying cardiovascular issues.
- Blood pressure response: Blood pressure is monitored for excessive increases or drops. Significant changes can suggest hypertension, hypotension, or other cardiovascular problems.
- ECG (electrocardiogram): The ECG monitors the electrical activity of the heart and can detect any abnormalities like arrhythmias (irregular heartbeats) or ischemia (reduced blood flow to the heart). ST-segment depression is a key indicator of myocardial ischemia during exercise.
- Symptom response: Symptoms reported by the individual (e.g., chest pain, shortness of breath, dizziness) are crucial for interpreting the results. These symptoms might indicate underlying pathology.
- VO2 max (if measured): The maximum oxygen uptake provides a quantitative measure of cardiorespiratory fitness.
Based on these parameters, the GXT can identify risk factors for cardiovascular disease, diagnose underlying cardiac problems, and guide the prescription of appropriate exercise training.
Example: A GXT showing significant ST-segment depression during moderate exercise might indicate coronary artery disease, requiring further cardiac evaluation. On the other hand, a normal GXT with a high VO2 max suggests excellent cardiovascular health and a high capacity for exercise.
Q 4. What are the contraindications for exercise testing?
Contraindications for exercise testing are conditions that make it unsafe or inappropriate to perform the test. These are categorized as absolute and relative contraindications.
- Absolute Contraindications: These are conditions that make exercise testing absolutely unsafe and should prevent the test from being performed. Examples include: acute myocardial infarction (heart attack) within the past 2 days; unstable angina (chest pain); uncontrolled heart rhythms; acute pulmonary embolism (blood clot in the lungs); severe aortic stenosis (narrowing of the aorta); uncontrolled hypertension (high blood pressure); and acute myocarditis or pericarditis (inflammation of the heart muscle or lining).
- Relative Contraindications: These conditions increase the risk of complications during exercise testing, and the decision to proceed requires careful consideration and risk-benefit assessment. Examples include: left main coronary stenosis; moderate stenotic valvular heart disease; electrolyte abnormalities; severe arterial hypertension; tachyarrhythmias; hypertrophic cardiomyopathy; and recent stroke or transient ischemic attack.
It’s crucial to conduct a thorough pre-exercise screening to identify any contraindications before proceeding with the test. A physician’s evaluation might be necessary in cases with relative contraindications.
Q 5. Explain the importance of pre-exercise screening questionnaires.
Pre-exercise screening questionnaires, such as the PAR-Q+ (Physical Activity Readiness Questionnaire+), are essential for identifying individuals at increased risk of adverse events during exercise. They help assess medical history, current health status, and lifestyle factors that could impact exercise safety.
Importance: These questionnaires help stratify individuals into low, moderate, or high-risk categories, guiding the need for further medical clearance or modifications to exercise programs. They help prevent potentially serious complications by identifying individuals who might require medical supervision during exercise testing or participation in physical activity.
For example, an individual who reports a history of heart disease or recent surgery would be considered high-risk and would need medical clearance before participating in vigorous exercise. By identifying these individuals through the questionnaire, we can avoid potential complications or even fatalities.
Q 6. How do you determine an individual’s training heart rate zones?
Training heart rate zones define different intensities of exercise, useful for setting individualized training goals. Several methods exist for determining these zones, all based on the maximum heart rate (MHR).
- Maximal Heart Rate (MHR) Method: This traditional method uses the formula
MHR = 220 - ageto estimate MHR. Then, percentages of MHR are used to define zones (e.g., 60-70% for low intensity, 70-80% for moderate, and 80-90% for high intensity). This method is simple but can be inaccurate due to individual variability in MHR. - Heart Rate Reserve (HRR) Method (Karvonen Method): This method considers resting heart rate (RHR) and offers a more personalized approach.
HRR = MHR - RHR. Then, target heart rates are calculated based on percentages of HRR added to RHR. This method is considered more precise than the MHR method. - Direct Measurement of Max Heart Rate: The most accurate method is to directly measure the individual’s maximum heart rate during a maximal graded exercise test. This involves performing an exercise test until exhaustion and recording the highest heart rate achieved during the test. This provides the most accurate MHR and HRR for zone calculations.
Once the heart rate zones are established, individuals can monitor their heart rate during exercise to ensure they’re training at the appropriate intensity for their goals. For example, someone aiming for improved cardiovascular endurance might focus on training within their moderate to high intensity zones (70-85% of HRR).
Q 7. What are the key components of a comprehensive fitness assessment?
A comprehensive fitness assessment provides a holistic picture of an individual’s physical capabilities and health status. It combines various assessments to create a personalized training plan. Key components include:
- Resting measurements: Height, weight, body mass index (BMI), resting heart rate, and blood pressure.
- Body composition assessment: Methods described in question 1 (e.g., skinfold calipers, BIA, DEXA).
- Cardiorespiratory fitness assessment: Tests like VO2 max testing or submaximal GXT.
- Muscular strength and endurance assessment: Tests like 1-repetition maximum (1RM) for strength and tests like push-up or sit-up tests for endurance.
- Flexibility assessment: Tests like sit-and-reach or goniometry.
- Balance and agility assessment: Tests that measure stability, coordination and quickness.
- Postural assessment: Evaluation of posture to identify potential musculoskeletal imbalances.
- Health History and Risk Factor Assessment: Including questionnaires like PAR-Q+ and information regarding medical history, lifestyle habits, family history of heart disease and other relevant factors.
This information is crucial for designing safe and effective exercise programs tailored to the individual’s needs and goals. It provides a baseline for monitoring progress and making adjustments over time. For example, the assessment data might indicate that an individual needs to focus on improving flexibility before starting a rigorous strength training program.
Q 8. Describe your experience with different types of fitness assessments (e.g., muscular strength, endurance, flexibility).
My experience encompasses a wide range of fitness assessments, tailored to individual needs and goals. For muscular strength, I utilize methods like one-repetition maximum (1RM) testing for major muscle groups (e.g., bench press, squat, deadlift), as well as submaximal testing using various resistance exercises. For muscular endurance, assessments involve repetitions-to-failure protocols, such as push-up or sit-up tests, or timed exercises like plank holds. Flexibility is assessed using goniometry (measuring joint angles) or range-of-motion tests like the sit-and-reach test. I also incorporate functional movement screens, like the Functional Movement Screen (FMS), to evaluate overall movement patterns and identify potential weaknesses or imbalances. These assessments provide a comprehensive picture of an individual’s fitness level, helping to guide program design and track progress.
For example, a client aiming to improve upper body strength might undergo 1RM testing for bench press and overhead press. Conversely, a client focusing on core stability might be assessed using a plank test and various core stability exercises.
Q 9. How do you modify exercise programs for individuals with specific health conditions?
Modifying exercise programs for individuals with specific health conditions requires careful consideration and collaboration with healthcare professionals. It’s crucial to understand the limitations and potential risks associated with each condition. For example, a client with hypertension might need modifications to reduce intensity and avoid exercises that cause a significant increase in blood pressure. Similarly, someone with arthritis might require low-impact exercises to minimize joint stress. A client with diabetes may need adjustments to manage blood glucose levels effectively. This involves adjusting exercise intensity, duration, type, and frequency based on individual needs and physician recommendations. Prioritizing proper form and technique is paramount to prevent injury.
Let’s say a client has osteoarthritis in their knees. Instead of high-impact activities like running, we might substitute low-impact alternatives like swimming or cycling. We’d focus on exercises that strengthen the muscles supporting the knee joint, while avoiding movements that aggravate pain.
Q 10. Explain the concept of progressive overload in exercise prescription.
Progressive overload is a fundamental principle in exercise prescription. It refers to gradually increasing the demands placed on the body during exercise over time. This can be achieved by increasing the intensity, duration, or frequency of workouts. Think of it like this: if you always lift the same weight, your muscles adapt and stop growing. Progressive overload forces them to continually adapt and grow stronger. It’s crucial for continued improvement in strength, endurance, and overall fitness. This principle must be applied cautiously, however, to prevent overtraining and injury. Gradual increases are key. The rate of progression should be individualised, depending on factors like the client’s fitness level, training experience, and health status.
For example, a beginner might start with a 10-minute walk, then gradually increase the duration to 15, 20, and 30 minutes over several weeks before increasing intensity. Similarly, a weightlifter might add a small amount of weight, 2.5 lbs for example, each week to maintain progressive overload.
Q 11. How do you assess an individual’s readiness for exercise?
Assessing an individual’s readiness for exercise involves a multi-faceted approach. It begins with a thorough health history review, including any pre-existing conditions, medications, and previous injuries. This information helps identify potential risks and contraindications to exercise. Next, a physical examination may be necessary to assess cardiovascular health and musculoskeletal integrity. Finally, I would often use standardized questionnaires, like the Physical Activity Readiness Questionnaire (PAR-Q), to screen for potential health issues that might warrant medical clearance before starting an exercise program. The goal is to ensure the exercise program is safe and appropriate for the individual’s unique health status.
For instance, a client with a history of heart disease would require medical clearance before initiating any vigorous exercise program. This process ensures that the exercise prescription is safe and tailored to their specific needs.
Q 12. How do you design a safe and effective exercise program for a sedentary individual?
Designing a safe and effective exercise program for a sedentary individual requires a gradual and progressive approach. We start with a focus on building a base level of fitness. The initial phase should emphasize low-impact activities like walking or cycling to improve cardiovascular fitness without causing undue stress on the body. The program should then gradually increase in intensity and duration over time. Incorporating strength training exercises, starting with bodyweight exercises or light weights, is important for building muscle strength and improving bone density. Flexibility and balance exercises are crucial to improve mobility and reduce the risk of injury. Throughout the process, careful monitoring of the individual’s response to exercise and adjustments to the program as needed are crucial.
For a sedentary individual, a sample program might begin with 20 minutes of walking three times a week, gradually increasing the duration and then incorporating light strength training sessions twice a week. Always prioritize proper form and technique to minimize risk of injury.
Q 13. Explain the importance of proper warm-up and cool-down routines.
Proper warm-up and cool-down routines are essential components of any exercise program. A warm-up prepares the body for exercise by increasing blood flow to the muscles, increasing heart rate and body temperature, and improving joint mobility. This reduces the risk of injury and enhances performance. A typical warm-up might include light cardio, like jogging or jumping jacks, followed by dynamic stretches, like arm circles and leg swings. A cool-down helps the body gradually transition back to a resting state by lowering heart rate and reducing muscle soreness. This typically involves light cardio followed by static stretches, holding each stretch for 15-30 seconds.
Think of it like this: a warm-up is like prepping your engine before driving and the cool-down is like letting your engine idle before turning it off.
Q 14. How do you motivate clients to adhere to their exercise programs?
Motivating clients to adhere to their exercise programs requires a multifaceted approach. Setting realistic and attainable goals, tailored to individual needs and capabilities, is crucial. Regular communication, providing feedback, and celebrating successes helps maintain motivation. Incorporating variety into workouts keeps them engaging. Finding an exercise buddy or participating in group fitness classes can enhance accountability and social support. I frequently use motivational interviewing techniques, focusing on the client’s own intrinsic reasons for wanting to exercise. Tracking progress and celebrating milestones also reinforces commitment to the program.
For example, instead of focusing on weight loss, I might focus with a client on how exercise improves energy levels and mood which may be more personally relevant and motivating for them.
Q 15. What are the common signs and symptoms of exercise-related injuries?
Exercise-related injuries manifest in various ways, depending on the type and severity of the injury. Common signs and symptoms can be broadly categorized into:
- Pain: This is the most common indicator, ranging from mild soreness to sharp, debilitating pain. The location of pain can pinpoint the affected area, such as knee pain during running or lower back pain after weightlifting.
- Swelling: Inflammation and fluid buildup in the injured area cause swelling, often accompanied by redness and warmth.
- Stiffness: Restricted range of motion and difficulty moving the injured joint or muscle are common symptoms.
- Bruising: Discoloration of the skin due to bleeding under the skin.
- Weakness: Difficulty or inability to perform movements normally.
- Numbness or tingling: Nerve damage can lead to sensations of numbness or tingling.
- Deformity: In severe cases, there might be visible deformities, such as a bone fracture.
For example, a runner experiencing sharp pain in their knee accompanied by swelling and limited range of motion likely has a knee injury, potentially requiring medical attention. It’s crucial to distinguish between normal muscle soreness (delayed-onset muscle soreness or DOMS) and pain indicative of an injury. DOMS typically peaks 24-72 hours post-exercise and gradually subsides. Persistent or worsening pain warrants immediate assessment.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Don’t miss out on holiday savings! Build your dream resume with ResumeGemini’s ATS optimized templates.
Q 16. How do you respond to an exercise-related emergency?
Responding to an exercise-related emergency requires a calm and efficient approach. My first priority is to ensure the safety of the injured individual. The acronym RICE provides a useful framework:
- R – Rest: Stop the activity immediately and prevent further injury.
- I – Ice: Apply ice packs to the injured area for 15-20 minutes at a time, several times a day. This helps to reduce swelling and pain.
- C – Compression: Use a compression bandage to minimize swelling and support the injured area. Avoid over-tightening, which could restrict blood flow.
- E – Elevation: Elevate the injured limb above the heart to reduce swelling.
After applying RICE, I would assess the severity of the injury. For minor injuries, I would advise rest and monitoring. For more severe injuries, such as suspected fractures or dislocations, I would immediately call emergency medical services (EMS) and provide necessary first aid until their arrival. This would include monitoring vital signs, providing comfort, and preventing further injury. Effective communication with EMS is vital, providing clear and concise details about the injury and the individual’s condition. I am also trained in CPR and would use those skills if necessary.
Q 17. Describe your experience with using wearable technology for exercise monitoring.
I have extensive experience utilizing wearable technology for exercise monitoring, including smartwatches, fitness trackers, and heart rate monitors. These devices provide valuable data for both clients and myself. I use this data to:
- Track activity levels: Quantify daily steps, distance covered, and calories burned, which helps establish baseline activity and monitor progress toward goals.
- Monitor heart rate: Assess cardiovascular fitness and ensure clients stay within their target heart rate zones during exercise. This is crucial for safe and effective training.
- Assess sleep patterns: Sleep quality significantly impacts recovery and performance. Wearable technology provides insights into sleep duration and quality, helping to optimize training schedules and recovery strategies.
- Provide objective feedback: Data from wearables provides concrete evidence of progress, motivating clients and allowing for adjustments to exercise programs based on real-time data.
For example, I recently worked with a client struggling to lose weight. By using a fitness tracker to monitor her daily activity, we identified a significant lack of activity on rest days. We incorporated short walks and other light activity into her routine, leading to improved results. However, I always emphasize that wearable technology is a tool, not a replacement for professional assessment and guidance. Data should be interpreted within the context of the individual’s overall health and training goals.
Q 18. How do you communicate assessment results to clients in a clear and understandable manner?
Communicating assessment results effectively is paramount. I use a client-centered approach, ensuring the information is tailored to their understanding. I avoid using overly technical jargon. Instead, I use plain language, visuals, and analogies to illustrate key findings. My approach typically involves:
- A summary of the key findings: This provides an overview of the client’s fitness level and any limitations identified.
- Visual aids: Charts, graphs, and diagrams help to present data in a clear and easily digestible format.
- Relatable explanations: I use analogies and real-world examples to explain concepts, such as comparing fitness levels to different speeds on a bicycle.
- Open discussion: I encourage questions and address concerns, ensuring the client fully understands the results and the recommendations.
- Personalized plan of action: The results form the basis for a personalized exercise plan designed to meet the client’s specific goals and needs.
For instance, I might present a client with a bar graph showing their progress on a particular exercise over time, and explain the implications for setting future goals. I create a collaborative environment encouraging the client’s participation in the process and empower them to take ownership of their health.
Q 19. Describe your experience with different types of exercise equipment.
My experience encompasses a wide range of exercise equipment, including:
- Cardiovascular equipment: Treadmills, stationary bikes, elliptical trainers, stair climbers – I am adept at using and assessing these for cardiovascular fitness and helping clients learn proper form to prevent injuries.
- Resistance training equipment: Free weights (dumbbells, barbells), weight machines, resistance bands – I have experience designing programs using various equipment, focusing on proper form, progressive overload and injury prevention.
- Functional training equipment: Kettlebells, medicine balls, stability balls – I use these to develop practical strength, balance and coordination relevant to everyday activities.
- Bodyweight training: I utilize bodyweight exercises like push-ups, squats, and lunges for building strength and improving fitness without equipment.
My knowledge extends beyond simply operating this equipment. I understand the biomechanics of each exercise and can assess how it impacts different muscle groups. This allows me to design safe and effective workout programs for my clients, always focusing on proper technique and individualized needs. For example, I might choose resistance bands for a client recovering from a shoulder injury, focusing on building strength gradually without stressing the injured area.
Q 20. How do you tailor exercise programs to meet individual client goals and needs?
Tailoring exercise programs requires a thorough understanding of individual client needs and goals. My approach begins with a comprehensive assessment including fitness levels, medical history, goals, and limitations. I then design a program that incorporates:
- Specific goals: Are they aiming for weight loss, muscle gain, improved cardiovascular health, or something else? The program aligns directly with their objectives.
- Fitness level: Beginners require different programming than experienced athletes. I carefully consider intensity, duration, and frequency to ensure a safe and effective approach.
- Limitations: Pre-existing conditions or injuries require modifications. I work within those limitations to provide a safe and effective program.
- Preferences: I incorporate exercise types they enjoy, fostering adherence and motivation. If they prefer group classes over solo workouts, that influences the program design.
- Progressive overload: I gradually increase the intensity or duration of the workout over time, challenging the body and promoting continuous improvement.
For example, a client aiming for weight loss might receive a program combining cardiovascular training, strength training, and flexibility exercises, while a client focusing on muscle building might have a program emphasizing resistance training with high intensity intervals. Regular monitoring and feedback ensure ongoing adjustments are made as the client progresses.
Q 21. What are the ethical considerations related to exercise assessment and prescription?
Ethical considerations are paramount in exercise assessment and prescription. Key ethical principles I adhere to include:
- Confidentiality: Protecting client information is crucial, adhering to privacy regulations and ensuring data security.
- Informed consent: Clients must fully understand the assessment and prescription process before participating. This includes explaining potential risks and benefits.
- Competence: Providing services only within my scope of expertise. Referrals to other healthcare professionals are made when necessary.
- Objectivity: Conducting assessments and designing programs based on objective data and scientific principles, avoiding bias.
- Non-maleficence: Avoiding actions that could harm the client. Prioritizing safety and minimizing the risk of injury.
- Beneficence: Acting in the client’s best interest, designing programs that promote health and well-being.
For example, if a client discloses a heart condition, I would not design a high-intensity exercise program without first consulting with their physician. Maintaining a client’s trust and working ethically are essential for building strong professional relationships and ensuring positive outcomes. I always operate within the boundaries of my professional certifications and continuously strive for continuing education to maintain my standards.
Q 22. Explain the role of exercise in managing chronic diseases (e.g., diabetes, hypertension).
Exercise plays a crucial role in managing chronic diseases like diabetes and hypertension by improving various physiological factors. For example, in diabetes, regular physical activity enhances insulin sensitivity, meaning the body uses insulin more effectively to regulate blood sugar levels. This reduces the risk of hyperglycemia (high blood sugar) and its associated complications. Similarly, in hypertension (high blood pressure), exercise helps lower blood pressure by reducing vascular resistance and improving heart function. This is achieved through improvements in both systolic and diastolic blood pressure.
The type and intensity of exercise are tailored to the individual’s condition and capabilities. For a diabetic patient, moderate-intensity aerobic exercise like brisk walking or cycling for at least 150 minutes per week is often recommended. For someone with hypertension, a combination of aerobic and resistance training is beneficial. It’s vital to remember that exercise should be integrated alongside medication and dietary changes as part of a comprehensive management plan. Failure to consult with a healthcare professional before starting any exercise program is dangerous, especially for those with pre-existing conditions.
For instance, I worked with a client with type 2 diabetes who was struggling with fatigue and high blood sugar. We started with short, low-intensity walks, gradually increasing the duration and intensity as their fitness improved. We closely monitored their blood glucose levels and adjusted the program as needed. The positive change in their blood sugar control and overall energy levels were incredibly rewarding and demonstrated the power of exercise in managing chronic diseases.
Q 23. How do you ensure client safety during exercise sessions?
Client safety is my paramount concern. Before any exercise session begins, I conduct a thorough health screening, including reviewing medical history, current medications, and assessing their physical limitations. I use standardized questionnaires like the PAR-Q (Physical Activity Readiness Questionnaire) and conduct relevant physical assessments to identify potential risks. This detailed assessment allows me to design safe and effective exercise programs customized to each individual’s needs.
During exercise sessions, I continuously monitor my clients’ vital signs (heart rate, blood pressure, perceived exertion) and observe their body language for any signs of discomfort or distress. I emphasize proper exercise technique to minimize the risk of injury. I also ensure the exercise environment is safe and well-equipped, with readily available emergency equipment and communication systems. Finally, I provide clear and concise instructions and encourage open communication to ensure clients feel comfortable reporting any issues. Think of it like a pilot performing pre-flight checks and continuously monitoring their instruments during a flight.
For example, if a client begins to experience chest pain during an exercise session, I immediately stop the activity, call for medical assistance if necessary, and provide appropriate first aid. Regularly scheduled check-ins and communication throughout the program are imperative to maintain the client’s safety.
Q 24. What are your preferred methods for documenting exercise assessments and progress?
I utilize a combination of methods for documenting exercise assessments and progress to ensure a comprehensive and easily accessible record. I maintain detailed electronic health records (EHRs) that include the client’s initial assessment data, including medical history, physical assessments (e.g., body composition, blood pressure, cardiovascular fitness tests), and exercise prescription. Progress notes are meticulously recorded after each session, documenting the exercises performed, duration, intensity, client response, and any observed changes or modifications.
I also use digital tools to track client progress objectively. This might include wearable technology to monitor heart rate, step count, and sleep patterns, or specialized fitness apps for recording workout data. Client self-reporting via questionnaires or feedback forms complements these objective measures, giving a holistic view of their progress. Finally, I regularly review and analyze the data to make informed decisions about adjusting exercise programs and ensuring client progress is on track. This data-driven approach facilitates clear communication with the client and other healthcare professionals involved in their care.
Q 25. How do you stay current with the latest research and best practices in exercise assessment and evaluation?
Staying current in this rapidly evolving field requires ongoing professional development. I regularly attend conferences, workshops, and seminars presented by professional organizations like the American College of Sports Medicine (ACSM) and the National Strength and Conditioning Association (NSCA). I also actively read peer-reviewed journals and subscribe to reputable online resources to stay informed about the latest research findings and evidence-based best practices. Participating in continuing education courses ensures my skills and knowledge are always up to date, allowing me to provide the most effective and safe exercise interventions. I actively seek out opportunities for mentoring and collaboration with other professionals in the field to learn and share knowledge.
Q 26. Describe a challenging situation you encountered during an exercise assessment and how you overcame it.
During an assessment, a client revealed a previously undisclosed history of a heart condition, significantly altering the safety considerations. My initial assessment plan involved more intense cardiovascular exercise, which was now unsuitable. To overcome this, I immediately revised the plan and prioritized a thorough discussion with the client about their medical history and current limitations. I contacted their cardiologist to get clearance and recommendations. The revised plan involved low-impact, low-intensity exercises that minimized cardiovascular stress, focusing on strength training and flexibility exercises. Regular monitoring and communication were increased to ensure safety. The situation highlighted the importance of open communication, continuous monitoring, and the necessity to adapt plans based on new information. Ultimately, we were able to devise a program that met the client’s needs while prioritizing their safety and well-being.
Q 27. How do you integrate client feedback into your exercise programs?
Client feedback is essential for creating effective and sustainable exercise programs. I regularly solicit feedback through informal conversations, structured questionnaires, and progress reviews. These discussions assess not only the program’s effectiveness but also address the client’s experience, enjoyment, and any challenges they’re encountering. This feedback informs adjustments to the exercise prescription, including modifications to intensity, duration, type of exercise, or scheduling. For example, if a client expresses difficulty with a particular exercise, I’ll either modify the exercise or find an alternative that achieves similar results without causing pain or frustration. Open and honest communication is vital to ensure the program aligns with the client’s preferences and promotes long-term adherence.
Q 28. What are your career goals in the field of exercise assessment and evaluation?
My career goals involve specializing in exercise assessment and rehabilitation for individuals with chronic conditions. I aim to expand my expertise in evidence-based exercise prescription and personalized training methods. This includes pursuing further education and certifications in specialized areas like cardiac rehabilitation or diabetes management. I also aspire to contribute to the advancement of the field through research and collaboration. My ultimate goal is to positively impact the lives of individuals with chronic diseases by helping them improve their physical health and overall well-being through the power of exercise.
Key Topics to Learn for Exercise Assessment and Evaluation Interview
- Exercise Prescription: Understanding principles of exercise prescription based on individual needs, goals, and limitations. This includes considering factors like age, fitness level, and medical history.
- Assessment Techniques: Mastering various methods for assessing fitness components (e.g., cardiovascular fitness, muscular strength and endurance, flexibility). Practical application involves understanding the limitations and validity of each technique.
- Test Selection and Administration: Learning how to choose appropriate tests based on client needs and available resources. This includes proper administration and ensuring test validity and reliability.
- Data Analysis and Interpretation: Developing skills in analyzing collected data to create meaningful reports and recommendations. This involves understanding statistical concepts relevant to fitness assessment.
- Program Design and Evaluation: Knowing how to design and implement effective exercise programs based on assessment results and adjusting the program as needed based on client progress and feedback.
- Risk Stratification and Safety: Identifying and mitigating potential risks associated with exercise. Understanding screening procedures and contraindications for specific populations.
- Ethical Considerations: Understanding professional ethics and legal responsibilities in the field of exercise assessment and evaluation.
- Technology and Software: Familiarity with software and technology used for data collection, analysis, and program management (this could vary depending on the specific job).
- Communication and Client Interaction: Developing strong communication skills to effectively interact with clients, explain assessment results, and provide motivation and support.
Next Steps
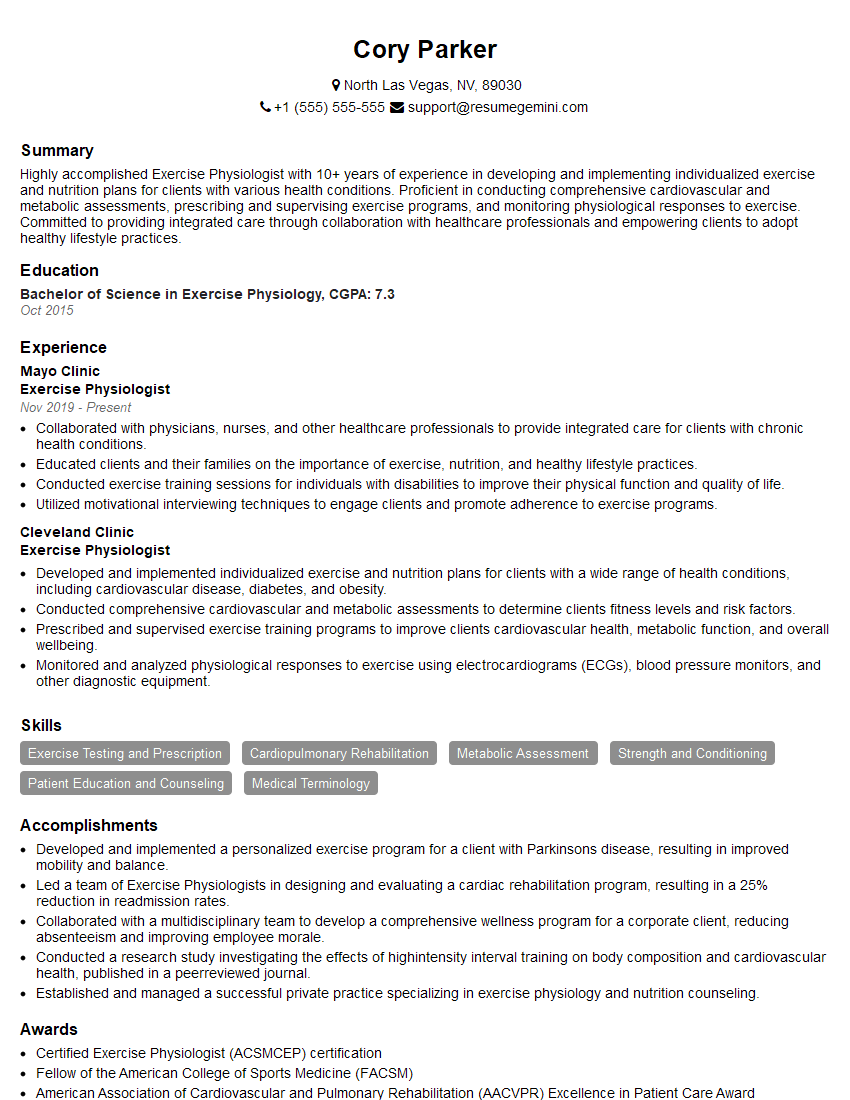
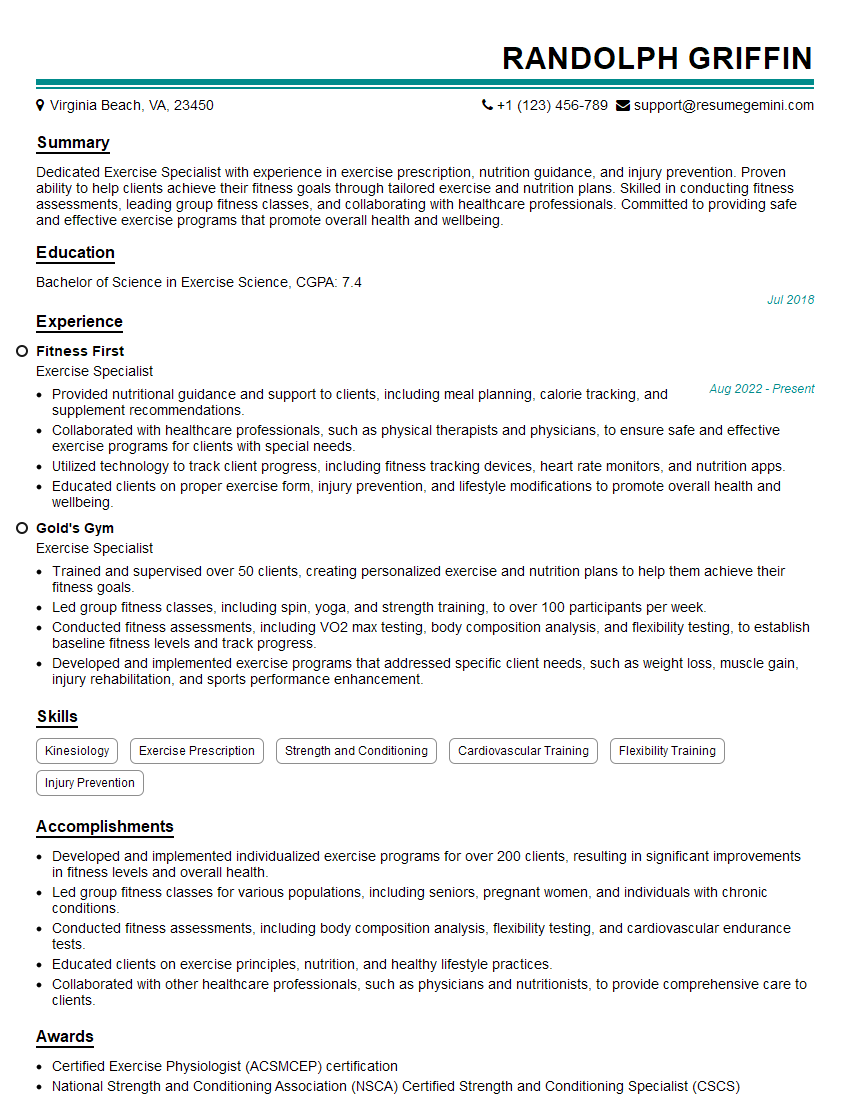
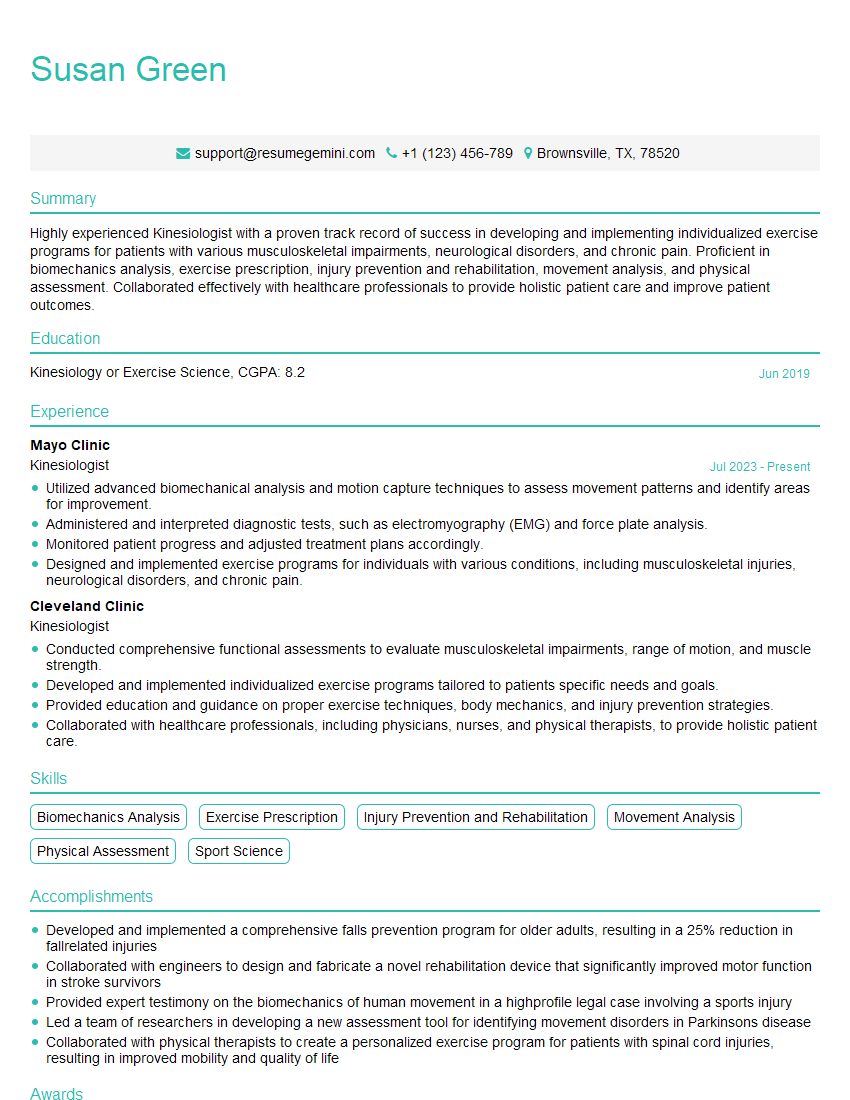
Mastering Exercise Assessment and Evaluation is crucial for career advancement in health and fitness. A strong understanding of these principles sets you apart and demonstrates your commitment to client safety and effective program design. To increase your chances of securing your dream role, crafting an ATS-friendly resume is paramount. Use ResumeGemini to build a professional resume that highlights your skills and experience effectively. ResumeGemini provides examples of resumes tailored to Exercise Assessment and Evaluation roles to help you create a compelling application.
Explore more articles
Users Rating of Our Blogs
Share Your Experience
We value your feedback! Please rate our content and share your thoughts (optional).
What Readers Say About Our Blog
Hi, I have something for you and recorded a quick Loom video to show the kind of value I can bring to you.
Even if we don’t work together, I’m confident you’ll take away something valuable and learn a few new ideas.
Here’s the link: https://bit.ly/loom-video-daniel
Would love your thoughts after watching!
– Daniel
This was kind of a unique content I found around the specialized skills. Very helpful questions and good detailed answers.
Very Helpful blog, thank you Interviewgemini team.